Abstract
Background
While it is clear that affect is negatively impacted by heavy drinking in adulthood and that it improves with abstinence, little is known about effects of heavy drinking on mood during adolescence.
Methods
The present study examined negative mood states among 16–18 year-old high school students with a history of recent heavy episodic drinking (HED; n = 39) and comparison youth with limited lifetime drinking experience (CON; n = 26). Affect was assessed at three time points during a 4–6 week period of monitored abstinence using the Hamilton Rating Scales for Anxiety and Depression; self-reports were obtained with the state portion of the State Trait Anxiety Inventory, and experience sampling of current affect was assessed via daily text messages sent at randomly determined times in the morning, afternoon, and evening.
Results
Youth with a recent history of HED reported more negative affect compared to non-drinking youth during early stages of abstinence (days since last HED at assessment 1: m = 6.46; SD = 5.06); however differences in affect were not observed after 4–6 weeks of abstinence. Sex differences were evident, with HED girls reporting greater depression and anxiety than HED male peers. Although not significant, response patterns indicated that males may experience faster resolution of negative emotional states than females with sustained abstinence.
Conclusions
Findings suggest that high dose drinking is associated with elevated negative affect for adolescents and that negative mood states may take longer to resolve for girls than for boys following heavy drinking episodes. Future research clarifying naturally occurring changes in affective response during early and sustained abstinence is necessary for improving programs designed to promote adolescent decision-making and to reduce risk for relapse.
Keywords: mood, depression, anxiety, experience sampling, text message
Introduction
Heavy drinking and alcohol use disorders have been associated with exacerbations in depression and anxiety symptoms in adults, both in clinical and community samples (Falk et al., 2008; Grant et al., 2009). Negative mood is a common precursor to relapse among adults (e.g., Brady et al., 2006; Breese et al., 2005; Brown et al., 1995a; Cooney et al., 1997; Sinha, 2007; Sinha et al., 2006) and adolescents (Cornelious et al., 2003; Rowe et al., 2004) following treatment for an alcohol use disorder; in some studies negative affect predicts poorer response to treatment (Glenn and Parsons, 1991), as well as higher service utilization (Wu et al., 1999). In adults, improvements in affect have been shown after 3–4 weeks of abstinence from heavy alcohol use (Brown and Shuckit, 1988; Brown et al., 1995b), but the impact of sobriety on adolescent mood has not yet been examined. Of note, intensity of recent drinking and adverse physiological consequences (e.g., withdrawal symptoms, blackouts) appear to be associated with slower recovery of affective functioning in adults (Brown et al, 1995b). Adolescent vacillation of affective states may result in greater exposure to negative mood states in the natural environment, which has been associated with alcohol use in early adolescence (Hussong et al., 2001).
National samples suggest that compared to adults, adolescent drinkers tend to drink in higher volumes. In the NESARC study (Naimi et al., 2003), while adults in the United States drink between 2–3 standard drinks per occasion, youth consume 4–5 drinks on average when they drink. Donovan (2009) has shown that these levels are consistently beyond the legal drinking level (.08 BAC) and are considered heavy episodic drinking (HED) or binge drinking (3–4 or more drinks per occasion for girls and 5 or more drinks per occasion for boys). Intensity of adolescent alcohol consumption is a critical concern due to alcohol related behavioral consequences including accidents, injuries, school dropout, suicide, and homicide (Ellickson et al., 2003; Hill et al., 2006; McCarty et al., 2004; Miller et al., 2007), and alcohol-related neurocognitive consequences of progression to, and persistence of heavy drinking (Brown et al., 2000, 2008; Squeglia et al., 2009). Recent models of youth alcohol use suggest that this binge-type drinking is a critical step in adolescent progression to alcohol abuse and dependence (Bekman et al., 2011).
Despite these concerns, the adverse impact of youth alcohol consumption on mood states has received relatively limited attention. In previous research, youth maintaining abstinence following treatment for an alcohol and/or other substance use disorder have shown improvements in both depression and anxiety during the first year following treatment (Anderson et al., 2008; Hogue, et al., 2008). In the general population, depression symptoms have been shown to be a risk factor for early alcohol involvement (e.g., Bekman et al., 2010) while anxiety can be both a protective factor for the onset of drinking (Tomlinson et al., in press) and a risk factor for escalation once drinking has been initiated (Abrantes et al., 2004). More recently, heavy drinking in adolescence has been associated with lower distress tolerance (Lejuez et al., 2003) that improves with sustained abstinence (Winward et al., under review).
Both negative affect and mood fluctuations increase with pubertal development (Brown et al., 2008); however, most standardized measures of negative affect ask individuals to summarize their mood state over a period of time (i.e., past week or month). Alternative state measures of affect are typically administered in the lab or interview setting and only capture affective feedback for that moment. Recently, researchers have utilized technological devices, such as pagers, cell phones, or other handheld electronic equipment to gather moment by moment data in the natural environment (Ravert et al., 2010; Reid et al., 2008). To our knowledge, experience based sampling, or measurement in the participants’ natural environment, via text message has never been utilized to evaluate fluctuations in mood among youth during early abstinence from alcohol and other drug use.
This study examined differences in mood during early abstinence among youth with recent HED compared to demographically-matched, non-drinking peer controls (CON), and affective changes over 4–6 weeks of continued abstinence. We predicted that HED youth would report greater depression and anxiety symptoms than CON during early abstinence, but that this pattern would normalize over 4–6 weeks of abstinence. Finally, we expected that youth engaged in heavier recent alcohol and other substance use prior to baseline would demonstrate more negative affect at baseline, and larger changes in negative affect with sustained abstinence.
In order to detect changes in both global affective ratings and daily mood fluctuations, we utilized a multi-method measurement approach which included a (a) standardized interview measure, (b) self-report measure, and (c) experience sampling via text messaging. Experience sampling in the natural environment provided a means to assess the relations between time varying characteristics (e.g., affect, fatigue) and alcohol abstention. We expected that these three methodologies of assessing affect would relate to one another, but that each would also provide unique information regarding fluctuations in adolescent affect.
Materials & Methods
Participants
As the overarching goal of the larger study was to examine the impact of repeated HED on neuropsychological and psychosocial functioning during adolescence and changes in this functioning with sustained abstinence, we specifically recruited a population of youth who had repeatedly engaged in HED but were not seeking treatment. Adolescents with recent HED and matched non-drinking CON, ages 16–18, were recruited from local school districts and the surrounding communities in metropolitan San Diego County as part of a larger longitudinal study. HED teens were selected if they had consumed alcohol on more than 100 occasions, had engaged in at least three heavy drinking episodes (5+drinks/occasion for boys, 4+ drinks/occasion for girls) during the past month, had experienced one or more withdrawal symptoms following a recent drinking episode, and had limited exposure to other substances (see Table 1). CON participants, selected to be matched on demographic characteristics, had no history of HED or alcohol or drug problems. Adolescents were excluded from participation if their parent or guardian did not agree to provide corroborating information about the participant’s history, if they had been diagnosed with a psychiatric or neurological disorder, had experienced a significant head trauma with loss of consciousness for 2 minutes or longer, did not speak English, or had a history of substance dependence or heavy recent drug use. Youth were not in treatment or seeking treatment when they participated in this study.
Table 1.
Alcohol and substance use at baseline.
| Controls (n = 26) | Heavy Episodic Drinkers (n = 39) | |||
|---|---|---|---|---|
| Within Group n | m (SD) | Within Group n | m (SD) | |
| # Alcohol use occasions (Lifetime) | 19% | 3.80 (3.70) | 100% | 219.77 (174.39) |
| # Binge drinking occasions (Lifetime) | 4% | 1 | 100% | 114.85 (92.07) |
| # Binge drinking occasions (Past 3 months) | 0% | - | 100% | 15.75 (11.65) |
| # Alcohol withdrawal symptoms (Lifetime) | 0% | - | 100% | 4.21 (2.34) |
| Max drinks/occasion (Lifetime) | 12% | 2.00 (1.00) | 100% | 11.05 (4.71) |
| # Marijuana use occasions (Lifetime) | 4% | 1 | 97% | 59.15 (75.83) |
| # Other drug use occasions (Lifetime) | 0% | - | 59% | 8.69 (17.09) |
| Days since last alcohol use at intake | 15% | 100.25 (73.90) | 100% | 5.62 (5.11) |
| Days since last alcohol binge at intake | 4% | 159 | 100% | 6.46 (5.06) |
| Days since last marijuana use at intake | 4% | 166 | 97% | 213.61 (34.65) |
| Days since last other drug use at intake | 0% | - | 59% | 193.22 (272.08) |
HED (n = 39) and CON (n = 26) youth were well matched on personal characteristics such as age (HED: m = 17.84, SD = .76; CON: m = 17.63, SD = .63), sex (HED: 51% male; CON: 54% male), racial and ethnic background (HED: 82% white, 23% Hispanic; CON: 73% white, 23% Hispanic), and socioeconomic status (Hollingshead Code, 1965; HED: m = 27.03, SD = 13.79; CON: m = 23.73, SD = 12.30), but differed with regards to family history of substance-dependence (HED: 63.3% positive; CON: 30% positive).
Procedure
Recruitment and Screening
Fliers advertising a research study examining adolescent development (without mention of alcohol or drug use criteria) and compensation (up to $485 for 6 weeks) were mailed to students at local high schools, as well as posted at colleges, universities and community settings (Brown et al., 2005; Tapert et al., 2003). Interested youth and/or their parents contacted study staff by phone and the study aims and protocol were described, verbal consent was obtained, and preliminary screens were administered to the youth and his or her parent (by two separate staff members to maintain confidentiality).
All participating teens and their parents provided informed consent and assent in compliance with the guidelines of the University of California, San Diego Research Protection Program. Youth were asked to remain abstinent for a period of up to six weeks, respond to text messaging prompts three to six times per day throughout their participation, and complete three in-person assessments, each two weeks apart (days between assessments 1 and 2; m = 14.39; SD = 2.33; days between assessments 2 and 3; m = 13.73, SD = 1.97). Participants were paid biweekly for assessment completion, and received a $100 bonus if they completed all scheduled assessments and remained abstinent throughout the study period. Additionally, a motivational interviewing-based protocol was used to encourage sustained abstinence among participating youth. Every CON participant completed all three primary assessments. Of the 39 initial HED participants, 4 were discontinued from participation due to substance use and one chose to discontinue due to scheduling conflicts (3 at Time 2; 5 at Time 3).
Abstinence Verification
Participant abstinence from alcohol and other drugs was monitored via daily self-reports and urine samples obtained 2–3 times per week for the duration of their participation and at each in-person assessment. Two alcohol metabolites, ethyl glucuronide (EtG) and ethyl sulfate (EtS), were tested, both which remain in urine for 24–72 hours after drinking (Wurst et al., 2006). These samples were analyzed using LC/MS/MS (liquid chromatography/mass spectrometry/mass spectrometry) and results were provided to staff within 1–3 days. Teens always provided a urine sample on Sunday to capture potential weekend drinking. To prevent tampering, subject belongings were left outside the bathroom, adulteration strips were used to detect diluted or altered samples, sample temperature was taken immediately, and the labeled sample was kept in view at all times. Additionally, samples were submitted to a 13-panel drug screen, including amphetamine, barbiturates, benzodiazepines, cocaine, marijuana, MDMA (ecstasy), methadone, opiates, oxycodone, phencyclidine, and tricyclic antidepressants. Participants also provided breath samples at each appointment.
Measures
The Hamilton Rating Scales for Anxiety & Depression (HAM-D, Hamilton, 1980; HAM-A, Hamilton, 1959)
All participants were administered the HAM-D and HAM-A by research staff trained to use these instruments. The HAM-D is a 26-item interview that quantifies the severity of depressive symptoms during the past week. Items measuring cognitive, affective, somatic, and vegetative symptoms associated with depression are rated on a 5 point scale from 0 (absent) to 4 (severe). The HAM-A is a 14-item interview that assesses the severity of global anxiety. Items assess anxious mood, tension, fears, insomnia, somatic complaints, and behavior via a 5 point scale that measures severity from 0 (none) to 4 (severe). Hamilton anxiety and depression interviews were conducted at all three timepoints. Extensive literature has documented the reliability and validity of both questionnaires for depression and anxiety, with data collected from clinical and nonclinical samples ages 12 and older (Addington, 1992; Fava, 1982; Hamilton, 1959; 1960; Maier et al., 1987; Trajković et al., 2011). In the current study, these two scales were combined to create a composite measure of negative affect (Hamilton Total).
State-Trait Anxiety Inventory-State (STAI-S; Spielberger et al., 1970a)
The STAI-S is a 20-item self-report questionnaire with 20 statements that measure current anxiety symptoms. The participants were asked how much they agree with statements assessing current anxiety symptoms on a four-point scale: 0 (not at all), 1 (somewhat), 2 (moderately), and 3 (very much). Scores range from 0–60, with a higher score indicating a greater degree of anxiety. Participants completed the STAI-S at all three time points. This measure has demonstrated reliability and validity in both clinical and research settings (Spielberger, 1983; Spielberger and Diaz-Guerrero, 1976; 1983; Spielberger et al., 1970b).
Text Message Experience Sampling (Hussong et al., 2001; Ravert et al., 2010)
Youth responded to daily text messages with mood ratings on a scale from 1 (low) – 5 (high) throughout their participation. They were asked to assess their mood in the following three domains: down, angry, and stressed. They received a text message prompt three times a day on any given day at randomly selected times between 10am–2pm, 2pm–6pm, and 6pm–10pm. This measure sampling was conducted to gather more detailed data regarding daily fluctuations in mood. Youth received an additional text during each time slot for a total of six mood samples per day within two days of their in-person assessments. Participants were also asked to report their location (e.g., home, school), and social context (e.g., friends, family) at each sampling. Four of the 65 participants utilized cell phones provided by the research project; all others used their own cell phones with text messaging capability.
To evaluate the effectiveness of our experience sampling via text messaging, we calculated the percentage of text message responses received within the requested time frame (within 90 minutes of participant’s receiving our prompt based on length of class time). Out of 7,674 scheduled text messages, 3% were not received due to errors with the automated text messaging service. HED and CON participants responded to equivalent rates of received text messages (96% and 93%, respectively); and 90% of the sample responded within 90 minutes. To summarize participants’ mood ratings in temporal proximity to their interview and self-report assessments, the current analyses utilized data collected during three days immediately prior to and/or following their in-person appointments. On average, 2–3 text messages per day were received within 90 minutes of the prompt text and summarized during this three day period. The percentage of text messages in which the participant reported any negative affect (i.e., medium, high, or very high ratings of ‘down’, ‘angry’ or ‘stressed’) is reported.
Structured Clinical Interview
This 90-min interview (Brown et al., 1994) assessed demographic information, social and academic functioning, physical and emotional health, and family history of alcohol use, including maternal use during pregnancy. This measure has been validated in an adolescent sample.
Timeline Followback (TLFB)
A modified TLFB (Sobell et al., 1979) procedure was used to assess alcohol, marijuana and other drug use for the 45 days prior to the youth’s initial assessment and in the 30 days after their participation in the study. Evaluations used a calendar format, and trained research personnel provided temporal cues (e.g., special events) to assist recall. For each day, teens indicated whether they had drunk alcohol or used substances, and if so, how much they used.
Customary Drinking and Drug Use Record (CDDR; Brown et al., 1998)
Alcohol, nicotine, marijuana, and other drug use, withdrawal symptoms, DSM-IV abuse and dependence criteria, substance-related life problems, and intentions to quit were assessed using the well-standardized CDDR. The lifetime version was administered during screening and assessed age of first and regular use, and general use patterns for alcohol, marijuana, nicotine, and other drugs every year since age 12.
Analytic Approach
The relationships among baseline interview (Hamilton Total), self-report (STAI-S), and experience sampling affect measures (% Texts Negative Affect) were examined via Pearson correlations, and t-tests were conducted to assess differences in negative affect between HED and CON at baseline. Linear mixed models were used to examine group and sex differences in mood during early abstinence. Separate models were created for each mood index. Models included “fixed” effect terms, which modeled the mean trajectory of subjects across the three assessment timepoints as a function of the covariates of group and sex. Models also included “random” effects, which allowed individual subject baseline levels (intercept) and rates of change (slope) to vary randomly about the mean trajectory described by the fixed-effect terms. Interaction terms of all covariates with time were included to test whether the influence changed over time. Finally, among HED youth, correlations between recent heavy alcohol and other substance use and both baseline mood and changes in mood with sustained abstinence were conducted. These analyses sought to evaluate the impact of intensity and frequency of recent alcohol and other substance use on mood states. Exploratory correlations were also conducted to evaluate the relationships between lifetime alcohol and other substance use, age of onset for use, and both baseline affect as well as affective changes with sustained abstinence.
Results
Baseline Mood Ratings
As hypothesized, in this non-clinical sample of HED and CON almost all affective ratings gathered via interview, self-report, and experience sampling methodologies were significantly correlated with one another at baseline with one exception: STAI-S was not correlated with either the mean or standard deviation of the mean percentage of negative affect youth reported via experience sampling procedures (see Table 2). While both measures queried participants’ affect, text messages were summarized over several days in participants’ natural environment, while the STAI-S measured momentary anxiety in the laboratory environment. All other measures were significantly related to one another; however, the sizes of the relationships among them indicate that unique variance is provided by each method, as well.
Table 2.
Baseline affective differences and correlations between interview, self-report, and experience sampling for CON (n = 26) and HED youth (n = 39)
| T-Test | Correlations (N = 65) | ||||
|---|---|---|---|---|---|
|
| |||||
| Controls | Heavy Episodic Drinkers | 1 | 2 | ||
| M (SD) | M (SD) | t (p) | r (p) | r (p) | |
| 1. Hamilton Total | 6.68 (5.23) | 10.74 (10.21) | −2.07 (.043) | ||
| 2. State Anxiety | 9.08 (5.91) | 12.08 (8.87) | −1.62 (.109) | 0.44 (.001) | |
| 3. % Texts Negative Affect | 15.87% (19.30%) | 29.10% (26.86%) | −2.07 (.044) | 0.45 (.001) | 0.23 (.107) |
At their first appointment, t-tests demonstrated that HED youth (approximately 6.5 days since their last binge drinking episodes) reported significantly higher levels of negative affect on interview and experience sampling summaries than CON, but not on self-report of state anxiety (STAI-S) in the laboratory setting (see Table 2). Additionally, HED youth had significantly more variability in their affective reports gathered via experience sampling than did CON youth.
Mood during period of sustained abstinence
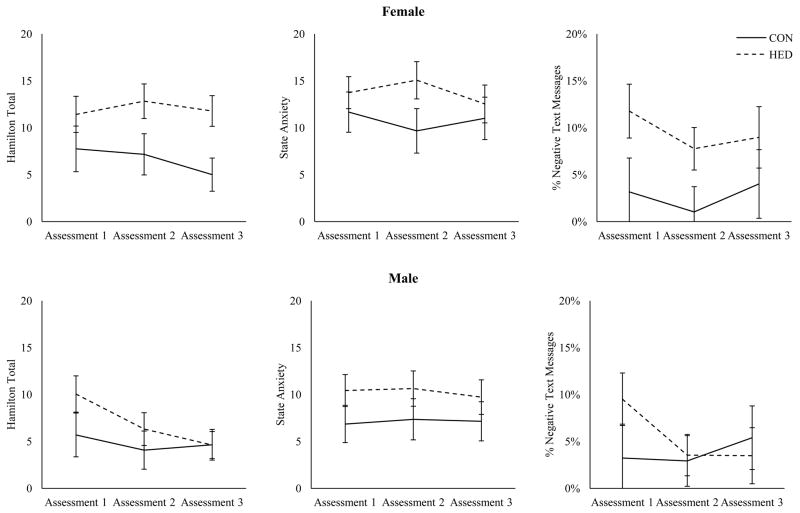
Linear mixed models examining group and sex differences in mood changes across a period of sustained abstinence were conducted for the combined Hamilton scales, state anxiety, and the percentage of text messages in which participants endorsed negative affect (see Table 3). Significant main effects were found for group and sex differences in youth’s affect on all three of these measures; HED reported more negative affect than CON participants, and females reported more negative affect than males. Contrary to hypotheses, significant changes in mood were not evident over the time of monitored abstinence. Visual inspection of the data suggests a potential pattern of gender difference among HED (see Figure 1). These interactions between group and gender, however, are not significant.
Table 3.
Mixed linear models examining differences in affect between male and female binge drinkers and controls across 4–6 weeks of sustained abstinence.
| Hamilton Total | State Anxiety | % Texts Negative Affect | |
|---|---|---|---|
| F (p) | F (p) | F (p) | |
| Intercept | 186.25 (<.001) | 322.65 (<.001) | 108.00 (<.001) |
| Group | 11.49 (.001) | 6.90 (.009) | 4.54 (.035) |
| Assessment | 1.37 (.258) | 0.11 (.899) | 0.12 (.886) |
| Sex | 9.44 (.002) | 9.44 (.002) | 4.31 (.040) |
| Group × Assessment | 0.04 (.962) | 0.31 (.735) | 0.23 (.795) |
| Group × Sex | 2.03 (.156) | 0.00 (.952) | 3.52 (.063) |
| Assessment × Sex | 0.57 (.567) | 0.04 (.957) | 0.39 (.675) |
| Group × Assessment × Sex | 0.97 (.382) | 0.23 (.795) | 0.13 (.878) |
Figure 1.
Marginal means for male and female youth’s report of negative affect across three assessments (4–6 weeks of monitored abstinence). Error bars indicate standard error.
Mood and Substance Use
To examine the relationship between prior alcohol/substance use and mood during sustained abstinence, we correlated all affective measures with the frequency and intensity of use prior to study intake among HED youth. At intake, HED who reported more lifetime experience of alcohol withdrawal symptoms also endorsed more negative affect on the Hamilton (r = .36, p < .05). HED with more experience using illicit substances other than alcohol and marijuana also reported more negative affect (Hamilton Total: r = .50, p < .01; STAI-S, r = .36, p < .05). Lifetime marijuana use was not significantly correlated with affective measures (p’s = .11 – .68).
To determine if recent and lifetime alcohol and other substance use history was associated with changes in mood with sustained abstinence, we subtracted negative affect scores at the third assessment from scores reported at the first assessment (positive scores indicate reduction in negative affect). As noted in Table 4, heavier recent drinking was associated with larger reductions in negative affect, but not reductions in state anxiety. Exploratory analyses demonstrated that lifetime history of alcohol and other drug use was weakly (non-significantly) associated with both reduced negative affect and state anxiety, but marijuana use was not associated with either. Additionally, negative correlations were found between age of first use (alcohol binge and marijuana) and reductions in state anxiety, but only marijuana was associated with other measures of negative affect. This indicates that individuals who began binge drinking and smoking marijuana at younger ages showed larger reductions in state anxiety with sustained abstinence.
Table 4.
Correlations between alcohol and substance use, age of first binge/use and changes in mood with 4–6 weeks of sustained abstinence.
| Δ Hamilton Total (n = 32) | Δ STAI-S (n = 33) | Δ % Texts Negative Affect (n = 28) | |
|---|---|---|---|
| Recent Substance Use (45 days) | |||
| Drinking days | 0.31† | 0.02 | 0.29 |
| Heavy drinking days | 0.33† | −0.03 | 0.28 |
| Max drinks/drinking day | 0.14 | 0.12 | 0.39* |
| Total # Drinks | 0.33† | 0.01 | 0.42* |
| Binge drinking (3 months) | 0.13 | 0.10 | 0.33† |
| Marijuana use days | −0.04 | 0.09 | 0.21 |
| Other drug use days | 0.08 | 0.08 | −0.06 |
| Lifetime Substance Use | |||
| Alcohol | −0.07 | 0.04 | 0.36† |
| Drunk | 0.22 | 0.33† | 0.36† |
| Marijuana | 0.09 | 0.17 | 0.15 |
| Other Drugs | 0.32† | 0.31† | 0.09 |
| High | 0.20 | 0.18 | 0.16 |
| Age of First Use | |||
| Binge | 0.07 | −0.38* | −0.14 |
| Marijuana | −0.24 | −0.38* | −0.42* |
| Other Drugs | −0.14 | −0.67** | −0.16 |
| (n = 18) | (n = 18) | (n = 16) | |
p = .05–.10;
p < .05,
p < .01
Discussion
To our knowledge, this is the first study to utilize multiple methodologies in both the laboratory (structured interview and self-report) and the natural environment (text messaging) to document mood fluctuations in relation to abstinence from alcohol in a community sample of adolescents abstaining following recent heavy episodic drinking. Overall we found that, consistent with our hypotheses, youth with extensive histories of lifetime and recent heavy episodic drinking evidenced poorer mood states across assessments and methodologies at baseline (1–2 weeks). As has been reported in the literature, adolescent girls reported more negative mood states than their male counterparts across assessments (Larson et al., 2002). Among HED youth, negative mood was associated with more frequent lifetime experience of hangover or alcohol withdrawal symptoms and more frequent use of illicit substances other than marijuana, but no significant relationships were found between baseline mood and marijuana use.
Contrary to hypotheses, changes in affect with sustained abstinence over time were not consistently demonstrated in linear mixed models. If higher levels of negative affect among HED result from alcohol exposure, these results may indicate that HED youth engaging in this heightened level of alcohol use require more than 4–6 weeks of abstinence to experience amelioration in negative affect. Alternatively these results might support hypotheses that some portion of the reported negative mood preceded alcohol and substance use and the higher rates of negative affect are reflective of internalizing symptoms present prior to heavy alcohol use. Among HED, however, higher intensity alcohol use prior to intake was related to greater changes in negative affect reported via experience sampling after 4–6 weeks of abstinence. Earlier age of onset of alcohol and other substance use was also related to greater changes in state anxiety and negative affect reported via experience sampling. In combination, these findings indicate that youth with heavier and more extensive alcohol and substance use experience may be more responsive to amelioration in negative affect with sustained abstinence. Alternatively, affective improvement at the end of study participation may also reflect youth’s positive emotions regarding reaching the end of their commitment to the project, including monitored abstinence and their freedom to return to drinking and drug use. Due to the small sample size for the current study, however, these findings are quite preliminary and require replication.
While male and female youth differed in their mood ratings, sample size limited the power of our analyses to detect significant interactions between group membership and sex. Graphed marginal means indicated, however, that girls experienced more negative affective states and that HED girls did not demonstrate affective improvement during the course of the study while HED boys reported improvements in mood after several weeks of abstinence. This improvement in mood among males suggests that at least a portion of the negative mood states they experienced reflected the impact of recent heavy episodic drinking. Gender differences in pattern of affective response during abstinence may indicate that negative affective states are slower to improve with sustained abstinence for girls. Alternatively, these differences might indicate increased levels of negative affect among girls that predated heavy alcohol use (Poulin et al., 2005), or may reflect a gender related difference in response style (Schwartz and Koenig, 1996). Future research is necessary to support these trends in a larger sample of heavy drinking adolescents. If replicated, these results are consistent with previous evidence that alcohol use can have a more deleterious effect on females than males (Mann et al., 2005).
Limitations
While the findings described here demonstrate the value of multimethod assessments of youth during early abstinence, there are several limitations that must be considered. As noted above, the primary limitation of this study was that our sample size was not sufficient to fully explore the impact of various personal characteristics on reductions in negative affect with abstinence, or increases in negative affect subsequent to youth’s return to heavy alcohol use. Additionally, this sample was selected to answer specific questions regarding how heavy episodic drinking relates to adolescent psychosocial functioning, as well as how that psychosocial functioning changes with sustained abstinence. As a result, the level of drinking reported by these youth was considerably higher than the adolescent population overall and consequently the results reported here may not generalize to youth with more normative drinking patterns.
Although youth with a history of affective disorders were excluded from study, we do not have information regarding participant’s affective state prior to the onset of their alcohol use. These personal characteristics may have assisted in determining the relative impact of youth’s premorbid affective styles and subsequent alcohol use on (a) mood state at intake and (b) amelioration of negative affect with sustained abstinence. Additionally, while we did utilize several different forms of assessment that were feasible in this adolescent sample, all of these measures relied on adolescents’ self-report. This is a strength of the study in that youth are more aware of their internal affective state than observers, but the veracity of their report may have been impacted by social desirability or expectation bias. Parent, peer, or observer ratings may have provided additional valuable information with reduced bias.
Implications & Future Directions
Consistent with previous literature, heavy drinking youth demonstrated heightened levels of negative affect when compared to demographically-matched peers, both in the laboratory and in their daily lives. Hypothesized improvements with sustained abstinence, however, were not supported in the current sample. While sample size limited our ability to detect smaller changes over time or elaborate on potential sex differences in mood improvement, it is also possible that youth at this age or level of alcohol experience require longer periods of time to demonstrate the improvements in mood that have been shown in adults (Brown and Schuckit, 1988). Additionally, this sample included youth that were not seeking or receiving any treatment that would actively target mood improvement. As negative affect is associated with higher alcohol and substance use and relapse in both adults (Breese et al., 2005; Sinha, 2007) and adolescents (Cornelius et al., 2003; Hussong et al., 2001), enhanced understanding of both naturally-occurring and treatment-enhanced changes in affective response during early and sustained abstinence is necessary for improving prevention and treatment programs designed to promote adolescent decision-making and reduce relapse risk among at-risk youth. The current study points to sex-specific processes that may provide valuable information towards meeting these goals.
Acknowledgments
Supported by the following NIAAA grants and fellowships: R21 AA017321 (PI: S. Brown) and T32 AA013525 (Fellow: N. Bekman; PI: E. Riley)
References
- Abe K, Suzuki T. Prevalence of some symptoms in adolescence and maturity: social phobias, anxiety symptoms, episodic illusions and ideas of reference. Psychopathology. 1986;19:200–205. doi: 10.1159/000284448. [DOI] [PubMed] [Google Scholar]
- Abrantes AM, Brown SA, Tomlinson K. Psychiatric comorbidity among inpatient substance abusing adolescents. J Child Adoles Subst. 2004;13:83–101. [Google Scholar]
- Addington D, Addington J, Maticka-Tyndale E, Joyce J. Reliability and validity of a depression rating scale for schizophrenics. Schizophr Res. 1991;6:201–208. doi: 10.1016/0920-9964(92)90003-n. [DOI] [PubMed] [Google Scholar]
- Anderson KG, Ramo DE, Schulte MT, Cummins K, Brown SA. Impact of relapse predictors on psychosocial functioning of SUD youth one year after treatment. Subst Abuse. 2008;29:97–105. doi: 10.1080/08897070802093411. [DOI] [PubMed] [Google Scholar]
- Arnett J. Adolescent storm and stress, reconsidered. Am Psychol. 1999;54:317–326. doi: 10.1037//0003-066x.54.5.317. [DOI] [PubMed] [Google Scholar]
- Bekman NM, Anderson KG, Trim RS, Metrik J, Diulio AR, Myers MG, Brown SA. Thinking and drinking: Alcohol-related cognitions across stages of adolescent alcohol involvement. Psychol Addict Behav. 2011;25:415–425. doi: 10.1037/a0023302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bekman NM, Cummins K, Brown SA. Affective and personality risk and cognitive mediators of initial adolescent alcohol use. J Stud Alcohol Drugs. 2010;71:570–580. doi: 10.15288/jsad.2010.71.570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brady KT, Back SE, Waldrop AE, McRae AL, Anton RF, Upadhyaya HP, Saladin ME, Randall PK. Cold pressor task reactivity: predictors of alcohol use among alcohol dependent individuals with and without comorbid posttraumatic stress disorder. Alcohol Clin Exp Res. 2006;30:938–946. doi: 10.1111/j.1530-0277.2006.00097.x. [DOI] [PubMed] [Google Scholar]
- Breese GR, Chu K, Dayas CV, Funk D, Knapp DJ, Koob GF, Le DA, O’Dell LE, Overstreet DH, Roberts AJ, Sinha R, Valdez GR, Weiss F. Stress enhancement of craving during sobriety: a risk for relapse. Alcohol Clin Exp Res. 2005;29:185–195. doi: 10.1097/01.alc.0000153544.83656.3c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown SA, Vik PW, Patterson TL, Grant I, Schuckit MA. Stress, vulnerability and adult alcohol relapse. J Stud Alcohol. 1995a;56:538–545. doi: 10.15288/jsa.1995.56.538. [DOI] [PubMed] [Google Scholar]
- Brown SA, Inaba RK, Gillin C, Schuckit MA, Stewart MA, Irwin MR. Alcoholism and affective disorder: clinical course and depressive symptoms. Am J Psychiat. 1995b;152:45–52. doi: 10.1176/ajp.152.1.45. [DOI] [PubMed] [Google Scholar]
- Brown SA, Schuckit MA. Changes in depression among abstinent alcoholics. J Stud Alcohol. 1988;49:412–417. doi: 10.15288/jsa.1988.49.412. [DOI] [PubMed] [Google Scholar]
- Brown SA, Tapert SF, Granholm E, Delis DC. Neurocognitive functioning of adolescents: effects of protracted alcohol use. Alcohol Clin Exp Res. 2000;24:164–171. [PubMed] [Google Scholar]
- Brown SA, Myers MG, Mott MA, Vik PW. Correlates of success following treatment for adolescent substance abuse. Appl Prev Psychol. 1994;3:61–73. [Google Scholar]
- Brown SA, Myers MG, Lippke L, Tapert SF, Stewart DG, Vik PW. Psychometric evaluation of the Customary Drinking and Drug Use Record (CDDR): a measure of adolescent alcohol and drug involvement. J Stud Alcohol. 1998;59:427–438. doi: 10.15288/jsa.1998.59.427. [DOI] [PubMed] [Google Scholar]
- Cooney NL, Litt MD, Morse PA, Bauer LO, Gaupp L. Alcohol cue reactivity, negative-mood reactivity, and relapse in treated alcoholic men. J Abnorm Psychol. 1997;106:243–250. doi: 10.1037//0021-843x.106.2.243. [DOI] [PubMed] [Google Scholar]
- Cornelius JR, Maisto SA, Pollock NK, Martin CS, Salloum IM, Lynch KG, Clark DB. Rapid relapse generally follows treatment for substance use disorders among adolescents. Addict Behav. 2003;28:381–386. doi: 10.1016/s0306-4603(01)00247-7. [DOI] [PubMed] [Google Scholar]
- Daughters SB, Reynolds EK, MacPherson L, Kahler CW, Danielson CK, Zvolensky M, Lejuez Distress tolerance and early adolescent externalizing and internalizing symptoms: the moderating role of sex and ethnicity. Behav Res Ther. 2009;47:198–205. doi: 10.1016/j.brat.2008.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donovan JE. Estimated blood alcohol concentrations for child and adolescent drinking and their implications for screening instruments. Pediatrics. 2009;123:e975–981. doi: 10.1542/peds.2008-0027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellickson PL, Tucker JS, Klein DJ. Ten-year prospective study of public health problems associated with early drinking. Pediatrics. 2003;111:949–955. doi: 10.1542/peds.111.5.949. [DOI] [PubMed] [Google Scholar]
- Falk DE, Yi H, Hilton ME. Age of onset and temporal sequencing of lifetime DSM-IV alcohol use disorders relative to comorbid mood and anxiety disorders. Drug Alcohol Depen. 2008;94:234–245. doi: 10.1016/j.drugalcdep.2007.11.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fava GA, Kellner R, Munari F, Pavan L. The Hamilton Depression Rating Scale in normal and depressives. Acta Psychiatrica Scandinavica. 1982;66:26–32. doi: 10.1111/j.1600-0447.1982.tb00911.x. [DOI] [PubMed] [Google Scholar]
- Glenn SW, Parsons OA. Prediction of resumption of drinking in post-treatment alcoholics. Int J Addict. 1991;26:237–254. doi: 10.3109/10826089109053186. [DOI] [PubMed] [Google Scholar]
- Grant BF, Goldstein RB, Chou SP, Huang B, Stinson FS, Dawson DA, Saha TD, Smith SM, Pulay AJ, Pickering RP, Ruan WJ, Compton WM. Sociodemographic an psychopathologic predictors of first incidence of DSM-IV substance use, mood and anxiety disorders: results from the Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions. Mol Psychiatr. 2009;14:1051–1066. doi: 10.1038/mp.2008.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamilton M. Rating depressive patients. J Clin Psychiat. 1980;41:21–24. [PubMed] [Google Scholar]
- Hamilton M. The assessment of anxiety states by rating. Brit J Med Psychol. 1959;32:50–55. doi: 10.1111/j.2044-8341.1959.tb00467.x. [DOI] [PubMed] [Google Scholar]
- Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hill KG, White HR, Chung IJ, Hawkins JD, Catalano RF. Early adult outcomes of adolescent binge drinking: person- and variable-centered analyses of binge drinking trajectories. Alcohol Clin Exp Res. 2000;24:892–901. [PMC free article] [PubMed] [Google Scholar]
- Hogue A, Henderson CE, Dauber S, Barajas PC, Fried A, Liddle HA. Treatment adherence, competence, and outcome in individual and family therapy for adolescent behavior problems. J Consult Clin Psychol. 2008;76:544–555. doi: 10.1037/0022-006X.76.4.544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hollingshead AB. Two-factor index of social position. New Haven, CT: Yale University Press; 1965. [Google Scholar]
- Hussong AM, Hicks RE, Levy SA, Curran PJ. Specifying the relations between affect and heavy alcohol use among young adults. J Abnorm Psychol. 2001;110:449–461. doi: 10.1037//0021-843x.110.3.449. [DOI] [PubMed] [Google Scholar]
- Larson RW, Moneta G, Richards M, Wilson S. Continuity, stability and change in daily emotional experience across adolescence. Child Dev. 2002;73:1151–1165. doi: 10.1111/1467-8624.00464. [DOI] [PubMed] [Google Scholar]
- Lejuez CW, Kahler CW, Brown RA. A modified computer version of the Paced Auditory Serial Addition Task (PASAT) as a laboratory-based stressor. Behav Ther. 2003;26:290–293. [Google Scholar]
- Mann K, Ackermann K, Croissant B, Mundle G, Nakovics H, Diehl A. Neuroimaging of gender differences in alcohol dependence: Are women more vulnerable? Alcohol Clin Exp Res. 2005;29:896–901. doi: 10.1097/01.alc.0000164376.69978.6b. [DOI] [PubMed] [Google Scholar]
- Maier W, Buller R, Philipp M, Heuser I. The Hamilton Anxiety Scale: reliability, validity, and sensitivity to change in anxiety and depressive disorders. J Affect Disorders. 1988;14:61–68. doi: 10.1016/0165-0327(88)90072-9. [DOI] [PubMed] [Google Scholar]
- McCarty CA, Ebel BE, Garrison MM, DiGiuseppe DL, Christakis DA, Rivara FP. Continuity of binge and harmful drinking from late adolescence to early adulthood. Pediatrics. 2004;114:714–719. doi: 10.1542/peds.2003-0864-L. [DOI] [PubMed] [Google Scholar]
- Miller JW, Naimi TS, Brewer RD, Jones SE. Binge drinking and associated health risk behaviors among high school students. Pediatrics. 2007;119:76–85. doi: 10.1542/peds.2006-1517. [DOI] [PubMed] [Google Scholar]
- Naimi TS, Brewer RD, Mokdad A, Denny C, Serdula MK, Marks JS. Binge drinking among U.S. adults. JAMA: J Am Med Assoc. 2003;289:70–75. doi: 10.1001/jama.289.1.70. [DOI] [PubMed] [Google Scholar]
- Poulin C, Hand D, Boudreau B, Santor D. Gender differences in the association between substance use and elevated depressive symptoms in a general adolescent population. Addiction. 2005;100:525–535. doi: 10.1111/j.1360-0443.2005.01033.x. [DOI] [PubMed] [Google Scholar]
- Ravert RD, Calix SI, Sullivan MJ. Research in brief: using mobile phones to collect daily experience data from college undergraduates. J Coll Student Dev. 2010;51:343–351. [Google Scholar]
- Rowe CL, Liddle HA, Greenbaum PE, Henderson CE. Impact of psychiatric comorbidity on treatment of adolescent drug abusers. J Subst Abuse Treat. 2004;26:129–140. doi: 10.1016/S0740-5472(03)00166-1. [DOI] [PubMed] [Google Scholar]
- Schwartz JA, Koenig LJ. Response styles and negative affect among adolescents. Cognitive Ther Res. 1996;20:13–36. [Google Scholar]
- Sinha R, Garcia M, Paliwal P, Kreek MJ, Rounsaville BJ. Stress-induced cocaine craving and hypothalamic-pituitary-adrenal responses are predictive of cocaine relapse outcomes. Arch Gen Psychiatry. 2006;63:324–331. doi: 10.1001/archpsyc.63.3.324. [DOI] [PubMed] [Google Scholar]
- Sinha R. The role of stress in addiction relapse. Curr Psychiatry Rep. 2007;9:388–395. doi: 10.1007/s11920-007-0050-6. [DOI] [PubMed] [Google Scholar]
- Sobell LC, Maisto SA, Sobell MB, Cooper AM. Reliability of alcohol abusers’ self-reports of drinking behavior. Behav Res Ther. 1979;17:157–160. doi: 10.1016/0005-7967(79)90025-1. [DOI] [PubMed] [Google Scholar]
- Spielberger CD. State–Trait Anxiety Inventory (Form Y) Palo Alto, CA: Consulting Psychologists Press; 1983. [Google Scholar]
- Spielberger CD, Diaz-Guerrero R. Cross-cultural anxiety. Washington, DC: Hemisphere/Wiley; 1976. [Google Scholar]
- Spielberger CD, Diaz-Guerrero R. Cross-cultural anxiety. Vol. 2. Washington, DC: Hemisphere/Wiley; 1983. [Google Scholar]
- Spielberger CD, Gorsuch RL, Lushene RE. State–Trait Anxiety Inventory for adults (Form X) Palo Alto, CA: Consulting Psychologists Press; 1970b. [Google Scholar]
- Spielberger CD, Spielberger CD, Gorsuch RL, Lushene RE. Manual for the State-Trait Anxiety Inventory. Palo Alto, CA: Consulting Psychologists Press; 1970a. [Google Scholar]
- Squeglia LM, Spadoni AD, Infante MA, Myers MG, Tapert SF. Initiating moderate to heavy alcohol use predicts changes in neuropsychological functioning for adolescent girls and boys. Psychol Addict Behav. 2009;23:715–722. doi: 10.1037/a0016516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomlinson KL, Cummins K, Brown SA. Social anxiety and onset of drinking in early adolescence. J Child Adoles Subst. doi: 10.1080/1067828X.2012.747994. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trajković G, Starčević V, Latas M, Leštarević M, Ille T, Bukumirić Z, Marinković J. Reliability of the Hamilton Rating Scale for Depression: A meta-analysis over a period of 49 years. Psychiatry Res. 2011;189:1–9. doi: 10.1016/j.psychres.2010.12.007. [DOI] [PubMed] [Google Scholar]
- Winward JL, Cummins K, Bekman NM, Hanson KL, Wagner C, Lejuez CW, Brown SA. Changes in distress tolerance among heavy drinking adolescents during sustained abstinence. (under review) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu P, Hoven CW, Bird H, Moore RE, Cohen P, Alegria M, Dulcan MK, Goodman SH, Horwitz SM, Lichtman JH, Narrow WE, Rae DS, Regier DA, Roper MT. Depressive and disruptive disorders and mental health service utilization in children and adolescents. J Am Acad Child Psy. 1999;38:1081–1090. doi: 10.1097/00004583-199909000-00010. [DOI] [PubMed] [Google Scholar]
- Wurst FM, Dresen S, Allen JP, Wiesbeck G, Graf M, Weinmann W. Ethyl sulphate: a direct ethanol metabolite reflecting recent alcohol consumption. Addiction. 2006;101:204–211. doi: 10.1111/j.1360-0443.2005.01245.x. [DOI] [PubMed] [Google Scholar]