Abstract
The safe handling of microorganisms in the teaching laboratory is a top priority. However, in the absence of a standard set of biosafety guidelines tailored to the teaching laboratory, individual educators and institutions have been left to develop their own plans. This has resulted in a lack of consistency, and differing levels of biosafety practices across institutions. Influenced by the lack of clear guidelines and a recent outbreak of Salmonella infections that was traced back to teaching laboratory exposures, the Education Board of the American Society for Microbiology charged a task force to develop a uniform set of biosafety guidelines for working with microorganisms in the teaching laboratory. These guidelines represent best practices for safely handling microbes, based on the safety requirements found in the Centers for Disease Control and Prevention’s (CDC’s) Biosafety in Microbiological and Biomedical Laboratories (BMBL). Guidelines for safely handling microbes at both biosafety level 1 (BSL1) and biosafety level 2 (BSL2) were developed. The guidelines are brief by design for ease of use and are accompanied by an extensive appendix containing explanatory notes, sample documents, and additional resources. These guidelines provide educators with a clear and consistent way to safely work with microorganisms in the teaching laboratory.
INTRODUCTION
Educators recognize the importance of biosafety when handling microorganisms and strive to minimize risk to students and the community, but a uniform, easy-to-follow set of biosafety guidelines for educators when handling microorganisms in the teaching laboratory does not exist. This has led to a lack of consensus among educators as to which are the best practices for achieving biosafety in the laboratory and a variety of biosafety practices across different institutions. Instructors may rely on their own history of biosafety training, techniques passed down from previous instructors at their institution, or safety presentations at conferences to shape their biosafety practices (4). Those educators who turn to federal guidance documents like Biosafety in Microbiological and Biomedical Laboratories (BMBL) can be quickly overwhelmed with the information presented due to its exhaustive scope and lack of clear direction for the educational laboratory setting. Furthermore, some educators assigned to teach microbiology may not have formal microbiology training. Given the wide bio-safety training background of educators, concise and clear biosafety guidelines are essential to assist educators and protect students when working with live microorganisms.
The low reported incidence of infections associated with microbiology teaching laboratories suggest that these laboratories are relatively safe (3). However, the importance of biosafety in the laboratory is highlighted by recent multi-state infections by Salmonella Typhimurium associated with clinical and teaching laboratories. Between August 2010 and June 2011 the Centers for Disease Control and Prevention (CDC) linked Salmonella Typhimurium infections in 109 individuals ranging in age from one to 91 years old to a strain used in clinical and teaching laboratories. The infections included twelve hospitalizations and one death (1). The majority of infected individuals had been in a clinical or microbiology teaching laboratory in the week prior to infection or were household contacts of people who had been in such a laboratory. This outbreak is an indication that exposures are likely more common than reported. Such exposures are not likely to have resulted in illness as the organisms used most often in teaching laboratories fall into the lowest risk group, Risk Group 1, and thus would not be reported. This CDC report prompted the American Society for Microbiology (ASM) to develop a Task Committee on Laboratory Biosafety charged with researching microbiology safety standards used in clinical and research laboratories and determining how they should best be implemented in the undergraduate microbiology teaching laboratory. The goal of the committee was to develop a clear, concise set of biosafety guidelines for instructors using microorganisms in both undergraduate and K–12 laboratories. The primary users of these guidelines are expected to be educators teaching introductory microbiology and biology courses using organisms that fall into Risk Group 1 or Risk Group 2 and procedures that would require biosafety level 1 (BSL1) or biosafety level 2 (BSL2) containment. Biosafety levels are determined by considering multiple factors such as the risk group of the organisms, the laboratory procedures, and the necessary safety equipment. Streak plating Staphylococcus epidermidis is an example of a procedure requiring BSL1 while pipetting Staphylococcus aureus is a procedure requiring BSL2. Educators using higher risk group organisms must be highly trained in biosafety principles that go beyond those considered by the committee.
Chaired by Elizabeth Emmert (Salisbury University, MD), and including Jeffrey Byrd (St. Mary’s College of Maryland, MD), Ruth Gyure (Western Connecticut State University, CT), Diane Hartman (Baylor University, TX), and Amy White (Virginia Western Community College, VA), the ASM Task Committee of Laboratory Biosafety drafted two sets of guidelines—one for BSL1 (Table 1) and a second set for BSL2 (Table 2). The guidelines are divided into six sections: personal protection requirements, laboratory physical space requirements, stock culture requirements, standard laboratory practices, training practices, and document practices. The Task Committee also developed an extensive appendix to enhance and expand upon the guidelines (Appendix 1). Some topics in the appendix include explanatory notes with practical suggestions for implementing the guidelines, how to safely handle unknown microbes cultured from the environment, and detailed information on biosafety cabinets, disinfecting spills, and validating autoclaves. Additionally, the appendix contains frequently used microbes and their common BSL for use, sample forms, and resources for more information.
TABLE 1.
Biosafety level 1 (BSL1) guidelines for teaching laboratories.
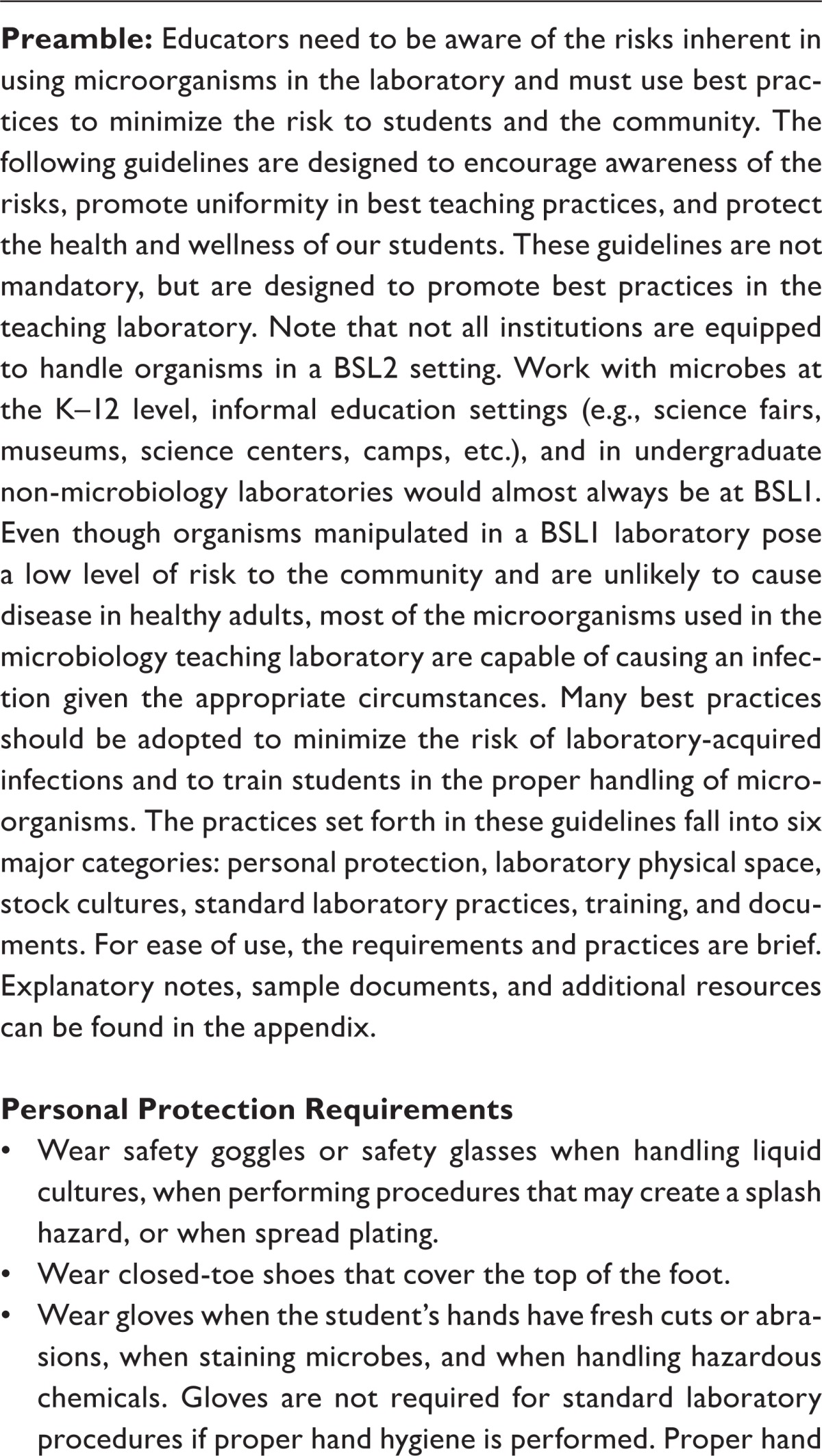
| Preamble: Educators need to be aware of the risks inherent in using microorganisms in the laboratory and must use best practices to minimize the risk to students and the community. The following guidelines are designed to encourage awareness of the risks, promote uniformity in best teaching practices, and protect the health and wellness of our students. These guidelines are not mandatory, but are designed to promote best practices in the teaching laboratory. Note that not all institutions are equipped to handle organisms in a BSL2 setting. Work with microbes at the K–12 level, informal education settings (e.g., science fairs, museums, science centers, camps, etc.), and in undergraduate non-microbiology laboratories would almost always be at BSL1. Even though organisms manipulated in a BSL1 laboratory pose a low level of risk to the community and are unlikely to cause disease in healthy adults, most of the microorganisms used in the microbiology teaching laboratory are capable of causing an infection given the appropriate circumstances. Many best practices should be adopted to minimize the risk of laboratory-acquired infections and to train students in the proper handling of micro-organisms. The practices set forth in these guidelines fall into six major categories: personal protection, laboratory physical space, stock cultures, standard laboratory practices, training, and documents. For ease of use, the requirements and practices are brief. Explanatory notes, sample documents, and additional resources can be found in the appendix. |
Personal Protection Requirements
|
Laboratory Physical Space Requirements
|
Stock Culture Requirements
|
Standard Laboratory Practices
|
Training Practices
|
Document Practices
|
TABLE 2.
Biosafety level 2 (BSL2) guidelines for teaching laboratories.
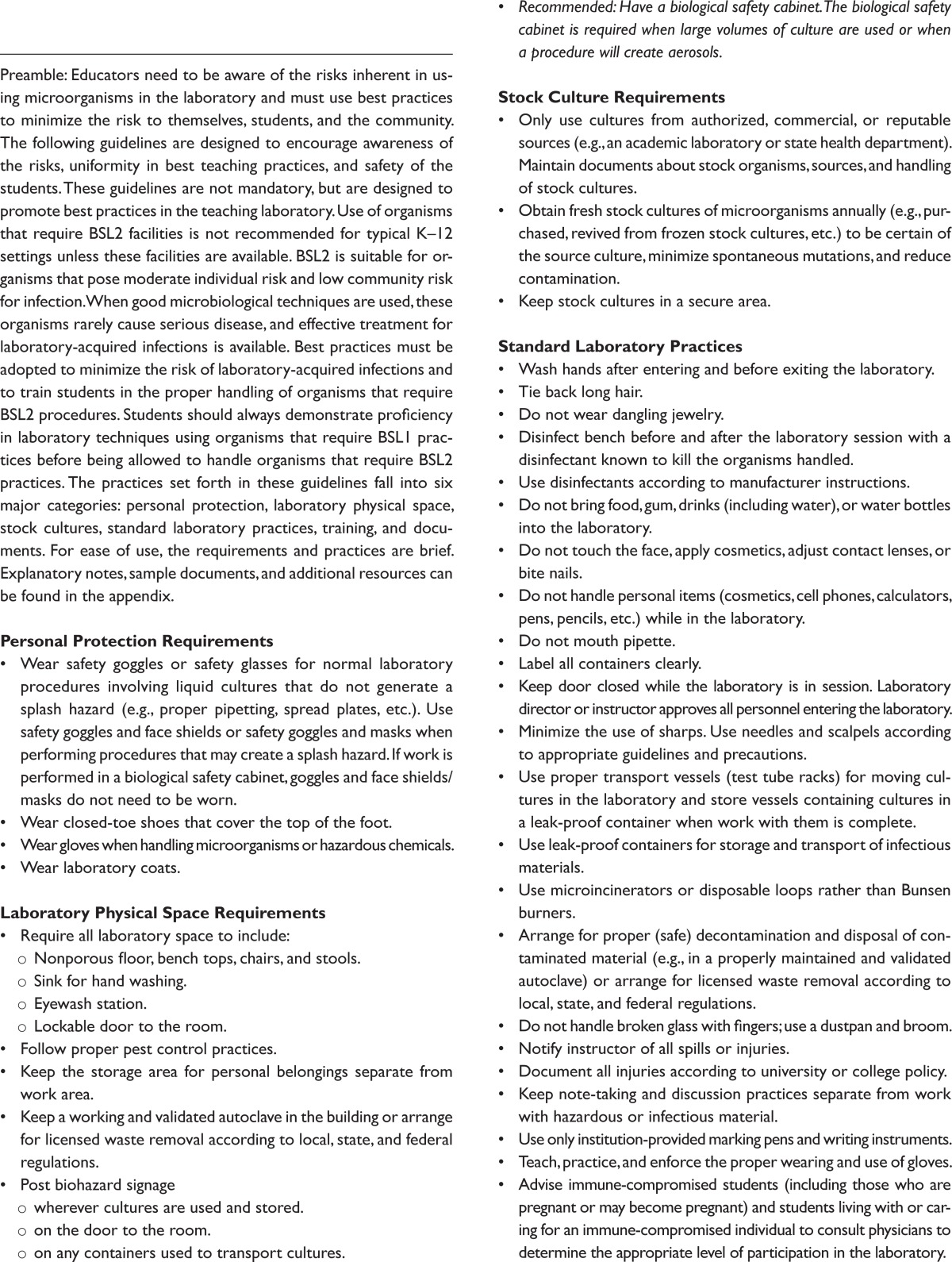
| Preamble: Educators need to be aware of the risks inherent in using microorganisms in the laboratory and must use best practices to minimize the risk to themselves, students, and the community. The following guidelines are designed to encourage awareness of the risks, uniformity in best teaching practices, and safety of the students. These guidelines are not mandatory, but are designed to promote best practices in the teaching laboratory. Use of organisms that require BSL2 facilities is not recommended for typical K–12 settings unless these facilities are available. BSL2 is suitable for organisms that pose moderate individual risk and low community risk for infection. When good microbiological techniques are used, these organisms rarely cause serious disease, and effective treatment for laboratory-acquired infections is available. Best practices must be adopted to minimize the risk of laboratory-acquired infections and to train students in the proper handling of organisms that require BSL2 procedures. Students should always demonstrate proficiency in laboratory techniques using organisms that require BSL1 practices before being allowed to handle organisms that require BSL2 practices. The practices set forth in these guidelines fall into six major categories: personal protection, laboratory physical space, stock cultures, standard laboratory practices, training, and documents. For ease of use, the requirements and practices are brief. Explanatory notes, sample documents, and additional resources can be found in the appendix. |
Personal Protection Requirements
|
Laboratory Physical Space Requirements
|
Stock Culture Requirements
|
Standard Laboratory Practices
|
Training Practices
|
Document Practices
|
The initial guidelines were reviewed in December 2011 by a small group of individuals including biological safety professionals, CDC personnel, and microbiology educators. Based on their comments, the guidelines were revised and sent out for further review in February 2012 through a survey of microbiology educators targeted at the ASM educator community. Approximately 1,400 individuals received a request to complete the survey and 400 individuals submitted survey results, representing a 30% response rate. This high response rate for the biosafety survey indicates the importance of this topic among educators. (An ASM educator community survey on curriculum guidelines in 2011 yielded a 12% response rate.) Twenty-eight percent of biosafety survey respondents teach at community colleges, 41% teach at primarily undergraduate institutions, 10% teach at comprehensive universities, 20% teach at doctoral-degree granting institutions, and 1% are not employed by a higher-education institution. Based on the survey feedback, the guidelines were revised again and presented in draft form to all attendees at the ASM Conference on Microbiology Education (ASMCUE) in June 2012. Twenty-six percent of 2012 ASMCUE attendees teach at community colleges, 28% teach at primarily undergraduate institutions, 10% teach at comprehensive universities, 33% teach at doctoral-degree granting institutions, and 3% are not employed by a higher-education institution. Attendees had the opportunity to comment on the guidelines and appendix during breakout sessions led by members of the Task Committee. The guidelines were also presented at the Division W business meeting during the ASM General Meeting in June 2012. Based on the comments received at these meetings, the guidelines were revised a third time. A final call for input on the guidelines went out to the ASM membership in the fall of 2012.
The challenge with developing guidelines for biosafety in the teaching laboratory is balancing the need for safety with the practical implementation and cost of the guidelines. Throughout the process, the Task Committee relied on the BMBL as its standard for biosafety in the laboratory (2). Indeed the guidelines presented here are derived from the BMBL and written as they apply to the teaching laboratory. The most contentious issue was whether gloves are necessary when handling Risk Group 1 microorganisms at BSL1. The BMBL is ambiguous on this issue since it states, “Biosafety Level 1 practices, safety equipment, and facility design and construction are appropriate for undergraduate and secondary educational training and teaching laboratories, and for other laboratories in which work is done with defined and characterized strains of viable microorganisms not known to consistently cause disease in healthy adult humans . . . BSL-1 represents a basic level of containment that relies on standard microbiological practices with no special primary or secondary barriers recommended, other than a sink for hand washing.” But under Personal Protective Equipment for BSL1 it states “Gloves must be worn to protect hands from exposure to hazardous materials” (2). Are microbes commonly handled at BSL1 considered to be hazardous material? Obviously this depends on multiple factors including how the microbe is being manipulated, the health status of the worker, etc. After much thought and discussion, the decision of the Task Committee was that the key issue is proper hand hygiene and if proper hand hygiene is performed, gloves are not necessary for handling microbes at BSL1. When gloves are required (i.e. at BSL2) the students must be trained in proper glove use as improper glove use can lead to contamination of the individual or the environment. All educators will likely not agree with every aspect of the guidelines, but we believe these represent best practices for biosafety and they should not be overly burdensome in either practicality or cost. One concern expressed during the review process is that overly burdensome or costly guidelines would encourage some institutions to do away with wet microbiology laboratories. That was certainly not our intent. In fact we believe that educating students in the proper safety protocols when handling microorganisms is essential and can best be accomplished through hands-on training.
The comments received from the survey of the ASM educator community in February 2012 highlighted the most controversial issues for the BSL1 biosafety guidelines. Many educators thought that safety glasses or safety goggles were not necessary at BSL1 because of the low risk of splashes, small culture volumes used, and low infection risk at BSL1. Others objected to using institution-provided writing instruments because they believed it was unnecessary or too expensive to implement. Many surveyed did not understand why students should be provided with a list of all cultures (and their sources) used in the course. They were also concerned that this would spoil the unknown laboratory experience if the students were aware of possible unknown microorganisms. Finally, many objected to not being able to subculture microbes isolated from the environment because they viewed this as the most exciting exercise for young microbiologists and they did not want to deny students the joy and wonder of this discovery-based laboratory. Our committee reviewed and discussed all the survey comments. Safety glasses or goggles were considered to be an inexpensive, easily implemented practice. Using only institution-required writing instruments is now recommended practice by the CDC based on the Salmonella Typhimurium infections (1), as the CDC epidemiologists believe that items handled in the laboratory (pens, notebooks, cell phones, etc.) have the possibility of becoming contaminated. As for providing students with a list of cultures, immunocompromised students need to be supplied with a list of cultures and their sources that they can provide to their personal physician. Due to HIPPA privacy reasons, students are not required to disclose their health status, so having immunocompromised students request a list of cultures could be seen as an invasion of privacy. It is better to make the list available to all and those that need it can use it. Our statement about isolating unknown microbes from the environment focuses on subculturing. Unknown environmental microbes can be isolated and plated in a BSL1 laboratory, but then the plates must be sealed and only observed. This exercise would still demonstrate the ubiquity, diversity, and abundance of environmental microbes. Any additional culturing of isolated microorganisms should be done in a BSL2 laboratory since the pathogenicity of the isolate is unknown. For additional information, a section of the appendix is devoted to isolation of unknown microbes from the environment.
A brief set of guidelines may be viewed as an oversimplification of biosafety. One response to these guidelines might be to only use Risk Group 1 microbes commonly handled at BSL1 and implement the BSL1 guidelines. An educator who does this might conclude their biosafety work is complete. Instead, a thorough risk assessment should be the key first step in any biosafety work. The goal of risk assessment is to determine the hazards associated with a procedure and to implement safety precautions to minimize the risk. Risk assessment involves examining the organisms used, the procedures performed with the organism, and the risks inherent in the laboratory activity. Educators need to examine all aspects of the laboratory (procedures, facilities, users, etc.) and not just the microbes used to conduct a thorough risk assessment. See the Risk Assessment and Biosafety Levels section of the appendix for additional information and resources. Lastly, educators need to be aware of any local and state regulations and requirements that may apply at their institution.
With these biosafety guidelines for teaching laboratories we have compiled a list of the best practices for handling microorganisms in the teaching laboratory. Since each laboratory is unique, risk assessments will differ between institutions, but many core biosafety practices will remain the same. This clear, concise set of guidelines should reduce confusion and anxiety among educators and direct them to safe standards in the laboratory. Although some educators may see some guidelines as burdensome or excessive, we believe these guidelines will minimize the possibility of laboratory-acquired infections among students and their close contacts. Ideally, these guidelines should apply to all educators handling live microbes including undergraduate introductory biology teachers, molecular biologists and geneticists, K–12 educators, science fair participants, and science camp counselors. A future challenge is making all educators who handle microbes aware of these guidelines and the importance of implementing them. Distance education and home schooling programs that require at home microbiology laboratory activities are a concern. Educators overseeing these programs and suppliers of the laboratory materials need to be aware of these guidelines. Since these activities are conducted in an unsupervised environment, with minimal facilities (kitchen countertop) they must be very low risk level activities (i.e. only Risk Group 1 organisms at BSL1). Presentations at conferences, informal talks with colleagues, and working with the appropriate scientific societies (SABER, The American Society for Cell Biology, etc.) will promote the dissemination of these guidelines. Additionally the production of short videos or slide shows depicting proper (and improper) biosafety practices in the laboratory would be immensely useful for instructors and students to visualize safe procedures in the laboratory. As these visual teaching tools are produced (by ASM members or others), they could be added to the appendix since it will be maintained online. As educators, our goal is to introduce students to the wonder and intricacy of the microbial world. We are also obligated to minimize the risks of harmful exposures in the laboratory. While implementation of these biosafety guidelines will not eliminate the risks of harmful exposures from microbes, it will significantly reduce these risks for our students while they learn how to work with and appreciate these amazing organisms.
SUPPLEMENTAL MATERIALS
Appendix 1: Accompanying materials for the guidelines for biosafety in teaching laboratories
Acknowledgments
The author would like to thank the entire Task Committee for their hard work and input. Their suggestions and contributions at each stage of the process made her job easier and improved the finalized guidelines. Thanks also to Amy Chang for her helpful direction and the support staff of ASM for their willing assistance with formatting the guidelines and managing the administrative tasks. Lastly, thanks to Neil Baker for his thoughtful insights on critical issues and assistance throughout the process. The author declares that there are no conflicts of interest.
Contributor Information
Collaborators: the ASM Task Committee on Laboratory Biosafety
REFERENCES
- 1.Centers for Disease Control and Prevention . Investigation update: human SalmonellaTyphimurium infections associated with exposure to clinical and teaching microbiology laboratories. Centers for Disease Control and Prevention; Atlanta, GA: 2012. http://www.cdc.gov/salmonella/typhimurium-laboratory/011712/. [Google Scholar]
- 2.Centers for Disease Control and Prevention . Biosafety in microbiological and biomedical laboratories. 5th ed. U.S. Department of Health and Human Services; Washington, D.C: 2009. Section IV—Laboratory Biosafety Level Criteria; pp. 30–59. http://www.cdc.gov/biosafety/publications/bmbl5/. [Google Scholar]
- 3.Harding L, Byers KB. Epidemiology of laboratory-associated infections. In: Fleming DO, Hunt DL, editors. Biological safety: principles and practices. 4th ed. ASM Press; Washington, DC: 2006. pp. 53–77. [Google Scholar]
- 4.Woolverton CJ. Teaching Laboratories. In: Gentry-Weeks C, Ellis R, Wooley D, editors. Biological safety: principles and practices. 5th ed. ASM Press; Washington, DC: in press. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix 1: Accompanying materials for the guidelines for biosafety in teaching laboratories