Abstract
Fibroadenomas are benign breast masses that can present a management challenge in adolescent populations. Most fibroadenomas may be managed conservatively without surgery, but those masses that are symptomatic or increasing in size may require surgical excision. In adolescents, the implications of surgical intervention in the breast are unclear, and there is little outcomes data. In this article, the authors discuss the presentation, diagnosis, and management of fibroadenoma in adolescents. Key considerations for physicians in treating these masses in this population are reviewed.
Keywords: fibroadenoma, breast, adolescent
Fibroadenomas are the most common breast masses in adolescents. They may present a challenge for physicians as treatment guidelines are lacking in this population. Fibroadenomas generally present as 2 to 3 cm in size, but they may increase to > 10 cm and cause associated breast asymmetry and/or hypertrophy. Types of fibroadenoma include juvenile, cellular, or giant. Differentiation must be made between giant fibroadenoma and juvenile hypertrophy. Adolescent patients who present with breast masses should undergo a detailed evaluation to assess the mass, including an ultrasound. If malignancy is ruled out, a fibroadenoma confirmed by imaging studies that is stable in size may be managed with careful observation and follow-up. Surgical excision of the fibroadenoma may be performed if the mass is symptomatic and/or rapidly growing. There are limited data on long-term outcomes after fibroadenoma excision in adolescents and no recommendations have been made regarding the optimal timing of reconstructive surgery if needed. Surgeons should discuss potential outcomes, cosmetic results, and the need for reconstructive surgery with patients prior to surgery and at subsequent follow-up appointments.
Presentation
Fibroadenomas are the most common surgically treated breast masses in adolescents, accounting for 44 to 94% of biopsied breast lesions.1 Fibroadenomas present as firm, nontender, clearly demarcated masses usually 2 to 3 cm in size, though they may range from < 1 cm to greater than 10. They are most commonly found in the upper-outer quadrant of the breast. These benign masses may enlarge slowly without associated pain or nipple and skin changes, but fluctuations in size may occur with the menstrual cycle; when symptoms are present, they last an average of 5 months.2 Patients may also have associated breast asymmetry. Multiple fibroadenomas occur in 10 to 25% of cases.3,4 In adolescents, the mass regresses completely between 10 and 40% of the time.1,5
Fibroadenomas are a stromal and epithelial proliferation arising from the terminal duct-lobular unit, though there are several histological variants. Juvenile fibroadenomas account for 7 to 8% of all fibroadenomas, occur most often in African American adolescents, and present as rapidly growing masses with associated skin ulcerations and prominent veins.4,6,7 The term cellular fibroadenoma is sometimes used to refer to juvenile fibroadenomas. Giant fibroadenomas are masses > 5 cm in diameter that display progressive, more rapid growth and have a greater degree of stromal cellularity. Giant fibroadenomas may replace and compress normal breast tissue and they may be initially mistaken for normal tissue. Differentiating between giant fibroadenoma and juvenile hypertrophy may be challenging, but juvenile hypertrophy is most often bilateral.4
Diagnosis
Patients who present with breast masses should undergo a medical evaluation, which includes detailed medical and family histories, the occurrence of any previous breast-related issues, history of any malignancy or mantle radiation, and constitutional symptoms. Providers should inquire about mass location, duration, change in size, whether it may be dependent on menses, associated pain or discharge, and the occurrence of additional masses. The physical exam should also assess size, mobility, and consistency of the mass. Attempts should be made to produce nipple discharge and palpation of the axillary lymph nodes should also be performed.4
Management
The diagnosis of a fibroadenoma in an adolescent presents unique challenges in treatment as compared with adults. Malignancy is rare in the adolescent population, but the discovery of a breast lump in a teenager may incite anxiety and worry in the patient and family. Furthermore, patients may be at increased risk of invasive breast cancer later in life,8,9 though this risk has not been quantified. Although there are no established standards of care for fibroadenomas in adolescents, considerations of treating fibroadenoma in adolescents include effectively communicating the risks and benefits of treatment options, reassurance that the mass is most likely benign, and the need for either excision or observation and continued follow-up.
Initial management of a mass thought to be fibroadenoma should include observation over at least one complete menstrual cycle, assuming a normal menstrual pattern. If the breast mass persists, imaging studies can be performed to determine if the mass is consistent with a fibroadenoma. Ultrasound is the most commonly used method to image breast masses in adolescents.10 This method can determine whether a mass is solid or cystic, although ultrasonography is limited when distinguishing between solid masses such as a fibroadenoma and a phyllodes tumor, a potentially malignant lesion.11 Serial ultrasounds may be useful to objectively document changes in size over time. Magnetic resonance imaging (MRI) and mammography are alternative techniques, but have not been recommended for use in adolescents due to the density of breast tissue in this population.6,12
A fibroadenoma confirmed by imaging studies that is small and not increasing in size may be managed with careful observation and follow-up. In the developing breast, the risk of iatrogenic injury may outweigh the benefits of surgery, especially because the risk of malignancy is low and fibroadenomas often resolve over time. Fine needle aspiration or core needle biopsy may be done, but these techniques present similar iatrogenic risks in the developing breast.6 Cryoablation has been used successfully in adults, but there are few reports in adolescents.
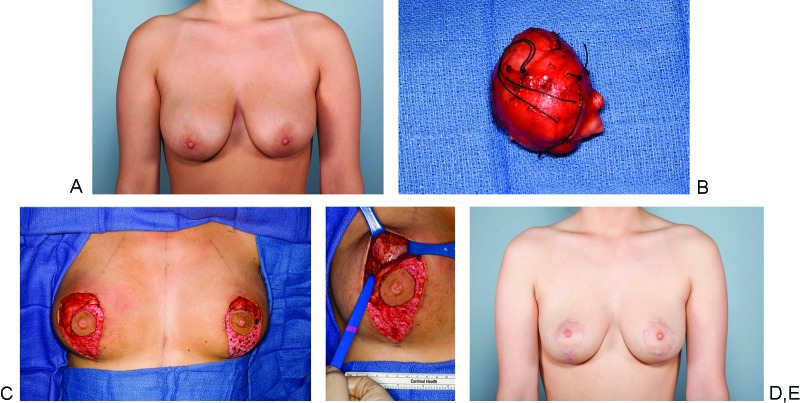
Surgical excision of the fibroadenoma may be performed if the mass is symptomatic and/or rapidly growing (Fig. 1). Juvenile fibroadenomas are typically treated surgically due to rapid growth, and giant fibroadenomas are excised due to size. Surgical excision of smaller fibroadenomas may be offered when masses are nonmobile, hard, enlarging, tender, fixed to overlying skin or nipple areolar complex, associated with axillary or supraclavicular lymphadenopathy, or the patient is experiencing undue anxiety because of the mass.4
Fig. 1.
(A) Enlarging fibroadenoma of the left breast and giant fibroadenoma of the right breast in a 17- year-old female. (B) Giant fibroadenoma measuring 5.7 × 5.8 × 5.0 cm. Note the solid, multinodular, well-circumscribed features of the mass. The left breast fibroadenoma (not shown) measured 2.7 × 2.4 × 2.2 cm. (C) Intraoperative incision planning by the breast surgeon and the plastic surgeon. Immediate breast reconstruction was planned due to the large size of the right breast mass and anticipated breast asymmetry following excision. Local advancement flaps of superior and inferior breast tissue were performed via a vertical scar mastopexy approach. (D) Right breast defect postresection of giant fibroadenoma, involving the upper-outer quadrant. (E) Postoperative result at one year. (Courtesy of Valerie Lemaine, MD, MPH, FRCSC)
Excision of fibroadenomas can be done under local and/or general anesthesia. The optimal incision is circumareolar or in the inframammary crease to minimize visible scarring; however, the size and location of the mass may ultimately guide the incision location and length. Curvilinear or semilunar incisions directly over the mass may be the best choice if the fibroadenoma is located further from the areolar border. Total enucleation of the mass should be performed.1,4,13 Masses that encompass more than one-third of the breast may be removed through an inframammary crease incision and may require drain placement.4 Alternatively, MRI-guided ultrasound surgery or ultrasound-guided cryoablation have resulted in good results in adolescents and adults, but these techniques are not widely used.14,15
Postoperatively, patients should refrain from strenuous activity for 6 to 8 weeks and wear compression vests or sports bras for 4 to 6 weeks to minimize swelling and pain. Patients should be examined around 4 and 8 weeks postoperatively, every 3 months for the next year, biannually for the second year, and then annually. These exams will assess any complications, recurrence of the mass, and additional incident masses. Patients may experience postoperative cosmetic deformity or secondary asymmetry, especially after the removal of a giant fibroadenoma, but reconstructive surgery is usually not considered until at least one year after the procedure and the patient has reached skeletal maturity. Additionally, the breast parenchyma may expand to fill a resulting defect and resolve any deformities over the course of development.1,16 In fact, we have observed young women with breast asymmetry who underwent excision of giant fibroadenomas during adolescence in whom the affected breast grew to be significantly larger than the unaffected side. There is limited data on long-term outcomes after fibroadenoma excision and no recommendations have been made about the exact timing of reconstructive surgery if needed. Surgeons should discuss all potential outcomes, expectations of aesthetic results, and the need for reconstructive surgery with patients prior to surgery and at subsequent follow-up appointments.
Conclusion
Fibroadenomas are the most common benign breast masses in adolescents, but management may present challenges if the mass is not resolving, is increasing in size, or is symptomatic. Diagnosis of fibroadenoma should entail a detailed medical evaluation with imaging studies. Management of fibroadenoma may be conservative, but excision by total enucleation of the mass may be performed. Patients should undergo regular follow-up to assess complications, measure outcomes, and evaluate the need for subsequent reconstructive surgery. Throughout treatment, patients should be counseled about the benign nature of the mass, the different surgical and nonsurgical approaches, and the need for continued follow-up to determine if additional surgery is necessary. More long-term outcomes data are needed to inform treatment recommendations for adolescent patients presenting with fibroadenomas of the breast.
References
- 1.Jayasinghe Y, Simmons P S. Fibroadenomas in adolescence. Curr Opin Obstet Gynecol. 2009;21(5):402–406. doi: 10.1097/GCO.0b013e32832fa06b. [DOI] [PubMed] [Google Scholar]
- 2.Turbey W J, Buntain W L, Dudgeon D L. The surgical management of pediatric breast masses. Pediatrics. 1975;56(5):736–739. [PubMed] [Google Scholar]
- 3.Diehl T, Kaplan D W. Breast masses in adolescent females. J Adolesc Health Care. 1985;6(5):353–357. doi: 10.1016/s0197-0070(85)80002-4. [DOI] [PubMed] [Google Scholar]
- 4.Divasta A D, Weldon C, Labow B I. Philadelphia, PA: Lippincott, Williams & Wilkins; 2012. The breast: examination and lesions; pp. 405–420. [Google Scholar]
- 5.Neinstein L S, Atkinson J, Diament M. Prevalence and longitudinal study of breast masses in adolescents. J Adolesc Health. 1993;14(4):277–281. doi: 10.1016/1054-139x(93)90174-n. [DOI] [PubMed] [Google Scholar]
- 6.Chung E M, Cube R, Hall G J, González C, Stocker J T, Glassman L M. From the archives of the AFIP: breast masses in children and adolescents: radiologic-pathologic correlation. Radiographics. 2009;29(3):907–931. doi: 10.1148/rg.293095010. [DOI] [PubMed] [Google Scholar]
- 7.Pettinato G, Manivel J C, Kelly D R, Wold L E, Dehner L P. Lesions of the breast in children exclusive of typical fibroadenoma and gynecomastia. A clinicopathologic study of 113 cases. Pathol Annu. 1989;24(Pt 2):296–328. [PubMed] [Google Scholar]
- 8.Dupont W D, Page D L, Parl F F. et al. Long-term risk of breast cancer in women with fibroadenoma. N Engl J Med. 1994;331(1):10–15. doi: 10.1056/NEJM199407073310103. [DOI] [PubMed] [Google Scholar]
- 9.El-Wakeel H, Umpleby H C. Systematic review of fibroadenoma as a risk factor for breast cancer. Breast. 2003;12(5):302–307. doi: 10.1016/s0960-9776(03)00123-1. [DOI] [PubMed] [Google Scholar]
- 10.García C J, Espinoza A, Dinamarca V. et al. Breast US in children and adolescents. Radiographics. 2000;20(6):1605–1612. doi: 10.1148/radiographics.20.6.g00nv171605. [DOI] [PubMed] [Google Scholar]
- 11.Yilmaz E, Sal S, Lebe B. Differentiation of phyllodes tumors versus fibroadenomas. Acta Radiol. 2002;43(1):34–39. doi: 10.1080/028418502127347619. [DOI] [PubMed] [Google Scholar]
- 12.Williams S M, Kaplan P A, Petersen J C, Lieberman R P. Mammography in women under age 30: is there clinical benefit? Radiology. 1986;161(1):49–51. doi: 10.1148/radiology.161.1.3763885. [DOI] [PubMed] [Google Scholar]
- 13.Chang D S, McGrath M H. Management of benign tumors of the adolescent breast. Plast Reconstr Surg. 2007;120(1):13e–19e. doi: 10.1097/01.prs.0000264396.03452.62. [DOI] [PubMed] [Google Scholar]
- 14.Jolesz F A, Hynynen K. Magnetic resonance image-guided focused ultrasound surgery. Cancer J. 2002;8 01:S100–S112. [PubMed] [Google Scholar]
- 15.Kaufman C S, Bachman B, Littrup P J. et al. Office-based ultrasound-guided cryoablation of breast fibroadenomas. Am J Surg. 2002;184(5):394–400. doi: 10.1016/s0002-9610(02)01010-3. [DOI] [PubMed] [Google Scholar]
- 16.Gobbi D, Dall'Igna P, Alaggio R, Nitti D, Cecchetto G. Giant fibroadenoma of the breast in adolescents: report of 2 cases. J Pediatr Surg. 2009;44(2):e39–e41. doi: 10.1016/j.jpedsurg.2008.11.041. [DOI] [PubMed] [Google Scholar]