Abstract
Recent publication of the global epidemiology of clonorchiasis and its relationship with cholangiocarcinoma in the journal of Infectious Diseases of Poverty has stressed the importance of Clonorchis sinensis infection. To further demonstrate its threat on public health, especially in China, comparisons between clonorchiasis and hepatitis B are made in terms of epidemiology, clinical symptoms and carcinogenicity, disability, as well as changing trends. Furthermore, major problems and prioritized researches are argued, from basic biology to intervention. Imbalance between the majority of infected population and the minority of researches in China urges for more work from Chinese scientists and international cooperation.
Keywords: Clonorchis sinensis, Clonorchiasis, Hepatitis B virus, Liver cancer, Research
Multilingual abstracts
Please see Additional file 1 for translations of the abstract into the six official working languages of the United Nations.
Background
A review on the global epidemiology of clonorchiasis and its relationship with cholangiocarcinoma (CCA) was published in the journal of Infectious Diseases of Poverty on 25th October 2012 [1]. A total of 15 million people are estimated to be infected with Clonorchis sinensis in East Asia and nearly 5,000 CCA cases attributed to this infection may occur annually in the coming decades. That article seeks to elucidate the situation and impact of clonorchiasis. However, some more deserve to be discussed, especially in China.
Discussion
Comparisons between clonorchiasis and hepatitis B in China
Clonorchiasis ranks among the top neglected tropical diseases [2]. Thus, comparing it with hepatitis B will promote revealing its threat on public health in China.
Firstly, most people infected with hepatitis B virus (HBV) distribute in China, and so do C. sinensis infections. A total population of 93 million is infected with HBV in China, which is about one quarter of the global number [3,4], while out of 15 million with C. sinensis infection globally, over 85% distributes in China (Figure 1A) [1]. Even after including another liver fluke infection, opisthorchiasis, the number in China is still over 50% (Figure 2B) [1,5,6]. Similar distribution characteristics in sexes and ages are shown in both infections, namely higher prevalence in males than in females and in adults than in children [1,7].
Figure 1.
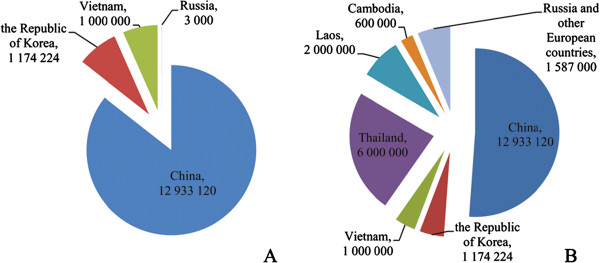
Population with liver fluke infections globally. A: Population with clonorchiasis. B: Population with clonorchiasis and opisthorchiasis.
Figure 2.
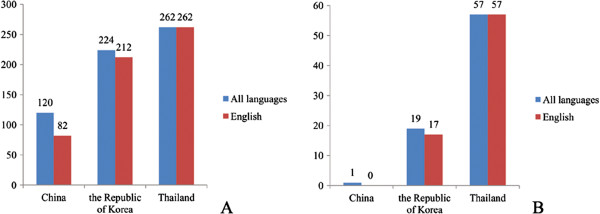
Number of papers documented in Pubmed on liver flukes from China, the Republic of Korea and Thailand. Searching strategy listed in Additional file 2. A: Papers focusing on liver flukes. B: Papers focusing on liver flukes and cholangiocarcinoma.
Secondly, as HBV mainly attacks the liver, C. sinensis infection also causes liver diseases, as well as biliary conditions. Although there are differences, some similarities may lead to misdiagnosis. Both may present non-specific symptoms or signs, such as fatigue, loss of appetite, fever, nausea, abdominal pain, jaundice and hepatomegaly [8,9]. What is most similar is that both can cause liver cancer [10,11]. Hepatocellular carcinoma and CCA are the two most common types of liver cancer [12]. HBV is a definite carcinogen to hepatocellular carcinoma, while C. sinensis is the one to CCA [10,11]. Meta-analyses captured a general odds ratio of 15.6 for HBV infection in causing hepatocellular carcinoma [13], and 4.5 for C. sinensis infection in causing CCA [1]. Inflammation is the crucial factor in the carcinogenesis of both agents [10]. As the carcinogenicity is associated with the virus load in HBV [14], it is relevant to the infection intensity in Opisthorchis viverrini-homologous to C. sinensis[15].
Thirdly, both HBV and C. sinensis infections cause significant disability. An average disability weight of 0.075 in C. sinensis infection is captured through community survey and model simulation [16], which is unexpectedly the same as that in hepatitis B [17].
Nevertheless, different changing trends appear. Although there is no availability of treatment to completely clear HBV, efficient vaccine and great efforts contribute to its obvious decline, especially in China [4,7,18]. Even though specific drug, namely praziquantel, is available, neglect and re-infection cause the significant increase in clonorchiasis [1,2].
Although there are fundamental differences in biology and some other aspects, comparisons above justify the public health importance of C. sinensis infection in China. Even though a relatively smaller population is infected with C. sinensis as compared with HBV nationally, the impact of clonorchiasis challenges hepatitis B in major endemic areas, namely the east part of China [1,19], where the former is becoming another killer of the liver and biliary health. The great success in controlling hepatitis B in China should provide valuable lessons for tackling clonorchiasis.
More problems raised and more researches needed in China
Recently, the Disease Reference Group on Helminth Infections (DRG4) established by the Special Programme for Research and Training in Tropical Diseases ranked prioritized researches for the control and elimination of major human helminthiases, including clonorchiasis [20]. Indeed, some have also been pointed out directly or indirectly in our former article.
Although three large-scale surveys involving clonorchiasis in China promote understanding the national situation and changes, epidemiology is only captured at the provincial level rather than at the county or lower level, which hampers the implementation of intervention measurements. Therefore, new methods, such as spatial techniques and modeling, deserve to be introduced to draw an epidemiological map for the disease [21,22]. Even though some epidemiological characteristics are known, social ecology and environmental determinants need to be elucidated further, such as the inherent drive for raw-fish-eating behavior, the cycle of infection-treatment-re-infection, factors involving in distributing and taking drug, roles of intermediate hosts, climate change [23], the property of zoonosis [24] and so on.
Whether other liver flukes and intestinal flukes are co-endemic in China challenges more accurate diagnosis, especially molecular methods [1,25]. Although two endemic zones have been classified [1] and some differences in biology have also been found [26], whether there exist differences in morbidity, especially in CCA, are also expected to be explored. It is already known that infection intensity is associated with carcinogenesis in O. viverrini infection [15], but corresponding studies in C. sinensis infection are not yet available, which causes unreasonably adopting the same OR in calculating CCA incidence in both sexes [1]. Furthermore, the impact of co-endemicity of C. sinensis and HBV infections on morbidity, especially on liver cancer in the east part of China, needs to be evaluated. Obviously, the establishment of tumor registry in China will promote related researches. Massive drug administration still counts on single drug, praziquantel [27], but no standardized principles of management are yet available. Additionally, tribendimidine, which shows promising efficiency against C. sinensis infection in vivo, in vitro, and in small field test, is expected to be further evaluated [28-30].
Even though most of the population infected with liver flukes distribute in China, corresponding researches are significantly less as compared with that in the Republic of Korea and Thailand, especially in CCA (Figure 2A and 2B, Additional file 2). The effort for controlling clonorchiasis in China will determine the global agenda for control and even elimination. Thus, more researches are anticipated from Chinese scientific workers. As it should be, international cooperation will be welcomed for tackling this problem [31].
Summary
The comparability between clonorchiasis and hepatitis B in epidemiology, clinical symptoms and carcinogenicity and disability, and contrast in changing trends, justify the threat of clonorchiasis and the urgency for intervention in China. Prioritized researches covering topics from basic biology to intervention are expected, which will benefit the control and even final elimination of clonorchiasis. However, the imbalance between the majority of infected population and the minority of researches in China draws more challenges. Thus, more efforts and outputs are expected from Chinese scientists, as well as international cooperation.
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
MBQ, YDC and FY discussed jointly. MBQ developed the first draft, and all authors read and approved the final manuscript.
Supplementary Material
Multilingual abstracts in the six official working languages of the United Nations.
Analysis on the number of papers documented in Pubmed on liver flukes from China, the Republic of Korea and Thailand.
Contributor Information
Men-Bao Qian, Email: ahtlqmb-007@163.com.
Ying-Dan Chen, Email: cyingdan@yahoo.com.cn.
Fei Yan, Email: fyan@shmu.edu.cn.
Acknowledgments
The authors would like to thank Dr. Xiao-Nong Zhou for his critical advice and the reviewers for their valuable suggestions. This project is funded through a capacity building initiative for Ecohealth Research on Emerging Infectious Disease in Southeast Asia supported by the International Development Research Centre (IDRC), the Canadian International Development Agency (CIDA), and the Australian Agency for International Development (AusAID) in partnership with the Global Health Research Initiative (grant No. 105509-00001002-023), as well as supported by the National S & T Major Program (grant No. 2008ZX10004-011), and by the National S & T Supporting Project (grant No. 2007BAC03A02).
References
- Qian MB, Chen YD, Liang S, Yang GJ, Zhou XN. The global epidemiology of clonorchiasis and its relation with cholangiocarcinoma. Infectious Diseases of Poverty. 2012;1:4. doi: 10.1186/2049-9957-1-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- First WHO report on neglected tropical diseases 2010: working to overcome the global impact of neglected tropical diseases. Available: http://www.who.int/neglected_diseases/2010report/en/ Accessed 27 October 2010. [PubMed]
- Lu FM, Zhuang H. Management of hepatitis B in China. Chin Med J (Engl) 2009;122:3–4. [PubMed] [Google Scholar]
- World Health Organization. Hepatitis B vaccines. Wkly Epidemiol Rec. 2009;84:405–419. [PubMed] [Google Scholar]
- WHO. Control of Foodborne Trematode Infections. Geneva: World Health Organization; 1995. (WHO technical Report Series). [PubMed] [Google Scholar]
- Sithithaworn P, Andrews RH, Nguyen VD, Wongsaroj T, Sinuon M, Odermatt P, Nawa Y, Liang S, Brindley PJ, Sripa B. The current status of opisthorchiasis and clonorchiasis in the Mekong Basin. Parasitol Int. 2012;61:10–16. doi: 10.1016/j.parint.2011.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liang X, Bi S, Yang W, Wang L, Cui G, Cui F, Zhang Y, Liu J, Gong X, Chen Y, Wang F, Zheng H, Wang F, Guo J, Jia Z, Ma J, Wang H, Luo H, Li L, Jin S, Hadler SC, Wang Y. Epidemiological serosurvey of hepatitis B in China–declining HBV prevalence due to hepatitis B vaccination. Vaccine. 2009;27:6550–6557. doi: 10.1016/j.vaccine.2009.08.048. [DOI] [PubMed] [Google Scholar]
- Keiser J, Utzinger J. Food-borne trematodiases. Clin Microbiol Rev. 2009;22:466–483. doi: 10.1128/CMR.00012-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilkins T, Zimmerman D, Schade RR. Hepatitis B: diagnosis and treatment. Am Fam Physician. 2010;81:965–972. [PubMed] [Google Scholar]
- Bouvard V, Baan R, Straif K, Grosse Y, Secretan B, El Ghissassi F, Benbrahim-Tallaa L, Guha N, Freeman C, Galichet L, Cogliano V. WHO International Agency for Research on Cancer Monograph Working Group. A review of human carcinogens-Part B: biological agents. Lancet Oncol. 2009;10:321–322. doi: 10.1016/S1470-2045(09)70096-8. [DOI] [PubMed] [Google Scholar]
- International Agency for Research on Cancer. A Review of Human Carcinogens Part B: Biological Agents. IARC monographs on the evaluation of carcinogenic risks to humans. Lyon: IARC; 2011. [Google Scholar]
- Srivatanakul P, Sriplung H, Deerasamee S. Epidemiology of liver cancer: an overview. Asian Pac J Cancer Prev. 2004;5:118–125. [PubMed] [Google Scholar]
- Shi J, Zhu L, Liu S, Xie WF. A meta-analysis of case–control studies on the combined effect of hepatitis B and C virus infections in causing hepatocellular carcinoma in China. Br J Cancer. 2005;92:607–612. doi: 10.1038/sj.bjc.6602333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen CJ, Yang HI, Su J, Jen CL, You SL, Lu SN, Huang GT, Iloeje UH. REVEAL-HBV Study Group. Risk of hepatocellular carcinoma across a biological gradient of serum hepatitis B virus DNA level. JAMA. 2006;295:65–73. doi: 10.1001/jama.295.1.65. [DOI] [PubMed] [Google Scholar]
- Haswell-Elkins MR, Mairiang E, Mairiang P, Chaiyakum J, Chamadol N, Loapaiboon V, Sithithaworn P, Elkins DB. Cross-sectional study of Opisthorchis viverrini infection and cholangiocarcinoma in communities within a high-risk area in northeast Thailand. Int J Cancer. 1994;59:505–509. doi: 10.1002/ijc.2910590412. [DOI] [PubMed] [Google Scholar]
- Qian MB, Chen YD, Fang YY, Xu LQ, Zhu TJ, Tan T, Zhou CH, Wang GF, Jia TW, Yang GJ, Zhou XN. Disability weight of Clonorchis sinensis infection: captured from community study and model simulation. PLoS Negl Trop Dis. 2011;5:e1377. doi: 10.1371/journal.pntd.0001377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO Global burden of disease 2004 update: disability weights for diseases and conditions. Available: http://www.who.int/healthinfo/global_burden_disease/GBD2004_DisabilityWeights.pdf Accessed 14 May 2010.
- Zhou YH, Wu C, Zhuang H. Vaccination against hepatitis B: the Chinese experience. Chin Med J (Engl) 2009;122:98–102. [PubMed] [Google Scholar]
- Huang TR, Yu JH, Li JL, Zhang ZQ, Deng W, Zhang CY, Zhao SF. A cross-sectional study on liver diseases in the rural residents in southern Guangxi, China. Zhonghua Yu Fang Yi Xue Za Zhi. 2007;41:123–126. in Chinese. [PubMed] [Google Scholar]
- Utzinger J. A research and development agenda for the control and elimination of human helminthiases. PLoS Negl Trop Dis. 2012;6:e1646. doi: 10.1371/journal.pntd.0001646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou XN, Lv S, Yang GJ, Kristensen TK, Bergquist NR, Utzinger J, Malone JB. Spatial epidemiology in zoonotic parasitic diseases: insights gained at the 1st International Symposium on Geospatial Health in Lijiang, China, 2007. Parasit Vectors. 2009;2:10. doi: 10.1186/1756-3305-2-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Basáñez MG, McCarthy JS, French MD, Yang GJ, Walker M, Gambhir M, Prichard RK, Churcher TS. A research agenda for helminth diseases of humans: modelling for control and elimination. PLoS Negl Trop Dis. 2012;6:e1548. doi: 10.1371/journal.pntd.0001548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gazzinelli A, Correa-Oliveira R, Yang GJ, Boatin BA, Kloos H. A research agenda for helminth diseases of humans: social ecology, environmental determinants, and health systems. PLoS Negl Trop Dis. 2012;6:e1603. doi: 10.1371/journal.pntd.0001603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Molyneux D, Hallaj Z, Keusch GT, McManus DP, Ngowi H, Cleaveland S, Ramos-Jimenez P, Gotuzzo E, Kar K, Sanchez A, Garba A, Carabin H, Bassili A, Chaignat CL, Meslin FX, Abushama HM, Willingham AL, Kioy D. Zoonoses and marginalised infectious diseases of poverty: where do we stand? Parasit Vectors. 2011;4:106. doi: 10.1186/1756-3305-4-106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCarthy JS, Lustigman S, Yang GJ, Barakat RM, García HH, Sripa B, Willingham AL, Prichard RK, Basáñez MG. A research agenda for helminth diseases of humans: diagnostics for control and elimination programmes. PLoS Negl Trop Dis. 2012;6:e1601. doi: 10.1371/journal.pntd.0001601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu GH, Li B, Li JY, Song HQ, Lin RQ, Cai XQ, Zou FC, Yan HK, Yuan ZG, Zhou DH, Zhu XQ. Genetic variation among Clonorchis sinensis isolates from different geographic regions in China revealed by sequence analyses of four mitochondrial genes. J Helminthol. 2012;86:479–484. doi: 10.1017/S0022149X11000757. [DOI] [PubMed] [Google Scholar]
- Prichard RK, Basáñez MG, Boatin BA, McCarthy JS, García HH, Yang GJ, Sripa B, Lustigman S. A research agenda for helminth diseases of humans: intervention for control and elimination. PLoS Negl Trop Dis. 2012;6:e1549. doi: 10.1371/journal.pntd.0001549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keiser J, Shu-Hua X, Chollet J, Tanner M, Utzinger J. Evaluation of the in vivo activity of tribendimidine against Schistosoma mansoni, Fasciola hepatica, Clonorchis sinensis, and Opisthorchis viverrini. Antimicrob Agents Chemother. 2007;51:1096–1098. doi: 10.1128/AAC.01366-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiao SH, Xue J, Xu LL, Zheng Q, Qiang HQ, Zhang YN. The in vitro and in vivo effect of tribendimidine and its metabolites against Clonorchis sinensis. Parasitol Res. 2009;105:1497–1507. doi: 10.1007/s00436-009-1579-6. [DOI] [PubMed] [Google Scholar]
- Qian MB, Yap P, Yang YC, Liang H, Jiang ZH, Li W, Tan YG, Zhou H, Utzinger J, Zhou XN, Keiser J. Efficacy and Safety of Tribendimidine against Clonorchis sinensis. Clin Infect Dis. 2013. p. . in press. [DOI] [PMC free article] [PubMed]
- Qian MB, Zhou XN, Fang YY, Liang S, Chen YD. Strengthening the research on clonorchiasis in China. Chin J Parasitol Parasit Dis. 2011;29:211–214. in Chinese. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Multilingual abstracts in the six official working languages of the United Nations.
Analysis on the number of papers documented in Pubmed on liver flukes from China, the Republic of Korea and Thailand.


