Abstract
Objectives:
Ketamine is a non-barbiturate agent with rapid action onset that induces profound sedation; however, some emergency physicians tend not to use ketamine because of the risk of emergence delirium (ED). This study aimed to evaluate the effectiveness of haloperidol prophylaxis in postoperative ketamine delirium in children.
Methods:
Prospective data relating to any emergence dreams, delirium, hallucinations, agitation, crying, altered perceptions, and necessary interventions were recorded in consecutive cases of ketamine delirium in patients attending Mansoura University Hospital, Egypt, from June 2010 to May 2011.
Results:
A total of 537 records were available for analysis. Of those, 267 received prophylactic haloperidol (49.7%). There were significant differences between the two groups regarding post-anaesthetic care unit behaviour. The ketamine-haloperidol groups included more patients who were sleepy, calm (P ≤0.01) and less irritable (P ≤0.01), with a lower incidence of crying (P ≤0.01) and disorientation (P ≤0.01).
Conclusion:
We found that preoperative administration of haloperidol decreases the incidence of postoperative delirium in a sample of Egyptian children undergoing minor surgery. This is congruent with earlier work conducted in adults. This work carries great hope to decrease and even prevent ED in hospitalised, non-surgical patients.
Keywords: Ketamine, Anesthesia, Children, Delirium, Haloperidol, Egypt
Advances in Knowledge
- This study is unique in investigating the use of prophylactic haloperidol in children to reduce postoperative ketamine delirium in our region.
- The results of this study revealed that the preoperative administration of haloperidol will reduce the incidence of postoperative delirium in children undergoing minor surgery.
Applications to Patient Care
- This study throws light on the possibility of haloperidol use in hospitalised patients to decrease or even prevent delirium.
Ketamine is a non-barbiturate agent with a rapid onset of action that induces profound analgaesia, sedation, and amnesia, with a short duration of action (15–30 minutes) and hence is associated with rapid recovery.1,2 Ketamine appears to have both central nervous system action and local anaesthetic properties. The main effects of this drug are mediated by the noncompetitive antagonism of the N-methyl-D-aspartate (NMDA) receptor in addition to binding to the muscarinic and opioid receptors.3
The main advantage of ketamine over other categories of sedatives lies in maintaining airway reflexes with minimal cardiovascular and respiratory side effects.4 Ketamine-induced emergence delirium (ED) is characterised by restlessness, agitation, and combativeness, and a non-cognisant state in relation to the patient’s surroundings. Transient physical restraint may be the only way to deal with the patients’ disorientation.5,6 Anaesthesiologists attempt to prevent patients from having such adverse effects by the co-administration of short acting benzodiazepine (midazolam). Early anaesthetic literature supports this practice.7,8 The rate of emergence agitation with midazolam displayed no change when comparing ketamine alone to a combination of ketamine and midazolam.9,10
Haloperidol is another psychotropic medication that has been commonly used for the treatment of elderly and adult delirium.11 Haloperidol prophylaxis has been a matter of debate in the last two decades. Schrader et al. used haloperidol with a dose of 0.5 mg three times daily in the elderly, resulting in a reduction of delirium duration (from a mean of 11.8 to 5.4 days) and length of hospital stay in affected participants (from a mean of 22.6 to 17.1 days).12 However, Atlas and Milles used haloperidol for the treatment of adult ketamine-induced ED in a single dose of 5 mg, administered intravenously (IV) to control delirium following maxillofacial surgery.13 Delirium among children and adolescents was managed well by haloperidol.14 In children with psychomotor agitation that was acutely threatening to their health status, IV haloperidol (at a loading dosage of 0.15–0.25 mg) was used over a period of 30–45 minutes, followed by a maintenance dose of 0.05–0.5 mg/Kg/24 hour.15–17 Critically ill children reportedly tolerate doses up to 1–1.5 mg/Kg/day (maximum 230 mg).18–20
The pharmacological half-life of haloperidol is significantly longer than that of ketamine. Specifically, haloperidol has a half-life of 14 to 26 hours, whereas ketamine has a half-life of 15 minutes for its alpha phase and 2.5 hours for its beta phase.21,13 Therefore, multiple doses or infusions of haloperidol would ordinarily not be necessary for the treatment of ketamine-induced ED. Normally, a single dose should suffice.22
Haloperidol is associated with cardiac dysrythmias and extrapyramidal side effects such as dystonia, tardative dyskinesia, akathisia, and neuroleptic malignant syndrome.23,24 However, these side effects occur infrequently, this is particularly notable given the relatively low dose of haloperidol which appears necessary for the treatment of ketamine-induced ED.22,25
To the best of the authors’ knowledge, no similar studies have been conducted in children who received haloperidol for the sake of preventing consequent postoperative ED. Furthermore, most of the studies were carried out in developed countries. This work aimed to evaluate the effectiveness of haloperidol prophylaxis on postoperative ketamine-induced delirium in children. The authors hypothesised that preoperative administration of haloperidol would greatly decrease the incidence of postoperative ED.
Methods
The subjects for this clinical prospective randomised study were 537 consecutive children undergoing minor surgery at the Mansoura University Hospital in Mansoura City, Egypt, between June 2010 and May 2011. Eligibility criteria included children aged 6–16 years undergoing removal of stitches, laceration repair, removal of foreign bodies, abscess incision and drainage, and any examination for which general anaesthesia was required. Inclusion criteria included those classified under the American Society of Anaesthesiologists’ (ASA) designations of class I or II. Exclusion criteria included children allergic to ketamine, those with porphyria or active respiratory tract infections, and those undergoing surgery of the oropharynx. Patients with hepatic or renal impairment or a previous history of psychiatric illness, or those taking antidepressants, benzodiazepines, or antipsychotics were also excluded.
Written informed consent was signed by a parent of each patient. For all patients, tests of preoperative liver or renal function, evaluations of the patient’s complete blood count and coagulation profile, and tests for levels of blood sugar and serum electrolytes were done. A systematic sample was taken (a sample design in which a list of the population is used as a sampling frame and cases are selected by skipping through the list at regular intervals) and the patients were classified into two groups. One hour before the start of anaesthesia, patients in Group I (haloperidol group, n = 267) were given a haloperidol 0.025 mg/Kg in 5 ml of distilled water IV while patients in Group II (placebo group, n = 270) were given a 5 ml distilled water IV. All equipment for intubation and ventilation was kept on standby. Anaesthesia was induced by ketamine 0.5–1 mg/Kg IV and increments as needed to facilitate surgery. The ASA standard of monitoring was carried out in the form of peripheral oxygen saturation, indirect blood pressure, and an electrocardiogram (ECG) and pulse rate were taken at intervals of 5 minutes during the procedure and 10 minutes during recovery. At the end of the surgery, the patients were moved to the post-anaesthesia care unit (PACU) which was under the supervision of an anaesthesiologist. For all patients, pain was assessed and treated so as to obtain a pain level <4 on the 0–10 visual analogue scale (VAS).26 Paracetamol (Perfalgan®) was given at a dose of 15 mg/Kg every 4–6 hours as a slow IV infusion over 15 minutes, for pain registering at a VAS score of above 3.
At the PACU, which was also staffed by a well-qualified nurses, the parents were guided to give their children psychological support, and there was no need to dim the lights or eliminate auditory and visual stimuli. As recommended by Cole et al., a prospective observation of the children’s behaviour was made in the recovery room 30 minutes after the patient’s arrival in the PACU.27 The children were eventually discharged under the supervision of the family and the treating physician. A follow-up telephone call was carried out by the research assistant and or the authors at the end of the first postoperative month.
Data were analysed using the Statistical Package for Social Sciences (SPSS), Version 11 (IBM, Inc., Chicago, Illinois, USA). Quantitative variables were tested for normality distribution by the Kolmogorov-Smirnov test. Quantitative variables were displayed as mean ± standard deviation (SD). Qualitative variables were presented as numbers and percentages. The differences between the means of the two groups were assessed using an independent t-test. The chi-square test was used for comparison of count and percentage of the two groups. A value of P ≤0.05 was considered statistically significant.
Results
A total of 537 children (386 males, 151 females) at Mansoura University Hospital were anaesthetised in 2010–2011 for minor surgery. The mean ages for the first group and second group were 10.69 ± 2.3 years and 10.98 ± 2.8 years, respectively. The mean anaesthesia time for the first and second groups was 23.8 ± 5.6 minutes and 24.4 ± 4.7 minutes, respectively. The mean surgery times for the first and second groups were 17.9 ± 3.9 minutes and 18.4 ± 3.5 minutes, respectively. The patients’ demographic features are shown in Table 1.
Table 1:
Pertinent characteristics of the study subjects
| Ketamine (n = 270) | Ketamine and haloperidol (n = 267) | P value | |
|---|---|---|---|
| Age | 10.69 ± 2.3 | 10.98 ± 2.8 | 0.19 |
| Weight | 34.9 ± 11.3 | 36.2 ± 9.4 | 0.148 |
| Anaesthesia time | 23.8 ± 5.6 | 24.4 ± 4.7 | 0.1795 |
| Surgical time (minutes) | 17.9 ± 3.9 | 18.4 ± 3.5 | 0.1186 |
| Sex (M/F) | 202/68 | 184/83 | 0.128 |
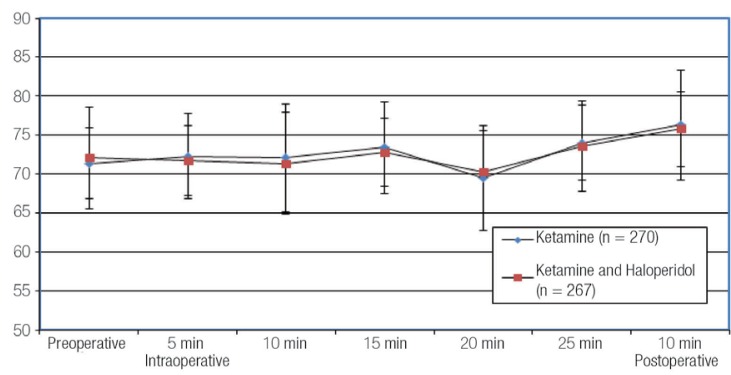
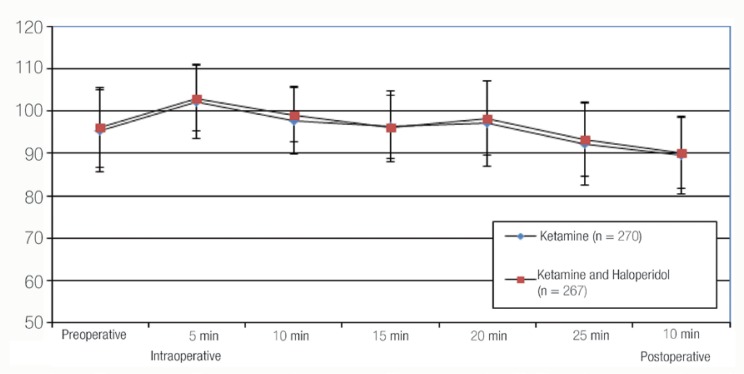
Insignificant haemodynamic changes were observed preoperatively, every five minutes intraoperatively and postoperatively between the two groups for both indirect blood pressure and heart rate [Figures 1 and 2].
Figure 1:
Mean blood pressure in the studied groups.
Figure 2:
Heart rate in the studied groups.
There were significant PACU behavioural differences between the two groups. The ketaminehaloperidol group yielded more sleepy, calm patients. In contrast, the ketamine group showed more irritability, inconsolable crying, and disorientation [Table 2]. There was a significant difference in VAS. The mean was 3.8 for the ketamine group and 2.1 for the ketamine-haloperidol group (P <0.001). The mean PACU stay duration for the ketamine group was 143.6 ± 12.9 minutes. For the ketamine-halperidol group it was 56.4 ± 8.7 minutes (P = 0.000).
Table 2:
Observations of child behaviour in the recovery room.
| Feature | Ketamine (n = 270) n (%) | Ketamine and haloperidol (n = 267) n (%) | P |
|---|---|---|---|
| Sleeping | 175 (64.8) | 234 (87.6) | 0.004** |
| Awake, calm | 41 (15.2) | 17 (6.4) | 0.002** |
| Irritable, crying | 21 (7.8) | 6 (2.2) | 0.004** |
| Inconsolable crying | 16 (5.9) | 5 (1.9) | 0.016* |
| (Severe restlessness) disorientation | 17 (6.3) | 5 (1.9) | 0.01** |
P = P value;
* = significant (P ≤0.05);
** = highly significant (P ≤0.01).
A telephone follow-up was attempted in all cases, and was successful in 434 patients (80.8%). In the haloperidol group, three patients (1.1%) experienced extrapyramidal side effects in the form of a dystonic reaction. In the ketamine group,11 4.07% of patients reported nightmares. Two could not see properly and one complained of the room spinning in the postoperative weeks. In the ketamine-haloperidol group, only two (0.75%) patients reported difficulties—one of them reported crying and another reported having nightmares (P 0.0126).
Discussion
Kalisvaart et al. reported that haloperidol prophylaxis significantly reduced the severity and duration of delirium and facilitated a rapid discharge from hospital.28 In a retrospective cohort study, Milbrandt et al.29 reported that haloperidol use was associated with a decreased mortality rate in mechanically ventilated patients.30 As a result, the burden of postoperative delirium on the patients and caregivers was less, as was the number of days patients stayed in the intensive care unit (ICU). In this study, we found that preoperative administration of haloperidol decreased the incidence of postoperative delirium from 6.3% to 1.9% in a sample of children undergoing minor surgery in Mansoura, Egypt, which is congruent with earlier work conducted in elderly adults.11 Moreover, haloperidol prophylaxis was found to be better than other medications used in previous paediatric practice. Midazolam is often combined with small doses of ketamine for sedation during local anaesthesia because it attenuates the cardiostimulatory response of ketamine and prevents unpleasant emergence reactions.31 Unfortunately, when small doses of ketamine are administered in combination with midazolam, patients may still become confused, disoriented, and experience vivid dreaming or blurred vision during the operation.32,33
Extrapyramidal symptoms, hypotension, altered cardiac conduction, and sedation are side effects associated with haloperidol and are dose-dependent; hence, it is advised that low doses of haloperidol are given for short periods of time, especially for elderly patients. In our study, it was administered IV by a bolus injection (0.5 mg), followed by a continuous infusion (at a rate of 0.1 mg/hour) for 12 hours. The aim of the bolus injection was to facilitate the patient reaching a therapeutic blood level rapidly once the drug was started. The bolus dose was chosen according to the suggested starting dose for the treatment of delirium in elderly patients.34 In critical children, haloperidol has to be given by IV, but continuous IV is associated with a more stable plasma level.35,36 In contrast to other studies, we used prophylactic haloperidol for a much shorter period of time in order to limit the ICU stay (143.6 ± 12.9 minutes; for the ketamine-haloperidol group the stay was 56.4 ± 8.7 minutes) and it decreased the incidence, course, and complications of early postoperative delirium.28,35
In our study, the use of haloperidol had a positive effect in reducing the duration of the PACU stay (143.6 ± 12.9 minutes for the ketamine group and 56.4 ± 8.7 minutes for the ketaminehaloperidol group). Honkaniemi et al. reported that the use of 5 mg of haloperidol in patients with migraines decreased VAS values. The current study also showed that the VAS was less in the ketamine-haloperidol group as compared to the ketamine group, as evidenced by more patients being able to remain sleepy and calm.37 Generally, low doses of haloperidol have been adequate in eliminating, or significantly reducing, the ED associated with ketamine. It is our recommendation that practitioners using ketamine have haloperidol readily available.
There are three limitations to the study. First, our study was conducted only in one faculty hospital; thus, we are not able to generalise our findings to all of Egypt. Secondly, only children undergoing minor surgery were recruited. Thirdly, risk factors that could possible modify our results, such as the temperaments of the children, were not assessed.
Conclusion
The administration of haloperidol greatly decreased the incidence of postoperative ED in a sample of children undergoing minor surgery. This work provides great hope of decreasing and even preventing delirium in hospitalised, nonsurgical patients. Limited resources and lack of well qualified nursing staff magnify the benefit of pharmacological approaches to delirium prevention in developing countries. It is our recommendation that haloperidol should be available for those children who are delirious from the use of ketamine.
References
- 1.Gilger MA, Spearman RS, Dietrich CL, Spearman G, Wilsey MJ, Zayat MN. Safety and effectiveness of ketamine as a sedative agent for pediatric GI endoscopy. Gastrointest Endosc. 2004;59:659–63. doi: 10.1016/s0016-5107(04)00180-4. [DOI] [PubMed] [Google Scholar]
- 2.Kirberg A, Sagredo R, Montalva G, Flores E. Ketamine for pediatric endoscopic procedures and as a sedation complement for adult patients. Gastrointest Endosc. 2005;61:501–2. doi: 10.1016/s0016-5107(04)02724-5. [DOI] [PubMed] [Google Scholar]
- 3.Durieux ME. Inhibition by ketamine of muscarinic acetylcholine receptor function. Anaesth Analg. 1995;81:57–62. doi: 10.1097/00000539-199507000-00012. [DOI] [PubMed] [Google Scholar]
- 4.Bishop RA, Litch JA, Stanton JM. Ketamine anesthesia at high altitude. High Alt Med Biol. 2000;1:111–14. doi: 10.1089/15270290050074251. [DOI] [PubMed] [Google Scholar]
- 5.Wells L, Rasch D. Emergence ‘delirium’ after sevoflurane anesthesia: A paranoid delusion? Anesth Analg. 1999;88:1308–10. doi: 10.1097/00000539-199906000-00020. [DOI] [PubMed] [Google Scholar]
- 6.Uezono S, Goto T, Terui K, Ichinose F, Ishguro Y, Nakata Y, et al. Emergence agitation after sevoflurane versus propofol in pediatric patients. Anesth Analg. 2000;91:563–6. doi: 10.1097/00000539-200009000-00012. [DOI] [PubMed] [Google Scholar]
- 7.White PF, Way WL, Trevor AJ. Ketamine – its pharmacology and therapeutic uses. Anesthesiology. 1982;56:119–36. doi: 10.1097/00000542-198202000-00007. [DOI] [PubMed] [Google Scholar]
- 8.Cartwright PD, Pingel SM. Midazolam and diazepam in ketamine anaesthesia. Anaesthesia. 1984;39:439–42. doi: 10.1111/j.1365-2044.1984.tb07312.x. [DOI] [PubMed] [Google Scholar]
- 9.Wathen JE, Roback MG, Mackenzie T, Bothner JP. Does midazolam alter the clinical effects of intravenous ketamine sedation in children? A double-blind, randomized, controlled, emergency department trial. Ann Emerg Med. 2000;36:579–88. doi: 10.1067/mem.2000.111131. [DOI] [PubMed] [Google Scholar]
- 10.Sherwin TS, Green SM, Khan A, Chapman DS, Dannenberg B. Does adjunctive midazolam reduce recovery agitation after ketamine sedation for pediatric procedures? A randomized, double blind, placebo-controlled trial. Ann Emerg Med. 2000;35:229–38. doi: 10.1016/s0196-0644(00)70073-4. [DOI] [PubMed] [Google Scholar]
- 11.Campbell N, Boustani MA, Ayub A, Fox GC, Munger SL, Ott C, et al. Pharmacological management of delirium in hospitalized adults—A systematic evidence review. J Gen Intern Med. 2009;24:848–53. doi: 10.1007/s11606-009-0996-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Schrader SL, Wellik KE, Demaerschalk BM, Caselli RJ, Woodruff BK, Wingerchuk DM. Adjunctive haloperidol prophylaxis reduces postoperative delirium severity and duration in at-risk elderly patients. Neurologist. 2008;14:134–7. doi: 10.1097/NRL.0b013e318166b88c. [DOI] [PubMed] [Google Scholar]
- 13.Atlas GM, Milles M. Haloperidol for the Treatment of Ketamine-Induced Emergence Delirium. J Anaesthiol Clin Pharmacol. 2007;23:65–7. [Google Scholar]
- 14.Hatherill S, Flisher AJ, Nassen R. Delirium among children and adolescents in an urban sub-Saharan African setting. J Psychosom Res. 2010;69:187–92. doi: 10.1016/j.jpsychores.2010.01.011. [DOI] [PubMed] [Google Scholar]
- 15.Schieveld JNM, Leentjens AFG. Delirium in severely ill young children in the pediatric intensive care unit. J Am Acad Child Adolesc Psychiatry. 2005;44:392–4. doi: 10.1097/01.chi.0000153231.64968.1a. [DOI] [PubMed] [Google Scholar]
- 16.Brown RL, Henke A, Greenhalgh DG, Warden GD. The use of haloperidol in the agitated, critically ill pediatric patient with burns. J Burn Care Rehabil. 1996;17:34–8. doi: 10.1097/00004630-199601000-00009. [DOI] [PubMed] [Google Scholar]
- 17.Harrison AM, Lugo RA, Lee WE, Appachi E, Bourdakos D, Davis SJ, et al. The use of haloperidol in agitated, critically ill children. Clin Pediatr. 2002;41:51–4. doi: 10.1177/000992280204100111. [DOI] [PubMed] [Google Scholar]
- 18.Tesar GE, Murray GB, Cassem NH. Use of high-dose intravenous haloperidol in the treatment of agitated cardiac patients. J Clin Psychopharmacol. 1985;5:344–7. [PubMed] [Google Scholar]
- 19.Adams F. Emergency intravenous sedation of the delirious, medically ill patient. J Clin Psychiatry. 1988;49:22–6. [PubMed] [Google Scholar]
- 20.Schieveld JN, Leroy PL, van Os J, Nicolai J, Vos GD, Leentjens AF. Pediatric delirium in critical illness: Phenomenology, clinical correlates and treatment response in 40 cases in the pediatric intensive care unit. Intensive Care Med. 2007;33:1033–40. doi: 10.1007/s00134-007-0637-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hassaballa HA, Balk RA. Torsade de pointes associated with the administration of intravenous haloperidol. Amer J Therap. 2003;10:58–60. doi: 10.1097/00045391-200301000-00013. [DOI] [PubMed] [Google Scholar]
- 22.Burke C, Fulda GJ, Castellano J. Neuroloeptic malignant syndrome in a trauma patient. J Trauma. 1995;39:796–8. doi: 10.1097/00005373-199510000-00038. [DOI] [PubMed] [Google Scholar]
- 23.Kudo S, Ishizaki T. Pharmacokinetics of haloperidol. Clin Pharmacokinet. 1999;37:425–38. doi: 10.2165/00003088-199937060-00001. [DOI] [PubMed] [Google Scholar]
- 24.Clements JA, Nimmo WS, Grant IS. Bioavailability, pharmacokinetics, and analgesic activity of ketamine in humans. J Pharm Sci. 1982;71:539–42. doi: 10.1002/jps.2600710516. [DOI] [PubMed] [Google Scholar]
- 25.Tollefson GD, Beasley CM, Ramura RN, Tran PV, Potvin JH. Blind, controlled, long-term study of the comparative incidence of treatment-emergent tardive dyskinesia with olanzapine or haloperidol. Am J Psy. 1997;154:1248–54. doi: 10.1176/ajp.154.9.1248. [DOI] [PubMed] [Google Scholar]
- 26.Wewers ME, Lowe NK. A critical review of visual analogue scales in the measurement of clinical phenomena. Res Nurs Health. 1990;13:227–36. doi: 10.1002/nur.4770130405. [DOI] [PubMed] [Google Scholar]
- 27.Cole JW, Murray DJ, McAllister D, Hirshberg GE. Emergence behavior in children: Defining the incidence of excitement and agitation following anaesthesia. Pediatr Anesth. 2002;12:442–7. doi: 10.1046/j.1460-9592.2002.00868.x. [DOI] [PubMed] [Google Scholar]
- 28.Kalisvaart KJ, de Jonghe JF, Bogaards MJ, Vreeswijk R, Egberts TC, Burger BJ, et al. Haloperidol prophylaxis for elderly hip surgery patients at risk for delirium: A randomized placebo-controlled study. J Am Geriatr Soc. 2005;53:1658–66. doi: 10.1111/j.1532-5415.2005.53503.x. [DOI] [PubMed] [Google Scholar]
- 29.Milbrandt EB, Kersten A, Kong L, Weissfeld LA, Clermont G, Fink MP, et al. Haloperidol use is associated with lower hospital mortality in mechanically ventilated patients. Crit Care Med. 2005;33:226–9. doi: 10.1097/01.ccm.0000150743.16005.9a. [DOI] [PubMed] [Google Scholar]
- 30.Motamed F, Aminpour Y, Hashemian H, Soltani AE, Najafi M, Farahmand F. Midazolam-ketamine combination for moderate sedation in upper GI endoscopy. J Pediatr Gastroenterol Nutr. 2012;54:422–6. doi: 10.1097/MPG.0b013e3182323c75. [DOI] [PubMed] [Google Scholar]
- 31.White PF. Comparative evaluation of intravenous agents for rapid sequence induction: Thiopental, ketamine, and midazolam. Anesthesiology. 1982;57:279–84. doi: 10.1097/00000542-198210000-00005. [DOI] [PubMed] [Google Scholar]
- 32.White PF, Vasconez LO, Mathes SA, Way WL, Wender LA. Comparison of midazolam and diazepam for sedation during plastic surgery. J Plast Reconstr Surg. 1988;81:703–12. doi: 10.1097/00006534-198805000-00009. [DOI] [PubMed] [Google Scholar]
- 33.Monk TG, Rater MJ, White PF. Comparison of alfentanil and ketamine infusions in combination with midazolam for outpatient lithotripsy. Anesthesiology. 1991;74:1023–8. doi: 10.1097/00000542-199106000-00009. [DOI] [PubMed] [Google Scholar]
- 34.Riker RR, Fraser GL, Cox PM. Continuous infusion of haloperidol controls agitation in critically ill patients. Crit Care Med. 1994;22:89–97. doi: 10.1097/00003246-199403000-00013. [DOI] [PubMed] [Google Scholar]
- 35.Seneff MG, Mathews RA. Use of haloperidol infusions to control delirium in critically ill adults. Ann Pharmacother. 1995;29:690–3. doi: 10.1177/106002809502907-806. [DOI] [PubMed] [Google Scholar]