Abstract
Objective
The purpose of this case study is to describe the chiropractic management of chronic low back pain in a patient with adjacent segment disease.
Clinical Features
The patient was a 30-year-old man with a 3-year history of chronic nonspecific low back pain following a lumbar disk herniation. Two years before this incident, he had severe lumbar fractures and cauda equina injury due to an aviation accident that required multilevel lumbar fusion surgery, vertebrectomy, and cage reconstruction.
Intervention and Outcome
The patient received chiropractic management using Cox Flexion Distraction over a 4-week period. A complete reduction of symptoms to 0/10 on a verbal numerical rating scale was achieved within 4 weeks. At 3 months, the patient was able to work 8 to 9 hours per day in his dental practice with no pain. At 9 months, the patient continued to report a complete reduction of symptoms.
Conclusions
This report describes the successful management of a patient with chronic low back pain associated with adjacent segment disease using Cox Flexion Distraction protocols.
Key indexing terms: Manipulation, chiropractic; Back pain; Spinal fusion; Failed back surgery syndrome; Complementary therapies
Introduction
The term adjacent segment degeneration was used by Hilibrand and Robbins to describe radiographic changes seen at levels adjacent to a previous spinal fusion procedure, which do not necessarily correlate with any clinical findings. The term adjacent segment disease (ASD), also used by Hilibrand and Robbins, has been used to designate the development of new clinical symptoms that are compatible with radiographic changes adjacent to the level of spinal fusion.1
Cox Flexion Distraction (FD) is a low-velocity manipulative procedure that is applied using a specialized treatment instrument along with manual contact by a specially trained chiropractic practitioner (Fig 1). The goal of treatment is to decrease intradiskal pressure, increase disk height, increase intervertebral foraminal diameter, improve physiologic ranges of motion to the vertebral motor unit, and afferentation of associated neural structures.2
Fig 1.

The Cox7 Adjusting Instrument. (Color version of figure is available online.)
Flexion distraction therapy has been shown to be effective in the treatment of low back pain.3,4 In a recent survey, 64% of all chiropractors in North America indicate use of Cox FD therapy in practice.5 A literature search found a recent case report of chiropractic management of ASD using FD.6,7
The purpose of this case study is to report on the chiropractic management of a patient with chronic low back pain associated with ASD using Cox FD.
Case report
Presenting complaint
A 34-year-old male dentist presented with chronic, right-sided lower back and hip pain of 3 years’ duration. The patient characterized the pain as sharp, stabbing, and continuous. Long periods of sitting or standing exacerbated the condition. Low back exercises along with general conditioning exercises prescribed by a physiotherapist gave no improvement. The patient was asked to verbally rate his subjective experience of pain on a 0 to 10 scale with 0 being no pain and 10 being a great deal of pain. A verbal numerical rating of his chronic pain was recorded as 6 out of 10 and correlates with the experience of moderate pain. At the time of examination, the patient had been in good health with no other symptoms.
History
This patient had been involved in an aviation crash during takeoff of a small private airplane, resulting in numerous serious injuries 8 years before seeking care. At the time of the accident, this patient was flown to a regional trauma center where he was diagnosed with lumbar spine burst fracture (Fig 2A, B, and C) with compression of the cauda equina (Fig 3), a fractured odontoid process, and a right tibial pilon fracture. The lumbar spine injury caused paralysis in both lower extremities. Multiple surgical procedures were performed over several weeks including spinal fusion using rods and screws between T11 and L4 (Fig 4), debridement and irrigation of deep spinal wound infection, and vertebrectomy of L1-2 with cage reconstruction to remove bone fragments causing cauda equina compression (Fig 4). The initial surgery did not improve neurologic deficits. A follow-up cage reconstruction surgery was successful, and the patient regained motor control of the legs and was able to walk with the assistance of a cane 4 months postsurgery. The patient subsequently began a career as a dentist. Two years after surgery, the patient experienced an L4-5 disk herniation of insidious onset resulting in chronic low back pain below the level of the fusion. There were no neurologic complications as a result of the herniation. The patient's spine surgeon suggested that additional surgery may be necessary in the future to stabilize the region below the original fusion. Reluctant to consider further surgery, the patient opted for a conservative approach including exercises prescribed by a physiotherapist, which gave no relief.
Fig 2.
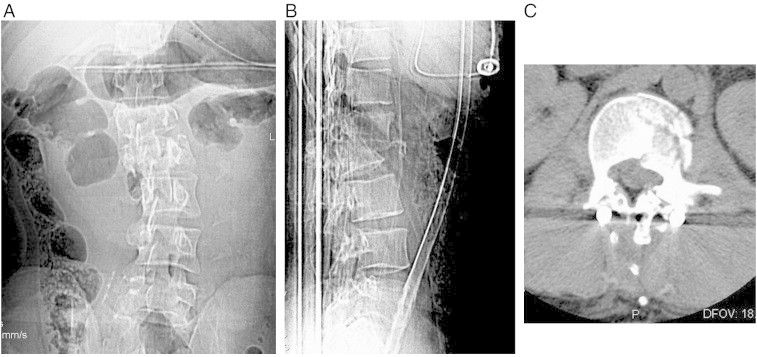
(A) Anteroposterior radiograph; initial presentation to trauma center. (B) Lateral radiograph; initial presentation. (C) Axial computed tomographic image of L2 burst fracture; initial presentation.
Fig 3.
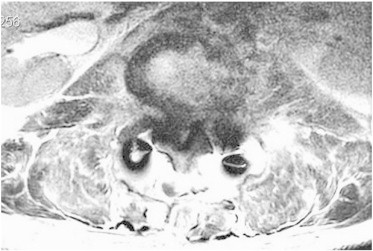
Axial magnetic resonance image of L2 postfusion demonstrating signal abnormality and mass lesion with significant compromise of the cauda equina within the central canal 5 weeks posttrauma.
Fig 4.

Postfusion lateral radiograph; 5 weeks posttrauma (observe the normal spacing between L4 and 5).
Examination
The patient presented with a 10° right lumbar lean with a slightly flexed lumbar spine, and movements were deliberate and somewhat guarded. Musculature around the lumbar spine was hypertonic and tender to palpation. Palpation of the spinous processes of L4 and L5 elicited pain locally. Range of motion of the lumbar spine was reduced with left and right lateral flexion to 10°, flexion to 30°, and extension to 10°. Heel/toe walk was normal, although balance was reduced on the right lower extremity. Deep tendon reflexes were 0 bilaterally for the Achilles, patella, and hamstring; but lower extremity strength was preserved at 5/5 bilaterally for hip flexors, hamstrings, and quadriceps and 4/5 bilaterally for extensor hallucis longus, tibialis anterior, and gastrocnemius. Result of sensory testing was normal with Wartenberg pinwheel at the ankles bilaterally. Babinski reflexes were absent bilaterally. Straight leg raise test result was negative for sciatic tension. Hip flexion was reduced to 30° bilaterally because of hamstring tightness. Soto-Hall test result was negative.
Diagnostic imaging
The most recent images available (Fig 5A and B) showed degenerative disk changes at the level of L4-L5, immediately caudal to the posterior rod and screw fusion. There are right lateral inferior disk wedging of the L4-5 disk, left lateral listhesis of L4 measuring 3 to 4 mm, retrolisthesis of L4 relative to L5 measuring 4 to 5 mm, and severe posterior disk space narrowing at L4-5.
Fig 5.
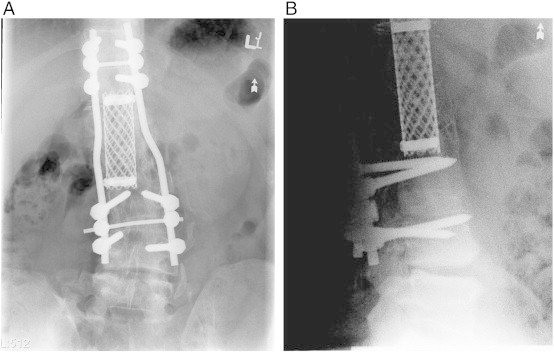
(A) Anteroposterior lumbar spine 8 years postvertebrectomy showing expandable cage (observe lateral disk wedging and lateral listhesis). (B) Lateral lumbar spine 8 years postvertebrectomy (observe disk space narrowing, subchondral sclerosis, and retrolisthesis of L4 on L5).
Diagnosis
The diagnosis supported by the history, examination, and diagnostic imaging was symptomatic degenerative disk disease at L4-5 at the segment immediately below the level of spinal fusion or ASD of L4-5.
Treatment
Flexion distraction treatment was applied following careful tolerance testing while the patient lay prone on the Cox7 Adjusting Instrument8 (Fig 1). Flexion of the lumbar spine was applied initially with no ankle restraints used and very light practitioner contact at the lamina pedicle junction of L4, just above the level of ASD. The effect of this contact was to isolate the tractive force of the treatment to the L4-5 segment. The area of spinal fusion was stabilized in this manner. The caudal section of the table was flexed to approximately 10° to the point that tautness was felt at the L4-5 segmental level and to the patient's tolerance. This procedure was repeated 5 times in 4-second intervals followed by a short rest, and this cycle was repeated 3 times. Flexion distraction was similarly applied 2 to 3 times per week for 4 weeks. After 4 weeks and 10 treatments, treatment was reduced to 1 time per week for 2 weeks.
Outcome
A complete reduction of symptoms to 0/10 on the verbal numerical rating scale was achieved within 4 weeks. At 3 months, the patient was able to work 8 to 9 hours per day in his dental practice with no pain. Minor stiffness in the lumbar spine was reported occasionally after long periods of flexion, which abated with rest. At 9 months, the patient continues to report a complete reduction of symptoms.
Discussion
There is ongoing research to evaluate the outcomes of spinal fusion surgery and strategies that may be used in managing ASD.9-11 The incidence of ASD is not considered to be high, but it is now reported to be accepted as a long-term complication of spinal surgery and a very important factor in determining the long-term consequences of spinal fusion.9 The wide range of variables associated with ASD such as level of original fusion, reason for surgery, the extent of fusion, age of patient, and prior degenerative changes may affect outcome measurements. There may also be surgical options available to improve the negative consequences of ASD; but these procedures are accompanied by additional risk to patients, and the outcomes must be studied over time to determine appropriateness and safety.10
The risk of ASD has been shown to be higher in patients with posterior fusion procedures, in those with a longer fusion including the L4 or L5 segments, and in those older than 50 years.11
There was an increase in the use of spinal fusion for common lower back complaints in the United States between 1991 and 2003.12 This may be a contributing factor to a higher reported incidence of ASD. Spinal fusion surgery for the purpose of managing destructive pathology or severe spinal trauma may be necessary to prevent lifelong disability or paralysis.13,14 In cases such as these, ASD is likely to be a nonissue in the surgical decision-making process.
Flexion distraction manipulation has been shown to improve biomechanical function at the vertebral motion segment including the disk and posterior facet joints. The improvement of joint function associated with chiropractic manipulation diminishes aberrant mechanical stimuli from a degenerative or dysfunctional joint complex, allowing relaxation of local musculature and decreasing subjective pain. Improved joint function may also lessen contractural changes of musculoligamentous structures, thereby permitting adequate rehabilitation of intersegmental muscles. The goal is to prevent future degenerative change due to instability, aberrant joint function, and chronic inflammation.
Aviation-related injuries resulted in approximately 1000 hospitalizations each year in the United States between 2000 and 2005, with an in-hospital mortality rate of 2%.15 An average of 40 serious aviation-related injuries per year were reported in Canada between 2000 and 2009.16
Spinal injuries requiring lumbar fusion surgical procedures in this population represent a statistically low number in relation to all cases of ASD. This case provides a very dramatic presentation and sequela leading to ASD and the role of FD manipulation in the management of ASD. By adding to the literature, new conservative, cost-effective standards of care may be developed for the treatment of back pain associated with ASD.
This case report is intended to demonstrate to doctors of chiropractic, spinal surgeons, and other health care providers that there is a possible alternative to spinal surgery for the management of chronic low back pain associated with some cases of ASD. More research into the relationship of ASD and lumbar fusion surgery, as well as the role of FD manipulation in the management of ASD, is needed. A clinical trial using FD for symptoms related to ASD should be undertaken to statistically assess the benefits of this form of care.
Limitations
The outcomes of this case study are not necessarily generalizable to other cases. Limitations exist because this is a retrospective, single-case study. As well, bias may exist because the author is a certified Cox Technique practitioner. The outcome measurements are subjective in nature and may be construed as unreliable. There may also exist the possibility of placebo effect given that the patient was motivated to avoid further surgery and his expectations of benefit may have been high.
Conclusion
This report describes the successful management of a unique case of chronic low back pain associated with ASD using Cox FD protocols in an aviation crash survivor with multilevel lumbar fusion.
Funding sources and potential conflicts of interest
There were no funding sources or conflicts of interest in the preparation of this report.
References
- 1.Hillibrand A.D., Robbins M. Adjacent segment degeneration and adjacent segment disease: the consequences of spinal fusion? Spine. 2004;4:190S–194S. doi: 10.1016/j.spinee.2004.07.007. [DOI] [PubMed] [Google Scholar]
- 2.Cox J.M., Feller J., Cox-Cid J. Distraction chiropractic adjusting: clinical application and outcomes of 1000 cases. Top Clin Chiropr. 1996;3(3):45–59. [Google Scholar]
- 3.Cambron J.A., Gudvalli R.M., Hedeker D., McGregor M., Jelicka J., Keenum M. One year follow up of a randomized clinical trial comparing flexion distraction with an exercise program for chronic low back pain. J Altern Complement Med. 2006;12:659–668. doi: 10.1089/acm.2006.12.659. [DOI] [PubMed] [Google Scholar]
- 4.Lillie G.R. Resolution of low back and radicular pain in a 40-year-old male United States Navy Petty Officer after collaborative medical and chiropractic care. J Chiropr Med. 2010;9(1):17–21. doi: 10.1016/j.jcm.2009.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.National Board of ChiropracticExaminers . A project report, survey analysis, and summary of the practice of chiropractic within the United States. NBCE; Greeley (Colo): 2010. [Google Scholar]
- 6.Kruse R.A., Cambron J.A. Cox decompression chiropractic manipulation of a patient with postsurgical lumbar fusion: a case report. J Chiropr Med. 2011;10(4):255–260. doi: 10.1016/j.jcm.2011.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kruse R.A., Cambron J. Chiropractic management of postsurgical lumbar spine pain: a retrospective study of 32 cases. J Manipulative Physiol Ther. 2011;34(6):408–412. doi: 10.1016/j.jmpt.2011.05.011. [DOI] [PubMed] [Google Scholar]
- 8.Cox J. Low back pain: mehanisms, diagnosis and treatment. 6th ed. Williams and Wilkins; Baltimore, MD: 1999. pp. 288–299. [Google Scholar]
- 9.Liu C.Y., Xia T., Tian J.W. New progress in adjacent segment degeneration/disease. Orthop Surg. 2010;2:182–186. doi: 10.1111/j.1757-7861.2010.00084.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bertagnoli R., Yue J.J., Fenk-Mayer A. Treatment of symptomatic adjacent-segment degeneration after lumbar fusion with total disc arthroplasty by using the ProDisc prosthesis: a prospective study with 2-year minimum follow up. J Neurosurg Spine. 2006;4:91–97. doi: 10.3171/spi.2006.4.2.91. [DOI] [PubMed] [Google Scholar]
- 11.Cheh G., Bridwell K.H., Lenke L.G., Buchowski J.M., Daubs M.D., Kim Y. Adjacent segment disease following lumbar/thoracolumbar fusion with pedicle screw instrumentation: a minimum 5-year follow-up. Spine (Phila Pa 1976) 2007;32(20):2253–2257. doi: 10.1097/BRS.0b013e31814b2d8e. [DOI] [PubMed] [Google Scholar]
- 12.Weinstein J., Lurie J.D., Olson P., Bonner K., Fisher E.S., Morgan T.S. United States trends and regional variations in lumbar spine surgery: 1992-2003. Spine. 2006;31:2707–2714. doi: 10.1097/01.brs.0000248132.15231.fe. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kingwell S.P., Curt A., Dvorak M.F. Factors affecting neurological outcome in traumatic conus medullaris and cauda equina injuries. Neurosurg Focus. 2008;25:E7. doi: 10.3171/FOC.2008.25.11.E7. [DOI] [PubMed] [Google Scholar]
- 14.Shen F.H., Marks I., Shaffrey C., Ouellet J., Arlet V. The use of an expandable cage for corpectomy reconstruction of vertebral body tumors through a posterior extracavitary approach: a multicenter consecutive case series of prospectively followed patients. Spine. 2008;8:329–339. doi: 10.1016/j.spinee.2007.05.002. [DOI] [PubMed] [Google Scholar]
- 15.Baker S.P., Brady J.E., Shanahan D.F., Li G. Aviation-related injury morbidity and mortality: data from U.S. health information systems. Aviat Space Environ Med. 2009;80:1001–1005. doi: 10.3357/asem.2575.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Transportation Safety Board of Canada, Statistical summary aviation occurrences 2009; Appendix A. Available from: http://www.tsb.gc.ca/eng/stats/aviation/index.asp.


