Abstract
Background
The increasing cost of providing health care is a national concern. Healthcare spending related to providing hospital care is one of the primary drivers of healthcare spending in the United States. Adoption of advanced medical technologies accounts for the largest percentage of growth in healthcare spending in the United States when compared with other developed countries. Within the specialty of orthopaedic surgery, a variety of implants can result in similar outcomes for patients in several areas of clinical care. However, surgeons often do not know the cost of implants used in a specific procedure or how the use of an implant or technology affects the overall cost of the episode of care.
Questions/purposes
The purposes of this study were (1) to describe physician-led processes for introduction of new surgical products and technologies; and (2) to inform physicians of potential cost savings of physician-led product contract negotiations and approval of new technology.
Methods
We performed a detailed review of the steps taken by two centers that have implemented surgeon-led programs to demonstrate responsibility in technology acquisition and product procurement decision-making.
Results
Each program has developed a physician peer review process in technology and new product acquisition that has resulted in a substantial reduction in spending for the respective hospitals in regard to surgical implants. Implant costs have decreased between 3% and 38% using different negotiating strategies. At the same time, new product requests by physicians have been approved in greater than 90% of instances.
Conclusions
Hospitals need physicians to be engaged and informed in discussions concerning current and new technology and products. Surgeons can provide leadership for these efforts to reduce the cost of high-quality care.
Introduction
The increasing cost of providing health care is a national concern. The expenditures for health care are estimated to equal 17% of the GDP in the United States [17]. The increasing cost of health care is recognized to be a multifaceted problem, and many potential strategies to control costs have been suggested [15, 17, 18].
Zuckerman et al. [24] in 1994 reported physician participation in value-analysis committees but this effort related to one specific procedure. In 2006 the University of California, San Francisco (UCSF) introduced a Healthcare Technology Assessment Program [15]. The program was unique in that it was a physician-led process. Previous literature cites references to hospital processes that address implant costs. Hospitals emphasize the need to engage physicians in the process, because the physicians are the end-users of the implant or technology [2, 3, 8, 23]. The physician-led process focusing on procurement of new technology or equipment in a variety of clinical areas is a recent development in health care.
Orthopaedic surgery has several areas of clinical care where a variety of implants can be used in a surgical procedure and result in similar outcomes for patients. Adult hip and knee arthroplasty are examples of such procedures. Primary THA for the treatment of end-stage arthritis is recognized as a cost-effective medical intervention [21], yet surgeons often do not know the cost of implants used in a specific procedure or how the use of an implant or technology affects the overall cost of the episode of care. Similarly, the cost information hospitals provide to their physicians through service line analyses often includes more than the actual cost of the implant [23]. The cost may include other supplies, indirect or overhead expenditures, and operating room time. The aggregation of these costs and others makes it difficult for the surgeon to understand the impact of their decision to use a specific implant on the cost of the episode of care. The cost accounting system may also take into account the revenue that follows the use of the implant and ultimately leads to the financial margin resulting from the episode of care; it is often this hospital margin that determines whether a cost reduction effort is viewed as successful [1, 23]. The positive margin is influenced by the payer mix and any change in reimbursement can quickly cause a positive margin to become negative. Therefore, a gap exists in providing data that are easily understandable and actionable information for surgeons. Regardless of margin contribution, it is critical that surgeons understand the actual cost drivers of their procedures.
The purpose of this work is to provide an overview of how two institution-implemented systems addressed three objectives: (1) technology/product approval; (2) product consolidation; and (3) analysis of process and variation of care.
Materials and Methods
This work provides an overview of development and implementation of physician-led processes to manage costs of implant and technology acquisitions in two unique centers.
Organization at Vanderbilt University Medical Center
Vanderbilt University Medical Center implemented a facility-based technology assessment committee (the Medical Economic Outcome Committee) in August 2008. The committee’s mission and vision statement is: “a clinician-driven process that standardizes and utilizes evidence-based, clinically sound, financially responsible methodologies for introduction or consolidation of new supplies, devices and technology within the University Medical Center to provide the highest quality of patient care.” Three committees have been formed, one comprised of surgical subspecialties and another comprised of radiology, cardiology, and cardiovascular subspecialists and a laboratory medicine committee from both the adult and pediatric facilities as well as senior administrators; physician representatives were recruited by physician leaders or were nominated by surgical chairs. The intent was to have physicians who were active clinically and understood evidence-based medicine processes.
Technology/Product Approval
The goals as outlined by the process were clinical and financial. Clinical goals included facilitating the adoption of safe and efficacious healthcare technologies to improve patient care, developing a capital assessment process that was transparent as well as data- and strategy-driven, and finding new and innovative ways to impact healthcare delivery and costs. Financial goals consisted of evaluating the cost-effectiveness and financial impact of new healthcare technologies and physician preference items, empowering clinicians to standardize procedures and improve hospital supply chain costs, identifying reimbursement for new healthcare technologies before their introduction, improving the institution’s capital budget, and using benchmark data to compare financial outcomes (see “Appendix 1”).
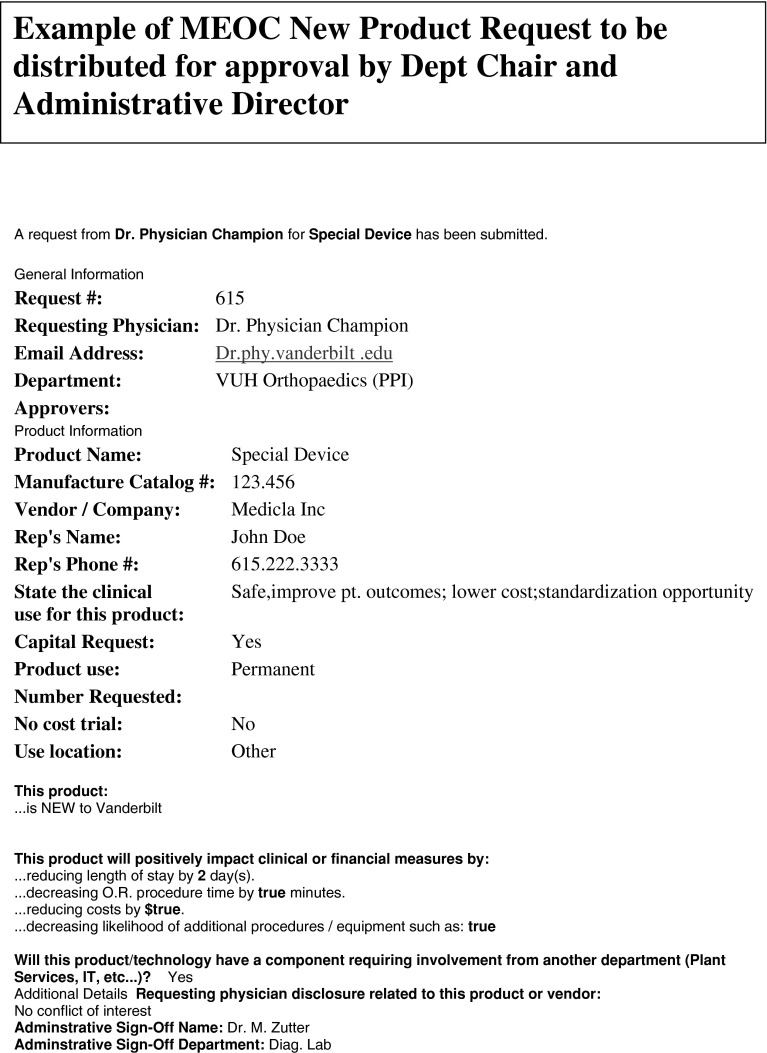
Each committee meets monthly and consists of 10 physicians and six administrators and/or supply chain officers. New technology requests are submitted through an online electronic form as either trial or permanent requests. A conflict of interest disclosure statement is present on the form and is required to be completed. However, if the physician does disclose a conflict, it does not preclude him or her from requesting the product (see “Appendix 2”). For a trial request, a short description of the Physician Preference Items (PPIs) is included as well as the physician champion’s input on its cost-benefit and potential quality improvement outcomes. This information is circulated to committee members who may approve a one-time or short-duration request of a trial product. Caveats are that the product is FDA-approved and cost-neutral with no negative contractual effects on existing contracts. If a physician requests permanent access to a PPI item before or after a trial request, more in-depth information is acquired from the physician champion. A physician will present their perception of the improvements in the quality or advantages of the product. Pertinent peer review articles are distributed before the committee meeting. Information is also obtained, when available, from external sources that have the capability of grading the technology based on review of scientific publications. The supply chain analytics team also provides information on potential use and the effect on contribution margin and net margin of a new technology implementation.
The intent is that the financial metrics are not the only or most important metric. The committee considers the financial impact obviously, but also considers the marketing advantages, innovation advantages, quality patient outcomes, and research potential. The “physician champion” presents information on potential marketing advantages by discussing current local and/or national utilization and how access to this product might impact volume. Innovation, outcomes, and research are assessed by colleagues on the committee who are familiar with the subject matter and/or peer review literature is provided to all voting members 1 week before the meeting. External evaluation is at this time available from either ECRI (www.ecri.org) or Advisory Board (www.advisory.com).
After a physician champion’s presentation is concluded, there is an open exchange of questions of the committee members to the physician champion. No industry representatives are permitted to be present or to present. After the physician champion has presented, the committee has a closed-door discussion and vote on product acceptance with a majority required for adoption of new technology or PPI. In the event one of the committee members has disclosed a conflict with the particular company being presented, the committee member can participate in the discussion but must recuse him- or herself from the final vote. The committee may grant full approval, reject the proposal, or approve with stipulations. Stipulations may include temporary approval for 6 months to 1 year with a requirement the requestor return to the committee to present clinical outcomes and have the product reevaluated. Another stipulation for approval may be that the product is cost-neutral and does not impact current contracting Product Consolidation.
Vanderbilt’s facility-based technology assessment committee has also undertaken standardization of PPIs to improve pricing, which has translated to improved contribution margins and net margins to the institution. The goal is that as net margins increase, the institution will have more funds available for investments in programs and/or capital acquisition.
Focused initiatives of physician preference items have been undertaken in surgical products including endomechanical stapling devices, orthopaedic joint arthroplasty, spine internal fixation, trauma internal fixation, cardiac rhythm management implants, drug-eluting stents, and cardiac valve implants (Table 1). The process selected for contract negotiation varied on the product category, physician preferences, existing contracts, and benchmark information related to potential opportunity. Endomechanical stapling devices were approached using an either/or vendor A or vendor B. After trial of several products by physicians who would be impacted, a single-source vendor was approved and continues to be under contract. General surgeons retrospectively performed an internal quality improvement case-control review of endomechnical staples to assess for any changes in complications and they saw no increase in length of stay, transfusion requirements, or reoperations in a select patient population with isolated intestinal stapling, which resulted in a savings of USD 750,000 for the 3-year contract. Items that were not available by the selected vendor and were without equivalent were able to be purchased at a higher negotiated price.
Table 1.
The areas of cost reduction and the strategy used are indicated for Vanderbilt University Hospital*
| Fiscal year | Project name | Strategy used | Total spent | Savings | Percentage |
|---|---|---|---|---|---|
| 2009 | Endo-Mechanical | Standardization | USD 1,262,545 | USD 171,544 | 14 |
| 2009 | Total Joints | Matrix pricing | USD 6,703,193 | USD 2,561,991 | 38 |
| 2009 | Cardiac Rhythm Management | Matrix pricing | USD 11,790,232 | USD 1,590,396 | 13 |
| 2009 | Drug Eluting Stents | Vendor consolidation | USD 4,825,400 | USD 454,044 | 9 |
| 2010 | Spine Implants | Matrix pricing | USD 7,054,266 | USD 1,895,110 | 27 |
| 2011 | Closure Devices | Standardization | USD 1,222,286 | USD 42,022 | 3 |
| 2011 | Interventional cardiology | Standardization | USD 6,381,054 | USD 1,111,050 | 17 |
| 2011 | Cardiac Surgery | Matrix pricing | USD 2,368,000 | USD 60,280 | 3 |
| 2011 | Transcription | Renegotiation | USD 3,026,144 | USD 293,673 | 10 |
| 2011 | Trauma | Request for proposal | USD 6,333,804 | USD 1,071,479 | 17 |
| 2011 | MESH | Vendor consolidation | USD 1,875,314 | USD 604,435 | 32 |
| 2011 | Oral Care | Renegotiation | USD 543,771 | USD 149,253 | 27 |
| 2011 | Reference Lab Phase I | Request for proposal | USD 2,518,306 | USD 176,283 | 7 |
* The total spent and savings achieved for each area is provided since the beginning of the Medical Economic Outcome Committee process.
Total joint arthroplasty implants maintained physician choice while achieving substantial savings. Strong physician support of the process led to “matrix” pricing. Matrix pricing refers to agreement on a set price for products with a similar function from a variety of vendors. This can also be referred to as a price per item strategy. Primary joints were negotiated at a set price. Any vendor was allowed to provide implants at this set price. Advice on negotiating this set price was obtained from an outside consultant who had national data on “like” institutions and provided input on a range of negotiating prices that would be commensurate with current market pricing. Sex-specific and “high-flex” knees were negotiated to standard pricing after published prospective data showed no major advantage with these implants.
A similar process was undertaken for spine implants. The actual total number of vendors increased from four to nine spine vendors who all met bid requirements. The vendor with the largest market share (48%) before this process would not meet contract terms and was hence excluded for a 90-day period of time. Again, strong physician support and leadership were essential to accomplishing this. After the 90 days, the vendor was allowed to come in at the prior negotiated contract pricing but attempted to insert nondisclosure language into the contract, which was rebuked by the hospital and ultimately crafted to protection of information while allowing for ongoing benchmarking. It should be noted that the prior market share has not returned to that vendor in this time period. At the end of the 3-year contract we have now consolidated to three vendors based on surgeon practices and saved an additional USD 750,000 per year in implant cost based on current volume.
Cardiac rhythm management also undertook matrix pricing at the component-level strategy but took it one step further by implementing internal controls on the placement of one particular device based on clinical criteria determined by the physicians. Additionally, the institution realized an improvement in the pricing for trauma implants reducing the number of vendors from seven to two.
-
2)
Analysis of Process and Variation of Care
We have recently begun to use hospital clinical, product use, and financial data consolidated by MedAssets (www.medassets.com) in an information tool, Service Line Analytics. Med Assets is a for-profit company that is also affiliated with the institution as a collaborator for their Group Purchasing Organization (GPO). This tool allows clinicians and administrators to evaluate product use/cost, clinical outcomes (including length of stay, complications, blood use), and financial data (contribution margin and net margin). Each service line is actively being trained and is evaluating their opportunities for process, quality, or financial improvement. To continue this success, it will be necessary for the participating physicians to see tangible return institutional support in finances, research, or facilities. We do not have data on cost savings with this next phase of the process.
Organization at Duke University Medical Center
In 2010 Duke University Hospital instituted a Medical Staff Committee with a charge to evaluate Equipment, Devices, and Information Technology (EDIT) to be brought into the operating room (OR) environments. The Duke process was developed primarily to address the first goal of technology/product approval. In general, the OR EDIT process looks at requests for new items to be added to the OR supply chain with a substantial financial impact of USD 50,000 or more per year for the hospital. These might include upgrades to the next version of the existing implants, alternative implant systems for arthroplasty or other procedures, or novel technology not presently in the OR.
OR EDIT committee members consist of those individuals needed to make purchasing decisions at the time of the committee meeting in the majority of instances. The members include Vice-President for Perioperative Services at Duke University Hospital, Associate Chief Nursing Officer for Perioperative Services, Medical Director for Perioperative Services, CFO of Duke University Hospital, Chief of Clinical Engineering for Duke University Hospital, Chief of Procurement for Duke University Hospital, and Perioperative Services Procurement Officer along with physician representation from the Department of Anesthesiology and Critical Services of Cardiothoracic Surgery, General Surgery, Neurosurgery, and Orthopaedic Surgery. The committee is chaired by the surgeon who chairs the Perioperative Services Committee for Duke University Hospital. The physician members of the committee are considered key to the OR EDIT review process. Together the four specialties of Cardiothoracic Surgery, General Surgery, Neurosurgery, and Orthopaedic Surgery represent over 95% of all requests for new implants or technology that meet OR EDIT review criteria. Having physicians who can speak to the clinical importance of requested items is invaluable in the discussions. The goal is to have financial decision-makers and medical representation at the table for all product discussions meeting OR EDIT criteria for a review. All members of the committee vote on requested items.
OR EDIT instituted the following process changes: (1) all requests for new equipment, devices or implants, and information technology are submitted through use of a form jointly completed by the requesting physician and nurse manager for the surgeon’s service line. Forms submitted that are completed by the vendor are returned; (2) surgeons are asked to answer three primary questions: (a) Is the request to replace or add to current technology? (b) How many other surgeons will be impacted by this request? (c) Does the medical evidence support the request?
The request is evaluated by a team of OR and procurement staff who conducts an analysis that identifies existing contracts for similar items, reviews contract status with the vendor and price of requested items, and estimates case volume of use for the requested item. Requests that meet a critical financial threshold of USD 50,000 or greater are subjected to a more detailed financial analysis and OR EDIT review. This detailed analysis includes assessing the entire hospital cost of the episode of care associated with the procedure in question. The analysis takes into account the cost difference of the requested item when compared with similar items in addition to the projected impact on length of stay.
The response and feedback provided to the surgeon may vary depending on several factors. Equipment costing less than USD 5000, the threshold for capital equipment, will be reviewed based on medical value and costs. Items that reduce cost and improve patient outcomes are approved rapidly. Whenever possible, the lower cost new item will replace all older items with similar functionality. However, this replacement is often challenging because individual physician preferences have added many duplicative items to the inventory over time. This physician-centered approach needs to be tempered with the reality of limitations in storage of inventory in addition to the inherent challenges with inventory management of many different items that are used in similar cases throughout the OR. In response to increasing downward pressure on reimbursement, efficiency in the OR will become exceedingly important.
In many circumstances when it is unclear whether the technology will be an improvement, or when the case volume is unknown and therefore the financial impact is unknown, the implant or technology is approved on a trial basis for a set period of time. Trial periods vary in length from 1 to 6 months depending on the frequency of the procedures in question. After this trial period, the surgeon’s opinion of success of the trial is assessed along with the financial impact of the use of the item, increased or decreased OR time, and impact on length of stay when possible.
When the item is acted on by OR EDIT, the requesting physician is notified of the committee’s decision. This communication includes reference to the item requested, the actual cost of the requested item, and the estimated financial impact of the request. Once the item is approved by OR EDIT, the Duke University Health System procurement office negotiates the final contracted price for the approved item, establishes the patient charge, and arranges for stocking within the supply chain.
Beginning in September 2010, OR EDIT has approved over 50 new items into inventory while limiting the overall incremental impact to under USD 20,000. Currently there are over 20 items in trial use.
The second process managed through OR EDIT includes systemwide contracting for major categories of implants or technology. The procurement office uses national and regional benchmarking tools to identify opportunities to lower cost. An example of such an initiative was to lower the total cost for primary hip and knee arthroplasty prostheses. In this example, OR EDIT engaged key physician leaders in this area of specialty. The physicians review the variability in cost among different vendors at all hospitals within the health system. Using external benchmark data and evidence from the medical literature, the physicians work to categorize the implants from each vendor. The implants are designated into a standard or premium category. The premium category indicates there are special characteristics of the product or implant that warrant an increase in cost based on impact to patient outcome. Once this work is complete and a cost strategy is developed, the vendors receive a letter from the Chair of the OR EDIT Committee and the Chief Procurement Officer for the Health System explaining the new program and reinforcing the important role vendors have in supporting the surgeons while partnering with Duke to reduce cost. The letter includes a copy to all surgeons within the specialty who are involved in the project.
Results
Vanderbilt Experience
At Vanderbilt over a 2-year period, 92% of products that were presented were approved, 5% approved with stipulations, and 3% rejected (Fig. 1). If the physician champion is unhappy with the committee’s decision, a formal appeal may be filed. The appeal is filed with the steering committee, which oversees all committees. The steering committee is comprised of administrative leaders, the chairpersons of the committees, and institutional leaders. The steering committee will review an appeal, and if new information is available or there was a misperception of some kind, the steering committee can ask the chair of the respective committee to revisit the product at its next meeting. The steering committee will not overturn a committee’s decision, and a reversal of decision has to come from each committee. Since inception of this process, no decision has been overturned. Two decisions were appealed at a later date as a result of new information. These two appeals were returned to the respective committee for repeat consideration and the committee altered their initial decision based on the new information.
Fig. 1.
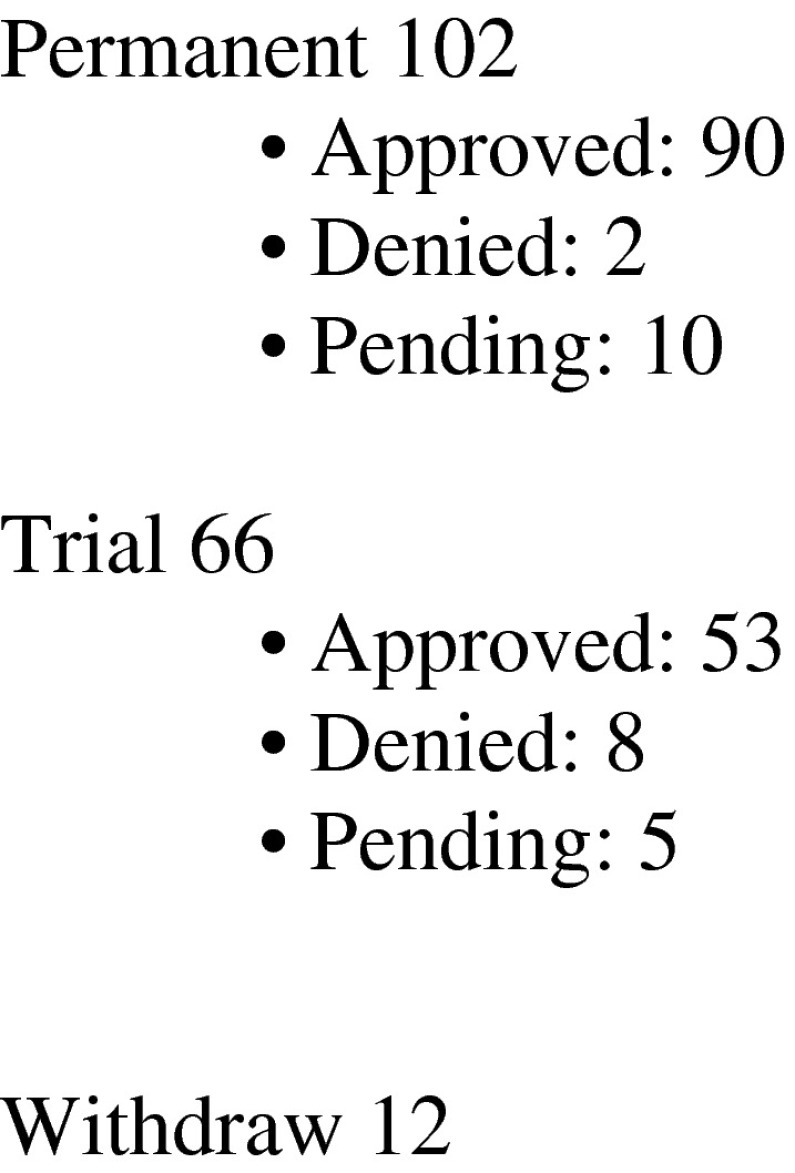
The volume of new product requests that required Medical Economic Outcome Committee review submitted over a 3-year period.
The system outlined here has been very beneficial to Vanderbilt University Medical Center in two ways. First, the institution has been able to achieve substantial savings in the mentioned categories. Prices have fallen 3% to 38% (Table 1) from initial costs, resulting in a total savings of greater than USD 8 million per year for the last 2 years. However, more importantly, it has also allowed for a collaborative and transparent approach on decision-making in the contracting and procurement process that did not previously exist. Development of this relationship has been key and has set the stage for the committees to engage in the next level of opportunities that will focus on use and peer-to-peer benchmarking.
Duke Experience
The implementation of the OR EDIT process at Duke has resulted in two outcomes. First is the establishment of a forum for surgeons who wish to add new technology. The second is a forum to standardize product and implants. The link between these two outcomes is important. The addition of new technology results in increased expense for these select surgical procedures, in our case approximately an increase of USD 50,000 for all added technology in the first year. However, the savings from implant standardization efforts substantially offset the added expense of new technology. Therefore, the decisions to add new technology can be supported by medical review and an overall fiscal argument of net savings overall through a responsible partnership between surgeons and administration.
At Duke, for costs for primary THA components across the three hospitals in the Duke University Health System, we found a range of less than USD 4000 to more than USD 9000 per case based on vendor and hospital. After implementation of this system, we now have a “Duke” price for primary hip and knee arthroplasty. This pricing strategy is a form of matrix pricing or price per item for hip and knee arthroplasty components. In this system, the majority of items is considered standard, and a small minority of items is approved as a premium product. All vendors who agree to participate have access to the Duke Health System hospitals. Surgeons have the freedom of choice of implants from vendors who participate in the program to allow the best care for their patients. We illustrate the cost savings achieved from OR EDIT and other related initiatives (Table 2).
Table 2.
The areas of cost reduction and the strategy used is indicated for the Duke University Health System
| Project name | Strategy used | Annual total spent | Savings | Percentage reduction In total spent |
|---|---|---|---|---|
| Endo‐Mechanical | Line item cost reduction | USD 7,300,000 | USD 400,000 | 5 |
| Total Joints | CAP price | USD 13,666,546 | USD 2,100,000 | 15 |
| Cardiac Rhythm Management | Matrix pricing | USD 13,088,936 | USD 933,007 | 7 |
| Drug Eluting Stents | Standardization | USD 1,739,925 | USD 200,000 | 11 |
| Spine Implants* (Hardware Only) | CAP price | USD 25,354,639 | USD 4,000,000 | 16 |
| Trauma | Line item cost reduction | USD 4,893,912 | USD 635,765 | 13 |
| MESH | Line item cost reduction and matrix | USD 1,949,923 | USD 213,231 | 11 |
| Heart Valves Rings | Line item cost reduction | USD 2,380,284 | USD 191,805 | 8 |
| Nerve Stimulation | Line item cost reduction | USD 2,577,154 | USD 210,000 | 8 |
| Kypho‐Vertebtal Plasty | Line item cost reduction | USD 681,062 | USD 102,718 | 15 |
| Negative wound pressure | Product conversion | USD 1,200,000 | USD 327,518 | 27 |
| EP Catheters and Accessories | Line item cost reduction and matrix | USD 4,100,000 | USD 235,000 | 6 |
| Bare Metal Stents | Line item cost reduction | USD 727,198 | USD 189,663 | 26 |
| Duke University Hospital System total | USD 79,659,579 | USD 9,738,707 | 12 |
The total spent and savings achieved for each area are provided; * savings achieved following establishing operating room Equipment, Devices, and Information Technology (OR EDIT). The remainder of savings reflects efforts through other procurement negotiations. These data allow a more complete comparison with Table 1.
Several important lessons have been learned from the work of standardizing implant systems that are applicable to any organization. They are: (1) key physicians who use the implants to be standardized must be engaged early and communicated with frequently; (2) a dedicated staff member should review the data with these key physicians individually. The number of components or products is often extensive, and descriptions are confusing at first review; (3) key physicians will need to identify the standard and premium categories of implants. Vendors will claim that a product has value beyond a standard product and therefore is entitled to a higher or premium price. The surgeons need to be able to apply evidence-based knowledge to support or refute the vendor’s claims. These differences should be communicated to procurement staff in a way that bridges the gap between procurement and manufacturer nomenclature (ie, part number and description) and clinical nomenclature (vacuum-irradiated highly crosslinked polyethylene liner). We have found it common that the procurement staff communicates with the vendor in a procurement nomenclature and the vendors respond with a clinical nomenclature. This sorting of implant categories is the single most important step and must be thoroughly vetted by the key physician leaders before sending to the vendors; (4) the leadership of the physician-led process should make contact with the vendor’s senior sales force before beginning communication around pricing. This important step in the process is critical to the initiative’s success because it reinforces with the vendor that physicians are aligned and leading the initiative; (5) the key physicians must agree on the number or mix of vendors required to care for the patient population in question; (6) the strategy must be shared with all surgeons who will use the implants. Key physician leaders engage all surgeons who use the implants. At hospitals where a mix of community surgeons and academic surgeons practice, the hospital administrator is also involved in discussions with those surgeons who are not in the same practice as the key physician leaders. The surgeons are asked to keep cost information confidential during this process and sign a confidentiality agreement; and (7) the new agreement is submitted to vendors and questions and concerns are addressed as quickly as possible. In certain instances, involving the surgeons in face-to-face discussions with the vendors can be very helpful in influencing the vendor to agree to participate.
Discussion
Hospital administrative leaders need clinical perspective to inform procurement decisions for the high-volume and high-expense setting of an OR platform. Increasingly this need is driving interest in finding ways for hospital administrators and physicians to collaborate. A collaborative arrangement should address three objectives in which hospitals must find ways to meet three objectives: (1) collaborate with medical staff leadership to provide surgeons with feedback regarding the financial impact of their implant selection on the cost of an episode of care; (2) ensure that medical staff leadership has an effective means of communication with hospital administration regarding the medical evidence supporting the use of newer, more expensive technologies or implants to benefit patient care; and (3) both the hospital and physicians need a system that allows tracking of the impact of efforts to manage implant use.
Both the literature and our review are limited. First there is very little peer-reviewed research and literature in this area. Second, the experiences in academic centers may not be applicable to other environments. Third, to achieve physician participation in these programs, some higher form of alignment between physicians and hospital or the health system must be in place. Fourth, we have very little published peer-reviewed data on cost savings. Such data will need to be accumulated in the future in a form that can be subject to peer-reviewed publication.
In 2006, the UCSF Medical Center introduced a Healthcare Technology Assessment Program (HTAP) [15]. The structure and impact of the UCSF HTAP program has been outlined by Gutowski et al. [15]. The experiences of the UCSF HTAP led to interest at two other academic medical centers (AMCs). Through collaboration with one of the leaders of the UCSF HTAP, a similar program was developed at these AMCs.
The development of technology assessment programs to add a clinical perspective to hospital purchasing decisions is one strategy used by hospitals that gives physicians a greater role and responsibility in decision-making related to the adoption of new technologies [9, 13]. These programs are increasingly popular because of the need for more thoughtful evaluation of new, expensive, and often unproven technologies [7, 9]. When new, more expensive technology supposedly delivers superior results to patients, there is often a lack of evidence-based analysis to support the added expense [8, 12]. The rapid innovation in the healthcare technology sector, a culture of minimal management of technology adoption practices within many hospitals, pervasive marketing pressure on physicians from manufacturers (through sales representatives and offers to participate in product development, speakers’ bureaus, and other consulting activities), demand for state-of-the-art care from patients, and increased emphasis placed on evidence-based medical decision-making underlie the environment in which technology assessment programs are of increasing value [9, 10, 13].
Although advantages for the hospital or health system have been discussed, there are potential disadvantages in setting up a physician-led system as well. For physicians leading such efforts, a substantial amount of time may be required. The value for hospital systems from these programs is centered around cost savings, whereas the value for surgeons is centered around access to technology and products required for cutting-edge medical care. Thoughtful communication to each of these key groups of stakeholders is necessary to ensure the successful work of the program is shared to each group. Finally, the development of such physician-led programs brings attention to the hospital-physician alignment structures in place. When surgeons begin to question why implant standardization efforts are being made, the explanation of how surgeons and their hospital or healthcare organization are aligned is valuable in these discussions.
The development of a Healthcare Technology Program is a means to achieve several important objectives. These include providing an objective method of tracking value or cost savings that result from the efforts of physicians who engage in cost reduction efforts. Such implant management efforts are often cited as providing a metric for judging physician engagement in a comanagement effort with a hospital or health system [2]. Other objectives include providing hospital leadership with a structure to have more informed, evidence-based procurement decision-making while having trust in the overall process; providing the structure for physicians to provide leadership for the process of informing technology procurement decisions; providing a method to inform physicians of the cost of implants they have requested; and providing an efficient process for the adoption of value-added clinical technologies while minimizing the number of nonvalue-added technologies that are used in clinical practice. Such programs give physicians leadership opportunities to influence the delivery of health care in their own environments.
Healthcare spending related to providing hospital care is one of the primary drivers of healthcare spending in the United States [5, 11]. Furthermore, the adoption of advanced medical technologies accounts for the largest percentage of growth in healthcare spending in the United States when compared with other developed countries [14]. Hospitals have long competed in a “medical arms race,” whereby they introduce newer, more sophisticated technologies in an attempt to attract patients who are seeking high-technology, high-quality care [19]. In some cases, the adoption of new technologies has led to improved patient outcomes and even a reduction in long-term healthcare spending [16, 20]. Examples include the polio vaccine and THA [6, 22]. However, there are many examples of healthcare technologies that have been widely adopted without evidence to support their use, and even long after their introduction, the benefits of these technologies as measured by improved patient outcomes or reduction in costs remain unproven [4].
A physician-led process to manage decisions to acquire new and often expensive implants and technology is effective. These systems track the value created through physician engagement in cost reduction efforts. Feedback is provided to both physicians and hospital administrators regarding decisions to acquire new technology. The underlying principle of this strategy is to engage physicians in considering the value of new technologies and the impact of their clinical decisions regarding choice of technology on the cost and quality of care they deliver in the hospital setting [2]. The physician-led process allows the consideration of the medical care benefits of new technology along with cost implications. This provides a structure that facilitates physician involvement in value-based purchasing in the OR environment.
Acknowledgments
We thank the staff and administrative support at Vanderbilt University Hospital and Duke University Hospital who made this work possible.
Appendix 1
Medical Economic Outcomes Committee (MEOC)
COMMITTEE CHARTER
March 2012
Mission and Vision: A clinician driven process that standardizes and utilizes evidence-based, clinically sound, financially responsible methodologies for introduction or consolidation of new supplies, devices and technology within Vanderbilt University Medical Center to provide the highest quality medical care.
Description: MEOC Committees will be comprised of subspecialty representatives who will be responsible for evaluating new product and device requests from within their peer group, or by request from the MEOC Executive Committee, as well as addressing identified opportunities in standardization, utilization or pricing obtained through internal/external analysis and benchmarking.
MEOC Committee Composition:
*Executive Medical Director
*Physician/Clinician Co-Chairs
*Physician/Physician Members, Subspecialties
*Supply Chain Officer
*Administrative Director, Supply Chain
*Clinical Administrator of Service Line
*Medical Sourcing Officer
*Financial Liaison
Supply Chain Analytics
*Clinicians (ad hoc)
*Voting Members
Tenure: Physicians serve 2 year terms (Rotation Process TBD). Non-physician members have no term limits.
Compensation: Participation will be on a volunteer level/designee basis.
Process: The MEOC Committees will evaluate new product/device/technology requests utilizing internal and external benchmark data as it relates to outcomes, quality and financial impact. Elements considered are to include but not limited to: evidenced based medicine reporting clinical outcomes, existence of like technology, existence of a current contract, proposed pricing, impact to overall cost per case, impact to operational expense, impact to revenue, impact to quality indicators such as decreased LOS, decreased mortality/morbidity and impact to the community. In addition, it will be the responsibility of the MEOC Committees to review market introduction of safety alternatives where previously there was not a safety version. The MEOC Committees will have oversight for designation of appropriate trial sites, collection and evaluation of the trial results and approval to implement based on end user feedback. This review will be conducted at least annually and documented in the committee minutes. All records will be retained by the medical sourcing office.
New Product Request for Trial or Permanent Placement: The requesting physician/clinician will complete the New Product Request Form available through the MEOC website at www.mc.vanderbilt.edu/meoc. The request will then be routed for approval to the Department Chair and the Administrative Director or Director having budgetary responsibility, thereby designating approval to proceed with the request. Requests will not be processed without this a acknowledgment.
Trials requests for products that are uncomplicated, have no conflict and are at no cost can be approved without going through a formal MEOC presentation. Requests for Trials that conflict with existing contracts, have a cost or have significant questions regarding the proposed use of the product/technology will need to be presented and requested through MEOC. The request must be submitted at least one month prior to the next committee meeting to be considered for presentation. Product/technology requests will fall into (3) categories:
Physician preferred items
Hospital based requests
Capital Technology
The requesting physician/clinician must be physically present at the meeting to present their request. No designees will be accepted; however additional non-vendors guests are welcome to provide support for the request. Failure to attend will result in the item being removed from the agenda until the physician/clinician resubmits. If the request is for a capital purchase, it should be listed on the current capital request list for approval from the financial liaison of the effective facility to validate available funding. No vendors are to be present nor can one present.
Conflict of Interest / Confidentiality Statement: All committee members and requesting physicians/clinicians must sign and comply with Vanderbilt policy. If a MEOC Committee member has a conflict of interest, he or she must disclose their potential conflict and may be present for discussion but not participate in the vote.
Attendance Requirements: Members are expected to attend all meetings. The Chair will contact members failing to attend meetings. Members failing to attend 50% of the scheduled meetings will be replaced following notification.
Quorum: A quorum is defined as fifty percent plus one for the voting members.
Meetings: MEOC Committees will meet at least monthly unless the volume warrants a decreased frequency.
Reporting Structure: MEOC Committees will report to the MEOC Steering Committee. Each Committee will provide a report of its actions and recommendations in presentation form by a selected member of the Committee to the MEOC Steering Committee.
Decision Making / Authority: MEOC Committees will have the authority to approve trials and evaluations of new products and technologies; give approval or denial for requests with values below $100,000; Send recommendations to the MEOC Steering Committee for a final review, approve or deny requests that meet any of the following criteria:
New requests for products or technology that value over $100,000.
New technology approval based on evidence based medicine.
Effects standardization or compliance with an existing contract.
Impacts operational expense by >20% on a cost per case basis.
New technology requires physician re-credentialing or has cross-departmental impact
Cost is not the sole consideration: the new technology may increase overall operational expense or decrease revenue, but has what is believed to be a significant clinical, marketing, research or community benefit.
MEOC Committees will have the ability to approve, deny or suggest a clinical evaluation of a new product/device if the following criteria are met:
Outcome data supports or refutes the superiority of propose product (when comparable product is currently being used).
It has no impact to an existing contract.
There is no comparable technology on the market.
There is funding available within the department to purchase.
Appeal Process: Physicians/clinicians wishing to appeal a decision of the MEOC Committees must submit a detailed communication describing the reason for the appeal along with supportive literature and/or data to the MEOC Steering Committee. The MEOC Steering Committee, or designated member(s), will review these materials and determine if the appeal is based on new and/or previously excluded information. A decision to entertain the appeal will only be granted to those who have submitted new and/or previously excluded information.
If the MEOC Steering Committee denies appeal, the request for new product is terminated.
If the MEOC Steering Committee is in favor of appeal, the request is forwarded back to the MEOC Committee for reconsideration.
Review of the Charter: The charter will be reviewed annually at the last meeting of the calendar year and as changes occur that would affect the operation of the Committees.
Appendix 2
Footnotes
Each author certifies that he or she, or a member of his or her immediate family, has no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
References
- 1.Bozic KJ. Value-based healthcare and orthopaedic surgery. Clin Orthop Relat Res. 2012;470:1004–1005. doi: 10.1007/s11999-012-2267-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bozic KJ, Roche M, Agnew SG. Hospital-based employment of orthopaedic surgeons—passing trend or new paradigm? AOA critical issues. J Bone Joint Surg Am. 2012;94:e59. doi: 10.2106/JBJS.L.00951. [DOI] [PubMed] [Google Scholar]
- 3.Briggs A, Sculpher M, Britton A, Murray D, Fitzpatrick R. The costs and benefits of primary total hip replacement. How likely are new prostheses to be cost-effective? Int J Technol Assess Health Care. 1998;14:743–761. doi: 10.1017/S0266462300012058. [DOI] [PubMed] [Google Scholar]
- 4.Campillo-Artero C. When health technologies do not reach their effectiveness potential: a health service research perspective. Health Policy. 2012;104:92–98. doi: 10.1016/j.healthpol.2011.09.010. [DOI] [PubMed] [Google Scholar]
- 5.Chandra C, Kumar S, Ghildayal NS. Hospital cost structure in the USA: what’s behind the costs? A business case. Int J Health Care Qual Assur. 2011;24:314–328. doi: 10.1108/09526861111125624. [DOI] [PubMed] [Google Scholar]
- 6.Chang RW, Pellisier JM, Hazen GB. A cost-effectiveness analysis of total hip arthroplasty for osteoarthritis of the hip. JAMA. 1996;275:858–865. doi: 10.1001/jama.1996.03530350040032. [DOI] [PubMed] [Google Scholar]
- 7.Eisenberg JM. Do better outcomes mean better quality care? Trans Am Clin Climatol Assoc. 1999;110:15–20. [PMC free article] [PubMed] [Google Scholar]
- 8.Eisenberg JM. Ten lessons for evidence-based technology assessment. JAMA. 1999;282:1865–1869. doi: 10.1001/jama.282.19.1865. [DOI] [PubMed] [Google Scholar]
- 9.Fine A. Developing an assessment process for new technologies. Healthc Financ Manage. 2003;57:84–87. [PubMed] [Google Scholar]
- 10.Gelberman RH, Samson D, Mirza SK, Callaghan JJ, Pellegrini VD., Jr Orthopaedic surgeons and the medical device industry: the threat to scientific integrity and the public trust. J Bone Joint Surg Am. 2010;92:765–777. doi: 10.2106/JBJS.I.01164. [DOI] [PubMed] [Google Scholar]
- 11.Goetghebeur MM, Forrest S, Hay JW. Understanding the underlying drivers of inpatient cost growth: a literature review. Am J Manag Care. 2003;9:SP3–SP12. [PubMed] [Google Scholar]
- 12.Gooch KL, Smith D, Wasylak T, Faris PD, Marshall DA, Khong H, Hibbert JE, Parker RD, Zernicke RF, Beaupre L, Pearce T, Johnston DW, Frank CB. The Alberta Hip and Knee Replacement Project: a model for health technology assessment based on comparative effectiveness of clinical pathways. Int J Technol Assess Health Care. 2009;25:113–123. doi: 10.1017/S0266462309090163. [DOI] [PubMed] [Google Scholar]
- 13.Gordon GJ, Tan KM. Technology assessment and equipment planning in Kaiser Permanente, Northern California Region. J Clin Eng. 1992;17:209–213. doi: 10.1097/00004669-199205000-00010. [DOI] [PubMed] [Google Scholar]
- 14.Goyen M, Debatin JF. Healthcare costs for new technologies. Eur J Nucl Med Mol Imaging. 2009;36(Suppl 1):S139–S143. doi: 10.1007/s00259-008-0975-y. [DOI] [PubMed] [Google Scholar]
- 15.Gutowski C, Maa J, Hoo KS, Bozic KJ. Health technology assessment at the University of California-San Francisco. J Healthc Manag. 2011;56:15–29. [PubMed] [Google Scholar]
- 16.Johnson DE. Will disruptive innovations cure health care? Harv Bus Rev. 2000;78:197–198. [PubMed] [Google Scholar]
- 17.Kaplan RS, Porter ME. How to solve the cost crisis in health care. Harv Bus Rev. 2011;89:46–52, 54, 56–61 passim. [PubMed]
- 18.Lansky D, Nwachukwu BU, Bozic KJ. Using financial incentives to improve value in orthopaedics. Clin Orthop Relat Res. 2012;470:1027–1037. doi: 10.1007/s11999-011-2127-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Luft HS, Garnick DW, Hughes RG, Hunt SS, McPhee SJ, Robinson JC. Hospital competition, cost, and medical practice. J Med Pract Manage. 1988;4:10–15. [PubMed] [Google Scholar]
- 20.McGrady E, Conger S, Blanke S, Landry BJ. Emerging technologies in healthcare: navigating risks, evaluating rewards. J Healthc Manag. 2010;55:353–364. [PubMed] [Google Scholar]
- 21.O’Shea K, Bale E, Murray P. Cost analysis of primary total hip replacement. Ir Med J. 2002;95:177–180. [PubMed] [Google Scholar]
- 22.Salk J. Immunization against poliomyelitis: risk/benefit/cost in a changing context. Dev Biol Stand. 1979;43:151–157. [PubMed] [Google Scholar]
- 23.Turnipseed WD, Lund DP, Sollenberger D. Product line development: a strategy for clinical success in academic centers. Ann Surg. 2007;246:585–590. doi: 10.1097/SLA.0b013e318155a97d. [DOI] [PubMed] [Google Scholar]
- 24.Zuckerman JD, Kummer FJ, Frankel VH. The effectiveness of a hospital-based strategy to reduce the cost of total joint implants. J Bone Joint Surg Am. 1994;76:807–811. doi: 10.2106/00004623-199406000-00003. [DOI] [PubMed] [Google Scholar]