Abstract
Background
Anti–N-methyl-d-aspartate receptor (NMDAR) encephalitis is a severe autoimmune disorder characterized by high intrathecal antibody synthesis. Little is known about the long-term follow-up of the cerebrospinal fluid antibody status.
Objective
To describe persistent intrathecal antibody synthesis in a clinically healthy person 15 years after recovering from anti-NMDAR encephalitis.
Design
Case report.
Setting
Academic medical center.
Patient
A 40-year-old woman who had been diagnosed as having encephalitis of unknown origin in 1995.
Main Outcome Measures
Clinical evaluation and NMDAR antibody testing.
Results
On reexamination in 2011, the patient had fully recovered. Investigation of archived as well as follow-up serum and cerebrospinal fluid samples revealed intrathecal synthesis of NMDAR antibodies.
Conclusions
This is the longest follow-up on a patient with anti-NMDAR encephalitis. Our findings emphasize that intrathecal antibody synthesis does not necessarily reflect disease activity and that the significance of NMDAR antibody titers needs to be interpreted for each patient according to the clinical context.
Anti–N-methyl-d-aspartate receptor (NMDAR) encephalitis is a severe autoimmune disorder associated with high intrathecal synthesis of antibodies against the NR1 subunit of the NMDAR.1–3 Serum antibodies may remain detectable for several years after clinical recovery,4 but little is known about the long-term follow-up of cerebrospinal fluid (CSF) antibody synthesis. Herein, we describe a patient who had declining but persistent intrathecal antibody synthesis 15 years after clinical recovery.
REPORT OF A CASE
In 1995, a 25-year-old kindergarten teacher presented with fear and anxiety. On examination, she had severe attention deficits and persecutory delusions. Within a week, she became catatonic and mute and had muscle rigidity and trismus. A week later, generalized myoclonic jerks and severe hyperthermia (temperature, 41.3°C) developed. After the third week, she developed central hypoventilation and required tracheostomy and ventilatory support. Results of blood tests for infectious and autoimmune etiologies and repeated brain magnetic resonance imaging were normal. Electroencephalography and CSF revealed abnormal findings (Figure 1). She was diagnosed as having encephalitis of unknown origin and received full supportive intensive care unit treatment and intravenous acyclovir for 2 weeks. Owing to continuous hyperthermia, no immunosuppression was started.
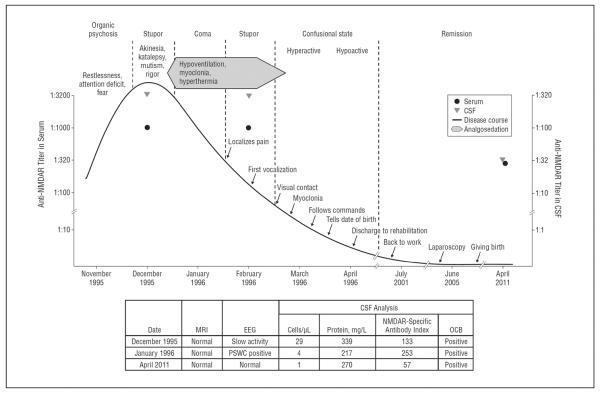
Figure 1.
Time course of clinical features and antibody titers in the cerebrospinal fluid (CSF) and serum. Disease onset in 1995–1996 is associated with high N-methyl-d-aspartate receptor (NMDAR) antibody titers in the CSF and serum, intrathecal antibody synthesis (NMDAR-specific antibody index), lymphocytic pleocytosis, and oligoclonal bands (OCB) in the CSF. Fifteen years after recovery from clinical symptoms, NMDAR antibodies persist in the serum and CSF, with an NMDAR-specific antibody index of 57 reflecting intrathecal antibody synthesis. EEG indicates electroencephalography; MRI, magnetic resonance imaging; and PSWC, periodic sharp wave complexes.
The first signs of improvement were restitution of visual contact and reduction of myoclonic jerks at week 9 after onset. Two weeks later, the patient tried to talk but was very slow, inattentive, amnestic, and dysphasic. She was profusely sweating and hypoventilating predominantly at night, requiring ventilatory support for 6 weeks. For 3 months, she had intense fluctuating episodes of restlessness and stupor. Comprehensive neurorehabilitation programs were started on the intensive care unit and were continued at a specialized institution for 18 months. She progressively recovered regarding goal-directed movements, speaking, learning, and walking and did not develop any clinical relapse.
On reexamination in 2011, she had returned to normal life. Complex motor skills had fully recovered and reached premorbid functional levels 5 years after disease onset (speaking, writing, and dancing). Despite some remaining learning impairment, she successfully completed 24 months of occupational retraining and requalified for her job 6 years after disease onset. Currently, the patient works as an occupational therapist and reports no significant limitation of sustained or divided attention, although she describes occasional difficulties in finding words, a problem that according to her husband is not noticeable. She gave birth to a healthy child 10 years after disease onset. Before her pregnancy, findings of a laparoscopy performed in an infertility clinic had been normal, excluding the presence of a teratoma.
A recent neuropsychiatric evaluation revealed no abnormal findings. In particular, there were no mental slowing, no disinhibition, and no attention deficit.
The patient had normal word fluency and delayed recall on clinical examination. There were no pyramidal or extrapyramidal signs and no involuntary movements or tremor. She had no complaints regarding sleep and had no signs of psychiatric disease. However, the initial clinical presentation was reconsidered and analysis of archived serum and CSF samples obtained at symptom presentation revealed high levels of NMDAR antibodies (Figure 1 and Figure 2), with a calculated antibody-specific index greater than 100 indicating intrathecal synthesis.5 Prompted by these results, follow-up serum and CSF samples were obtained after informed consent, revealinga decline of NMDAR antibody titers. However, significant intrathecal synthesis (antibody-specific index, 57) was still present. The same results were obtained by 2 laboratories (in Lübeck, Germany, and Barcelona, Spain) using several methods: NR1-transfected cell-based assay and immunohistochemical techniques on cultured hippocampal neurons and rat brain tissue, as reported previously.1,5 At symptom presentation and 15 years thereafter, ie, in both early and long-term samples, NMDAR antibodies were of the IgG1 subclass and specific for the NR1 subunit of the receptor.
Figure 2.
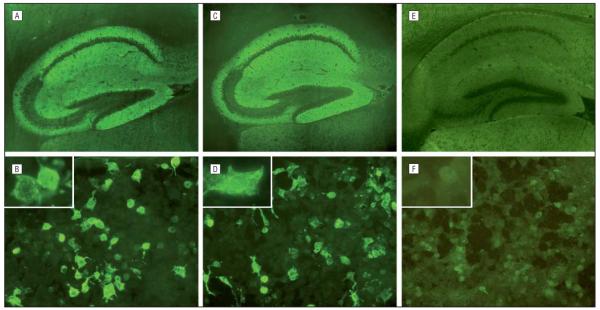
Reactivity of the patient's cerebrospinal fluid at disease onset (A and B) and 15 years thereafter (C and D) and a negative control (E and F). Comparisons of the immunofluorescence pattern on hippocampal sections of mouse brain (A, C, and E; original magnification ×50) and NR1-transfected cells (B, D, and F; original magnification ×200; insets, original magnification ×400) are shown.
COMMENT
We show persistent intrathecal antibody synthesis in a clinically healthy person 15 years after recovering from anti-NMDAR encephalitis, the longest follow-up reported to date to our knowledge. Our findings emphasize that, as in most antibody-mediated disorders including those of the neuromuscular synapse, the significance of antibody titers should be interpreted for each patient according to the clinical context and immunological follow-up (ie, treat the patient, not the serum or CSF antibody titers).6
It is assumed that the immune response underlying this disorder is triggered systemically by a tumor or other unknown causes and is reactivated and expanded in the central nervous system.6 In the brain of patients with acute anti-NMDAR encephalitis, infiltrates of lymphocytes and plasma cells were found in perivascular, interstitial, and Virchow-Robin spaces, providing an explanation for the intrathecal antibody synthesis.7 It is conceivable that in our patient, after a severe disease that lasted many months, the intracerebral inflammatory and plasma cell infiltrates may have disappeared as reflected by normalization of CSF pleocytosis and protein concentration and persistently normal findings on magnetic resonance imaging. However, self-contained meningeal germinal centers with or without systemic antibody synthesis may have remained. This may have resulted in decreased, albeit persistent antibody synthesis without pathogenic effects on the brain. Alternatively but not mutually exclusive, our patient may have chronic mild, subclinical central nervous system autoimmune reactivations with antibody titers below the threshold to cause symptoms. This hypothesis is supported by the observation that relapses are more common in nonparaneoplastic cases and in patients who did not receive immunotherapy in the first episode, as is also the case in our patient.8
Acknowledgments
Funding/Support: Dr Dalmau was supported in part by grants R01NS077851 and R01MH094741 from the National Institutes of Health, grant R01CA89054 from the National Cancer Institute, Fundació la Marató de TV3, and a McKnight Neuroscience of Brain Disorders Award.
Footnotes
Author Contributions: Study concept and design: Hansen and Wandinger. Acquisition of data: Hansen, Li, Weißbrich, and Wandinger. Analysis and interpretation of data: Klingbeil, Dalmau, and Wandinger. Drafting of the manuscript: Hansen, Klingbeil, and Wandinger. Critical revision of the manuscript for important intellectual content: Hansen, Klingbeil, Dalmau, Li, Weißbrich, and Wandinger. Administrative, technical, and material support: Klingbeil, Li, Weißbrich, and Wandinger. Study supervision: Hansen, Dalmau, and Wandinger.
Financial Disclosure: Ms Klingbeil and Drs Li and Wandinger are employees of EUROIMMUN, and Drs Li and Wandinger hold stock in EUROIMMUN. Dr Dalmau receives royalties from the editorial board of Up To Date and from patents for the use of Ma2 and NMDAR as autoantibody test and has received a research grant from EUROIMMUN.
REFERENCES
- 1.Dalmau J, Tüzün E, Wu HY, et al. Paraneoplastic anti-N-methyl-D-aspartate receptor encephalitis associated with ovarian teratoma. Ann Neurol. 2007;61(1):25–36. doi: 10.1002/ana.21050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Irani SR, Bera K, Waters P, et al. N-methyl-D-aspartate antibody encephalitis: temporal progression of clinical and paraclinical observations in a predominantly nonparaneoplastic disorder of both sexes. Brain. 2010;133(pt 6):1655–1667. doi: 10.1093/brain/awq113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Frechette ES, Zhou L, Galetta SL, Chen L, Dalmau J. Prolonged follow-up and CSF antibody titers in a patient with anti-NMDA receptor encephalitis. Neurology. 2011;76(suppl 2):S64–S66. doi: 10.1212/WNL.0b013e31820c34de. 7. [DOI] [PubMed] [Google Scholar]
- 4.Alexopoulos H, Kosmidis ML, Dalmau J, Dalakas MC. Paraneoplastic anti-NMDAR encephalitis: long term follow-up reveals persistent serum antibodies. J Neurol. 2011;258(8):1568–1570. doi: 10.1007/s00415-011-5982-4. [DOI] [PubMed] [Google Scholar]
- 5.Prüss H, Dalmau J, Harms L, et al. Retrospective analysis of NMDA receptor antibodies in encephalitis of unknown origin. Neurology. 2010;75(19):1735–1739. doi: 10.1212/WNL.0b013e3181fc2a06. [DOI] [PubMed] [Google Scholar]
- 6.Dalmau J, Lancaster E, Martinez-Hernandez E, Rosenfeld MR, Balice-Gordon R. Clinical experience and laboratory investigations in patients with anti-NMDAR encephalitis. Lancet Neurol. 2011;10(1):63–74. doi: 10.1016/S1474-4422(10)70253-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Martinez-Hernandez E, Horvath J, Shiloh-Malawsky Y, Sangha N, Martinez-Lage M, Dalmau J. Analysis of complement and plasma cells in the brain of patients with anti-NMDAR encephalitis. Neurology. 2011;77(6):589–593. doi: 10.1212/WNL.0b013e318228c136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gabilondo I, Saiz A, Galán L, et al. Analysis of relapses in anti-NMDAR encephalitis. Neurology. 2011;77(10):996–999. doi: 10.1212/WNL.0b013e31822cfc6b. [DOI] [PubMed] [Google Scholar]