Abstract
Background
Traumatic posterior hip dislocation in adults is generally understood to be the result of a high-energy trauma. Aside from reduced femoral antetorsion, morphologic risk factors for dislocation are unknown. We previously noticed that some hips with traumatic posterior dislocations had evidence of morphologic features of femoroacetabular impingement (FAI), therefore, we sought to evaluate that possibility more formally.
Questions/purposes
We asked whether hips with a traumatic posterior hip dislocation present with (1) a cam-type deformity and/or (2) a retroverted acetabulum.
Methods
We retrospectively compared the morphologic features of 53 consecutive hips (53 patients) after traumatic posterior hip dislocation with 85 normal hips (44 patients) based on AP pelvic and crosstable axial radiographs. We measured the axial and the lateral alpha angle for detection of a cam deformity and the crossover sign, ischial spine sign, posterior wall sign, retroversion index, and ratio of anterior to posterior acetabular coverage to describe the acetabular orientation.
Results
Hips with traumatic posterior traumatic dislocation were more likely to have cam deformities than were normal hips, in that the hips with dislocation had increased axial and lateral alpha angles. Hips with posterior dislocation also were more likely to be retroverted; dislocated hips had a higher prevalence of a positive crossover sign, ischial spine sign, and posterior wall sign, and they had a higher retroversion index and increased ratio of anterior to posterior acetabular coverage.
Conclusions
Hips with posterior traumatic dislocation typically present with morphologic features of anterior FAI, including a cam-type deformity and retroverted acetabulum. An explanation for these findings could be that the early interaction between the aspherical femoral head and the prominent acetabular rim acts as a fulcrum, perhaps making these hips more susceptible to traumatic dislocation.
Level of Evidence
Level III, prognostic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
Morphologic risk factors for prosthetic dislocation are well known, including decreased femoral head-neck offset [1, 10], decreased femoral antetorsion [8], and retroversion of the acetabular cup [9, 16]. In contrast, there is limited information regarding the etiology of traumatic hip dislocations of the native hip. Traumatic hip dislocation in the adult is generally understood to be the result of a high-energy injury [2]. Upadhyay et al. [27] investigated morphologic parameters that make hips more susceptible to posterior hip dislocations and showed reduced femoral antetorsion or even retrotorsion predisposes the hip to posterior dislocation. More recently, Philippon et al. [13] reported nine of 14 traumatic hip dislocations in athletes treated with arthroscopy for residual problems had evidence of femoroacetabular impingement (FAI) [5]. Analogous to prosthetic impingement, this pathologic femoroacetabular conflict theoretically would act as a fulcrum for posterior dislocation in deep flexion and internal rotation [15]. We have made the clinical observation that hips with traumatic posterior dislocation often present with pathomorphologic variations related to FAI.
We therefore asked whether hips with a traumatic posterior hip dislocation present with (1) a cam-type deformity and/or (2) a retroverted acetabulum compared with data from normal hips.
Patients and Methods
This study was approved by the local institutional review board. Using our institutional database, we identified 169 patients with 195 traumatic hip dislocations who were seen at the emergency room of a Level I trauma center from August 1998 to November 2010. We excluded 63 patients with 89 prosthetic dislocations and 10 patients with 10 anterior traumatic hip dislocations. This resulted in 96 traumatic posterior dislocations in 96 patients. These hips were classified according to Thompson and Epstein [25]: Type I with or without a minor fracture, Type II with a large single fracture of the posterior acetabular rim, Type III with comminution of the rim of the acetabulum with or without a major fragment, Type IV with a fracture of the acetabular floor, and Type V with a fracture of the femoral head. Owing to the extent of osseous damage in hips with Types III and IV dislocations making accurate evaluation of morphologic features of the hip impossible, 43 dislocations in 43 patients were excluded. Eventually, the study group consisted of 53 dislocations in 53 patients (Table 1), including 28 hips (53%) with Type I, 15 (28%) with Type II, and 10 (19%) with Type V dislocations according to Thompson and Epstein [25].
Table 1.
Demographic and radiographic factors of the two study groups
| Parameter | Normative data† | Study group | p value |
|---|---|---|---|
| Number of patients (hips) | 44 (85) | 53 (53) | |
| Percentage of bilateral hips | 48 | 0 | < 0.001 |
| Age (years)* | 40 ± 10.5 (18–59) | 35 ± 16.4 (10–73) | 0.058 |
| Sex (% male of all hips) | 56 | 72 | 0.052 |
| Side (% right of all hips) | 51 | 47 | 0.415 |
| Radiographic parameters* | |||
| Lateral center-edge angle (°) | 32 ± 7.1 (18–55) | 32 ± 7.8 (17–50) | 0.714 |
| Acetabular index (°) | 2 ± 5.4 (−11 to 13) | 4 ± 6.2 (−9 to 17) | 0.053 |
| Extrusion index (%) | 18 ± 6.5 (−2 to 33) | 18 ± 7.4 (−5 to 32) | 0.986 |
| Centrum-collum-diaphyseal angle (°) | 126 ± 5.3 (102–137) | 133 ± 6.2 (118–145) | < 0.001 |
The morphologic features of the hips were compared between the study group and normative data from the literature [17]. These normative data were based on a group of 86 patients (172 hips) in whom an AP pelvic radiograph was performed for nonorthopaedic indications (gynecologic and genitourinary indications) between January and December 2000. All patients of this group presented with no history of hip pain, known childhood hip diseases, or connective tissue disorders. Sixteen hips (six patients with bilateral involvement [12 hips], four patients with unilateral involvement [four hips]) were excluded owing to radiographic signs of hip osteoarthritis resulting in 156 hips (80 patients [76 bilateral]). Since this group differed from the study group in terms of age and percentage of male patients, a matched series of 44 patients (85 hips) was selected for evaluation (Table 1). For these patients no lateral hip radiographs were available and therefore the normal values for the alpha angle on the axial view were derived from a previously published CT study [19].
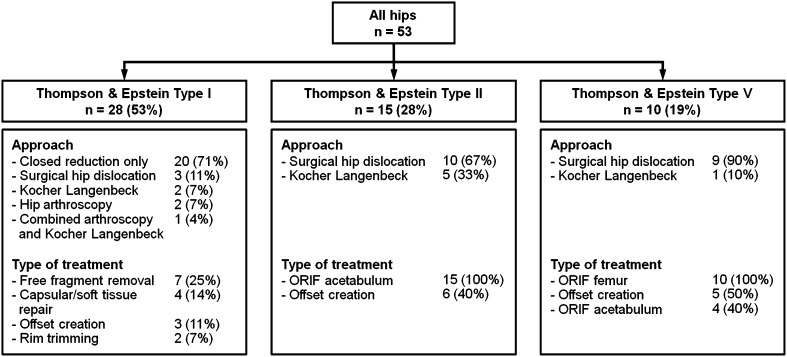
Patients with a traumatic hip dislocation either were admitted directly through the emergency department of our hospital or were referred from another institution. The trauma mechanism was a car accident in 20 hips (38%), motorcycle accident in 11 hips (21%), fall in 11 hips (21%), sport accident in five hips (9%), bicycle accident in one hip (2%), and other mechanisms in five hips (9%). After resuscitation, an AP pelvic radiograph was obtained. All patients underwent immediate closed reduction under general anesthesia. After reduction of the femoral head, a second AP pelvic radiograph and a crosstable axial radiograph of the hip were acquired. All radiographs were taken according to a previously defined standardized technique [23]. Surgical treatment after closed reduction was performed in 33 hips (62%) (Fig. 1). The indications for surgery were a dislocated fracture of the acetabulum and/or femoral head, free intraarticular fragments, and capsular/soft tissue lesions (Fig. 1). Eventual femoral osteochondroplasty was performed if a surgical hip dislocation was the surgical approach of choice and a nonspherical femoral head-neck junction was identified intraoperatively with spherical templates [22].
Fig. 1.
A flowchart illustrates the approach and surgical treatment of the hips with posterior traumatic dislocation. ORIF = open reduction and internal fixation.
One observer (CEA) then assessed the radiographic morphologic features of the proximal femur and acetabulum for both groups using a previously developed and validated computer software (Hip2Norm; University of Bern, Bern, Switzerland) [20, 24, 30]. The measurements were corrected for pelvic rotation. Next to conventional radiographic parameters the software allowed us to calculate acetabular coverage of the femoral head (Fig. 2). Only radiographs after closed reduction performed in a standardized manner [23] were used for evaluation in hips without fractures (Thompson and Epstein Type I). In hips with a large single fracture of the posterior acetabular wall (Type II) or femoral head (Type V) the radiographs were evaluated after open reduction and internal fixation (ORIF).
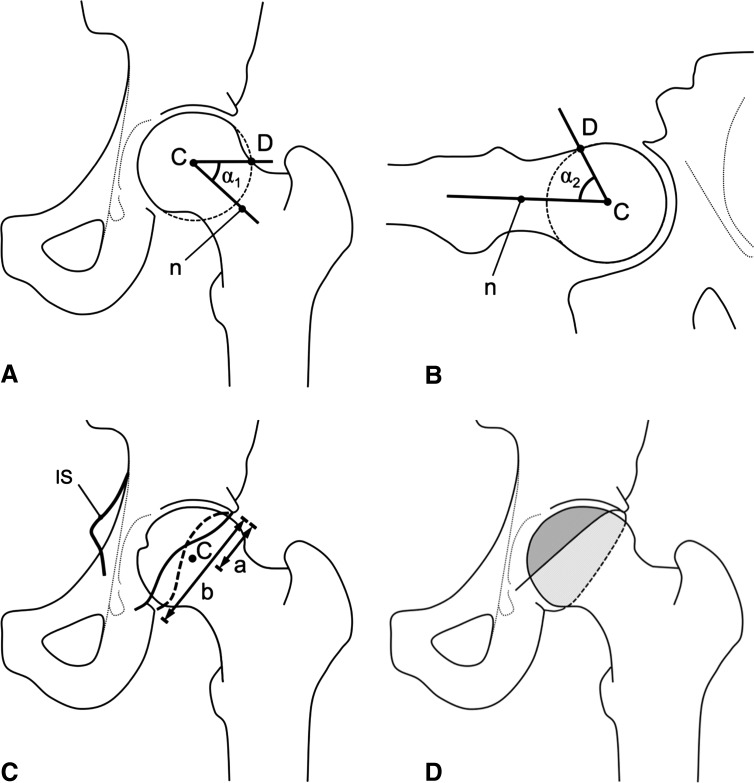
Fig. 2A–D.
Radiographic parameters for assessment of cam deformity and acetabular retroversion are shown. (A) The AP alpha angle (α1) is formed by the neck axis (n) and a line through the center of the head (C) and the point (D) where the femoral neck exceeds the circle outlying the femoral head (dashed line). (B) The axial alpha angle (α2) is formed in a similar way on the crosstable axial radiograph. (C) The crossover sign is positive when the anterior wall of the acetabulum (solid line) crosses the posterior wall (dashed line). The retroversion index is the ratio of distance (a) to the length of the acetabular cup opening (b). The ischial spine sign is positive when the ischial spine (IS) protrudes into the true pelvis. The posterior wall sign is positive when the posterior wall (dashed line) is projected medially to the femoral head center (C). (D) Anterior and posterior coverage is defined as the percentage of area of the femoral head covered by the anterior (gray area) or posterior (dashed area) wall, respectively. The ratio of anterior to posterior coverage is a measure for the acetabular orientation.
The femoral head-neck asphericity was assessed on AP pelvic and crosstable axial radiographs of the hip. To exclude malpositioning effects of the pelvis on the radiograph, only radiographs obtained after closed reduction were used for evaluation. Parameters included the lateral alpha angle on AP radiographs (Fig. 2A) and the axial alpha angle on crosstable axial radiographs (Fig. 2B) [12].
Measurement for the acetabular orientation included the presence of the crossover sign [15], retroversion index [17], ischial spine sign [6, 7], and posterior wall sign [15] (Fig. 2C), and the ratio of anterior to posterior coverage on the AP pelvic radiograph (Fig. 2D). The ischial spine sign is an indirect radiographic indicator for acetabular retroversion since the entire hemipelvis is externally rotated in these hips [6, 21]. It is positive if the ischial spine protrudes into the true pelvis on the orthograde AP pelvic radiograph. The posterior wall sign is positive if the posterior wall is projected medially to the femoral head center, indicating a retroverted acetabulum [15].
All determined study variables were reliable and reproducible [10, 18, 20].
We tested the data for normal distribution using the Kolmogorov-Smirnov test. Because not all the parameters were normally distributed, we used the Mann-Whitney U test for comparison of the demographic and radiographic parameters between the two study groups. Binominal and categorical data were compared using Fisher’s exact test. Statistical analysis was performed using WinStat® (R. Fitch Software, Bad Krozingen, Germany).
Results
Femoral cam deformities were more common in the hips with traumatic posterior dislocation compared with normative data. Lateral and axial alpha angles were increased in the study group compared with normative data (p < 0.001) (Table 2).
Table 2.
Radiographic results
| Parameter | Normative data†,‡ | Study group | p value |
|---|---|---|---|
| Proximal femoral morphologic features | |||
| Lateral alpha angle (°)* | 47 ± 8.5 (36–83)† | 58 ± 13.6 (37–91) | < 0.001 |
| Axial alpha angle (°)* | 43 ± 4.8 (34–50)‡ | 57 ± 10.9 (40–80) | < 0.001 |
| Acetabular orientation | |||
| Crossover sign (% positive) | 33† | 79 | < 0.001 |
| Retroversion index (%)* | 24 ± 11.6 (6–45)† | 33 ± 14.8 (6–67) | 0.019 |
| Ischial spine sign (% positive) | 22† | 64 | < 0.001 |
| Posterior wall sign (% positive) | 29† | 83 | < 0.001 |
| Anterior/posterior coverage (%)* | 56 ± 14 (21–89)† | 68 ± 24 (34–124) | 0.004 |
Likewise, hips with posterior dislocations were more likely to be retroverted. The prevalence of positive crossover, ischial spine, and posterior wall signs were increased in the study group (p < 0.001), as was the retroversion index (p = 0.019) (Table 2). The ratio of anterior to posterior coverage also was increased in the study group compared with normative data (p = 0.004) (Table 2).
Discussion
Traumatic hip dislocation in adults is generally understood to result from high-energy trauma. Aside from reduced femoral antetorsion in hips with posterior dislocation, morphologic risk factors are unknown. Following the concepts of prosthetic hip dislocation and in accordance with the clinical observation, we asked whether hips with a traumatic posterior hip dislocation have (1) a cam-type deformity and/or (2) a retroverted acetabulum.
This study has several limitations. First, we were unable to quantify femoral torsion accurately. Conventional radiographs are too sensitive to the individual positioning of the patient’s femur [11, 29]. Although a whole-body CT scan of some of the patients existed, measurement of femoral torsion was not possible in these cases because the femoral condyles were not included [11]. Second, for comparison, normative data from the literature were used [17, 19]. Since the patients in the study group were typically younger and a greater percentage of men were present in this group, a series of patients with matched demographic parameters was selected. However, even with that adjustment, there was a trend toward more men in the study group (p = 0.052; Table 1), which could have biased the incidence of an increased alpha angle since cam-type FAI is more common in males. Another limitation is the lack of crosstable axial radiographs in this population. Instead, the normal values for the alpha angle were acquired from a previously published CT-based study [19]. This should not jeopardize our results since alpha angles measured on conventional radiographs generally are underestimated [4, 14]. Therefore, an even greater difference between the two groups can be expected. Next, the study group included hips with a single posterior acetabular wall fracture (28%) or femoral head fracture (19%). This could have biased the measurements of morphologic features of the hips. Therefore, only radiographs obtained after ORIF were used for evaluation. Because nonanatomic reductions of the posterior wall fragment would lead to overestimation of the posterior wall and therefore decreased incidence of radiographic parameters indicating acetabular retroversion, we believe this has not jeopardized our results.
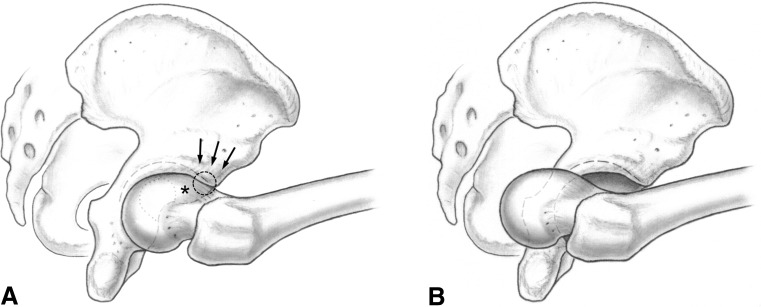
We found hips with a posterior traumatic hip dislocation more often present with an increased alpha angle and retroverted acetabulum. Based on these results, we speculate that the observed morphologic features of FAI may mechanically predispose these hips to dislocation; with increasing flexion and internal rotation, the femoral head-neck junction comes into contact with the prominent acetabular rim, which then acts as a fulcrum (Fig. 3). The increasing force of the long femoral lever arm pushes the femoral head posteriorly. Hips with a fulcrum need less impact and may dislocate without a fracture, even more so when the posterior border is less prominent. As shown in the literature for prosthetic posterior hip dislocations, low femoral antetorsion or even retrotorsion [8] and an increased centrum-collum-diaphyseal (CCD) angle [28] have the same effect in decreasing the clearance for internal rotation in flexion. This is consistent with the literature for dislocation of native hips with femoral retroversion [27]. The CCD angle was increased (p < 0.001) for hips with posterior dislocation in the current series compared with normative data (Table 1). In a morphologically normal hip, the femoral head may dislocate with a posterior wall fracture after heavy axial impact, eg, a dashboard injury (Fig. 4). Although this explanation seems plausible, and although we observed more hips with cam deformities and acetabular retroversion in the group with posterior dislocation, our study design does not prove the mechanism that we theorized.
Fig. 3A–B.
Mechanisms in posterior traumatic hip dislocation are illustrated. (A) With increasing flexion and internal rotation, the aspherical femoral head-neck junction (asterisk) comes into contact with the prominent acetabular rim (arrows), which then acts as a fulcrum (circle). (B) The increasing force of the long femoral lever arm pushes the femoral head posteriorly. Hips with a fulcrum need less impact and may dislocate without a fracture, even more so when the posterior border is less prominent.
Fig. 4A–C.

(A) An AP radiograph shows the hips of a 19-year-old man who sustained a posterior hip dislocation after a car injury. Hips with posterior traumatic dislocation typically present with morphologic features of anterior FAI, including a cam-type deformity and retroverted acetabulum, as indicated by (B) a positive crossover sign (arrow) and increased lateral alpha angle (α1) and (C) increased axial alpha angle (α2).
Only a few authors have identified morphologic osseous abnormalities as causative factors of traumatic hip dislocations. Upadhyay et al. [27] has identified reduced femoral antetorsion as a predisposing factor that in fact increases the risk of impingement [5]. Recently, morphologic features of impingement were observed in traumatic hip dislocations in athletes [13] who regularly used their hip mobility to the extremes. However, there was no control group in that study. Although one could assume dysplastic hips predispose for traumatic dislocation, there is only one case report in the literature [26]. This suggests that a fulcrum may be more important for dislocation than a deficiency of coverage.
Hips with posterior traumatic dislocation typically present with morphologic features of FAI, including a cam-type deformity and retroverted acetabulum (Fig. 4). An explanation for these findings could be that the early interaction between the aspherical femoral head and the prominent acetabular rim acts as a fulcrum. This makes these hips more susceptible to traumatic dislocation. We believe this finding is clinically important. Impingement [23] and traumatic dislocation [3] predispose patients to early arthritis. Patients with traumatic hip dislocation should be carefully analyzed, and consideration given to correcting their pathomorphologic abnormalities.
Footnotes
Each author certifies that he or she, or a member of his or her immediate family, has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution has approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
References
- 1.Amstutz HC, Lodwig RM, Schurman DJ, Hodgson AG. Range of motion studies for total hip replacements: a comparative study with a new experimental apparatus. Clin Orthop Relat Res. 1975;111:124–130. doi: 10.1097/00003086-197509000-00016. [DOI] [PubMed] [Google Scholar]
- 2.Clegg TE, Roberts CS, Greene JW, Prather BA. Hip dislocations: epidemiology, treatment, and outcomes. Injury. 2010;41:329–334. doi: 10.1016/j.injury.2009.08.007. [DOI] [PubMed] [Google Scholar]
- 3.Dreinhofer KE, Schwarzkopf SR, Haas NP, Tscherne H. Isolated traumatic dislocation of the hip: long-term results in 50 patients. J Bone Joint Surg Br. 1994;76:6–12. [PubMed] [Google Scholar]
- 4.Dudda M, Albers C, Mamisch TC, Werlen S, Beck M. Do normal radiographs exclude asphericity of the femoral head-neck junction? Clin Orthop Relat Res. 2009;467:651–659. doi: 10.1007/s11999-008-0617-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ganz R, Parvizi J, Beck M, Leunig M, Notzli H, Siebenrock KA. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res. 2003;417:112–120. doi: 10.1097/01.blo.0000096804.78689.c2. [DOI] [PubMed] [Google Scholar]
- 6.Kalberer F, Sierra RJ, Madan SS, Ganz R, Leunig M. Ischial spine projection into the pelvis: a new sign for acetabular retroversion. Clin Orthop Relat Res. 2008;466:677–683. doi: 10.1007/s11999-007-0058-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kakaty DK, Fischer AF, Hosalkar HS, Siebenrock KA, Tannast M. The ischial spine sign: does tilt and rotation matter? Clin Orthop Relat Res. 2010;468(3):769–774. doi: 10.1007/s11999-009-1021-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kim YH, Choi Y, Kim JS. Influence of patient-, design-, and surgery-related factors on rate of dislocation after primary cementless total hip arthroplasty. J Arthroplasty. 2009;24:1258–1263. doi: 10.1016/j.arth.2009.03.017. [DOI] [PubMed] [Google Scholar]
- 9.Lewinnek GE, Lewis JL, Tarr R, Compere CL, Zimmerman JR. Dislocations after total hip-replacement arthroplasties. J Bone Joint Surg Am. 1978;60:217–220. [PubMed] [Google Scholar]
- 10.Marchetti E, Krantz N, Berton C, Bocquet D, Fouilleron N, Migaud H, Girard J. Component impingement in total hip arthroplasty: frequency and risk factors. A continuous retrieval analysis series of 416 cup. Orthop Traumatol Surg Res. 2011;97:127–133. doi: 10.1016/j.otsr.2010.12.004. [DOI] [PubMed] [Google Scholar]
- 11.Murphy SB, Simon SR, Kijewski PK, Wilkinson RH, Griscom NT. Femoral anteversion. J Bone Joint Surg Am. 1987;69:1169–1176. [PubMed] [Google Scholar]
- 12.Notzli HP, Wyss TF, Stoecklin CH, Schmid MR, Treiber K, Hodler J. The contour of the femoral head-neck junction as a predictor for the risk of anterior impingement. J Bone Joint Surg Br. 2002;84:556–560. doi: 10.1302/0301-620X.84B4.12014. [DOI] [PubMed] [Google Scholar]
- 13.Philippon MJ, Kuppersmith DA, Wolff AB, Briggs KK. Arthroscopic findings following traumatic hip dislocation in 14 professional athletes. Arthroscopy. 2009;25:169–174. doi: 10.1016/j.arthro.2008.09.013. [DOI] [PubMed] [Google Scholar]
- 14.Rakhra KS, Sheikh AM, Allen D, Beaule PE. Comparison of MRI alpha angle measurement planes in femoroacetabular impingement. Clin Orthop Relat Res. 2009;467:660–665. doi: 10.1007/s11999-008-0627-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Reynolds D, Lucas J, Klaue K. Retroversion of the acetabulum: a cause of hip pain. J Bone Joint Surg Br. 1999;81:281–288. doi: 10.1302/0301-620X.81B2.8291. [DOI] [PubMed] [Google Scholar]
- 16.Siebenrock K, Ganz R. The impingement problem in total hip arthroplasty. In: Rieker C, Oberholzer ST, Wyss U, editors. World Tribology Forum in Arthroplasty. Bern, Switzerland: Hans Huber; 2001. pp. 47–52. [Google Scholar]
- 17.Siebenrock KA, Kalbermatten DF, Ganz R. Effect of pelvic tilt on acetabular retroversion: a study of pelves from cadavers. Clin Orthop Relat Res. 2003;407:241–248. doi: 10.1097/00003086-200302000-00033. [DOI] [PubMed] [Google Scholar]
- 18.Steppacher SD, Tannast M, Werlen S, Siebenrock KA. Femoral morphology differs between deficient and excessive acetabular coverage. Clin Orthop Relat Res. 2008;466:782–790. doi: 10.1007/s11999-008-0141-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tannast M, Kubiak-Langer M, Langlotz F, Puls M, Murphy SB, Siebenrock KA. Noninvasive three-dimensional assessment of femoroacetabular impingement. J Orthop Res. 2007;25:122–131. doi: 10.1002/jor.20309. [DOI] [PubMed] [Google Scholar]
- 20.Tannast M, Mistry S, Steppacher SD, Reichenbach S, Langlotz F, Siebenrock KA, Zheng G. Radiographic analysis of femoroacetabular impingement with Hip2Norm: reliable and validated. J Orthop Res. 2008;26:1199–1205. doi: 10.1002/jor.20653. [DOI] [PubMed] [Google Scholar]
- 21.Tannast M, Pfannebecker P, Schwab JM, Albers CE, Siebenrock KA, Büchler L. Pelvic morphology differs in rotation and obliquity between developmental dysplasia of the hip and retroversion. Clin Orthop Relat Res. 2012;470:3297–3305. doi: 10.1007/s11999-012-2473-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tannast M, Siebenrock KA. [Open therapy of femoroacetabular impingement] [in German] Oper Orthop Traumatol. 2010;22:3–16. doi: 10.1007/s00064-010-3001-7. [DOI] [PubMed] [Google Scholar]
- 23.Tannast M, Siebenrock KA, Anderson SE. Femoroacetabular impingement: radiographic diagnosis—what the radiologist should know. AJR Am J Roentgenol. 2007;188:1540–1552. doi: 10.2214/AJR.06.0921. [DOI] [PubMed] [Google Scholar]
- 24.Tannast M, Zheng G, Anderegg C, Burckhardt K, Langlotz F, Ganz R, Siebenrock KA. Tilt and rotation correction of acetabular version on pelvic radiographs. Clin Orthop Relat Res. 2005;438:182–190. doi: 10.1097/01.blo.0000167669.26068.c5. [DOI] [PubMed] [Google Scholar]
- 25.Thompson VP, Epstein HC. Traumatic dislocation of the hip; a survey of two hundred and four cases covering a period of twenty-one years. J Bone Joint Surg Am. 1951;33:746–778; passim. [PubMed]
- 26.Trojan E. [Case of traumatic hip dislocation in bilateral hip dysplasia (coxa valga luxans)] [in German] Z Orthop Ihre Grenzgeb. 1953;83:469–471. [PubMed] [Google Scholar]
- 27.Upadhyay SS, Moulton A, Burwell RG. Biological factors predisposing to traumatic posterior dislocation of the hip: a selection process in the mechanism of injury. J Bone Joint Surg Br. 1985;67:232–236. doi: 10.1302/0301-620X.67B2.3884614. [DOI] [PubMed] [Google Scholar]
- 28.Widmer KH, Majewski M. The impact of the CCD-angle on range of motion and cup positioning in total hip arthroplasty. Clin Biomech (Bristol, Avon). 2005;20:723–728. [DOI] [PubMed]
- 29.Wissing H, Buddenbrock B. [Determining rotational errors of the femur by axial computerized tomography in comparison with clinical and conventional radiologic determination] [in German] Unfallchirurgie. 1993;19:145–157. doi: 10.1007/BF02588038. [DOI] [PubMed] [Google Scholar]
- 30.Zheng G, Tannast M, Anderegg C, Siebenrock KA, Langlotz F. Hip2Norm: an object-oriented cross-platform program for 3D analysis of hip joint morphology using 2D pelvic radiographs. Comput Methods Programs Biomed. 2007;87:36–45. doi: 10.1016/j.cmpb.2007.02.010. [DOI] [PubMed] [Google Scholar]