Abstract
Risk communication is an important component of genetic counseling. However, many authors have noted that after genetic counseling, subjective risk frequently does not match the objective risk provided by the counselor. This inevitably leads to the conclusion that the risk communication process was not “effective”. There has been much discussion about how this problem can be better addressed, such that our clients recall numeric risks more accurately after genetic counseling. This article draws on the risk and probability literature from other fields (including psychology, economics, philosophy and climate change) to deconstruct the concept of “risk” and to attempt to expand upon and develop thought and discussion about and investigation of the risk communication process in genetic counseling.
Keywords: risk assessment, risk perception, risk communication, probability, clinical genetics
“Risk is a close relation to uncertainty. Where we cannot be certain of the link between cause and effect, we clutch at the straw of probability.”
Introduction
Communicating about genetic risks is an important component of genetic counseling. Indeed, the 2006 definition of genetic counseling states that the process integrates:
“Interpretation of family and medical histories to assess the chance of disease occurrence or recurrence.”
The risk communication component of genetic counseling is thought to have important potential consequences (e.g. affecting variables like anxiety and distress, as well as decision making around screening and intervention). Because of this, it has received much attention (Bottorff et al 1998). However, to broadly summarize the findings of those investigations of risk communication in genetic counseling that have been performed to date: recall by clients of the numeric “risks” that they were provided in genetic counseling is typically poor. This leads the effectiveness of the risk communication component of genetic counseling to be called into question.
In 2008, Sivell et al reviewed the genetic counseling literature for studies looking at the effects on decision making of risk perception, construction, and interpretation (Sivell et al 2008). The paper concluded:
“Studies of risk perception often make the assumption that individuals have a quantitative notion of risk which can be measured in various ways. However, the evidence also demonstrates that risk is something experiential and is not something individuals can easily quantify.”
The purpose of this article is to build on and explore the concept of risk as an experience (Sivell et al 2008) - with the aim of encouraging the formulation of new strategies to investigate this important topic. Specifically, I aim to explore the semantics around, and deconstruct the concept of “risk” in the context of genetic counseling – and in particular, the perception of risk. To achieve this, I will draw upon previous work relating to risk from the genetic counseling literature as well as literature from other fields.
What is “risk”?
Although “risk” is a commonly used term, there are many different ways in which it can be interpreted (Bottorff et al 1998). As genetic counselors, we tend to use it as a synonym – at least in our professional communications with each other - for “probability”. It is important to note though, that this interpretation of meaning is likely not to be shared by many of our clients. According to the Oxford English Dictionary, by definition, “risk” is “the possibility that something unpleasant will happen”, this concept conveys two components: possibility (or, to express this more mathematically, probability) and some kind of nebulous negative attribute. It is for the reason that the word “risk” has a negative connotation inherent to it that when engaged in the process we professionally refer to as “risk assessment” many genetic counselors choose to talk about the more value-neutral “chances” rather than “risks”.
Thus, as Sivell et al alluded to: risk, as a concept, is more than numeric probability alone (Sivell et al 2008). Intuitively for example, the meaning of a numeric probability depends on the nature of the outcome to which the numeric probability is related. Further support for, and additional nuance to this idea comes from Shiloh (Shiloh 2006), who applied illness regulatory theory to genetic counseling, and noted that:
“peoples’ perceptions of and beliefs about an illness, are important mediating links between health threats and reactions to them” (Shiloh 2006)
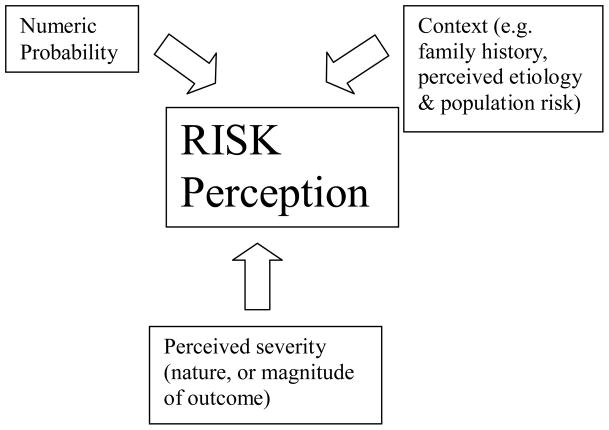
In the above quote, it seems to be quite legitimate, with regard to the preservation of meaning, to substitute “perceived risks” for “health threats”. Doing this illuminates the relevance of peoples’ perceptions of and beliefs about an illness to risk perception (Etchegary and Perrier 2007) (Shiloh and Sagi 1989). In fact, in the psychology and behavioural economy literature, perception of risk for a particular outcome has been framed as being based on perceptions of a combination of factors including: numeric probability, context, and nature of the potential outcome (Patt and Schrag, 1993). See Figure 1.
Figure 1.
Model of contributors to the concept of risk, applied to genetic counseling.
Applying this model to risk in a genetic counseling scenario, we arrive at the following:
Context: factors such as the client’s perceptions of: illness etiology, family history, population prevalence of the condition, etc
Nature of potential outcome: the perceived severity of illness for which numeric probability is being provided.
Numeric probability: initially, the pre-existing subjective numeric probability figure perceived by the client; subsequently this may be modified by the objective numeric probability provided by the counselor.
In the following sections, the evidence (from the broader literature as well as that relating directly to genetic counseling) regarding the influence on risk perception of each of these three components will be reviewed.
Context and risk perception
A non-genetic counseling related example of how context influences risk perception comes from the work of Windschitzl and Weber, 1999. In their experiment, the authors gave psychology students one of two scenarios which both involved a traveler (Windschitl and Weber 1999). In each scenario the students were told that the traveler had a 30% chance to develop mild malaria. In this experiment, the influence of context on risk perception was tested by providing the same numeric probability for malaria in each of the two scenarios, but different destinations – India and Hawaii. When the traveler’s destination was India, not only did the students use language conveying more certainty to describe the risk for malaria, but also when challenged later, they recalled higher numeric probabilities.
In relation to genetic counseling, Walter et al (2004) found that individuals’ perceptions of risk for illness was informed by factors including family history and perceived etiology (Walter et al 2004) – both aspects of context (See Sivell et al, 2008 for an excellent review of studies that have identified association of risk perception in genetic counseling with various contextual factors.)
Severity and risk perception
Individuals are more likely to describe numeric probabilities relating to outcomes they perceive to be more severe as being, for example, “quite high” or “very high”. This phenomenon is well illustrated by an experiment conducted by Patt and Schrag, who gave undergraduate students one of two scenarios both of which involved a numeric probability of 10% for one of two different weather events. In one scenario the weather event was snow flurries, in the other it was a hurricane (Patt and Schragg 2003). The authors found that the students with the hurricane scenario (more severe) were more likely to use descriptors conveying increased likelihood (likely, very likely) than the students with the snow flurry scenario.
In relation to evidence for influence of severity on risk perception in the realm of genetic counseling, Walter and Emery (2006) looked at perceptions of illnesses including diabetes, heart disease, and cancer, and found that individuals with a family history of heart disease or diabetes tended to have a lower sense of personal vulnerability than those individuals with a family history of cancer. Indeed, the authors reported that some perceived heart disease to be “a good way to go” (Walter and Emery 2006). This demonstrates that a lower sense of vulnerability (lower perceived risk) can be associated with perceiving the disease for which one is at risk for to be less “severe” (See Sivell et al 2007, for a review of the genetic counseling related literature that has associated risk perception with personal experience of illness and its treatment.)
Numeric probability and risk perception
Recall of objective numeric probability after genetic counseling tends to be inaccurate (e.g. (Hallowell et al 1997; Hallowell et al 1998). In fact, the subjective numeric probability for illness an individual perceived prior to counseling predicts numeric probability perceived after counseling – a phenomenon clearly reviewed and described elsewhere (Senay and Kaphingst 2009). Typically, in studies where subjective numeric probabilities have been assessed before and after genetic counseling, the post-counseling figure usually lies between the pre-counseling subjective probability, and the objective probability.
Relationship between descriptors of risk and numeric probability
An important side note to this discussion relates to the relationship between descriptors used when communicating about numeric probability. As we see from the experiments of Patt and Schrag outlined above, descriptors such as “likely” or “unlikely” are used and interpreted as not simply relating to numeric probability (Patt and Schragg 2003). Rather, these descriptors also incorporate and code for perceptions of nature of the outcome (or severity). These descriptors convey risk, rather than simply numeric probability (Shiloh and Saxe 1989). Thus, it is not surprising that a review of the literature showed that rather than there being any mechanism by which numeric probabilities and descriptors (such as likely, or unlikely) could be mapped onto each other, “people perceive the word likely to imply probabilities anywhere between .5 and .99” (Weber 1994).
Implications for genetic counseling
There are a number of potential implications of re-conceptualizing risk in this way for genetic counseling practice.
First, although it has been suggested as a risk communication strategy (Crowson et al 2007), on the strength of the evidence from other disciplines, it seems that genetic counselors should not use their own risk descriptors (high chance, low chance etc) in clinical practice. Because contexts and perceptions of the nature of the potential outcome are likely to be quite different between individuals (Shiloh 2006), a “low chance” for the counselor may be conceptualized as something very different to the client. Also however, not only do people describe numeric probabilities relating to outcomes they perceive to be more severe with a greater degree of certainty, but:
“people are also sensitive to this practice in others, expecting a certain amount of exaggeration about the likelihood of high magnitude events” (Patt and Schrag, 2003).
In the context of genetic counseling, this kind of miscommunication could potentially have quite dramatic negative sequelae. At the very least, genetic counselors should not use descriptors of risk: (a) without qualifiers (regarding genetic counselors perceptions of context and severity, and acknowledgement that this may be markedly different from that of their client), or (b) in place of numeric probability.
Second, while we do far more as genetic counselors during the process of risk communication than provide and discuss numeric probabilities, we should be aware that when we are providing numbers in the context of risk communication, (in any of the myriad forms, percentages, 1 in X, visual aids etc) we are providing information only about the numeric probability of an event – not about the broader concept of “risk”, which would include severity, context, and potentially other factors too. As a profession founded on valuing clear communication, our current tendency to use “risk” when we actually mean “probability” seems to be somewhat at odds with our goals and values. Based on our professional principles, we have a responsibility to make the conceptual distinction – if we agree there is one – between risk and probability explicit for both ourselves and our clients, by being careful about the language we use relating to the numbers (i.e. not referring to them risks, but probabilities).
This is related to another point, that to date, the genetic counseling literature relating to risk communication overall has implicitly communicated the view that the counselor is the “risk expert”, whose role is to impart information about “risk” to the patient. Often, the client then recalls that information inaccurately. Implied in this, is that one party here is at fault – either the counselor for not communicating the information well enough, or the client for not attending to it. For example, in 2009, a study of “risk perception” amongst a population at “increased risk” for cancer concluded that: “the participants accuracy in risk perception was poor” (Rantala et al 2009). In this, the genetic counseling literature is not alone, in fact this phenomenon occurs in other fields, as stated by Finkel in 2008:
“…the risk assessment literature clearly sees many of the risk perceptions of laypeople as arising from deficiencies and errors in judgment rather than from ways of processing empirical and other information that are worthy of some deference, if not respect.” (Finkel 2008)
Some have argued that genetic counselors should use techniques by which clients can helped to think about risks more rationally and logically, essentially dismissing the context and nature of outcome components of risk, in favor of promoting logical decisions based on accurate estimation of numeric probability (Etchegary and Perrier 2007). Conversely, I would suggest the following: First, this strategy fails to recognize any contributors to decision making other than subjective numeric probability, despite the fact that other variables are very important (Senay and Kaphingst, 2009). Thus, rather than encouraging clients to make logical decisions based on accurate estimation of numeric probability, why should our goal as genetic counselors not be to ensure that our clients make the best possible - emotionally inclusive - decision that they can based on thorough conscious awareness of their perceptions of context and nature of outcome? Second, if we accept that risk perception is a multifaceted construct – of which numeric probability is only one component, perception of which seems to be heavily influenced by other information that is “worthy of deference” - one could make a strong case that it is such an individualistic concept, that the question of whether an individual’s risk perception is accurate is essentially unanswerable. This would allow us to acknowledge the client as the “risk expert” for themselves (thus better reflecting the ethos of genetic counseling) and reframe ourselves, as genetic counselors – perhaps more appropriately - as the “experts” in numeric probabilities, and helping the client to be consciously aware of their perceptions of context and nature of outcome). Last, I would also argue that while it has the appeal of simplicity, the concept of measuring recall accuracy of objective numeric probability is too heavily informed by the medical-model and paternalism to either accurately reflect the client-centred ethos of genetic counseling (Edwards et al 1999), or usefully assess the effectiveness of the complex process that constitutes risk communication in the context of genetic counseling.
This leads to the last, and perhaps most important potential implication of this re-conceptualization of risk for genetic counseling – it could be applied to attempt to illuminate the issue of why recall of numeric probability is poor after genetic counseling. Specifically, perhaps this phenomenon exists because numeric probabilities alone are meaningless without context and nature of outcome, and because these components of risk perception are so interwoven that they are not separable (Walter et al 2004).
To be more explicit: hypothetically, when provided an objective numeric probability, the client integrates that into their perception of risk (according to context and perception of severity etc). The meaningful concept that the client takes away then, is perhaps, not the objective numeric probability, but rather a modified risk concept (Shiloh 2006). Support for the hypothesis that context influences numeric probability recall comes from the results of the experiment by Windschitzl and Weber, 1999, described above (Windschitl and Weber 1999). Specifically, when students were all provided the same numeric probability – in this case for a traveler in the scenario they had been provided with to develop malaria - and were later asked to recall this they gave higher numbers if the destination was India than if it was Hawaii, demonstrating that their risk concept had been altered by context, and that this context influenced the numeric probabilities they recalled when prompted.
Support for the idea that perception of illness severity influences recall of objective numeric probability is documented by Sivell et al, who offer the following insight into the situation where after receiving an objective numeric probability, some individuals continue to overestimate:
“…being able to understand and reiterate an objective numerical risk estimate is not necessarily their primary goal; rather they are seeking ways in which they can manage and cope with their risk status as indicated by a desire expressed by some to obtain access to health services that are not indicated for their level of risk.” (Sivell et al 2008)
To elaborate further, if we assume that the nature of the potential outcomes for which the numeric probability is provided is, in the context of genetic counseling, likely to be perceived by our clients as undesirable, the observation that some people tend to overestimate numeric probability even after having been provided with objective assessment, is directly in accordance with the expectations based on the concept of “asymmetric loss functions”. This concept posits that overestimation occurs because the more undesirable the potential outcome, the more costly are underestimates of the probability of that outcome (Weber, 1994). More specifically, to underestimate the risk for breast cancer for example:
“….could potentially result in death due to insufficient medical monitoring because of inadequate concern. Overestimates of the probability level on the other hand carry few costs (some unnecessary monitoring, perhaps) and will give rise to relief when the danger turns out to be smaller than expected.” (Weber 1994)
Thus, overestimated recall of numeric probability after genetic counseling likely reflects (at least in part) the client’s perception of severity of the illness for which the numeric probability was provided.
To return to the hypothetical genetic counseling scenario, and the proposition that the meaningful concept that the client takes away from the risk communication process, is not the objective numeric probability, but rather a modified risk concept (Shiloh 2006), it is important to note that even then, this newly-modified risk concept will not remain static (Shiloh, 2006). That is, over time, if additional family members become affected, this could modify perceptions of family history (and therefore potentially alter context), and new or additional impact of illness on the family (e.g. death or suffering) could lead to modification of perception of severity. Thus, when asked after genetic counseling to recall the objective numeric probability that was provided, the individual is more likely to provide a number that – in their perception - reflects their composite sense of risk that has been modified not only by the genetic counseling, but also by the context and perception of severity that existed prior to genetic counseling, and other life events since the intervention.
If we conclude that risk perception is multifaceted and dynamic (and comprises more than numeric probability), it becomes easy to feel that rich opportunity to learn about the impact of genetic counseling is lost through the conflation of these concepts. In fact, in 1999, Edwards and Elwyn suggested that “affective” outcomes like satisfaction, certainty that the best option was selected in resulting decision-making etc, would potentially be more sensitive and specific for application to risk communication research than the more traditional tools of assessing knowledge or risk perception (Edwards et al 1999). If we accept that perception of risk involves more than subjective numeric probability alone, and further that risk perception is an important contributor to, but not the sole contributor to decision making, it becomes apparent that a reappraisal of the strategies by which we attempt to measure and describe effectiveness of risk communication in genetic counseling is urgently needed.
Conclusion
Perhaps it is because we use “risk” as a synonym for probability, that we tend to oversimplify the concepts of both risk perception and decision making, as manifested in our attempts to measure these processes having been largely founded on subjective numeric probability. As genetic counselors we do far more during the process of risk communication than simply deliver objective numeric probabilities. Indeed, Edwards et al 2008 suggested on the strength of their review of the literature, that it is the supportive, counseling component of genetic counseling that has the most value to patients, rather than the informational component (Edwards et al 2008). When we embark upon psychosocial investigation of the impact of objective numerical probabilities with our patients, we are addressing “risk”. Prior to providing the objective numeric probabilities we have derived for them, many of us explore our patients’ pre-existing of numeric probability of illness, family history, and etiology – this could be conceptualized in terms of the model of risk presented here as investigating the context. We also ask about our patients’ experiences with the illness for which we are calculating numeric probabilities – again, in the context of the model of risk presented here as providing us with information about their perceptions of severity or nature of outcome.
I propose that a more thorough and nuanced conceptualization of risk perception, as a multifaceted entity comprising numerical probability, context, and severity would better serve the advancement of the genetic counseling profession in that it would open the potential for conceptualizing and developing novel strategies by which to investigate the impact of an integral and important component of the genetic counseling session - the risk communication process (Edwards et al 1999). By conflating risk and probability, and assessing recall of objective numeric probability as the sole measure of whether or not our risk communication is effective, we have only been able to show - at best - limited evidence of improved accuracy of “risk perception” (Edwards et al 2006). By continuing with this tack, we lose opportunity to learn about the impact of what we do. In this, we do ourselves - and potentially our clients - a disservice.
In this era of evidence-based medicine, our credibility as a profession depends on our ability to measure, and ideally quantify, the effect of our intervention such that we can demonstrate a meaningful positive impact. I propose that it is time for the genetic counseling profession to make it an urgent priority to develop concepts and metrics by which to more appropriately capture the effects of our intervention.
Acknowledgments
This concept for this manuscript was developed as a result of interactions with scholars from a wide variety of disciplines at the UBC Peter Wall Institute for Advanced Studies – the author thanks the institute’s 2009–2010 cohort of Early Career Scholars. Sincere thanks to Victoria Lemieux and Susan Creighton for their thoughtful comments and suggestions on earlier drafts of this manuscript. JA was supported by the Provincial Health Services Authority of BC, the Canadian Institutes of Health Research, and the Michael Smith Foundation for Health Research.
References
- Adams J. Risk and morality: three framing devices. In: Ericson RV, Dobson W, editors. Risk and Morality. Toronto: University of Toronto Press; 2003. pp. 86–103. [Google Scholar]
- Bottorff JL, Ratner PA, Johnson JL, Lovato CY, Joab SA. Communicating cancer risk information: the challenges of uncertainty. Patient Educaction and Counseling. 1998;33:67–81. doi: 10.1016/s0738-3991(97)00047-5. [DOI] [PubMed] [Google Scholar]
- Crowson CP, Therneau TM, Matteson EL, Gabriel SE. Primer: demystifying risk - understanding and communicating medical risks. Nature Clinical Practice. 2007;3(3):181–7. doi: 10.1038/ncprheum0397. [DOI] [PubMed] [Google Scholar]
- Edwards A, Elwyn G. How should effectiveness of risk communication to aid patients’ decisions be judged? A review of the literature. Medical Decision Making. 1999;19:428–434. doi: 10.1177/0272989X9901900411. [DOI] [PubMed] [Google Scholar]
- Edwards A, Evans R, Dundon J, Haigh S, Hood K, Elwyn GJ. Personalized risk communication for informed decision making about taking screening tests. Cochrane Database of Systematic Reviews. 2006;18(4):CD001865. doi: 10.1002/14651858.CD001865.pub2. [DOI] [PubMed] [Google Scholar]
- Edwards A, Gray J, Clarke A, Dundon J, Elwyn G, Gaff C, Hood K, Iredale R, SIvell S, Shaw C, Thornton H. Interventions to improve risk communication in clinical genetics: systematic review. Patient Educaction and Counseling. 2008;71:4–25. doi: 10.1016/j.pec.2007.11.026. [DOI] [PubMed] [Google Scholar]
- Etchegary H, Perrier C. Information processing in the context of genetic risk: implications for genetic-risk communication. Journal of Genetic Counseling. 2007;16(4):419–32. doi: 10.1007/s10897-006-9082-z. [DOI] [PubMed] [Google Scholar]
- Finkel AM. Perceiving others’ perceptions of risk: still a task for Sisyphus. Annals of the New York Academy of Science. 2008;1128:121–37. doi: 10.1196/annals.1399.013. [DOI] [PubMed] [Google Scholar]
- Hallowell N, Green JM, Statham H, Murton F, Richards MPM. Recall of numerical risk estimates and counsellees’ perceptions of the importance of risk information following genetic counselling for breast and ovarian cancer. Psychology, Health and Medicine. 1997;2(2):149–169. [Google Scholar]
- Hallowell N, Statham H, Murton F. Women’s understanding of their risk of developing breast/ovarian cancer before and after genetic counseling. Journal of Genetic Counseling. 1998;7(4):345–364. doi: 10.1023/A:1022072017436. [DOI] [PubMed] [Google Scholar]
- Patt AG, Schrag DP. Using specific language to describe risk and probability. Climatic change. 2003;61:17–30. [Google Scholar]
- Rantala J, Platten U, Lindgren G, Nilsson B, Arver B, Lindblom A, Brandberg Y. Risk perception after genetic counseling in patients with increased risk of cancer. Hereditary Cancer in Clinical Practive. 2009;73(1):15. doi: 10.1186/1897-4287-7-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Resta RG. Defining and redefining the scope and goals of genetic counseling. American Journal of Medical Genetics. 2006;142(4):269–275. doi: 10.1002/ajmg.c.30093. [DOI] [PubMed] [Google Scholar]
- Senay I, Kaphingst KA. Anchoring and Adjustment bias in communication of disease risk. Medical Decision Making. 2009;29(2):193–201. doi: 10.1177/0272989X08327395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shiloh S. Illness representations, self-regulation, and genetic counseling: A theoretical review. Journal of Genetic Counseling. 2006;15(5):325–337. doi: 10.1007/s10897-006-9044-5. [DOI] [PubMed] [Google Scholar]
- Shiloh S, Sagi M. Effect of framing on the perception of genetic recurrence risks. American Journal of Medical Genetics. 1989;33(1):130–5. doi: 10.1002/ajmg.1320330121. [DOI] [PubMed] [Google Scholar]
- Shiloh S, Saxe L. Perception of risk in genetic counseling. Psychology and Health. 1989;3(1):45–61. [Google Scholar]
- Sivell S, Elwyn G, Gaff CL, Clarke AJ, Iredale R, Shaw C, Dundon J, Thornton H, Edwards A. How risk is perceived, constructed and interpreted in clients in clinical genetics, and the effects on decision making: a systematic review. Journal of Genetic Counseling. 2008;17(1):30–63. doi: 10.1007/s10897-007-9132-1. [DOI] [PubMed] [Google Scholar]
- Walter FM, Emery J. Perceptions of family history across common diseases: a qualitative study in primary care. Family Practice. 2006;23(4):472–80. doi: 10.1093/fampra/cml006. [DOI] [PubMed] [Google Scholar]
- Walter FM, Emery J, Braithwaite D, Marteau TM. Lay understanding of familial risk of common chronic diseases: A systematic review and synthesis of qualitative research. Annals of Family Medicine. 2004;2(6):583–94. doi: 10.1370/afm.242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weber EU. From subjective probabilities to decision weights: the effect of asymmetric loss functions on the evaluation of uncertain outcomes and events. Psychological Bulletin. 1994;115(2):228–242. [Google Scholar]
- Windschitl PD, Wever EU. The interpretation of “likely” depends on context, but “70%” is 70% - right? The influence of associative processes on perceived certainty. Journal of Experimental Psychology: Learning, Memory and COgnition. 1999;25:1514. doi: 10.1037//0278-7393.25.6.1514. [DOI] [PubMed] [Google Scholar]