Abstract
In the interest of improving child maltreatment prevention science, this longitudinal, community based study of 499 mothers and their infants tested the hypothesis that mothers’ childhood history of maltreatment would predict maternal substance use problems, which in turn would predict offspring victimization. Mothers (35% White/non-Latina, 34% Black/non-Latina, 23% Latina, 7% other) were recruited and interviewed during pregnancy, and child protective services records were reviewed for the presence of the participants’ target infants between birth and age 26 months. Mediating pathways were examined through structural equation modeling and tested using the products of the coefficients approach. The mediated pathway from maternal history of sexual abuse to substance use problems to offspring victimization was significant (standardized mediated path [ab]=.07, 95% CI [.02, .14]; effect size=.26), as was the mediated pathway from maternal history of physical abuse to substance use problems to offspring victimization (standardized mediated path [ab]=.05, 95% CI [.01, .11]; effect size =.19). There was no significant mediated pathway from maternal history of neglect. Findings are discussed in terms of specific implications for child maltreatment prevention, including the importance of assessment and early intervention for maternal history of maltreatment and substance use problems, targeting women with maltreatment histories for substance use services, and integrating child welfare and parenting programs with substance use treatment.
Keywords: Child maltreatment, Substance abuse, Intergenerational processes
Child maltreatment and parental substance use problems are significant public health problems that disproportionately affect young children. In 2008, 772,000 US children were reported as victims of child abuse or neglect (10.3 per 1,000 children [1.0%]; US Department of Health and Human Services [US DHHS] 2010). Rates for children between birth and age 1 were more than twice as high (2.2%; US DHHS 2010). The 2001 National Household Survey on Drug Abuse estimated that 6.1 million US children (9%) were living in households with at least one parent with substance abuse or dependence (SAMHSA Office of Applied Studies 2003). Over one third of these children (35.9%) were 5 years old or younger.
Research to date has suggested developmental links between these two public health problems. Childhood maltreatment predicts later substance use problems (e.g., Widom et al. 2007), and parental substance use problems predict offspring victimization (e.g., Chaffin et al. 1996). There is intergenerational continuity in child maltreatment which may be explained by multiple propagating processes (e.g., parental substance use and mental health problems, family social isolation; see Berlin et al. in press). Understanding the specific processes underlying the connections among childhood maltreatment, parental substance use, and offspring victimization is important for identifying critical targets for prevention and treatment (e.g., Chassin et al. 2004). In the interest of further explicating these processes to inform child maltreatment prevention, we conducted a longitudinal mediational analysis of the extent to which mothers’ history of childhood maltreatment predicted maternal substance use problems, which in turn predicted their offspring’s victimization between birth and age two. We used retrospective reports of mothers’ history of maltreatment and prospective examination of offspring victimization.
Intergenerational Associations among Child Maltreatment and Substance Use Problems
Studies offer converging evidence that child maltreatment predicts later substance use problems. Retrospective studies have demonstrated significant associations between adults’ self-reported history of childhood maltreatment and current or lifetime substance use problems (e.g., Anda et al. 2006; MacMillan et al. 2001; Molnar et al. 2001). More rigorous, prospective studies have also identified associations between childhood maltreatment and later substance use problems. Strong evidence comes from Widom and colleagues’ prospective longitudinal study of approximately 1,000 individuals, approximately half of whom had documented cases of childhood maltreatment (the remainder were matched controls). In this study, childhood maltreatment predicted young adult alcohol abuse and/or dependence symptoms (Widom et al. 1995) and substance use disorders (Widom and White 2008). For females only, these effects persisted into middle adulthood (Widom et al. 2006, 2007).
Echoing Widom’s finding concerning the robustness of the effect for females, another prospective longitudinal study following 503 individuals found that, for females only, physical abuse in the first 5 years of life predicted adolescent and young adult alcohol and other drug use (Lansford et al. 2010). A third prospective study of 842 individuals found that self-reported physical (though not sexual) abuse occurring between ages 10 and 17 predicted later self-reported adult alcohol, marijuana, and other drug problems (Lo and Cheng 2007).
As with the associations between childhood maltreatment and substance use problems, associations between parental substance use and offspring maltreatment have been well documented. Extant literature has demonstrated repeatedly that children in substance abusing families are at significantly increased risk for physical and sexual abuse, neglect, abandonment, and foster placement (e.g., Smith et al. 2007; Wasserman and Leventhal 1993). The ACE study of over 8,000 adult HMO members found that adults’ retrospective reports of their parents’ alcohol abuse were significantly related to these adults’ recollections of childhood abuse and neglect (Dube et al. 2001). Moreover, several prospective longitudinal studies have identified parental substance use problems as a risk factor for offspring victimization (Chaffin et al. 1996; Kotch et al. 1999). For example, a prospective study using two waves of the Epidemiologic Catchment Area Survey of over 7,000 parents demonstrated that individuals identified with substance use disorders at any one time point were at higher risk of reporting abuse and neglect of their children at a later time point (Chaffin et al. 1996).
Although parents’ substance use is a risk factor for offspring maltreatment, this victimization is not always perpetrated by the parents themselves. Children of alcoholic mothers, for example, are at increased risk for sexual abuse by someone outside the family (Fleming et al. 1997). Thus, parental substance use may result in victimization directly through impaired parent behavior and discipline or indirectly through inadequate child monitoring and protection (Widom and Hiller-Sturmhofel 2001).
Taken as a whole, the research literature linking child maltreatment and subsequent substance use problems, on the one hand, and parents’ substance use problems and offspring victimization, on the other hand, can be viewed as suggesting an intergenerational pathway. According to this pathway, childhood maltreatment increases the risk for subsequent substance use problems which then, as individuals become parents, increase the risk of their own children’s abuse and neglect. To date, only two known studies have begun to examine this intergenerational pathway as a whole, however, and findings are inconclusive. First, Marcenko et al. (2000) proposed and examined a developmental model of the intergenerational transmission of child maltreatment through maternal factors, including substance use. In their cross-sectional study of 127 high-risk families, mothers were interviewed regarding childhood history of maltreatment, substance abuse, and their child(ren)’s current placement. Bivariate analyses revealed that self-reported childhood sexual abuse was significantly related to lifetime heavy alcohol or other drug use. Separate multivariate analyses indicated that mothers with heavy substance use histories were more likely to have children who were placed outside their home. The full, mediated model (i.e., maternal history of childhood sexual abuse predicting heavy substance abuse predicting offspring’s out-of-home placements) was not tested, however.
Similarly, a study of 318 mothers and fathers examined cross-sectional associations among parents’ retrospectively self-reported childhood maltreatment (emotional and physical abuse, sexual abuse, and emotional and physical neglect); self-reported current use of alcohol, marijuana, and cocaine; and self-reported current parenting practices (neglect, aggression, rejection, warmth) (Locke and Newcomb 2004). Using structural equation modeling for mothers and multiple regression analysis for fathers (after no significant associations were found in structural models), the authors found direct links between parents’ retrospectively self-reported childhood maltreatment and lower-quality parenting practices. For mothers, they also found significant paths between self-reported substance use and lower-quality parenting practices. Self-reported substance use problems were not predicted by mothers’ childhood maltreatment, however. Therefore, there was no evidence of an intergenerational pathway from parents’ maltreatment histories to self-reported substance use to parenting practices.
The Current Study
Although the literature documents multiple associations among child maltreatment and substance use problems, the extent to which there is an intergenerational pathway from parental history of child maltreatment to substance use problems to offspring victimization is not well understood. A key limitation in the literature is a lack of statistical control for confounding factors such as ethnicity, socioeconomic status (SES), and mothers’ mental health problems, which often coexist with substance use problems. Mental health problems also might affect both recollections about childhood maltreatment and parenting behaviors. Moreover, the literature on the effects of childhood maltreatment on later substance use problems is inconsistent with respect to maltreatment type: Marcenko et al. (2000) found that a history of sexual abuse, though not physical abuse, was significantly related to drug use, whereas Lo and Cheng (2007) found the opposite; MacMillan et al. (2001) found that both types predicted substance use disorders. None of these studies tested the effects of a childhood history of neglect.
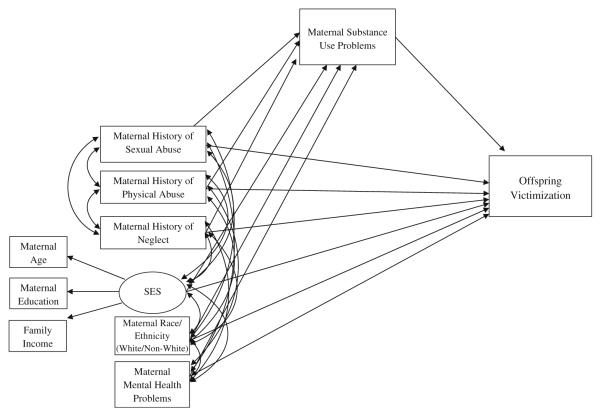
In the current study, in the interest of informing the design and implementation of services to prevent child maltreatment across generations, we drew on a representative community-based sample of pregnant women who were followed across time to test the hypothesis that mothers’ self-reported history of childhood maltreatment (by parents or other perpetrators) would predict maternal substance use problems, which in turn would predict prospectively their offspring’s victimization (by any perpetrator) between birth and age two. Using structural equation modeling, we examined each of three types of maternal childhood maltreatment history (sexual abuse, physical abuse, and neglect) and covaried mothers’ mental health problems, race/ethnicity, and SES (see Fig. 1). We tested mediation with the product of the coefficients approach (MacKinnon 2008; MacKinnon et al. 2002).
Fig. 1.
Structural equation model used to test associations among maternal history of maltreatment (sexual abuse, physical abuse, and neglect), maternal substance use problems, and offspring victimization, controlling for maternal race/ethnicity, SES (age, education, family income), and maternal mental health problems
Method
Participants
Participants were 499 mothers and their infants from a small southeastern city and its surrounding county. Mothers were recruited during pregnancy by one of three trained female research assistants in the waiting rooms of prenatal care providers, including a large public health clinic and private OB/GYN practices. In addition, flyers were posted at these clinics and in other community locations. Potential participants were offered $20 per interview. Of the 383 women approached, 351 (92%) agreed to participate. Another 148 were recruited after responding to the flyer.
Fifty-two percent of the mothers were first-time mothers. Mothers selected from a list of racial/ethnic groups to identify themselves as White (non-Latina) (35%), Black (non-Latina) (34%), Latina (23%), Asian (3%), bi- or multi-racial (3%) or other (1%). Mothers ranged in age from 12 to 41 (M=27.31, s=5.88). Twenty-eight percent of the mothers had not completed high school, 13% had completed high school or a GED, and 17% had completed some college or vocational training. Twenty-three percent of the mothers had graduated from college and 18% had completed a post-graduate degree. Annual family income ranged from $0 to $400,000, with a median of $35,000. Seventy-six percent of the mothers lived with a husband, boyfriend, or partner. Comparison to population statistics for race, ethnicity, and education for mothers giving birth in the county during the year that study participants were interviewed indicated that the sample was representative of the county from which it was drawn.
Procedures
During the second half of pregnancy, participants completed an hour-long, face-to-face interview assessing family demographics, history of childhood maltreatment, and mental health and substance use problems. Interviews were conducted in English or Spanish, according to the participant’s preference; Spanish interviews were conducted by a native Spanish speaker. As part of informed consent procedures, participants provided written consent for the research team to access county child protective service records for up to 7 years after their child’s birth.
Measures
Demographic Variables
Demographic variables were based on maternal self-report of race/ethnicity (dummy coded to White=1, non-White=0), age, education (8-point scale ranging from 0=none to 7=post college; range=0–7; M=4.36, s=2.08), and standard score of annual family income (range=−1.12–8.64; M=0.00, s=1.00).
Maternal History of Maltreatment During Childhood
Mothers responded to 14 items adapted from the widely-used Parent-Child Conflict Tactics Scale (PC-CTS; Straus et al. 1998). The PC-CTS asks adults about types of discipline that they experienced as a child. Mothers were asked if, during their childhood, they had never, sometimes, or often experienced each of 11 parental disciplinary or neglectful actions included in the PC-CTS. Mothers were classified as having experienced childhood physical abuse if they reported that they were often hit on the bottom or on some other part of the body “with something like a belt, hairbrush, a stick, or some other hard object,” or if they reported that they were sometimes or often “beat up (hit over and over as hard as [their parent] could).” This classification indicated that 9.6% (n=48) of the mothers had a history of childhood physical abuse.
Mothers were classified as having experienced childhood neglect if they reported that they were often “left alone when an adult should have been with you” during the day or during the night, if they reported that they were sometimes left alone during the day and during the night, or if their parent or caregiver was often “so drunk or high that they could not take care of you.” This classification indicated that 10.6% (n=53) of the mothers had a history of childhood neglect.
For the purposes of the present study, mothers were also asked if, during their childhood, they had never, sometimes, or often experienced each of three inappropriate sexual actions included in the PC-CTS. Mothers were classified as having experienced childhood sexual abuse if they reported that before age 18 they had ever been touched sexually, been pressured to touch in a sexual way, or been pressured to have sex by an older child or adult. This classification indicated that 25% (n=125) of the mothers had a history of childhood sexual abuse.
Two percent (n=11) of the mothers experienced all three types of maltreatment (sexual abuse, physical abuse, and neglect). This represents 9% of the 125 mothers who had been sexually abused, 23% of the 48 mothers who had been physically abused, and 21% of the 53 mothers who had been neglected.
Maternal Mental Health Problems
Three questions concerning mental health problems during the past year were adapted from the Composite International Diagnostic Interview Short Form (CIDI-SF; Kessler et al. 1998). Mothers indicated whether they had felt sad, blue, or depressed for 2 or more consecutive weeks, whether they had lost interest in most things that usually give them pleasure for 2 or more consecutive weeks, and whether they had felt worried, tense, or anxious most of the time for 1 month or longer. Responses were summed to create a 4-point index of total mental health problems (range=0–3; M=0.85, s=1.10). Forty-four percent of the mothers reported at least one mental health problem during the past year.
Maternal Substance Use Problems
Substance use problems were assessed during the pregnancy interview using 6 items developed for the purpose of this study. Mothers indicated whether during the year before they became pregnant they ever “had such a strong desire or urge to (a) drink or (b) use drugs that you could not keep from drinking/drug use” or whether “your (a) drinking or (b) drug use or being hung over interfered with your work at school, or a job, or at home,” and whether they had ever received treatment for (a) alcohol or (b) drug problems. Responses were summed to create a 6-point index of substance use problems (range=0–5, M=0.12, s=0.53; α=.70). Responses indicated that 90.4% of mothers (n=451) reported no substance use problems, 6.2% (n=31) reported at least one substance use problem, and 3.4% (n=17) did not respond to the questions. Among the 31 individuals who reported at least one substance use problem, the mean number of problems was 1.84.
Offspring Victimization
County records of allegations and substantiations of child maltreatment, organized according to child victims, were reviewed for the presence of participants’ target infants. In accordance with county regulations, information about perpetrators was explicitly excluded from the records available to our research team. Records were reviewed through the child’s age of 26 months. We identified 40 children (8%) with at least one incident of alleged or substantiated abuse or neglect. There was a total of 79 incidents for these 40 children, with 17 (43%) of the children having more than one allegation or substantiation. Of these 79 incidents, 62 (78%) were allegations only and 17 (22%) were substantiations. Of these 17 substantiations, 14 (82%) were substantiated for neglect, 2 (12%) were substantiated for abuse (physical, sexual, or emotional), and 1 (6%) was classified “in need of services.” (“In need of services” is a relatively new sub-classification introduced through the implementation of a statewide child welfare reform, the Multiple Response System.) The high proportion of neglect substantiations reflects the state’s stringent criteria for abuse substantiations and broad criteria for neglect substantiations. For example, to be substantiated for physical abuse, a child must have a currently visible bruise or physical injury, which might have disappeared by the time of investigation. Substantiations for neglect include “inappropriate discipline,” including inappropriate physical discipline. This sample’s distributions are consistent with county patterns.
For analytic purposes, children were classified as victimized if they had at least one allegation or substantiation of abuse or neglect at or before age 26 months. As noted, 40 (8%) of the children met this criterion. We combined allegations and substantiations for several reasons. First, analysis of this county’s records as well as those from a national probability study has indicated that allegations and substantiations are equally good predictors of subsequent involvement with child protective services (Durham Family Initiative 2009; Kohl et al. 2009). Second, several studies have demonstrated that the developmental outcomes of alleged versus substantiated maltreatment do not differ significantly (Black et al. 2002; Hussey et al. 2005; Leiter et al. 1994), and that both alleged and substantiated cases in fact substantially underestimate the true prevalence of child abuse and neglect and associated developmental risks (Straus et al. 1998; Theodore et al. 2005; Williams et al. 2009). Third, analyzing substantiated maltreatment only has been shown to result in limited representation, presumably from biases in the substantiation processes (Black et al. 2002; Cross and Casanueva 2009). Thus, including children with alleged maltreatment should result in more generalizable findings (Manly 2005).
Results
Analytic Strategy
All principal analyses were conducted with structural equation models using Mplus (Muthén and Muthén 1998–2006), with missing values handled by maximum likelihood estimation using missing-data-relevant covariates. Family income was missing in 13% and substance use problems were missing in 3.4% of the data due to nonresponse. For all other variables, between 99% and 100% of the data were present. Analyses included a comprehensive set of socio-demographic covariates that typically predict and/or are predicted by child maltreatment.
As a robust test of mediation, we used the product of the coefficients approach, including tests of asymmetric confidence intervals (MacKinnon 2008; MacKinnon et al. 2002). This procedure uses the path coefficients generated by the structural equation model to provide a joint estimation of mediating variable effects on the outcome, where path a is the path between the predictors (mothers’ childhood history of sexual abuse, physical abuse, and neglect) and the mediator (substance use problems) and path b is the path between the mediator and the outcome (offspring victimization). First, we computed the product of the coefficients term, ab (coefficient for path a X coefficient for path b). Second, we computed the product of the coefficients test statistic (ab/SE of the product). Third, because the distribution of the test statistic is not expected to be normal, we computed asymmetric confidence intervals (ACIs) for each test statistic based on the distribution of the product of the two variables (MacKinnon 2008). Mediated effects are significant when the ACIs do not cross zero.
Preliminary Analyses
Table 1 provides descriptive information for key socio-demographic, independent, and dependent variables and the bivariate correlations between the variables. There were significant bivariate associations between maternal history of two types of maltreatment (sexual abuse, physical abuse) and offspring victimization, between all three types of maltreatment and maternal substance use problems, as well as between maternal substance use problems and offspring victimization. Given significant associations in previous studies as well as numerous significant associations in this study between several maternal socio-demographic characteristics and the key dependent variable (offspring victimization) and/or independent variables (mothers’ childhood sexual abuse, physical abuse, and neglect), the structural model covaried maternal race/ethnicity (White/non-White), age, education, family income, and maternal mental health problems. Given associations among age, education, and income, these variables were represented in the structural equation model as reflective indicators forming a single latent variable (i.e., SES). Maternal race was maintained as a separate variable due to its unique bivariate associations with maternal history of maltreatment.
Table 1.
Means, standard deviations, and inter correlations among variables (prior to maximum likelihood estimation)
| 1. | 2. | 3. | 4. | 5. | 6. | 7. | 8. | 9. | 10. | |
|---|---|---|---|---|---|---|---|---|---|---|
| N | 496 | 495 | 498 | 432 | 498 | 499 | 495 | 499 | 482 | 499 |
| M (s) | N/A | 27.31 (5.88) | 4.36 (2.08) | 0.00 (1.00) | N/A | N/A | N/A | 0.85 (1.10) | 0.12 (0.53) | N/A |
| Range | 0–1 | 12–41 | 0–7 | −1.12–8.64 | 0–1 | 0–1 | 0–1 | 0–3 | 0–5 | 0–1 |
| Percent of Yes Responses | 35% | n/a | n/a | n/a | 25% | 9.6% | 10.6% | n/a | n/a | 8% |
| 1. Maternal Race/Ethnicity (1 = White) | – | |||||||||
| 2. Maternal Age | .34*** | – | ||||||||
| 3. Maternal Education | .53*** | .54*** | – | |||||||
| 4. Family Income | .46*** | .43*** | .56*** | – | ||||||
| 5. Maternal History of Sexual Abuse | −.004 | .02 | −.01 | −.05 | – | |||||
| 6. Maternal History of Physical Abuse | −.07 | −.03 | −.14** | −.12* | .19*** | – | ||||
| 7. Maternal History of Neglect | −.08^ | −.02 | −.07 | −.12* | .19*** | .27*** | – | |||
| 8. Maternal Mental Health Problems | −.10* | −.13** | −.24*** | −.22*** | .12* | .17*** | .09^ | – | ||
| 9. Maternal Substance Use Problems | .003 | .04 | −.11* | −.11* | .20** | .14** | .09* | .18*** | – | |
| 10. Offspring Victimization | −.11* | −.13** | −.17*** | -.15** | .14** | .10* | .02 | .12* | .25** | – |
p<.10
p<.05
p<.01
p<.001.
Structural Equation Model
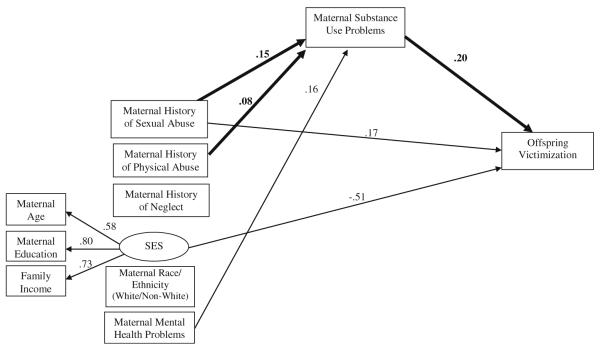
Figure 1 illustrates the structural equation model used to test the longitudinal relations among maternal history of maltreatment (sexual abuse, physical abuse, and neglect), maternal substance use problems, and offspring victimization, controlling for maternal race/ethnicity (White/non-White), SES (age, education, family income), and maternal mental health problems. The model fit the data well (χ2= 21.85, df=10, p=.02, CFI=.99, TLI=.97, RMSEA=.05). Figure 2 summarizes the significant path coefficients for the structural equation model.
Fig. 2.
Summary of structural equation model fitting associations among maternal history of maltreatment (sexual abuse, physical abuse, neglect), maternal substance use problems, and offspring victimization, controlling for maternal race/ethnicity, SES (age, education, family income), and maternal mental health problems. Only standardized, significant (p<.05) coefficients are provided. The most relevant paths and coefficients are depicted in bold. To simplify the presentation, the following significant covariances among variables are not depicted: maternal mental health problems with SES=−.28; maternal health problems with White=−.10; maternal mental health problems with maternal history of physical abuse = .17; maternal mental health problems with maternal history of neglect = .09; maternal mental health problems with maternal history of childhood sexual abuse = .12; White with SES=.62; maternal history of physical abuse with SES=−.13; maternal history of sexual abuse with physical abuse = .19; maternal history of sexual abuse with neglect = .19; maternal history of neglect with physical abuse = .27
The product of the coefficients test of the mediated pathway from maternal history of sexual abuse to substance use problems to offspring victimization was significant, ab=.07, 95% CI [.02, .14]. Figure 2 indicates that childhood sexual abuse significantly increased the likelihood of mothers’ substance use problems, which in turn significantly increased the likelihood of infant/toddler victimization. The mediated effect from maternal history of sexual abuse to substance use problems was associated with a .26 standard deviation unit change in the likelihood of offspring victimization.
The product of the coefficients test of the mediated pathway from maternal history of physical abuse to substance use problems to offspring victimization was significant, ab=.05, 95% CI [.01, .11]. Figure 2 indicates that childhood physical abuse increased the likelihood of mothers’ substance use problems, which in turn increased the likelihood of infant/toddler victimization. The mediated effect from maternal history of physical abuse to substance use problems to offspring victimization was associated with a .19 standard deviation unit change in the likelihood of offspring victimization.
Regarding maternal history of neglect, the path from maternal history of neglect to maternal substance use problems was not significant. As a result, there could not be a significant mediated path.
Because the mediated pathways from both maternal sexual abuse and physical abuse to substance use to offspring victimization were significant, we conducted a follow-up test using model comparison procedures to examine equivalence of the SEM parameter estimates for the two significant mediated paths. The chi-square difference test revealed no significant differences, indicating that the pathways from maternal childhood sexual abuse to substance use problems to offspring victimization and from maternal childhood physical abuse to substance use problems to offspring victimization were not significantly different.
Regarding the covariates, SES was significantly related to offspring victimization, and maternal mental health problems were significantly related to maternal substance use problems. Because maltreatment may be related to our covariates in a predictive manner, consistent with Miller and Chapman (2001), we also analyzed the structural model without the covariates. The results were virtually identical. To test further the robustness of our model, we analyzed the model with each type of maternal maltreatment history individually. Again, the results did not change appreciably.
Discussion
In the interest of informing child maltreatment prevention, this investigation examined and found evidence for an intergenerational pathway from mothers’ self-reported history of childhood maltreatment to maternal substance use problems to offspring victimization. The study’s prospective design, use of a community based sample, inclusion of relevant covariates, use of official records of offspring maltreatment, and stringent tests of mediation help to illuminate an intergenerational pathway to child victimization that had, until the current study, been suggested but not rigorously tested.
We found significant mediated pathways from maternal history of sexual abuse and physical abuse–but not neglect–to substance use problems and then to official reports of offspring victimization between birth and age 26 months. Follow-up model comparison tests indicated that these mediated pathways were equivalent, and persisted with and without accounting for maternal race/ethnicity, age, education, family income, and maternal mental health problems. Covarying maternal mental health problems, however, overcame a methodological limitation of many previous studies (in which maternal mental health problems were not examined) and helped to address the limitation in the present study that mothers’ maltreatment histories and substance use problems were simultaneously, and retrospectively, self-reported. Specifically, covarying mental health problems helped to alleviate the concern that the associations among mothers’ maltreatment histories, substance use problems, and offspring victimization may have been spuriously inflated due to the associations between each variable and maternal depression and/or anxiety, or due to distortions in self-reports that may themselves have been a product of childhood maltreatment (Chu et al. 1999).
Our findings paint a picture of one pathway to child victimization whereby mothers’ history of sexual and/or physical abuse increases the likelihood that mothers will experience substance use problems, which in turn increases the likelihood of offspring maltreatment. These findings both build on and extend previous studies which heretofore tested only bifurcated pathways instead of the full mediated model (e.g., Locke and Newcomb 2004; Marcenko et al. 2000).
A number of explanatory processes may underlie this pathway. For example, the disruptive effects of childhood maltreatment on psychosocial functioning and in the stress-response and limbic systems may lead to risky health behaviors, including substance use (Anderson et al. 2002; Repetti et al. 2002). Substance use also may serve as a self-medicating or coping strategy to alleviate the negative effects of childhood maltreatment (Marcenko et al. 2000; Widom et al. 1995). Parental substance abuse has been discussed as interfering with supportive parenting by impairing awareness of and sensitivity to environmental and child cues, and by disrupting motor skills, emotion regulation, judgment capacity, and executive functioning (Mayes and Truman 2002). Households with parental substance abuse also are characterized by disorganization, disruption, and instability that can lead directly to child neglect, including long parental absences and food insecurity, and to child sexual abuse due to parental lack of monitoring and supervision (e.g., Widom and Hiller-Sturmhofel 2001).
The lack of a mediated pathway from maternal history of childhood neglect to substance use problems to offspring victimization is also notable. This finding may be due in part to our relatively limited assessment of maternal history of neglect. Specifically, our measure only included two items (i.e., often being left alone when an adult should have been with you, caregiver often so drunk or high that they could not take care of you). Other forms of neglect (e.g., failure to meet physical needs, supervision by an unsafe caregiver, exposure to unsafe environments other than substance-related concerns) and very early experiences of neglect (perhaps not remembered by respondents) not tapped here may have more pervasive and problematic outcomes (Kotch et al. 2008). It is also possible that the intergenerational effects of mothers’ childhood neglect will increase as our participants are followed longer. We focused here on the first 2 years of life, given the data available as well as evidence that youngest children are at the highest risk of maltreatment (US DHHS 2010). As children age, however, it is possible they will come to the attention of more individuals outside their homes (e.g., child care, school), which may result in more opportunities for maltreatment reports. Future data collection may further illuminate these pathways.
Although the pathway examined here was significant, the relatively modest effect size indicated that this pathway explains a small portion of the variance in offspring victimization. Thus, it is important to bear in mind that our findings depict one of many pathways to child victimization that merit investigation. For example, studies are beginning to show other intergenerational pathways that do not involve maternal substance use (e.g., from mothers’ childhood neglect to social isolation to child victimization [Berlin et al., in press]; from parents’ maltreatment history to mental health problems to child victimization [Dixon et al. 2005]). A goal for future research will be not only to explicate the multiple developmental pathways to child victimization but also to illuminate how, and for whom, these pathways interact.
Suggestions for Future Research
One limitation of this study is that an unmeasured third variable could account for the relations among childhood maltreatment, maternal substance use, and offspring victimization. We included several possible third variables (e.g., maternal ethnicity, age, education, income, mental health problems), but it is plausible that another, unmeasured variable accounts for the identified paths. Another limitation of the present data set–to be overcome by future studies–is that neither the perpetrator(s) nor the type(s) of maltreatment experienced by the child could be analyzed. With perpetrator data, researchers could establish if and how mothers’ maltreatment histories lead them to perpetrate maltreatment themselves, and/or to have children who are victimized by others. In addition, examining child maltreatment types in comparison with mothers’ maltreatment types could reveal the extent to which there is intergenerational continuity in specific subtypes of maltreatment. This more specific information in turn could guide prevention strategies.
Additionally, our measure of maternal substance use was limited to mothers’ history up to the time of pregnancy. Assessing parental substance use during and shortly after pregnancy can be challenging due to underreporting associated with mothers’ fears of child protective actions. Future studies that include prospective and concurrent measures of parental substance use would enhance our understanding of the proposed theoretical model.
Child maltreatment research is particularly methodologically complex, especially when assessing both parent and offspring victimization. Specifically, legally defined cases of maltreatment underestimate prevalence (e.g., Theodore et al. 2005), whereas self-report data are subject to reporting distortions (e.g., Chu et al. 1999). The use of multiple measures to assess maltreatment in both generations is ideal, and helps to avoid the problem of method variance. The current study is limited by its reliance on maternal report for both independent and mediating variables, although it is strengthened by its use of non-maternal report assessments for its dependent variable. At the same time, this approach means that we used different metrics to assess maltreatment in mothers than in their children, which may be criticized as an “apples to oranges” comparison. In order to create more parallel measures, even if studies cannot provide prospective, official data on both parents’ and children’s victimization, parents could be asked if their parent(s) were ever reported for abuse or neglect. We recommend this step for future research on intergenerational continuity in child maltreatment.
Implications for Child Maltreatment Prevention
Whereas there are many routes to child victimization, our findings simultaneously incorporate two major risk factors (maternal history of maltreatment and maternal substance use problems) that have specific implications for the prevention of child maltreatment. First, our findings point to the importance of assessing maltreatment history and substance use problems in pregnant women and new mothers. Our interviews of a community based sample revealed prevalence rates of sexual abuse (25%) that were concerning, yet consistent with previous research (22.3% in an aggregate of 25 samples, Gorey and Leslie 1997; 19.7% in a meta-analysis, Pereda et al. 2009). These rates underscore the need to assess and to make service referrals in community settings. Gatekeepers (e.g., prenatal care providers, public health nurses, social workers, substance abuse counselors, pediatricians) can be trained to screen and identify maternal trauma history and substance use problems and to make appropriate referrals to prevention and intervention services (e.g., Lieberman and Amaya-Jackson 2005). In order for such screening procedures to be successful, community members need to be aware of the risks and open to referrals. To this end, public health and media campaigns can educate the general public about the risk factors for parenting problems. Such campaigns have been shown to reduce risk for child maltreatment (e.g., Barr et al. 2009; Prinz et al. 2009). Community based child maltreatment prevention efforts can change community norms about parenting, thereby reducing stigma regarding seeking help and support during the transition to parenthood (Daro and Dodge 2009).
A second implication of our findings for child maltreatment prevention centers on the importance of targeting females with abuse histories for prevention and/or treatment of substance abuse problems. Trauma-informed cognitive-behavioral treatments to promote better coping strategies and to resolve past trauma, such as the Seeking Safety program, have demonstrated significant reductions in trauma and substance use symptoms among adolescent females with dual diagnoses of substance use disorder and PTSD (Najavits et al. 2006). Without such efforts, problems stemming from unresolved traumas are more likely to recur across the lifespan, increasing risk for substance use initiation or relapse, and, in turn, parenting problems.
A third implication of our findings for child maltreatment prevention centers on the high level of risk for offspring victimization among women with histories of both childhood maltreatment and substance use problems. Pregnant women and new mothers with such histories, faced with the enormous task of parenting a new baby, may be particularly vulnerable. At the same time, during this transition, such women may also be particularly open to treatment and to creating different experiences for their own children. Such strategies will require integration of substance use treatment with child welfare and parenting services, exemplified by the work of Suchman (e.g., Suchman et al. 2010). Increasingly integrated and evidence-based prevention efforts should in turn help to reduce child maltreatment, parental substance use, and the intergenerational patterns between the two.
Acknowledgments
This research was supported by NIMH K01MH70378 awarded to Lisa Berlin, NIDA P20DA017589 and NIDA P30DA023026 awarded to the Duke University Transdisciplinary Prevention Research Center, NIDA K05 DA015226 awarded to Kenneth Dodge, and a grant from The Duke Endowment awarded to Kenneth Dodge. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. We thank Chongming Yang and Antonio Morgan Lopez for assistance with statistical analysis and for feedback on an earlier draft of the paper. We also thank Rebecca Dunning and Claire Osgood for assistance with data management, and Jamilah Taylor for assistance with manuscript preparation.
Footnotes
Author Note Karen Appleyard, Center for Child and Family Health, Duke University; Lisa J. Berlin, Center for Child and Family Policy, Duke University; Katherine D. Rosanbalm, Center for Child and Family Policy, Duke University; Kenneth A. Dodge, Center for Child and Family Policy, Duke University.
Contributor Information
Karen Appleyard, Center for Child and Family Health, Duke University, 411 W. Chapel Hill St., Suite 908, Durham, NC 27701, USA.
Lisa J. Berlin, Center for Child and Family Policy, Duke University, Box 90545, Durham, NC 27708, USA
Katherine D. Rosanbalm, Center for Child and Family Policy, Duke University, Box 90545, Durham, NC 27708, USA
Kenneth A. Dodge, Center for Child and Family Policy, Duke University, Box 90545, Durham, NC 27708, USA
References
- Anda RF, Felitti VJ, Bremner JD, Walker JD, Whitfield C, Perry BD, et al. The enduring effects of abuse and related adverse experiences in childhood: A convergence of evidence from neurobiology and epidemiology. European Archives of Psychiatry and Clinical Neuroscience. 2006;256:174–186. doi: 10.1007/s00406-005-0624-4. doi:10.1007/s00406-005-0624-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson CM, Teicher MH, Polcari A, Renshaw PF. Abnormal T2 relaxation time in the cerebellar vermis of adults sexually abused in childhood: Potential role of the vermis in stress-enhanced risk for drug abuse. Psychoneuroendocrinology. 2002;27:231–244. doi: 10.1016/s0306-4530(01)00047-6. doi:10.1016/S0306-4530(01)00047-6. [DOI] [PubMed] [Google Scholar]
- Barr RG, Rivara FP, Barr M, Cummings P, Taylor J, Lengua LJ, et al. Effectiveness of educational materials designed to change knowledge and behaviors regarding crying and shaken-baby syndrome in mothers of newborns: A randomized, controlled trial. Pediatrics. 2009;123:972–980. doi: 10.1542/peds.2008-0908. doi:10.1542/peds.2008-0908. [DOI] [PubMed] [Google Scholar]
- Berlin LJ, Appleyard K, Dodge KA. Intergenerational continuity in child maltreatment: Mediating mechanisms and implications for prevention. Child Development. doi: 10.1111/j.1467-8624.2010.01547.x. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Black MM, Papas MA, Hussey JM, Dubowitz H, Kotch JB, Starr RH., Jr. Behavior problems among preschool children born to adolescent mothers: Effects of maternal depression and perceptions of partner relationships. Journal of Clinical Child and Adolescent Psychology. 2002;31:16–26. doi: 10.1207/S15374424JCCP3101_04. doi:10.1207/S15374424JCCP3101_04. [DOI] [PubMed] [Google Scholar]
- Chaffin M, Kelleher K, Hollenberg J. Onset of physical abuse and neglect: Psychiatric, substance abuse, and social risk factors from prospective community data. Child Abuse & Neglect. 1996;20:191–203. doi: 10.1016/s0145-2134(95)00144-1. doi:10.1016/S0145-2134(95)00144-1. [DOI] [PubMed] [Google Scholar]
- Chassin L, Carle AC, Nissim-Sabat D, Kumpfer KL. Fostering resilience in children of alcoholic parents. In: Maton KI, editor. Investing in children, youth, families, and communities: Strengths-based research and policy. APA Books; Washington: 2004. pp. 137–155. [Google Scholar]
- Chu JA, Frey LM, Ganzel BL, Matthews JA. Memories of childhood abuse: Dissociation, amnesia, and corroboration. The American Journal of Psychiatry. 1999;156:749–755. doi: 10.1176/ajp.156.5.749. [DOI] [PubMed] [Google Scholar]
- Cross TP, Casanueva C. Caseworker judgments and substantiation. Child Maltreatment. 2009;14:38–52. doi: 10.1177/1077559508318400. doi:10.1177/1077559508318400. [DOI] [PubMed] [Google Scholar]
- Daro D, Dodge KA. Creating community responsibility for child protection: Possibilities and challenges. The Future of Children. 2009;19(2):67–93. doi: 10.1353/foc.0.0030. doi:10.1353/foc.0.0030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dixon L, Browne K, Hamilton-Giachritsis C. Risk factors of parents abused as children: A mediational analysis of the intergenerational continuity of child maltreatment (Part I) Journal of Child Psychology and Psychiatry. 2005;46:47–57. doi: 10.1111/j.1469-7610.2004.00339.x. doi:10.1111/j.1469-7610.2004.00336.x. [DOI] [PubMed] [Google Scholar]
- Dube SR, Anda RF, Felitti VJ, Croft JB, Edwards VJ, Giles WH. Growing up with parental alcohol abuse: Exposure to childhood abuse, neglect, and household dysfunction. Child Abuse & Neglect. 2001;25:1627–1640. doi: 10.1016/s0145-2134(01)00293-9. doi:10.1016/S0145-2134(01)00293-9. [DOI] [PubMed] [Google Scholar]
- Durham Family Initiative . Investigated children with repeat investigations and substantiations. Duke University; Durham, NC: 2009. Unpublished raw data. [Google Scholar]
- Fleming J, Mullen P, Bammer GA. A study of potential risk factors for sexual abuse in childhood. Child Abuse & Neglect. 1997;21:49–58. doi: 10.1016/s0145-2134(96)00126-3. doi:10.1016/S0145-2134(96)00126-3. [DOI] [PubMed] [Google Scholar]
- Gorey KM, Leslie DR. The prevalence of child sexual abuse: Integrative review adjustment for potential response and measurement biases. Child Abuse & Neglect. 1997;21:391–398. doi: 10.1016/s0145-2134(96)00180-9. doi:10.1016/S0145-2134(96)00180-9. [DOI] [PubMed] [Google Scholar]
- Hussey JM, Marshall JM, English DJ, Knight ED, Lau AS, Dubowitz H, et al. Defining maltreatment according to substantiation: Distinction without a difference? Child Abuse and Neglect. 2005;29:479–492. doi: 10.1016/j.chiabu.2003.12.005. doi:10.1016/j.chiabu.2003.12.005. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Andrews G, Mroczek D, Ustun TB, Wittchen H-U. The World Health Organization Composite International Diagnostic Interview short form (CIDI-SF) International Journal of Methods in Psychiatric Research. 1998;7:171–185. doi: 10.1002/mpr.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kohl PL, Jonson-Reid M, Drake B. Time to leave substantiation behind: Findings from a national probability study. Child Maltreatment. 2009;14:17–26. doi: 10.1177/1077559508326030. doi:10.1177/1077559508326030. [DOI] [PubMed] [Google Scholar]
- Kotch JB, Browne DC, Dufort V, Winsor J, Catellier D. Predicting child maltreatment in the first 4 years of life from characteristics assessed in the neonatal period. Child Abuse & Neglect. 1999;23:305–319. doi: 10.1016/s0145-2134(99)00003-4. doi:10.1016/S0145-2134(99)00003-4. [DOI] [PubMed] [Google Scholar]
- Kotch JB, Lewis T, Hussey JM, English D, Thompson R, Litrownik AJ, et al. Importance of early neglect for childhood aggression. Pediatrics. 2008;121:725–731. doi: 10.1542/peds.2006-3622. doi:10.1542/peds.2006-3622. [DOI] [PubMed] [Google Scholar]
- Lansford JE, Dodge KD, Pettit GS, Bates JE. Does physical abuse in early childhood predict substance use in adolescence and early adulthood? Child Maltreatment. 2010;15:190–194. doi: 10.1177/1077559509352359. doi:10.1177/1077559509352359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leiter J, Myers KA, Zingraff MT. Substantiated and unsubstantiated cases of child maltreatment: Do their consequences differ? Social Work Research. 1994;18:67–82. [Google Scholar]
- Lieberman AF, Amaya-Jackson L. Reciprocal influences of attachment and trauma: Using a dual lens in the assessment and treatment of infants, toddlers, and preschoolers. In: Berlin LJ, Ziv Y, Amaya-Jackson LM, Greenberg MT, editors. Enhancing early attachments: Theory, research, intervention, and policy. Guilford Press; New York: 2005. pp. 100–124. [Google Scholar]
- Lo CC, Cheng TC. The impact of childhood maltreatment on young adults’ substance abuse. The American Journal of Drug and Alcohol Abuse. 2007;33:139–146. doi: 10.1080/00952990601091119. doi:10.1080/00952990601091119. [DOI] [PubMed] [Google Scholar]
- Locke TF, Newcomb MD. Child maltreatment, parent alcohol and drug-related problems, polydrug problems, and parenting practices: A test of gender differences and four theoretical perspectives. Journal of Family Psychology. 2004;18:120–134. doi: 10.1037/0893-3200.18.1.120. doi:10.1037/0893-3200.18.1.120. [DOI] [PubMed] [Google Scholar]
- MacKinnon DP. Introduction to statistical mediation analysis. Lawrence Erlbaum Associates; Mahwah, NJ: 2008. [Google Scholar]
- MacKinnon DP, Lockwood CM, Hoffman JM, West SG, Sheets V. A comparison of methods to test mediation and other intervening variable effects. Psychological Methods. 2002;7:83–104. doi: 10.1037/1082-989x.7.1.83. doi:10.1037/1082-989X.7.1.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacMillan HL, Fleming JE, Streiner DL, Lin E, Boyle MH, Jamieson E, et al. Childhood abuse and lifetime psychopathology in a community sample. American Journal of Psychiatry. 2001;158:1878–1883. doi: 10.1176/appi.ajp.158.11.1878. doi:10.1176/appi.ajp.158.11.1878. [DOI] [PubMed] [Google Scholar]
- Marcenko MO, Kemp SP, Larson NC. Childhood experiences of abuse, later substance use and parenting outcomes among low-income mothers. American Journal of Orthopsychiatry. 2000;70:316–326. doi: 10.1037/h0087853. doi:10.1037/h0087853. [DOI] [PubMed] [Google Scholar]
- Manly JT. Advances in research definitions of child maltreatment. Child Abuse and Neglect. 2005;29:425–439. doi: 10.1016/j.chiabu.2005.04.001. doi:10.1016/j.chiabu.2005.04.001. [DOI] [PubMed] [Google Scholar]
- Mayes LC, Truman SD. Substance abuse and parenting. In: Bornstein MH, editor. Handbook of parenting: Vol. 4. Social conditions and applied parenting. 2nd ed Lawrence Erlbaum Associates; Mahwah, NJ: 2002. pp. 329–360. [Google Scholar]
- Miller GA, Chapman JP. Misunderstanding of analysis of covariance. Journal of Abnormal Psychology. 2001;110:40–48. doi: 10.1037//0021-843x.110.1.40. doi:10.1037/0021-843X.110.1.40. [DOI] [PubMed] [Google Scholar]
- Molnar BE, Buka SL, Kessler RC. Child sexual abuse and subsequent psychopathology: Results from the National Comorbidity Survey. American Journal of Public Health. 2001;91:753–760. doi: 10.2105/ajph.91.5.753. doi:10.2105/AJPH.91.5.753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus user’s guide. Fourth edition Authors; Los Angeles: 1998–2006. [Google Scholar]
- Najavits LM, Gallop RJ, Weiss RD. Seeking Safety: Therapy for adolescent girls with PTSD and substance use disorder: A randomized controlled trial. Journal of Behavioral Health Services & Research. 2006;33:453–463. doi: 10.1007/s11414-006-9034-2. doi:10.1007/s11414-006-9034-2. [DOI] [PubMed] [Google Scholar]
- Pereda N, Guilera G, Forns M, Gomez-Benito J. The prevalence of child sexual abuse in community and student samples: A meta-analysis. Clinical Psychology Review. 2009;29:328–338. doi: 10.1016/j.cpr.2009.02.007. doi:10.1016/j.cpr.2009.02.007. [DOI] [PubMed] [Google Scholar]
- Prinz RJ, Sanders MR, Shapiro CJ, Whitaker DJ, Lutzker JR. Population-based prevention of child maltreatment: The U.S. Triple P system population trial. Prevention Science. 2009;10:1–12. doi: 10.1007/s11121-009-0123-3. doi:10.1007/s11121-009-0123-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Repetti RL, Taylor SE, Seeman TE. Risky families: Family social environments and the mental and physical health of offspring. Psychological Bulletin. 2002;128:330–366. doi:10.1037/0033-2909.128.2.330. [PubMed] [Google Scholar]
- Smith DK, Johnson AB, Pears KC, Fisher PA, DeGarmo DS. Child maltreatment and foster care: Unpacking the effects of prenatal and postnatal parental substance use. Child Maltreatment. 2007;12:150–160. doi: 10.1177/1077559507300129. doi:10.1177/1077559507300129. [DOI] [PubMed] [Google Scholar]
- Straus MA, Hamby SL, Finkelhor D, Moore DW, Runyan D. Identification of child maltreatment with the Parent-Child Conflict Tactics Scales: Development and psychometric data for a national sample of American parents. Child Abuse and Neglect. 1998;22:249–270. doi: 10.1016/s0145-2134(97)00174-9. doi:10.1016/S0145-2134(97)00174-9. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration (SAMHSA) Office of Applied Studies The NHSDA Report: Children living with substance-abusing or substance-dependent parents. 2003 Retrieved from www.oas.samhsa.gov/2k3/children/children.pdf.
- Suchman NE, DeCoste C, Castiglioni N, McMahon TJ, Rounsaville B, Mayes L. The Mothers and Toddlers Program, an attachment-based parenting intervention fro substance using women: Post-treatment results from a randomized clinical pilot. Attachment & Human Development. 2010;12:483–504. doi: 10.1080/14616734.2010.501983. doi:10.1080/14616734.2010.501983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Theodore AD, Chang JJ, Runyan DK, Hunter WM, Bangdiwala SI, Agans R. Epidemiologic features of the physical and sexual maltreatment of children in the Carolinas. Pediatrics. 2005;115:e331–e337. doi: 10.1542/peds.2004-1033. doi:10.1542/peds.2004-1033. [DOI] [PubMed] [Google Scholar]
- US Department of Health and Human Services. Administration on Children, Youth and Families . Child maltreatment 2008. Government Printing Office; Washington: US: 2010. [Google Scholar]
- Wasserman DR, Leventhal JM. Maltreatment of children born to cocaine-dependent mothers. American Journal of Diseases of Children. 1993;147:1324–1328. doi: 10.1001/archpedi.1993.02160360066021. [DOI] [PubMed] [Google Scholar]
- Widom CS, Hiller-Sturmhofel S. Alcohol abuse as a risk factor for and consequence of child abuse. Alcohol Research & Health. 2001;25:52–57. [PMC free article] [PubMed] [Google Scholar]
- Widom CS, Ireland T, Glynn PJ. Alcohol abuse in abused and neglected children followed-up: Are they at increased risk? Journal of Studies on Alcohol & Drugs. 1995;56:207–217. doi: 10.15288/jsa.1995.56.207. [DOI] [PubMed] [Google Scholar]
- Widom CS, Marmorstein NR, White HR. Childhood victimization and illicit drug use in middle adulthood. Psychology of Addictive Behaviors. 2006;20:394–403. doi: 10.1037/0893-164X.20.4.394. doi:10.1037/0893-164X.20.4.394. [DOI] [PubMed] [Google Scholar]
- Widom CS, White HR. Three potential mediators of the effects of child abuse and neglect on adulthood substance use among women. Journal of Studies on Alcohol & Drugs. 2008;69:337–347. doi: 10.15288/jsad.2008.69.337. [DOI] [PubMed] [Google Scholar]
- Widom CS, White HR, Czaja SJ, Marmorstein NR. Long-term effects of child abuse and neglect on alcohol use and excessive drinking in middle adulthood. Journal of Studies on Alcohol & Drugs. 2007;68:317–326. doi: 10.15288/jsad.2007.68.317. [DOI] [PubMed] [Google Scholar]
- Williams SL, Rosanbalm KD, Christopoulos C, Dodge KA. Novel methods for estimating community child maltreatment rates. Duke University; Durham, NC: 2009. Unpublished manuscript. [Google Scholar]