Abstract
Background
The prevention of medical and surgical harm remains an important public health problem despite increased awareness and implementation of safety programs. Successful introduction and maintenance of surgical safety programs require both surgeon leadership and collaborative surgeon-hospital alignment. Documentation of success of such surgical safety programs in orthopaedic practice is limited.
Questions/purposes
We describe the scope of orthopaedic surgical patient safety issues, define critical elements of orthopaedic surgical safety, and outline leadership roles for orthopaedic surgeons needed to establish and sustain a culture of safety in contemporary healthcare systems.
Methods
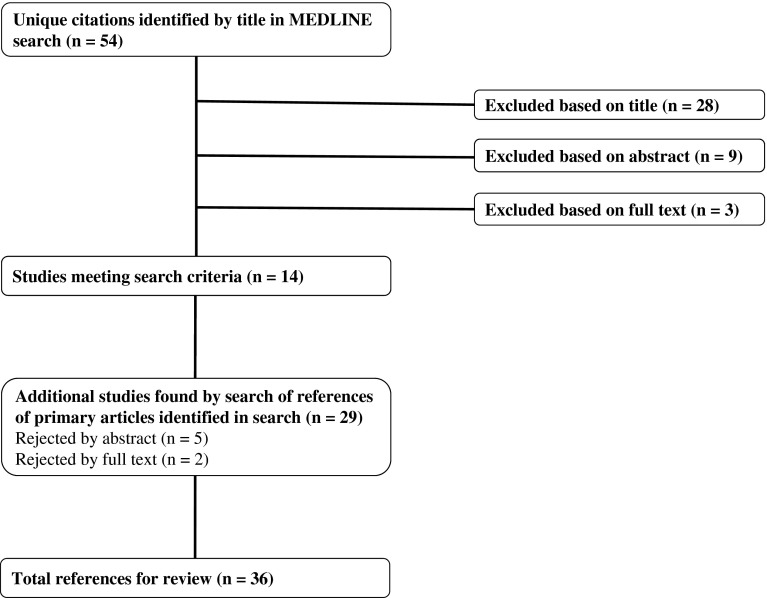
We identified the most common causes of preventable surgical harm based on adverse and sentinel surgical events reported to The Joint Commission. A comprehensive literature review through a MEDLINE® database search (January 1982 through April 2012) to identify pertinent orthopaedic surgical safety articles found 14 articles. Where gaps in orthopaedic literature were identified, the review was supplemented by 22 nonorthopaedic surgical references. Our final review included 36 articles.
Results
Six important surgical safety program elements needed to eliminate preventable surgical harm were identified: (1) effective surgical team communication, (2) proper informed consent, (3) implementation and regular use of surgical checklists, (4) proper surgical site/procedure identification, (5) reduction of surgical team distractions, and (6) routine surgical data collection and analysis to improve the safety and quality of surgical patient care.
Conclusions
Successful surgical safety programs require a culture of safety supported by all six key surgical safety program elements, active surgeon champions, and collaborative hospital and/or administrative support designed to enhance surgical safety and improve surgical patient outcomes. Further research measuring improvements from such surgical safety systems in orthopaedic care is needed.
Introduction
More than a decade ago, the Institute of Medicine published “To Err is Human, Building a Safer Health System” [23]. Much attention has been given to this report but, to date, there is little evidence of reduction of preventable medical harms, including surgical harms [28]. The American Academy of Orthopaedic Surgeons (AAOS) introduced the Sign Your Site program in 1997 designed to reduce the rate of wrong-site surgery [7]. More than a decade later, there is little evidence that wrong-site surgery has decreased [18, 45].
The Joint Commission (TJC) introduced the Universal Protocol (UP) initiative in 2004 to increase the reliability of perioperative surgical safety processes [42]. The UP initiative has been adopted by many hospitals and healthcare systems. In 2007, the WHO introduced the Safe Surgery Saves Lives program. This international surgical safety program demonstrated improved surgical team communication, use of standardized surgical processes, and routine surgical safety and quality data collection reduced surgical errors, complications, and mortalities [17]. Although many of the elements of the UP and WHO programs have been adopted in hospitals and healthcare systems within the United States, information concerning the impact such programs have had on orthopaedic care is limited [40].
There are several barriers to adoption of these newer safety processes needed to build and sustain a culture of safety within the orthopaedic community (Table 1). Historically, communication and workflow in orthopaedic operating rooms (ORs) were not designed to systematically prevent and reduce preventable surgical harm. Orthopaedic surgeons worked with unchallenged authority among their OR teams, used highly individualized surgical workflows, and rarely routinely collected safety or quality data. This created a surgeon-centric OR culture that is both less reliable and safe for patients undergoing orthopaedic surgery.
Table 1.
Characteristics of historical and contemporary orthopaedic surgeon OR behavior
| Surgeon behavior | Historical OR | Contemporary OR |
|---|---|---|
| Communication | ||
| Style | Authoritative | Facilitative |
| Management of responsibilities | Surgeon-driven | Delegated/shared among team members |
| Surgical processes | ||
| Surgical techniques | Individualized | Standardized |
| Care plans | Surgeon-centric | System-centric |
| Data | ||
| Collection | Limited, irregular | Active data management, routine accumulation |
| Decision making | Experience- or memory-based | Systematic data collection and analysis |
OR = operating room.
Dr. Mark Chassin, president of TJC, identified the following most common causes for sentinel surgical events reported to TJC: (1) inadequate information, (2) scheduling discrepancies, (3) irregularities in the preoperative holding process, (4) inadequate/absent surgical site marking, (5) inadequate/absent time-out, (6) poor communication, and (7) distractions in the OR [33].
The cultural requirements of a safe contemporary OR require surgeon leadership of teams that consistently use surgical processes designed to systematically prevent and reduce surgical harm (Table 1). Surgical care pathways need to be standardized, uniform, and system-centric. Surgical workflows and responsibilities are delegated among the entire team. Orthopaedic surgeons share responsibility for every component of the surgical care episode. Their leadership is essential to provide the safest possible care through effective and reliable surgical team communication and the implementation and maintenance of standardized surgical processes designed to prevent surgical harm and improve surgical outcomes.
Our purpose is to (1) describe the need for renewed focus on the safety of patients undergoing orthopaedic surgery, (2) define critical elements of orthopaedic surgical safety, and (3) outline the leadership roles for orthopaedic surgeons needed to establish a culture of safety in contemporary healthcare systems.
Search Strategy and Criteria
We identified the most frequent causes of adverse orthopaedic and surgical events reported to TJC Sentinel Events Database since 2002 [41]. We performed a comprehensive review of the literature in MEDLINE® for articles published from January 1982 through April 2012 to evaluate orthopaedic patient safety knowledge related to TJC Sentinel Surgical Events using the following search terms: “patient safety” AND “orthopedic procedures” AND (“communication” OR “checklist” OR “patient care team/organization & administration” OR “preoperative care/standards” OR “medical errors” OR “preventable harm”). The articles reviewed were limited to the English language and complete articles from peer-reviewed journals. Fifty-four articles were initially identified with these search terms (Fig. 1). Articles were considered relevant if they met the following criteria: (1) the article’s main objectives were related to patient safety and (2) included orthopaedic surgery in its study setting. The authors (CCK, WJR) independently reviewed each title, abstract, and/or full article content to determine relevance, excluding articles that were unrelated to patient safety and orthopaedics. Based on these criteria, 14 relevant articles were selected, identifying critical elements of orthopaedic safety in the perioperative period. Where gaps in orthopaedic literature were identified, the review was supplemented by nonorthopaedic surgical references included in the original 54 articles, yielding an additional 22 relevant publications. Our final review included 36 articles.
Fig. 1.
A flowchart shows the literature review process used in this study.
The Need for Renewed Focus on Safety for Patients Undergoing Orthopaedic Surgery
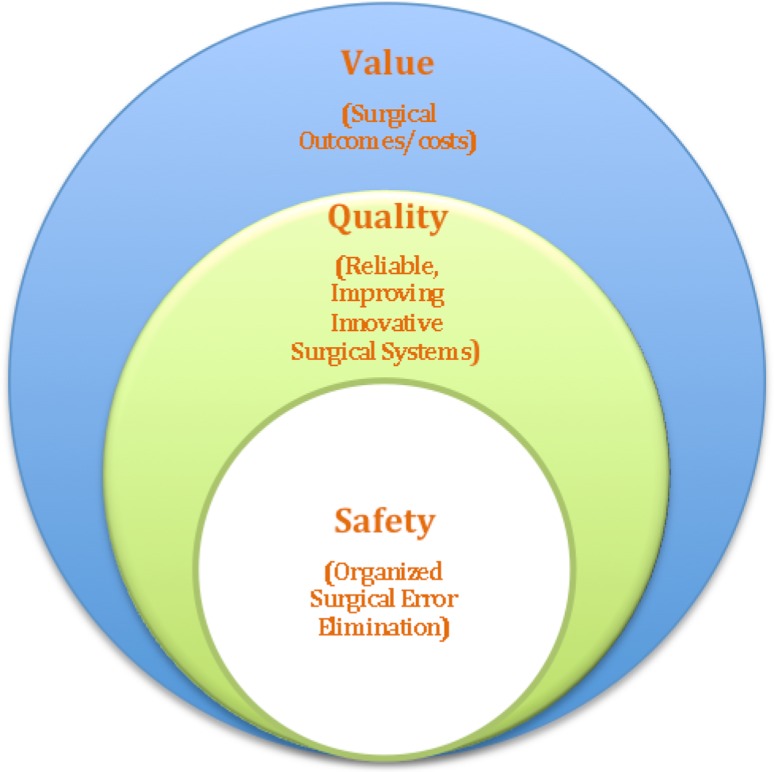
Patient safety and quality are essential components of contemporary healthcare delivery systems (Fig. 2). Surgical patient safety can be defined as highly organized systems of surgical care designed to minimize, with an ultimate goal to eliminate, preventable surgical harms. As such safety is a critical core element of surgical quality. Surgical quality can be defined as highly reliable, continually improving and innovative surgical care systems providing best possible surgical outcomes. Leadership and collaboration among orthopaedic surgeons, hospitals, ambulatory surgical centers (surgicenters), and healthcare systems are needed to foster the safest possible surgical environments and best-quality surgical patient care [44].
Fig. 2.
Surgical safety is the core of quality and value.
In 2011, the AAOS conducted a Surgical Safety Survey that uncovered several concerns regarding knowledge of surgical safety among orthopaedic surgeons [1]. The survey revealed a considerable number of orthopaedic surgeons had insufficient knowledge of UP and safety processes despite their common use in the hospital ORs. In surgicenters and office procedure rooms, time-outs and other standardized surgical safety processes were used by less than 50% of those surveyed. Although the survey included many orthopaedic leaders, few were engaged as safety leaders in their practices, surgicenters, hospitals, healthcare systems, or professional organizations. Younger surgeons were found to have less support and understanding of surgical team communication. Preventable surgical harm was reported in all orthopaedic practice settings with contemporary 2-year error rates consistent with historical error rates [1].
Six Critical Elements of Surgical Safety (Six C’s)
Based on the most frequent causes of surgical harm and error reported to TJC Sentinel Events Database, the following six important surgical safety elements have been identified: (1) communication, (2) consent, (3) checklists, (4) confirmation, (5) concentration, and (6) collection (Table 2). Knowledge and regular use of these six elements in orthopaedic surgical practice address the concerns identified in the AAOS 2011 Surgical Safety Survey by reducing preventable surgical harm and improving orthopaedic surgical care.
Table 2.
Six C’s of orthopaedic surgical safety
| Element | Description |
|---|---|
| 1. Communication | Efficient and reliable surgical team communication |
| 2. Consent | Accurate, timely, and fully informed surgical consent |
| 3. Checklists | Consistent use of evidence- or best-practice-based surgical workflows |
| 4. Confirmation | Redundant confirmation of proper surgical site, side, level, implant, procedure, and patient |
| 5. Concentration | Maintenance of a focused and distraction-free surgical environment |
| 6. Collection | Regular collection and analysis of surgical performance and outcome data |
Communication
Effective communication is paramount for reliable surgical team performance. Safe surgical communication requires transparent dialogue and effective teamwork among preoperative, OR, and recovery surgical team members. Critical care team training programs, such as TeamSTEPPS™, have demonstrated improved surgical performance and safety outcomes in OR and perioperative settings [22, 30, 36, 43]. Such team communication programs improve teamwork behaviors through the use of surgical briefings and debriefings, improved situation monitoring, and mutually supportive team communication [36, 43]. Successful surgical team training programs focus on team commitment to shared knowledge, skills, and attitudes. These observed improvements in teamwork rely on the team’s willingness to cooperate and communicate effectively while focusing on a common goal of achieving an optimal outcome for every surgical patient. The surgeon, who balances roles of team leader and collaborative team member, sets the tone and fosters the sustainability of efficient, effective, and transparent team communication.
Consent
Surgical consent is critically important for patient safety, as well as patient understanding and satisfaction. The consent document itself is used many times by all surgical team members as a key reference for surgical site, procedure, and patient confirmation during the UP process. The consent must be accurate, legible, understandable, and entered into the patient record in a timely manner before surgery. When inaccurate, surgical sentinel events have occurred, which have been reported to TJC, including wrong-site, -side, -level, -implant, -procedure, and -patient surgeries [41].
The consent process is also an important element of patient-centered care and patient-surgeon communication. Surgical information provided to patients should consider their best interest, level of understanding, and competence [2, 8]. A recent study [10] showed the comprehension and immediate recall after informed consent of patients undergoing orthopaedic surgery were unexpectedly low. Preoperative recall rates were accurate in only 71% of cases. Recall rates dropped to 59.5% at the time of the first postoperative visit. Postoperative recall was particularly low for older (53.8%) and less educated (53.7%) orthopaedic patients. Orthopaedic surgeons can improve patient understanding by testing recollection at key points during the consent discussion. In one study, patient recall was tested with a new consent requiring patients to describe the planned surgery in their own words. This increased patient participation and satisfaction compared with a traditionally patient-passive consent process [27]. Multiple orthopaedic studies [5, 9, 35] have demonstrated multimedia educational tools improve consent recall, particularly if the multimedia format is patient-centered and patient-interactive. Another study showed, if the time spent on the consent process was at least 10 minutes, patient comprehension improved by 7% and repetition of key consent elements increased comprehension by an additional 3% [13]. Several studies [19, 27] have shown patients who were satisfied with the consent process have better recall of the risks/benefits and realistic expectations of surgical outcomes.
Checklists
Checklists are validated, evidence- and/or consensus-based standardized surgical processes. TJC supports checklists as a component of their UP initiative. The UP requires presurgical procedure verification, surgical site marking, and a time-out performed immediately before the surgical procedure [42]. The WHO has demonstrated utility and effectiveness of checklists in their Safe Surgery Saves Lives program [17, 39]. Seventy-seven percent of orthopaedic OR team members in the WHO program believed checklists improved communication, compared with only 47% before WHO surgical safety program implementation [39]. An analysis of patient safety incidents in the United Kingdom National Health Service determined 21% of orthopaedic wrong-site surgery, including 83% of cases with identified harm, could have been prevented with use of the WHO surgical checklist [31].
Confirmation
Confirmation is the timely and accurate verification of the correct surgical site, side, level, implant, procedure, and patient. Compliance with proper surgical site verification and confirmation in orthopaedic settings has been reported as inconsistent or absent. In one recent study, the surgical time-out was performed before skin incision in only 70% of cases, after skin incision in 19%, or not at all in 11% of cases [20]. Wrong-site surgery continues to occur in orthopaedic surgery despite orthopaedic efforts to reduce these errors and prevent harm through the AAOS Sign Your Site program. The rate of wrong-site surgeries reported by candidates for certification by American Board of Orthopaedic Surgery from 1999 to 2005 did decrease during 2006 to 2010, but the improvement was not statistically significant. Despite compliance monitoring of Sign Your Site since 2007, surgery involving incorrect sites, sides, levels, implants, procedures, and patients continues to be reported at nearly the same historical rate [18]. The goal of elimination of wrong surgeries requires improved communication within the surgical team, standardized safety processes within the healthcare system, and active surgeon leadership [18, 40].
Concentration
Concentration among surgical team members fosters focused surgical team performance without distractions. Simple interruptions among surgical team members can be associated with increased errors through disruption and alteration of normal surgical team workflows. Nonurgent, unessential communication during surgery made up 26% of stressors to the surgeon in one study [4]. Despite recent reports on distractions in the OR [6, 32, 38], the impact of intraoperative stressors on performance has yet to be directly studied in orthopaedics.
Collection
Ongoing, regular collection of surgical safety, quality, and outcome data provides the foundation for surgical performance assessment. Reporting of preventable harm is infrequent by surgical team members, including surgeons [34, 37]. Data on the effects of interventions, such as checklists [39], on complications and mortality can help evaluate their efficacy. Complete and systematic reporting of preventable harm incidents by surgeons and surgical team members is essential for the establishment and maintenance of an effective surgical safety program. Incomplete data reporting undermines safety and limits observations that enable prevention or elimination of preventable surgical harm.
Surgeons as Safety Leaders Within the Hospital or Healthcare System
Orthopaedic surgeons are vital to establish a culture of safety within their own offices, surgicenters, hospitals, and healthcare systems. The traditional role of the surgeon as authoritative captain needs to be replaced by a surgical team leader who is an effective lead communicator and a collaborative team member (Table 1). Alignment with the patient safety goals of institutional leadership is also essential for successful surgical safety programs.
Preventable surgical harm has frequently been caused by ineffective, limited, inaccurate, or authoritative surgical team communication. In one study, failures of communication in the OR occurred in approximately 30% of team exchanges, and 1/3 of those failures resulted in effects that negatively impacted patient safety [24]. Similarly, poor communication has been cited as a major cause of incorrect surgery [29]. Communication techniques such as team briefings and debriefings have improved surgical performance and safety [25]. Borrowing concepts of crew resource management from aviation, team briefings address objectives, special interest items, and execution, allow for time to identify problems and knowledge gaps, and plan followup actions to protect the patient. Debriefings allow the team to learn from and improve the process by reconstructing the plan and events, finding negative root cause, generating lessons learned, and creating future plans to avoid negative root causes [26].
Effective team communication requires a collaborative tone among the surgeon and team members that reinforce teamwork values. Adopted by many hospital systems, the TeamSTEPPS™ training program reportedly improves surgical patient safety, efficiency, and surgical team member attitudes. One report in general surgery demonstrated first surgical cases starting on time improved from 69% to 81%, National Surgical Quality Improvement Program measure improvements (venous thromboembolism prophylaxis, antibiotic and beta-blocker administration), patient satisfaction from 77% to 83%, decreased mortality from 2.7% to 1%, and decreased morbidity from 20.2% to 11% [3]. Another study reported improved teamwork behaviors among trained teams that included improvements in preoperative briefings, situation monitoring, mutual support, and communication [43].
Within hospitals and healthcare systems, the organizational commitment to surgical patient safety is important to enable learning from adverse surgical patient safety events. Several researchers have found formal organizational commitment to patient safety is an important predictor of learning from events and dissemination of knowledge [11, 16, 30]. Administrative leadership support in smaller hospitals (< 100 beds) is particularly critical where formal leadership safety training is closely tied to successful implementation and maintenance of surgical patient safety programs [16]. Researchers observed improvements in surgical care when leadership was visible and close to the frontline of patient care and that perceived lack of administrative leadership was associated with less engagement in patient safety and infection control activities [14].
Formal team training programs for OR personnel within the Veterans Health Administration system compared performance of surgical teams trained for 2 months in safety processes compared to performance of teams without surgical team training. Both were challenged to identify safety risks, conduct checklist-guided preoperative briefings and postoperative debriefings, and implement other communication strategies. The trained surgical teams performed better, with a greater reduction in annual mortality (an 18% decrease compared to 7%) [30]. In another general surgery multihospital study, the use of a comprehensive safety system where the ward physician, nurse, surgeon, anesthesiologist, and operating assistant were all responsible for completion of selected surgical checklists of the surgical care pathway (preoperative, operative, recovery or intensive care, and postoperative periods of care), resulted in 10.6% fewer complications and decreased mortality (from 1.5% to 0.8%) [11]. The authors concluded every hospital, particularly those without high standard baselines of care, could benefit from implementation of a comprehensive safety system. Hospital systems that facilitate continuous safety monitoring, sharing of learning points from adverse or near-miss events, and supporting innovation opportunities among surgical teams are more likely to sustain a model of safety.
Discussion
Surgical patient safety is central to any surgical intervention and is critical to the delivery of quality surgical care. Without safe surgical care, there can be no surgical quality. Six key safety elements have been identified based on TJC Sentinel Events Database and serve as the basis for this orthopaedic surgical safety literature review. Investigation of the impact of orthopaedic surgery specific safety processes and programs has been limited. Orthopaedic surgeon leadership in development, refinement, and maintenance of patient safety programs is needed.
Readers should be aware of the limitations of the literature and this review. First, there are limited research and literature on orthopaedic surgery-specific patient safety systems or programs based on our search. Secondly, the differing study methodologies and levels of evidence in these reported orthopaedic articles make rigorous review, such as meta-analysis, impossible. These studies do, however, serve as a foundation for future research in the safety of patients undergoing orthopaedic surgery. Third, the use of Medical Subject Headings (MeSH®) terms may have inadvertently excluded some relevant studies. Review of the references in each article was performed to circumvent this limitation.
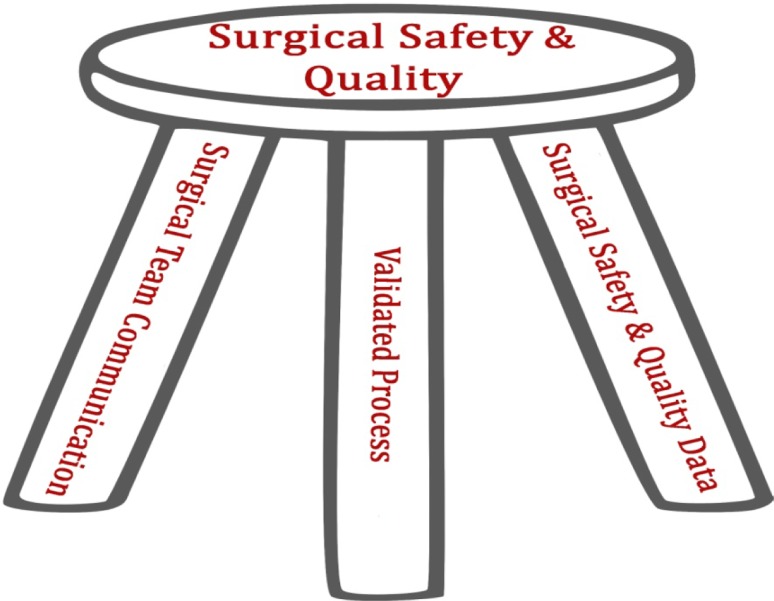
We have attempted to review and present available orthopaedic-specific patient safety scientific data focusing on surgical team communication, validated surgical safety processes, and systematic collection and analysis of surgical safety and quality data. These three safety components, when used together effectively, support a sustainable surgical safety model, as represented by the AAOS orthopaedic surgical safety and quality stool (Fig. 3). Currently, knowledge gaps exist among orthopaedic surgeons regarding surgical patient safety, as reported in the 2011 Surgical Safety Survey [1].
Fig. 3.
The AAOS Orthopaedic Surgical Safety and Quality Stool is shown.
The identified six C’s of surgical safety should provide a useful framework around which orthopaedic surgical safety programs can be built, tested, and validated based on their causative importance as reported in TJC Sentinel Event Database. Communication improvements through team training have been validated and shown to reduce adverse events in general surgery [3, 22, 30, 36, 43], but the effects of communication training for orthopaedic surgical teams has not been extensively studied [39].
Consent is a critical safety process element. It should effectively inform the patient and family and accurately describe the surgical site, side, level, implant, procedure, and patient. Although considerable literature demonstrates the value of informed surgeon-patient communication regarding consent [5, 9, 13, 19, 27, 35, 36], we found none that documented the utility of proper timely and accurate consent to reduce preventable surgical harm in orthopaedic surgery.
Surgical safety checklists have reduced mortality and complications in global populations in general surgery. In a prospective multicenter study before and after implementation of the WHO Surgical Safety Checklist, the rate of death decreased from 1.5% to 0.8% and complications decreased from 11% to 7% after the introduction of a surgical checklist [17]. Although the entire surgical team participates in the use of validated checklists, leadership from the surgeon is required to ensure all checklist elements are consistently and accurately verified during each procedure. Only one study included orthopaedic patients regarding use of the WHO Checklist [39]. In the short study period, statistically significant improvements in orthopaedic mortality or complications were not observed despite improvements in team behavior and performance. Further investigations could elucidate the impact of surgical checklists on complications or mortality; no reports were found to date in the orthopaedic literature.
Confirmation of the correct site, side, level, implant, procedure, and patient is needed in all orthopaedic settings to minimize preventable harm. Compliance with this important process has been performed inconsistently in some orthopaedic surgeries and not at all in some others in one report [20]. UP/time-out effectiveness requires not merely completion of the time-out but also surgeon leadership to ensure the time-out is a focused communication tool for all surgical team members. Although confirmation was the original safety process measure introduced by the Sign Your Site program in 1997 by the AAOS, an effective confirmation process in orthopaedic settings in reducing preventable harm has yet to be demonstrated.
An OR environment conducive to concentration is another critical element of safety. The sterile cockpit has been used for years in aviation and decreases errors during critical phases of flight such as take-off, landings, or emergencies [12]. A similar method can be applied to the OR where team members refrain from nonessential activities, particularly during critical portions of the surgical procedure. Two-thirds of irrelevant communication during surgery in one study has involved the surgeon [38]. Such distractions can degrade the performance of the surgeon and the entire surgical team [6]. In more complex surgical cases, such as those involving patients with unstable trauma, greater levels of noise have been demonstrated to increase surgical team distraction. In one study, noise levels averaged 85 dB during general trauma surgery, higher than pronounced voice efforts under normal conditions (66 dB) [32]. No analysis was identified on the association of the inability to hear or communicate during critical moments in surgery with preventable surgical harm incidents. Research to date in orthopaedic settings assessing the impact of distraction on surgical performance is limited to one study [4].
Collection of data on safety performance has not been a focus in orthopaedics. State-based databases have been utilized in other surgical specialties [15] to study adverse events. National databases, such as the National Surgical Quality Improvement Program [21], contain orthopaedic modules that have not been utilized widely by the orthopaedic community to study the effects of orthopaedic safety or quality interventions. Our review highlights the need for safety data collection to assess which safety processes and programs are most efficacious for orthopaedic patients.
What is needed to foster a culture of patient safety? First, the surgeon and surgical team can critically evaluate their current OR environment, existing surgical patient safety programs, and the measurements available to evaluate surgical outcomes. Orthopaedic surgical care requires support by all three legs needed to build a balanced and strong sustainable safety stool (Fig. 3). Has the OR team had surgical team communication training and is it being used? Have surgical checklists and standardized surgical processes been developed and implemented? Are they used with continual updating? Is the OR environment conducive to focused team performance without distraction? Is there active safety monitoring with data collection and compliance with performance evaluation? The surgeon is critical to the promotion and maintenance of a culture of surgical patient safety. Furthermore, a successful surgical patient safety program requires the entire surgical team to continually advance and actively innovative its care processes to reduce surgical harms and improve surgical quality.
In summary, the orthopaedic surgeon is a key leader working with administrative leadership and surgical team members in offices, surgicenters, hospitals, and healthcare systems to ensure safe and optimal surgical patient outcomes occur in every orthopaedic setting. A new model for the safety of patients undergoing orthopaedic surgery is presented based on available TJC data and orthopaedic literature review. Six key surgical safety elements are described: communication, consent, checklists, confirmation, concentration, and collection. Orthopaedic surgeon leadership, combined with successful hospital alignment and collaboration, is required to share these common goals, vision, and responsibilities that promote and maintain the safest possible environment for every patient.
Footnotes
Each author certifies that he or she, or a member of his or her immediate family, has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
This work was performed at NorthShore University HealthSystem, Evanston, IL, USA.
References
- 1.Surgical Safety Survey. Rosemont, IL: American Academy of Orthopaedic Surgeons; 2011. [Google Scholar]
- 2.Appelbaum PS. Clinical practice. Assessment of patients’ competence to consent to treatment. N Engl J Med. 2007;357:1834–1840. doi: 10.1056/NEJMcp074045. [DOI] [PubMed] [Google Scholar]
- 3.Armour Forse R, Bramble JD, McQuillan R. Team training can improve operating room performance. Surgery. 2011;150:771–778. doi: 10.1016/j.surg.2011.07.076. [DOI] [PubMed] [Google Scholar]
- 4.Arora S, Hull L, Sevdalis N, Tierney T, Nestel D, Woloshynowych M, Darzi A, Kneebone R. Factors compromising safety in surgery: stressful events in the operating room. Am J Surg. 2010;199:60–65. doi: 10.1016/j.amjsurg.2009.07.036. [DOI] [PubMed] [Google Scholar]
- 5.Beamond BM, Beischer AD, Brodsky JW, Leslie H. Improvement in surgical consent with a preoperative multimedia patient education tool: a pilot study. Foot Ankle Int. 2009;30:619–626. doi: 10.3113/FAI.2009.0619. [DOI] [PubMed] [Google Scholar]
- 6.Broom MA, Capek AL, Carachi P, Akeroyd MA, Hilditch G. Critical phase distractions in anaesthesia and the sterile cockpit concept. Anaesthesia. 2011;66:175–179. doi: 10.1111/j.1365-2044.2011.06623.x. [DOI] [PubMed] [Google Scholar]
- 7.Canale ST. Wrong-site surgery: a preventable complication. Clin Orthop Relat Res. 2005;433:26–29. doi: 10.1097/01.blo.0000159827.93813.53. [DOI] [PubMed] [Google Scholar]
- 8.Capozzi J, Rhodes R, Chen D. Discussing treatment options. J Bone Joint Surg Am. 2009;91:740–742. doi: 10.2106/JBJS.H.01104. [DOI] [PubMed] [Google Scholar]
- 9.Cornoiu A, Beischer AD, Donnan L, Graves S, de Steiger R. Multimedia patient education to assist the informed consent process for knee arthroscopy. ANZ J Surg. 2011;81:176–180. doi: 10.1111/j.1445-2197.2010.05487.x. [DOI] [PubMed] [Google Scholar]
- 10.Crepeau AE, McKinney BI, Fox-Ryvicker M, Castelli J, Penna J, Wang ED. Prospective evaluation of patient comprehension of informed consent. J Bone Joint Surg Am. 2011;93:e114(1–7). [DOI] [PubMed]
- 11.de Vries EN, Prins HA, Crolla RM, den Outer AJ, van Andel G, van Helden SH, Schlack WS, van Putten MA, Gouma DJ, Dijkgraaf MG, Smorenburg SM, SURPASS Collaborative Group Effect of a comprehensive surgical safety system on patient outcomes. N Engl J Med. 2010;363:1928–1937. doi: 10.1056/NEJMsa0911535. [DOI] [PubMed] [Google Scholar]
- 12.Federal Aviation Administration. Flight crewmember duties. FAR 121.542. Available at: http://ecfr.gpoaccess.gov/cgi/t/text/text-idx?c=ecfr&sid=21fa54465a4bfaebbc18090246f44bb4&rgn=div8&view=text&node=14:3.0.1.1.7.20.3.8&idno=14. Accessed October 11, 2012.
- 13.Fink AS, Prochazka AV, Henderson WG, Bartenfeld D, Nyirenda C, Webb A, Berger DH, Itani K, Whitehill T, Edwards J, Wilson M, Karsonovich C, Parmelee P. Predictors of comprehension during surgical informed consent. J Am Coll Surg. 2010;210:919–926. doi: 10.1016/j.jamcollsurg.2010.02.049. [DOI] [PubMed] [Google Scholar]
- 14.Fukuda H, Imanaka Y, Hirose M, Hayashida K. Factors associated with system-level activities for patient safety and infection control. Health Policy. 2009;89:26–36. doi: 10.1016/j.healthpol.2008.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gawande AA, Thomas EJ, Zinner MJ, Brennan TA. The incidence and nature of surgical adverse events in Colorado and Utah in 1992. Surgery. 1999;126:66–75. doi: 10.1067/msy.1999.98664. [DOI] [PubMed] [Google Scholar]
- 16.Ginsburg LR, Chuang YT, Berta WB, Norton PG, Ng P, Tregunno D, Richardson J. The relationship between organizational leadership for safety and learning from patient safety events. Health Serv Res. 2010;45:607–632. doi: 10.1111/j.1475-6773.2010.01102.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Haynes AB, Weiser TG, Berry WR, Lipsitz SR, Breizat AH, Dellinger EP, Herbosa T, Joseph S, Kibatala PL, Lapitan MC, Merry AF, Moorthy K, Reznick RK, Taylor B, Safe Surgery Saves Lives Study Group A surgical safety checklist to reduce morbidity and mortality in a global population. N Engl J Med. 2009;360:491–499. doi: 10.1056/NEJMsa0810119. [DOI] [PubMed] [Google Scholar]
- 18.James MA, Seiler JG 3rd, Harrast JJ, Emery SE, Hurwitz S. The occurrence of wrong-site surgery self-reported by candidates for certification by the American Board of Orthopaedic Surgery. J Bone Joint Surg Am. 2012;94:e2(1–12). [DOI] [PubMed]
- 19.Johnson MR, Singh JA, Stewart T, Gioe TJ. Patient understanding and satisfaction in informed consent for total knee arthroplasty: a randomized study. Arthritis Care Res (Hoboken). 2011;63:1048–1054. doi: 10.1002/acr.20475. [DOI] [PubMed] [Google Scholar]
- 20.Johnston G, Ekert L, Pally E. Surgical site signing and “time out”: issues of compliance or complacence. J Bone Joint Surg Am. 2009;91:2577–2580. doi: 10.2106/JBJS.H.01615. [DOI] [PubMed] [Google Scholar]
- 21.Khuri SF, Daley J, Henderson W, Barbour G, Lowry P, Irvin G, Gibbs J, Grover F, Hammermeister K, Stremple JF. The National Veterans Administration Surgical Risk Study: risk adjustment for the comparative assessment of the quality of surgical care. J Am Coll Surg. 1995;180:519–531. [PubMed] [Google Scholar]
- 22.King HB, Battles J, Baker DP, Alonso A, Salas E, Webster J, Toomey L, Salisbury M. TeamSTEPPS™: team strategies and tools to enhance performance and patient safety. In: Henriksen K, Battles J, Keyes M, Grady M, editors. Advances in Patient Safety: New Directions and Alternative Approaches (Vol 3: Performance and Tools) Rockville, MD: Agency for Healthcare Research and Quality; 2008. [PubMed] [Google Scholar]
- 23.Kohn LT, Corrigan JM, Donaldson MS. To Err Is Human: Building a Safer Health System. Washington DC: National Academy Press; 2000. [PubMed] [Google Scholar]
- 24.Lingard L, Espin S, Whyte S, Regehr G, Baker GR, Reznick R, Bohnen J, Orser B, Doran D, Grober E. Communication failures in the operating room: an observational classification of recurrent types and effects. Qual Saf Health Care. 2004;13:330–334. doi: 10.1136/qshc.2003.008425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lingard L, Regehr G, Orser B, Reznick R, Baker GR, Doran D, Espin S, Bohnen J, Whyte S. Evaluation of a preoperative checklist and team briefing among surgeons, nurses, and anesthesiologists to reduce failures in communication. Arch Surg. 2008;143:12–17. doi: 10.1001/archsurg.2007.21. [DOI] [PubMed] [Google Scholar]
- 26.McGreevy JM, Otten TD. Briefing and debriefing in the operating room using fighter pilot crew resource management. J Am Coll Surg. 2007;205:169–176. doi: 10.1016/j.jamcollsurg.2007.03.006. [DOI] [PubMed] [Google Scholar]
- 27.Miller MJ, Abrams MA, Earles B, Phillips K, McCleeary EM. Improving patient-provider communication for patients having surgery: patient perceptions of a revised health literacy-based consent process. J Patient Saf. 2011;7:30–38. doi: 10.1097/PTS.0b013e31820cd632. [DOI] [PubMed] [Google Scholar]
- 28.Neily J, Mills PD, Eldridge N, Carney BT, Pfeffer D, Turner JR, Young-Xu Y, Gunnar W, Bagian JP. Incorrect surgical procedures within and outside of the operating room: a follow-up report. Arch Surg. 2011;146:1235–1239. doi: 10.1001/archsurg.2011.171. [DOI] [PubMed] [Google Scholar]
- 29.Neily J, Mills PD, Eldridge N, Dunn EJ, Samples C, Turner JR, Revere A, DePalma RG, Bagian JP. Incorrect surgical procedures within and outside of the operating room. Arch Surg. 2009;144:1028–1034. doi: 10.1001/archsurg.2009.126. [DOI] [PubMed] [Google Scholar]
- 30.Neily J, Mills PD, Young-Xu Y, Carney BT, West P, Berger DH, Mazzia LM, Paull DE, Bagian JP. Association between implementation of a medical team training program and surgical mortality. JAMA. 2010;304:1693–1700. doi: 10.1001/jama.2010.1506. [DOI] [PubMed] [Google Scholar]
- 31.Panesar SS, Noble DJ, Mirza SB, Patel B, Mann B, Emerton M, Cleary K, Sheikh A, Bhandari M. Can the surgical checklist reduce the risk of wrong site surgery in orthopaedics? Can the checklist help? Supporting evidence from analysis of a national patient incident reporting system. J Orthop Surg Res. 2011;6:18. doi: 10.1186/1749-799X-6-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pereira BM, Pereira AM, Cdos SC, Marttos AC, Fiorelli RK, Fraga GP. Interruptions and distractions in the trauma operating room: understanding the threat of human error. Rev Col Bras Cir. 2011;38:292–298. doi: 10.1590/S0100-69912011000500002. [DOI] [PubMed] [Google Scholar]
- 33.Raheja D. Safer Hosptial Care: Strategies for Continuous Innovation. New York, NY: CRC Press; 2011. [Google Scholar]
- 34.Robinson PM, Muir LT. Wrong-site surgery in orthopaedics. J Bone Joint Surg Br. 2009;91:1274–1280. doi: 10.2106/JBJS.H.00409. [DOI] [PubMed] [Google Scholar]
- 35.Rossi MJ, Guttmann D, MacLennan MJ, Lubowitz JH. Video informed consent improves knee arthroscopy patient comprehension. Arthroscopy. 2005;21:739–743. doi: 10.1016/j.arthro.2005.02.015. [DOI] [PubMed] [Google Scholar]
- 36.Salas E, Diaz Granados D, Klein C, Burke CS, Stagl KC, Goodwin GF, Halpin SM. Does team training improve team performance? A meta-analysis. Hum Factors. 2008;50:903–933. doi: 10.1518/001872008X375009. [DOI] [PubMed] [Google Scholar]
- 37.Seiden SC, Barach P. Wrong-side/wrong-site, wrong-procedure, and wrong-patient adverse events: are they preventable? Arch Surg. 2006;141:931–939. doi: 10.1001/archsurg.141.9.931. [DOI] [PubMed] [Google Scholar]
- 38.Sevdalis N, Healey AN, Vincent CA. Distracting communications in the operating theatre. J Eval Clin Pract. 2007;13:390–394. doi: 10.1111/j.1365-2753.2006.00712.x. [DOI] [PubMed] [Google Scholar]
- 39.Sewell M, Adebibe M, Jayakumar P, Jowett C, Kong K, Vemulapalli K, Levack B. Use of the WHO surgical safety checklist in trauma and orthopaedic patients. Int Orthop. 2011;35:897–901. doi: 10.1007/s00264-010-1112-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Stahel PF, Sabel AL, Victoroff MS, Varnell J, Lembitz A, Boyle DJ, Clarke TJ, Smith WR, Mehler PS. Wrong-site and wrong-patient procedures in the universal protocol era: analysis of a prospective database of physician self-reported occurrences. Arch Surg. 2010;145:978–984. doi: 10.1001/archsurg.2010.185. [DOI] [PubMed] [Google Scholar]
- 41.The Joint Commission. Sentinel Event Database. Available at: http://www.jointcommission.org/sentinel_event.aspx. Accessed October 11, 2012.
- 42.The Joint Commission. Universal Protocol. Available at: http://www.jointcommission.org/standards_information/up.aspx. Accessed April 22, 2012.
- 43.Weaver SJ, Rosen MA, Diaz Granados D, Lazzara EH, Lyons R, Salas E, Knych SA, McKeever M, Adler L, Barker M, King HB. Does teamwork improve performance in the operating room? A multilevel evaluation. Jt Comm J Qual Patient Saf. 2010;36:133–142. doi: 10.1016/s1553-7250(10)36022-3. [DOI] [PubMed] [Google Scholar]
- 44.Wilson NA, Ranawat A, Nunley R, Bozic KJ. Aligning stakeholder incentives in orthopaedics. Clin Orthop Relat Res. 2009;467:2521–2524. doi: 10.1007/s11999-009-0909-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Wong DA, Herndon JH, Canale ST, Brooks RL, Hunt TR, Epps HR, Fountain SS, Albanese SA, Johanson NA. Medical errors in orthopaedics: results of an AAOS member survey. J Bone Joint Surg Am. 2009;91:547–557. doi: 10.2106/JBJS.G.01439. [DOI] [PubMed] [Google Scholar]