Abstract
This practice-based, randomized clinical trial evaluated and compared the success of direct pulp capping in permanent teeth with MTA (mineral trioxide aggregate) or CaOH (calcium hydroxide). Thirty-five practices in Northwest PRECEDENT were randomized to perform direct pulp caps with either CaOH (16 practices) or MTA (19 practices). Three hundred seventy-six individuals received a direct pulp cap with CaOH (n = 181) or MTA (n = 195). They were followed for up to 2 yrs at regular recall appointments, or as dictated by tooth symptoms. The primary outcomes were the need for extraction or root canal therapy. Teeth were also evaluated for pulp vitality, and radiographs were taken at the dentist’s discretion. The probability of failure at 24 mos was 31.5% for CaOH vs. 19.7% for MTA (permutation log-rank test, p = .046). This large randomized clinical trial provided confirmatory evidence for a superior performance with MTA as a direct pulp-capping agent as compared with CaOH when evaluated in a practice-based research network for up to 2 yrs (ClinicalTrials.gov NCT00812887).
Keywords: clinical research, dental pulp, dental pulp exposure, pulp-capping agents, sodium hypochlorite, dental cavity liner
Introduction
A direct pulp cap is a procedure in which a medicament is placed directly over the exposed dental pulp, with the specific aim of maintaining pulp vitality and health (Camp and Fuks, 2006; Hilton, 2009; Mente et al., 2010). Advantages of a successful direct pulp cap are numerous, including the avoidance of more extensive treatment, such as root canal treatment or extraction. Calcium hydroxide (CaOH) has been considered the “gold standard” of direct pulp-capping materials for several decades (Baume and Holz, 1981; Camp and Fuks, 2006; Hilton, 2009). While a new cement (mineral trioxide aggregate, MTA) has become a popular alternative, a recent Cochrane Review found that evidence is lacking as to the most effective pulp-capping material (Miyashita et al., 2007).
Calcium hydroxide possesses antibacterial properties which can minimize or eliminate bacterial penetration and subsequent irritation of pulpal tissue (Barthel et al., 1997). Historically, the repair mechanism has not been fully understood. Recent research has demonstrated that the repair mechanism may be due in part to the release of bioactive molecules from dentin matrix, including Bone-Morphogenetic Protein (BMP) and Transforming Growth Factor-Beta One (TBF-β1). Both have demonstrated the ability to stimulate pulp repair and dentin remineralization (Barthel et al., 1997; Graham et al., 2006; Zhang et al., 2007). The disadvantages of calcium hydroxide are that it has no inherent adhesive properties and provides a poor seal, and the self-cure formulations are soluble and subject to dissolution over time (Hilton, 2009).
MTA is comprised of calcium oxide in the form of tricalcium silicate, dicalcium silicate, tricalcium aluminate, and bismuth oxide for radiopacity (Camilleri, 2008). Calcium hydroxide is the main reaction product of MTA and water (Camilleri, 2008). The biocompatibility of MTA is likely due to the formation of CaOH, which stimulates pulpal repair. Unlike CaOH, MTA has a significant advantage in that it provides some seal to tooth structure (Luketic et al., 2008). Disadvantages of MTA are that it is highly soluble and has a prolonged setting time of approximately 2 hrs and 45 min (Fridland and Rosado, 2005; Islam et al., 2006).
Three human studies have shown no significant differences between MTA and CaOH for superficial and deep inflammatory cell response, the presence of a dentin bridge, and pulp vitality (Colceriu et al., 2005; Iwamoto et al., 2006; Accorinte et al., 2008). Four other human studies found that MTA treatment was more effective for pulp capping (Aeinehchi et al., 2003; Chacko and Kurikose, 2006; Min et al., 2008; Nair et al., 2008). However, these studies tended to exhibit shortcomings such as low subject numbers, as well as differing methodologies. The histological studies demonstrated less pulpal inflammation and a superior hard-tissue barrier with MTA.
The specific aim of this randomized clinical trial was to evaluate and compare the success of direct pulp capping in permanent teeth with MTA vs. CaOH. This study was executed in Northwest PRECEDENT (NWP), a practice-based research network (DeRouen et al., 2010). The study was designed to be the largest randomized trial of adult direct pulp caps, and the first conducted by dentists in their own practices.
Study Population & Methods
Practitioner Participants
All eligible dentist-investigators of NWP were offered the opportunity to participate, provided the practitioner agreed to be randomized by material. Each provider and ancillary personnel received training in utilization of the appropriate pulp-capping material to ensure uniformity among the providers.
Subject Participants
The study was reviewed and approved by the Oregon Health & Science University Institutional Review Board. All patients, ages 7 yrs or older, exhibiting pulp exposure (carious, traumatic, or mechanical) were eligible. During the course of treatment, if the dentist-investigator deemed that a direct pulp cap was the appropriate clinical procedure, he/she then performed the pulp cap using the assigned capping agent (MTA or CaOH). Pulp vitality was determined by the presence (vital) or absence (non-vital) of pulp bleeding from the exposure site. The tooth had to be part of the permanent dentition and could not have any radicular radiolucency. Additionally, there could be no history of spontaneous or lingering pain in response to temperature or biting. Only one pulp cap per patient was eligible. A radiograph was taken after the pulp-capping procedure if one within the preceding 6 mos was not available. Written informed consent was obtained after the appointment was complete. Patients had the right to decline enrollment and to opt out of the study at any time.
Interventions
After pulp exposure and vitality confirmation, the exposure and surrounding area were rinsed with water to remove debris. A cotton pellet moistened with 5.25% sodium hypochlorite was placed over the exposure for 1 to 2 min to control pulp hemorrhage and to disinfect the area. The cotton pellet was removed, and if bleeding continued, a new cotton pellet moistened in the sodium hypochlorite solution was re-applied for several min. This was repeated until bleeding was controlled or the practitioner decided that pulp capping was not appropriate. The pulp-capping agent (MTA; Pro Root, Tulsa Dental, Tulsa, OK, USA; or CaOH, Life, Kerr, Orange, CA, USA) was then applied by the dentist. A resin-modified glass-ionomer liner (Vitrebond, 3M/ESPE) was placed over the pulp-capping agent and extended peripherally beyond it. The materials were used according to the manufacturer’s clinical directions. The teeth were restored as deemed appropriate by the dentist.
Recalls
Patients were contacted by the practice by telephone within 1 mo of the procedure and were subsequently seen every 6 mos up to 2 yrs, unless a problem developed that required earlier assessment. A telephone interview was attempted if the patient could not be seen at these intervals.
Outcomes Measures
Treated teeth were followed for up to 2 yrs or until the tooth required extraction or root canal therapy. At each appointment, the tooth was assessed for pulp vitality. A periapical radiograph was taken and assessed for signs of pulpal (resorption, calcification) or peri-radicular (radiolucency) pathology at the practitioner’s discretion. A periapical radiograph was requested at the final follow-up (2 yrs or study end).
Sample Size
Based on previous work on pulp capping with CaOH, showing annual failure rates ranging from 5% to 21% (Fitzgerald and Heys, 1991; Matsuo et al., 1996; Clement et al., 2000), a 20% pulp cap failure rate was assumed after 1 yr and a 30% failure rate after 2 yrs for CaOH. A sample size of 40 practices, each enrolling 16 patients and assuming 20% loss to follow-up, would provide 90% power to detect a 50% reduction in the 2-year failure rate, from 30% to 15%. This is based on a modified chi-square test with adjustment for correlation between patients in the same practice at a two-sided 0.05 significance level and a 0.05 intraclass correlation coefficient (Donner and Klar, 2000). Because of lower than expected enrollment, the initial sample size and 2 yrs of follow-up on all patients were not feasible. Based on an average follow-up of 1.5 yrs and 35 practices enrolling 375 individuals, the power was recalculated as 81% to detect a 60% reduction, and 63% to detect a 50% reduction in the pulp cap failure rate.
Randomization/Allocation Concealment/Blinding
Randomization was done by practice rather than by patient to avoid any delays in material selection. Practices were randomly pre-assigned in blocks of 2 or greater by the NWP Data Coordinating Center using the Sample function of R Version 2.15 (The R Foundation for Statistical Computing, 2012). Randomization was stratified on practice type, usual pulp cap material, number of pulp caps performed per month, practice location, and years in practice (see Table 1). It was not feasible to blind the practitioners to the materials, because their handling characteristics are dissimilar.
Table 1.
Descriptive Characteristics for Dentists (n = 35) and Subjects (n = 358)
| All (n = 35) | CaOH (n = 16) | MTA (n = 19) | |
|---|---|---|---|
| Dentist Characteristics | % (n) | % (n) | % (n) |
| Yrs in practice | |||
| ≤ 10 | 31.4% (11) | 43.8% (7) | 21.1% (4) |
| > 10 to 25 | 28.6% (10) | 37.5% (6) | 21.1% (4) |
| > 25 | 40.0% (14) | 18.8% (3) | 57.9% (11) |
| Practice location | |||
| Urban | 14.3% (5) | 12.5% (2) | 15.8% (3) |
| Suburban | 48.6% (17) | 50.0% (8) | 47.4% (9) |
| Rural | 37.1% (13) | 37.5% (6) | 36.8% (7) |
| Practice type | |||
| Private practice | 80.0% (28) | 81.3% (13) | 78.9% (15) |
| Community clinic | 20.0% (7) | 18.8% (3) | 21.1% (4) |
| Usual pulp-capping material | |||
| CaOH | 74.3% (26) | 75.0% (12) | 73.7% (14) |
| GI | 14.3% (5) | 12.5% (2) | 15.8% (3) |
| MTA | 11.4% (4) | 12.5% (2) | 10.5% (2) |
| Number of pulp caps per month | |||
| 1 to 5 | 71.4 % (25) | 81.3% (13) | 63.2% (12) |
| > 5 | 28.6% (10) | 18.7% (3) | 36.8% (7) |
| Number of patients per month | |||
| ≤ 200 | 54.3% (19) | 50.0% (8) | 57.9% (11) |
| > 200 | 45.7% (16) | 50.0% (8) | 42.1% (8) |
| All (n = 358) | CaOH (n = 175) | MTA (n = 183) | |
| Patient characteristics | Mean (SD) [Range] | Mean (SD) [Range] | Mean (SD) [Range] |
| Age, yrs | 37.9 (18.3) [8-90] | 36.5 (18.0) [8-89] | 39.4 (18.5) [8-90] |
| % (n) | % (n) | % (n) | |
| Gender (female) | 51.7% (185) | 52.0% (91) | 51.4% (94) |
| Race (white) | 82.1% (294) | 81.1% (142) | 83.1% (152) |
Statistical Methods
For the primary treatment comparison, a recommendation for tooth extraction or root canal therapy was counted as a failure, even if the patient had not yet completed treatment by the final follow-up. Secondary analysis also considered a pulp cap to have failed if the radiograph showed a radiolucency. The study protocol called for comparing failure rates based on an intent-to-treat analysis using a modified chi-square test with adjustment for correlation between patients in the same practice and assuming 2 yrs of follow-up on all patients (Donner and Klar, 2000). The statistical plan was modified because of lower than expected practice and subject numbers and varying follow-up times. A clustered permutation test with 10,000 random permutations based on the log rank test statistic was used for the primary treatment comparison to account for censoring and to ensure proper test size given the number of practices (Stedman et al., 2009). A confirmatory analysis, adjusted for patient, dentist, pulp exposure, and tooth characteristics, and incorporating follow-up time, was performed by a marginal Cox proportional hazards regression with robust standard error estimates that accounted for clustering by practice (Lin, 1994).
Results
Participant Flow/Recruitment
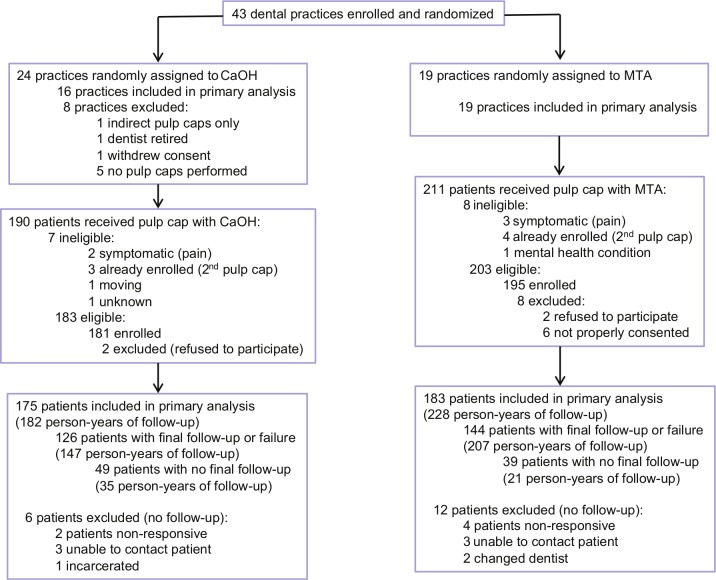
Forty-three practices were enrolled and randomized, of which 35 enrolled 376 patients between May 2009 and March 2011; 358 were included in the primary analysis (Fig. 1).
Figure 1.
Patient flow diagram.
Baseline Data
Table 1 describes study subjects and dentists, and Table 2 describes pulp exposure, pulp capping, and tooth characteristics used in the proportional hazards regression.
Table 2.
Pulp Exposure, Pulp Capping, and Tooth Characteristics Used for the Confirmatory Cox Proportional Hazards Model (n = 358)
| All (n=358) % (n) | CaOH (n=175) % (n) | MTA (n=183) % (n) | |
|---|---|---|---|
| Time to pulp cap | |||
| 0 to < 4.3 min | 50.3% (180) | 56.0% (98) | 44.8% (82) |
| ≥ 4.3 min | 49.7% (178) | 44.0% (77) | 55.2% (101) |
| Amount of bleeding | |||
| Light | 83.8% (300) | 86.3% (151) | 81.4% (149) |
| Moderate to heavy | 16.2% (58) | 13.7% (24) | 18.6% (34) |
| Size of pulp exposure, mm | |||
| ≤ 0.5 | 55.9% (200) | 50.9% (89) | 60.7% (111) |
| 1.0 | 28.8% (103) | 30.9% (54) | 26.8% (49) |
| ≥ 1.5 | 15.4% (55) | 18.3% (32) | 12.6% (23) |
| Location of pulp exposure | |||
| Pulpal floor | 49.2% (176) | 57.1% (100) | 41.5% (76) |
| Axial/proximal wall | 50.8% (182) | 42.9% (75) | 58.5% (107) |
| Rubber dam at time of exposure | |||
| No | 81.0% (290) | 84.6% (148) | 77.6% (142) |
| Yes | 19.0% (68) | 15.4% (27) | 22.4% (41) |
| Type of exposure | |||
| Carious | 88.8% (318) | 91.4% (160) | 86.3% (158) |
| Non-carious | 11.2% (11) | 8.6% (15) | 13.7% (25) |
| Clean exposure with hypochlorite | |||
| No | 12.3% (44) | 17.1% (30) | 7.7% (14) |
| Yes | 87.7% (314) | 82.9% (145) | 92.3% (169) |
| Restoration type at baseline | |||
| Permanent | 90.8% (325) | 85.1% (149) | 96.1% (176) |
| Temporary | 9.2% (33) | 14.9% (26) | 3.8% (7) |
| Tooth mobility | |||
| No | 83.2% (298) | 76.6% (134) | 89.6% (164) |
| Yes | 16.8% (60) | 23.4% (41) | 10.4% (19) |
| Type of existing restoration | |||
| None | 36.9% (132) | 34.3% (60) | 39.3% (72) |
| Amalgam | 35.2% (126) | 34.9% (61) | 35.5% (65) |
| Composite | 21.5% (77) | 24.0% (42) | 19.1% (35) |
| Other | 6.4% (23) | 6.9% (12) | 6.0% (11) |
Follow-up Time
Subjects were followed up for 2 yrs or at study end, May 2012. The median (range) CaOH group follow-up was 12.1 mos [(range, 0.2 to 30.9 mos)] and the median MTA group follow-up was 15.6 mos. [(range, 0.2 to 33.5 mos)]. Additional information on follow-up and those lost to follow-up can be found in the Appendix. No adverse events due to direct pulp-capping occurred.
Outcomes
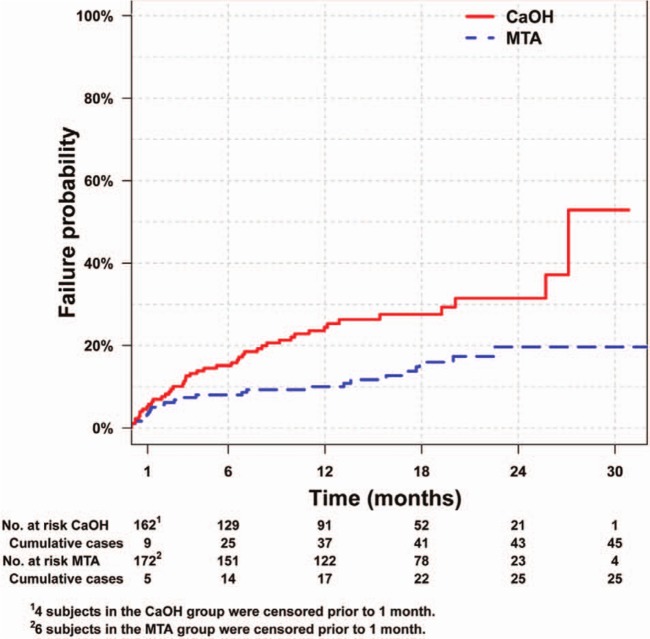
Forty-five CaOH pulp-capped teeth were recommended for either extraction (7) or root canal therapy (38); 25 MTA pulp-capped teeth were recommended for either extraction (6) or root canal therapy (19). The primary analysis indicated a higher failure rate in the CaOH group than in the MTA group (permutation log-rank test, p = .046). The Kaplan-Meier estimate for pulp cap failure by 24 mos for CaOH treatment was 31.5% vs. 19.7% for teeth pulp-capped with MTA (Fig. 2). The Kaplan-Meier estimates, which take into account censoring, are higher than the crude failure rates, 24.6% (43/175) for CaOH and 13.6% (25/183) for MTA. In the secondary analysis, 3 additional radiographic pulp-cap failures (radiolucency) were identified in the MTA group. Recalculating the probability of failure with these failures resulted in a failure rate of 31.5% for CaOH and 22.4% for MTA (p = .067). One practice randomized to the CaOH group experienced a high failure rate (14/25; 56%) and accounted for 31% (14/45) of all CaOH failures. Recalculating the probability of failure excluding this site resulted in a failure rate of 27.1% for CaOH and 19.7% for MTA (p = .090). A confirmatory Cox proportional hazards model, adjusted for patient, dentist, and pulp exposure, pulp capping, and tooth characteristics, demonstrated that the difference between CaOH and MTA was virtually unchanged. For example, based on all practices, the unadjusted hazard ratio for CaOH vs. MTA was 2.15 (95% CI, 1.19-3.87), and the adjusted hazard ratio was 2.35 (95% CI, 1.19-4.66).
Figure 2.
Kaplan-Meier failure curve by treatment group.
Discussion
There are limited published data comparing the effectiveness of CaOH and MTA in clinical situations involving a carious pulp exposure. Subsequent to the launch of this study, Mente et al. (2010) performed a case-control study involving carious pulp exposures with follow-up ranging from 12 to 80 mos (median, 27 mos). There were several differences in this study compared with the current results: It took place in an academic setting, there were 122 pulp caps in 108 patients, 72% of the pulp caps were accomplished by undergraduate dental students, there was no random treatment assignment, and the study was underpowered. Nonetheless, the results were similar to those in the present study, in that MTA showed a 22% failure rate compared with a 40% failure rate for CaOH (p = .05). Based on the results of the present study, and on those of others in humans and animals, there is evidence that MTA is more effective than CaOH for direct pulp caps. Considering the similarities in the reaction products of the 2 materials, it would seem that the likely explanation for this is the superior sealing ability of MTA.
This study has some significant strengths. First, it is the largest controlled clinical trial to date comparing direct pulp-capping success (Aguilar and Linsuwanont, 2011). It was conducted in private and public health practices, primarily on carious pulp exposures. This reflects the clinical scenario most confronted in the practice of dentistry, as opposed to institutional studies on virgin premolars or third molars slated for extraction in young individuals (Iwamoto et al., 2006; Accorinte et al., 2008; Min et al., 2008). Finally, the median (range) follow-up was 12.8 mos (range, 0-33.5 mos), compared with a follow-up of 2 to 4 mos in many institutional studies (Iwamoto et al., 2006; Accorinte et al., 2008; Min et al., 2008).
Although practitioners were trained in a standard pulp-cap procedure, one of the limitations of this practice-based study was a lack of ongoing monitoring of the study procedures. It is possible that a lack of adherence to study protocol was the cause for an inordinate number of failures in one practice. Exclusion of this practice reduced the magnitude of the difference between the 2 materials, which became statistically insignificant, and thus there is reluctance to declare that this study by itself provides conclusive evidence of better outcomes for MTA. However, given similar trends in other studies, and the strong trend toward MTA in this study even when the one practice was excluded, there is cumulative evidence for MTA superiority. A challenge to this study was the randomization procedure. Since there was concern that a delay in accomplishing the pulp cap could have an adverse impact on pulp-cap success (Aguilar and Linsuwanont, 2011), it was considered inappropriate to utilize a randomization scheme at the time of pulp exposure. Instead, randomization was by practice, and this meant that dentists may have used a material with which they were less familiar. Because most dentist investigators were using CaOH before the study, this situation would have been most relevant for the MTA group, suggesting that the results with MTA may have been even better if the dentists had been as familiar with it as they were with CaOH. A cross-over design was not considered feasible because of the extra training burden on the dentists and increased length of the study.
This article presents the main results of a randomized clinical trial comparing the effectiveness of CaOH and MTA in direct pulp capping. The numerous co-variables collected and their associations with pulp-cap failure, regardless of the treatment material used, will be the subject of a future article.
In conclusion, this large randomized clinical trial, conducted for up to 2 yrs within a practice-based research network, provided confirmatory evidence for a superior performance with MTA as a direct pulp-capping agent as compared with CaOH.
Supplementary Material
Acknowledgments
Special thanks to the Northwest NWP regional coordinators, research staff, practitioner members, and their excellent staffs.
Footnotes
This work was supported in part by NIH/NIDCR Grants U01 DE016750 and U01 DE016752.
The authors declare no potential conflicts of interest with respect to the authorship and/or publication of this article.
Group Authors: Other NWP members and contributors to this study and article are C. Baltuck, C. Barnes, D. Beaudry, J. Shao, E. Lubisich, A. Gilbert, and L. Lowder.
A supplemental appendix to this article is published electronically only at http://jdr.sagepub.com/supplemental.
Contributor Information
for Northwest Practice-based Research Collaborative in Evidence-based Dentistry (NWP):
C. Baltuck, C. Barnes, D. Beaudry, J. Shao, E. Lubisich, A. Gilbert, and L. Lowder
References
- Accorinte Mde L, Holland R, Reis A, Bortoluzzi MC, Murata SS, Dezan E, Jr, et al. (2008). Evaluation of mineral trioxide aggregate and calcium hydroxide cement as pulp-capping agents in human teeth. J Endod 34:1-6. [DOI] [PubMed] [Google Scholar]
- Aeinehchi M, Eslami B, Ghanbariha M, Saffar AS. (2003). Mineral trioxide aggregate (MTA) and calcium hydroxide as pulp-capping agents in human teeth: a preliminary report. Int Endod J 36:225-231. [DOI] [PubMed] [Google Scholar]
- Aguilar P, Linsuwanont P. (2011). Vital pulp therapy in vital permanent teeth with cariously exposed pulp: a systematic review. J Endod 37:581-587. [DOI] [PubMed] [Google Scholar]
- Barthel CR, Levin LG, Reisner HM, Trope M. (1997). TNF-alpha release in monocytes after exposure to calcium hydroxide treated Escherichia coli LPS. Int Endod J 30:155-159. [DOI] [PubMed] [Google Scholar]
- Baume LJ, Holz J. (1981). Long term clinical assessment of direct pulp capping. Int Dent J 31:251-260. [PubMed] [Google Scholar]
- Camp JH, Fuks AB. (2006). Pediatrics: endodontic treatment for the primary and young permanent dentition. In: Pathways to the pulp. 9th ed Cohen S, Hargreaves KM, editors. St. Louis, MO: Mosby Elsevier, pp. 822-882. [Google Scholar]
- Camilleri J. (2008). Characterization of hydration products of mineral trioxide aggregate. Int Endod J 41:408-417. [DOI] [PubMed] [Google Scholar]
- Chacko V, Kurikose S. (2006). Human pulpal response to mineral trioxide aggregate (MTA): a histological study. J Clin Pediatr Dent 30:203-209. [DOI] [PubMed] [Google Scholar]
- Clement AW, Willemsen WL, Bronkhorst EM. (2000). Success of direct pulp capping after caries excavations. Ned Tijdschr Tandheelkd 107:230-232. [PubMed] [Google Scholar]
- Colceriu L, Cimpean S, Pop A, Moldovan M, Colceriu A. (2005). Using mineral trioxide aggregate and calcium hydroxide as pulp-capping materials. Eur Cells Mater 10(Suppl 1):1473-2262. [Google Scholar]
- DeRouen TA, Cunha-Cruz J, Hilton TJ, Ferracane J, Berg J, Zhou L, et al. (2010). Northwest Practice-based REsearch Collaborative in Evidence-based DENTistry (PRECEDENT). What’s in a dental practice-based research network? Characteristics of Northwest PRECEDENT dentists, their patients and office visits. J Am Dent Assoc 141:889-899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donner A, Klar N. (2000). Design and analysis of cluster randomization trials in health research. London, UK: Arnold. [Google Scholar]
- Fitzgerald M, Heys RJ. (1991). A clinical and histological evaluation of conservative pulpal therapy in human teeth. Oper Dent 16:101-112. [PubMed] [Google Scholar]
- Fridland M, Rosado R. (2005). MTA solubility: a long term study. J Endod 31:376-379. [DOI] [PubMed] [Google Scholar]
- Graham L, Cooper PR, Cassidy N, Nör JE, Sloan AJ, Smith AJ. (2006). The effect of calcium hydroxide on solubilisation of bio-active dentine matrix components. Biomaterials 27:2865-2873. [DOI] [PubMed] [Google Scholar]
- Hilton TJ. (2009). Keys to clinical success with pulp capping: a review of the literature. Oper Dent 34:615-625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Islam I, Chng HK, Yap AU. (2006). Comparison of the physical and mechanical properties of MTA and Portland cement. J Endod 32:193-197. [DOI] [PubMed] [Google Scholar]
- Iwamoto CE, Adachi E, Pameijer CH, Barnes D, Romberg EE, Jefferies S. (2006). Clinical and histological evaluation of white ProRoot MTA in direct pulp capping. Am J Dent 19:85-90. [PubMed] [Google Scholar]
- Lin DY. (1994). Cox regression analysis of multivariate failure time data: the marginal approach. Stat Med 13:2233-2247. [DOI] [PubMed] [Google Scholar]
- Luketic S, Malci A, Jukic S, Anic I, Šegovic S, Kaleni S. (2008). Coronal microleakage of two root-end filling materials using a polymicrobial marker. J Endod 34:201-203. [DOI] [PubMed] [Google Scholar]
- Matsuo T, Nakanishi T, Shimizu H, Ebisu S. (1996). A clinical study of direct pulp capping applied to carious-exposed pulps. J Endod 22:551-556. [DOI] [PubMed] [Google Scholar]
- Mente J, Geletneky B, Ohle M, Koch MJ, Ding PGF, Wolff D, et al. (2010). Mineral trioxide aggregate or calcium hydroxide direct pulp capping: an analysis of the clinical treatment outcome. J Endod 36:806-813. [DOI] [PubMed] [Google Scholar]
- Min KS, Park HJ, Lee SK, Park SH, Hong CU, Kim HW, et al. (2008). Effect of mineral trioxide aggregate on dentin bridge formation and expression of dentin sialoprotein and heme oxygenase-1 in human dental pulp. J Endod 34:666-670. [DOI] [PubMed] [Google Scholar]
- Miyashita H, Worthington HV, Qualtrough A, Plasschaert A. (2007). Pulp management for caries in adults: maintaining pulp vitality. Cochrane Database Syst Rev 18:CD004484. [DOI] [PubMed] [Google Scholar]
- Nair PN, Duncan HF, Pitt Ford TR, Luder HU. (2008). Histological, ultrastructural and quantitative investigations on the response of healthy human pulps to experimental capping with mineral trioxide aggregate: a randomized controlled trial. Int Endod J 41:128-150. [DOI] [PubMed] [Google Scholar]
- Stedman MR, Gagnon DR, Lew RA, Solomon DH, Losina E, Brookhart MA. (2009). A SAS macro for a clustered permutation test. Comput Methods Programs Biomed 95:89-94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang W, Walboomers XF, Jansen JA. (2007). The formation of tertiary dentin after pulp capping with a calcium phosphate cement, loaded with PLGA microparticles containing TGF-β1. J Biomed Mater Res A 85:439-444. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.