Abstract
Background:
Puerto Ricans share a disproportionate burden of childhood asthma in the United States. Little is known about the impact of low parental numeracy (a health literacy skill) on asthma morbidity in Puerto Rican children. Our objective was to examine whether low parental numeracy is associated with increased asthma morbidity in Puerto Rican children.
Methods:
This was a cross-sectional study of 351 children with asthma, aged 6 to 14 years, living in San Juan, Puerto Rico. Parents of study participants completed a modified version of the Asthma Numeracy Questionnaire. Multivariate linear or logistic regression was used to examine the relation between low parental numeracy (defined as no correct answers in the modified Asthma Numeracy Questionnaire) and indicators of asthma morbidity (severe asthma exacerbations, core measures of asthma exacerbations, and lung function measures). All multivariate models were adjusted for age, sex, household income, reported use of inhaled corticosteroids in the previous 6 months, and exposure to secondhand tobacco smoke.
Results:
Low parental numeracy was associated with increased odds of visits to the ED or urgent care for asthma (adjusted OR [aOR] = 1.7, 95% CI = 1.03-2.7, P = .04). The association between low parental numeracy and hospitalizations for asthma was significant only among children not using inhaled corticosteroids (aOR = 2.8, 95% CI = 1.4-5.6, P = .004). There was no association between low parental numeracy and use of systemic steroids or lung function measures.
Conclusions:
Low parental numeracy is associated with increased asthma morbidity in Puerto Rican children.
Both Puerto Ricans living in the island of Puerto Rico and those living in the mainland United States bear a disproportionate burden of childhood asthma in this country.1‐4 The prevalence of childhood asthma is higher in Puerto Ricans (18.4%) than in non-Hispanic blacks (14.6%) or in non-Hispanic whites (8.2%).5 Compared with non-Hispanic blacks or non-Hispanic whites, Puerto Rican children with asthma also have an increased use of health-care services.6 Little is known about the risk factors that lead to worse asthma outcomes in this population.1,2
Health literacy can be defined as an individual’s capacity to obtain and understand basic information required to make appropriate health decisions.7 Health literacy includes not only reading and writing but also other skills, such as numeracy, the mathematical knowledge required to understand and act upon instructions given by health-care providers (eg, knowing that a prescribed dose of 40 mg of prednisone is the same as taking four 10-mg tablets of prednisone, understanding that a 1% chance is equivalent to a one in 100 chance, and so forth).8,9 The 2003 National Assessment of Adult Literacy found that 44% of adults in the United States have basic or below basic health literacy and that 22% possess no more than the most simple and concrete quantitative skills.10,11 Findings from this national survey also indicate that members of Hispanic subgroups have, on average, the lowest health literacy level of all ethnic groups in this country.11 An increasing body of research suggests that low health literacy may partially explain health disparities for some diseases.12
Parents are largely responsible for following health-care instructions related to asthma management in their children. Among children aged 3 to 12 years, low parental health literacy (assessed primarily by reading skills) has been associated with increased lifetime risk of asthma exacerbations in some studies13 but not others.14 Numeracy appears to be specifically related to asthma outcomes, and higher numeracy has been associated with lower asthma morbidity and higher asthma-related quality of life in adults.15,16 To date, there has been no study of parental numeracy and asthma morbidity in childhood.
We hypothesized that low parental numeracy is associated with increased asthma morbidity in Puerto Rican children, independent of indicators of socioeconomic status and access to health care. To test this hypothesis, we examined the relation between parental numeracy and indicators of asthma morbidity in a cohort of children with asthma living in San Juan, Puerto Rico.
Materials and Methods
Study Population
From March 2009 to June 2010, children in San Juan (Puerto Rico) were chosen from randomly selected households using a scheme similar to that of a prior study.17 In brief, households in the metropolitan area of San Juan were selected by a multistage probability sample design. Primary sampling units were randomly selected neighborhood clusters based on the 2000 United States census, and secondary sampling units were randomly selected households within each individual primary sampling unit. A household was eligible if one or more residents was a child aged 6 to 14 years old. In households with more than one eligible child, one child was randomly selected for screening by using Kish tables.17 On the basis of the sampling design, 7,073 households were selected, and 6,401 (90.5%) were contacted. Of these 6,401 households, 1,111 had one or more children within the age range of the study who met other inclusion criteria (see later description). In an effort to reach a target sample size of approximately 700 children, we attempted to enroll a random sample (n = 783) of these 1,111 children. Parents of 105 of these 783 eligible households refused to participate or could not be reached. There were no significant differences in age, sex, or area of residence between eligible children who did (n = 678 [86.6%]) and did not (n = 105 [13.4%]) agree to participate. We selected as cases children who had parental report of physician-diagnosed asthma and wheeze in the previous year (n = 351). All study participants had to have four Puerto Rican grandparents to ensure that they were of Puerto Rican descent.3 Because we focused on indicators of asthma morbidity, only cases were included in this analysis.
Study Procedures
Study participants completed a protocol that included administration of questionnaires, spirometry, and collection of blood samples (for measurement of serum IgE to common allergens). The child’s parents completed a questionnaire used in the Genetics of Asthma in Costa Rica Study, which was slightly modified from one used in the Collaborative Study of the Genetics of Asthma.18 This questionnaire was used to obtain information about the child’s general and respiratory health, sociodemographic characteristics, family history, (current) exposure to secondhand tobacco smoke, in utero smoking, use of inhaled corticosteroids (ICSs) in the previous 6 months, and asthma outcomes (including information about severe asthma exacerbations19 and core measures of asthma exacerbations20 [see later description]). Parental numeracy was measured in one of the parents using a slightly modified version of the Asthma Numeracy Questionnaire (ANQ), a four-item validated test that uses arithmetic or percentage-based statements or questions derived from the National Asthma Education and Prevention Program guidelines that patients with asthma might encounter during a clinic visit.15 Because peak flow meters are seldom used in Puerto Rico,21 we replaced two of the original questions in the ANQ with one about weight (e-Table 1 (359.3KB, pdf) ). This modification was done with the permission of the developer (Dr Apter). The questionnaire was translated into Spanish by a certified translator and then back-translated into English, with comparison of the two English versions. The number of correct questions ranges from zero to three.
Height and weight were measured to the nearest centimeter and pound, respectively. Spirometry was conducted with an EasyOne spirometer (NDD Medical Technologies, Inc). All subjects had to be free of respiratory illnesses for ≥ 4 weeks before spirometry, and they were also instructed (when possible) to avoid use of inhaled short- and long-acting bronchodilators for ≥ 4 and ≥ 12 h before testing, respectively. Forced expiratory maneuvers were judged to be acceptable if they met or exceeded American Thoracic Society criteria modified for children.22 After performing baseline spirometry, subjects were given two puffs (180 μg) of albuterol through a metered-dose inhaler with a spacer. After waiting 15 min, each subject repeated the spirometric maneuvers to assess bronchodilator responsiveness. The best FEV1 and FVC were selected for data analysis. Serum levels of total IgE and IgE specific to common allergens (dust mite [Der p 1], cockroach [Bla g 2], cat dander [Fel d 1], dog dander [Can f 1], and mouse urinary protein [Mus m 1]) were determined using the UniCAP 100 system (Pharmacia & Upjohn). For each allergen, an IgE ≥ 0.35 IU/mL was considered positive.
Written parental consent was obtained for participating children, from whom written assent was also obtained. The study was approved by Institutional Review Boards of the University of Puerto Rico (San Juan, Puerto Rico), Brigham and Women’s Hospital (Boston, Massachusetts), and the University of Pittsburgh (Pittsburgh, Pennsylvania).
Statistical Analysis
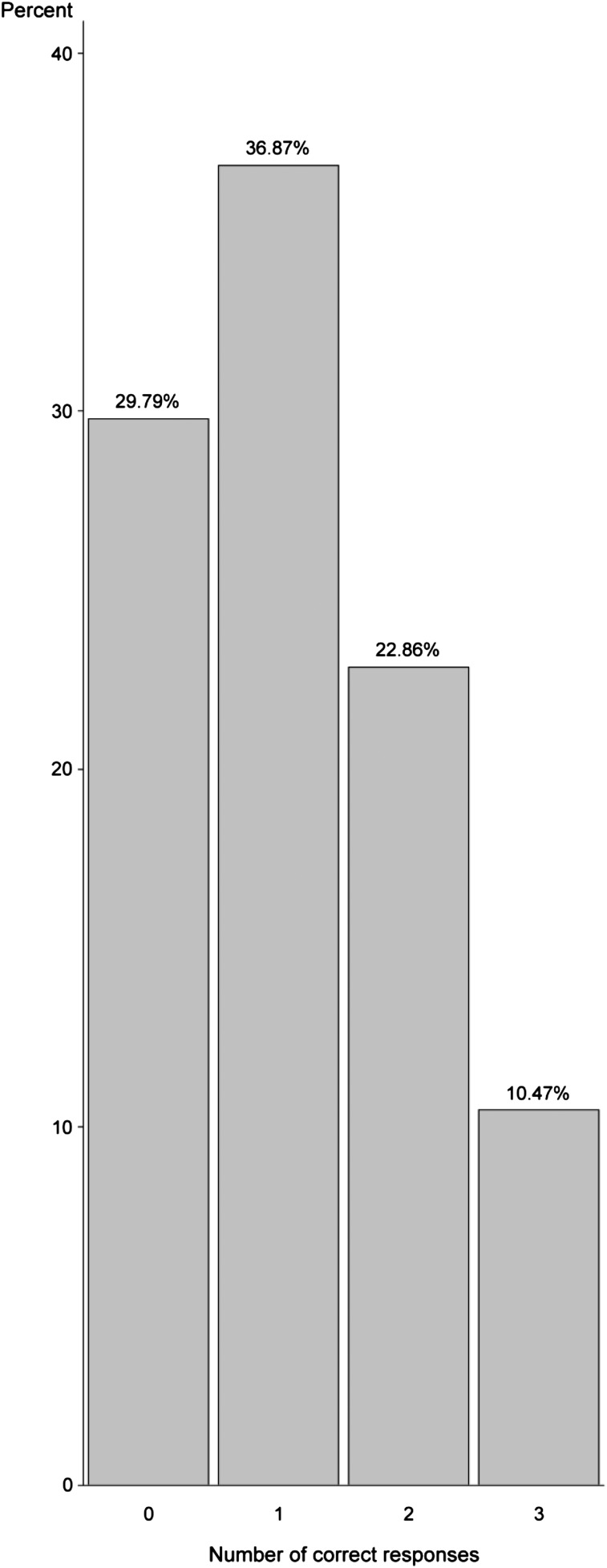
Parental numeracy was treated as a binary variable (ie, 0 vs ≥ 1 correct answer) based on the distribution of correct responses in the modified ANQ (Fig 1). Our primary outcomes were severe asthma exacerbations (≥ 1 course of systemic steroids for asthma in the prior year),19 core measures of asthma exacerbations (≥ 1 visit to the ED or urgent care for asthma in the prior year and ≥ 1 hospitalization for asthma in the prior year),20 and measures of lung function (FEV1 and FEV1/FVC).
Figure 1.
Percentage of number of correct responses in the modified Asthma Numeracy Questionnaire by parents of participating Puerto Rican children with asthma (n = 351).
Because of their potential correlation with numeracy and/or the outcomes of interest, the following covariates were examined in bivariate analyses: age, sex, parental asthma, BMI23 as a z score (based on 2000 Centers for Disease Control and Prevention growth charts24), household income (less than vs ≥ $15,000/y [near the median income for households in Puerto Rico in 2008-200925]), type of health insurance (private or employer-based health insurance vs others), one or more positive allergen-specific IgE, parental education (one or more parents completed high school vs none), parental report of the child’s use of ICS in the prior 6 months, exposure to secondhand tobacco smoke,26 and in utero smoking.
A stepwise approach was used to build the multivariate models using linear or logistic regression. All models included age, sex, household income, use of ICS, and exposure to secondhand tobacco smoke; models for FEV1 were additionally adjusted for height. Additional covariates (described earlier) were included in the initial multivariate models if they were associated with the outcome at a P ≤ .20 in bivariate analyses. Variables remained in the final models if they were statistically significant (P < .05) or if they changed the parameter estimate (β) by ≥ 10%. After the final models were built, we tested for interactions between parental numeracy and other covariates. All analyses were performed using SAS, version 9.3 (SAS Institute, Inc).
Results
The main characteristics of the study participants are shown in Table 1. Although most participating children had one or more parents who graduated from high school, > 60% came from families whose household income was below the median household income for Puerto Rico or did not have private or employer-based health insurance. Overall, approximately 30% of the parents of study participants had low numeracy (no correct answers in the modified ANQ), and only approximately 10.5% of the parents achieved a perfect score in the modified ANQ (Fig 1).
Table 1.
—Baseline Characteristics of Participating Puerto Rican Children With Asthma
| Covariate | N = 351 |
| Age, y | 10.0 (2.6) |
| Female sex | 150 (42.7) |
| BMI, z score | 0.7 (1.2) |
| Exposure to secondhand tobacco smoke | 155 (44.2) |
| In utero smoking | 39 (11.9) |
| Household income < $15,000/y | 225 (65.4) |
| No parent graduated from high school | 63 (17.9) |
| No private or employer-based health insurance | 239 (68.1) |
| No correct answers in the modified ANQ | 109 (31.1) |
| Prebronchodilator FEV1, La | 1.9 (0.7) |
| Prebronchodilator FEV1/FVC | 0.81 (0.1) |
| ≥ 1 Positive allergen-specific IgE level | 210 (68.9) |
Data are presented as No. (%) for binary variables or mean (SD) for continuous variables. ANQ = Asthma Numeracy Questionnaire.
FEV1 presented as absolute values because of lack of predicted values for Puerto Ricans.
Table 2 shows the results of the bivariate analyses of parental numeracy and the covariates or outcomes of interest. Compared with children without low parental numeracy, those with low parental numeracy were significantly less likely to have a household income ≥ $15,000/y, to have one or more parents who graduated from high school, to have private or employer-based health insurance, or to have used ICS in the previous 6 months. Children with low parental numeracy also had a significantly lower BMI and were more likely to have had one or more visits to the ED/urgent care for asthma or to have been hospitalized for asthma in the previous year than children without low parental numeracy. Parental numeracy was not significantly associated with having received one or more courses of systemic corticosteroids in the previous year, lung function measures, or other covariates.
Table 2.
—Baseline Characteristics of Participating Puerto Rican Children With Asthma According to Parental Numeracy
| Covariate | No Correct Answers in the Modified ANQ (n = 109) | ≥ 1 Correct Answer in the Modified ANQ (n = 242) |
| Age, y | 9.8 (2.8) | 10.1 (2.5) |
| Female sex | 42 (38.5) | 108 (44.6) |
| BMI, z score | 0.5 (1.3) | 0.8 (1.1)a |
| ≥ 1 Positive allergen-specific IgE | 60 (63.2) | 150 (71.4) |
| Exposure to secondhand tobacco smoke | 48 (44.0) | 107 (44.2) |
| In utero smoking | 13 (13.0) | 26 (11.4) |
| Household income < $15,000/y | 83 (79.1) | 142 (59.4)b |
| No parent graduated from high school | 29 (26.6) | 34 (14.1)c |
| No private or employer-based health insurance | 87 (79.8) | 152 (62.8)c |
| Use of ICS in the prior 6 mo | 25 (22.9) | 89 (36.8)a |
| History of parental asthma | 73 (67.0) | 159 (66.0) |
| ≥ 1 ED or urgent care visit for asthma in the prior y | 65 (59.6) | 112 (46.3)a |
| ≥ 1 Hospitalization for asthma in the prior y | 32 (29.4) | 43 (17.8)a |
| ≥ 1 Course of systemic steroids for asthma in the prior y | 42 (38.5) | 113 (47.1) |
| Prebronchodilator FEV1,d L | 1.8 (0.7) | 1.9 (0.7) |
| Prebronchodilator FEV1/FVC | 0.8 (0.1) | 0.8 (0.1) |
Data are presented as the No. (%) for binary variables or mean (SD) for continuous variables. ICS = inhaled corticosteroid. See Table 1 legend for expansion of other abbreviation.
P< .05.
P< .001.
P< .01.
FEV1 presented as absolute values because of lack of predicted values for Puerto Ricans.
The child’s mother completed the modified ANQ in 327 of the 351 (93.2%) participants. The proportion of mothers who answered the modified ANQ was similar in children with and without low parental numeracy (90.8% vs 94.2%, P = .26). Table 3 shows the results of the multivariate analysis of parental numeracy and one or more visits to the ED/urgent care for asthma in the previous year. After adjustment for age, sex, household income, use of ICS, and exposure to secondhand tobacco smoke, children with low parental numeracy had nearly twofold greater odds of having had one or more visits to the ED/urgent care than those without low parental numeracy. There was no significant modification of the estimated effect of parental numeracy on ED/urgent care visits for asthma by any of the variables in the model.
Table 3.
—Multivariate Analysis of Parental Numeracy and at Least One ED or Urgent Care Visit for Asthma in the Prior Year in Cases
| Covariate | ≥ 1 ED or Urgent Care Visit for Asthma in the Prior Year |
| Unadjusted | |
| Low parental numeracya | 1.8 (1.1-2.8) (.02) |
| Adjustedb | |
| Low parental numeracy | 1.7 (1.03-2.7) (.04) |
| Household income < $15,000/y | 2.3 (1.4-3.8) (.002) |
| Use of ICS in the prior 6 mo | 2.0 (1.2-3.3) (.007) |
| Exposure to secondhand tobacco smoke | 0.7 (0.5-1.1) (.2) |
Results presented as OR (95% CI) (P value). See Table 2 legend for expansion of abbreviation.
Low parental numeracy defined as no correct answers in the modified Asthma Numeracy Questionnaire.
Multivariate model additionally adjusted for age and sex.
In a multivariate analysis, we found significant evidence for modification of the effect of parental numeracy on asthma hospitalizations by use of ICS (P for interaction = .04). Thus, we conducted the multivariate analysis of parental numeracy and asthma hospitalizations after stratification by use of ICS (Table 4). In this stratified analysis, low parental numeracy was significantly associated with nearly threefold increased odds of having had one or more hospitalizations for asthma in the previous year among children not using ICS. Among cases using ICS, there was no significant association between low parental numeracy and hospitalizations for asthma.
Table 4.
—Multivariate Analysis of Parental Numeracy and at Least One Hospitalization for Asthma in the Prior Year in Cases According to the Use of ICS
| Covariate | Not Using ICS in the Prior 6 mo (n = 237) | Using ICS in the Prior 6 mo (n = 114) |
| Unadjusted | ||
| Low parental numeracya | 3.2 (1.6-6.2) (< .001) | 1.0 (0.4-2.8) (1.0) |
| Adjustedb | ||
| Low parental numeracy | 2.8 (1.4-5.6) (.004) | 0.7 (0.2-2.2) (.6) |
| Household income < $15,000/y | 3.4 (1.1-10.3) (.03) | 4.4 (1.7-11.5) (.002) |
| Exposure to secondhand tobacco smoke | 1.1 (0.6-2.3) (.8) | 1.8 (0.7-4.4) (.2) |
Data are presented as OR (95% CI) (P value) for ≥ 1 hospitalization for asthma in the prior year. See Table 2 legend for expansion of abbreviation.
Low parental numeracy defined as no correct answers in the modified Asthma Numeracy Questionnaire.
All multivariate models additionally adjusted for age and sex.
Because of high collinearity between household income and type of health insurance or parental education, we did not include all indicators of socioeconomic status in the same models. Replacing household income with insurance type or parental education did not significantly change our findings (e-Tables 2 (359.3KB, pdf) , 3 (359.3KB, pdf) ).
To further assess potential confounding by asthma severity, we repeated the multivariate analysis of visits to the ED/urgent care or hospitalizations for asthma after additional adjustment for other indicators of asthma severity or control (FEV1/FVC, one or more positive allergen-specific IgE, and use of leukotriene antagonists), obtaining similar results (e-Tables 4 (359.3KB, pdf) , 5 (359.3KB, pdf) ).
Discussion
We found that low parental numeracy is associated with an increased risk of visits to the ED/urgent care for asthma in Puerto Rican children. In our study, low parental numeracy was also associated with an increased risk of hospitalizations for asthma, but only among children not using ICS. To our knowledge, this is the first report of an association between low parental numeracy and asthma exacerbations in childhood. Our findings are meaningful because, unlike some other sociodemographic characteristics, parental numeracy can potentially be addressed in health-care settings.27,28
Very few studies have examined the association between parental health literacy and childhood asthma. In a retrospective study of 150 children (47% African American and 45% white) attending three outpatient clinics in Chapel Hill, North Carolina, low parental health literacy (assessed using the Rapid Estimate of Adult Literacy in Medicine [REALM], a word-recognition test that measures reading abilities) was associated with an increased risk of ED visits, hospitalizations, use of rescue medications, and school absences for asthma.13 In that study, parents with low health literacy were more likely to have reduced asthma knowledge and to have children with moderate to severe persistent asthma. In contrast to those findings, two larger cross-sectional studies (one using the REALM test and another using a modified version of the Newest Vital Sign, a test that measures both reading comprehension and numeracy) found no significant association between limited parental health literacy and indicators of asthma morbidity or control (ie, ED visits or hospitalizations) in childhood.14,29 However, low parental numeracy was associated with worse parental perception of child’s overall health,14 lower parental quality of life and asthma knowledge,14 or lower parental self-efficacy (ie, a person’s confidence in his or her ability to succeed in a health-related behavior) to manage their child’s asthma.29 The inconsistent results of these studies may be explained by the different tools used to measure health literacy, divergent analytical approaches, and the heterogeneity of participants across studies. In adults, low numeracy has been associated with increased risks of lifetime ED visits and hospitalizations for asthma.15
The management of childhood asthma relies on a parent’s ability to monitor his or her child’s illness, and numeracy is likely required to accomplish complex tasks such as estimating the correct dose of a medication and understanding risks and benefits of asthma treatment.8,30 Numeracy may also promote parental behavior change, influence information-seeking behaviors, and affect health-care system navigation skills.30,31 In addition, numeracy is also closely related to other health literacy skills (ie, reading, writing, speech, speech comprehension, and cultural and conceptual knowledge) as well as self-efficacy.32
In our study, low parental numeracy was associated with one or more hospitalizations for asthma in children who were not on ICS in the previous 6 months. In contrast, there was no significant association between parental numeracy and asthma hospitalizations in children whose parents reported use of ICS in the previous 6 months. The negative finding among children for whom ICS had been prescribed in the recent past could be explained by obscuration of the detrimental effects of low parental numeracy by poverty (eg, if parents of children from low-income households had no private or employer-based health insurance [68.1% of our study participants], they would not be able to continuously purchase ICS once prescribed, thus making parental numeracy less relevant). Consistent with this hypothesis, children from low-income households whose parents reported ICS use in the previous 6 months had nearly fivefold increased odds of having been hospitalized for asthma in the previous year.
The absence of an association between low parental numeracy and use of systemic corticosteroids for asthma is likely due to prescription patterns in the island of Puerto Rico. There is a suboptimal use of ICS in children with asthma and widespread use of systemic steroids in Puerto Rico, especially in children without private or employer-based insurance (due to a current health-care policy that makes providers directly financially responsible for medications costs, a major barrier to the use of relatively expensive medications such as ICS).33‐35
Our study has considerable strengths, including the use of a multistage probability sampling design for subject recruitment and a sample size that is larger than that of any previous study of health literacy and childhood asthma. We also recognize several limitations to our findings. First, our study was cross-sectional, and we are thus unable to assess causal or temporal relationships. For example, the observed association between reported use of ICS and ED/urgent care visits or hospitalizations is likely due to “reverse causation” (eg, if only children with more severe asthma were prescribed ICS). Second, we lack data on adherence to prescribed ICS. Third, low parental numeracy is tightly linked to poverty, and there could thus be residual confounding by socioeconomic status, asthma severity, or other unmeasured factors (eg, housing quality, health beliefs, or cultural patterns). However, confounding by socioeconomic status or disease severity is an unlikely explanation for our findings, because we obtained similar results in multivariate models adjusting for various indicators of socioeconomic status (household income, type of health insurance, or parental education) or asthma severity/control (FEV1/FVC, one or more positive allergen-specific IgE, or use of leukotriene inhibitors). Fourth, we did not measure child’s numeracy, which may be relevant to older children taking most of the responsibility for their asthma care. Fifth, although the ANQ is a validated test, the modified version used for our analyses was not previously validated. Finally, our results may not be generalizable to Puerto Rican children living in the mainland United States (as individuals who emigrate may differ from those who do not) or children in other ethnic groups. However, Puerto Rican children living in the mainland United States are more likely to come from families with a lower socioeconomic status3 and, therefore, are more likely to be exposed to low parental numeracy.
In summary, our results suggest that low parental numeracy leads to increased asthma morbidity in Puerto Rican children independent of indicators of socioeconomic status or access to health care. Longitudinal studies are needed to further examine the relation between parental numeracy and asthma morbidity in Puerto Rican children.
Supplementary Material
Online Supplement
Acknowledgments
Author contributions: Dr Celedón had full access to all the data in the study and he takes full responsibility for the integrity of the data and the accuracy of the data analysis. He also assumes full responsibility for the integrity of the submission as a whole, from inception to published article.
Dr Rosas-Salazar: contributed to data analysis and manuscript writing.
Dr Ramratnam: contributed to data analysis and manuscript writing.
Dr Brehm: contributed to data analysis and manuscript writing.
Dr Han: contributed to data analysis and manuscript writing.
Dr Acosta-Pérez: contributed to data collection and manuscript writing.
Dr Alvarez: contributed to data collection and manuscript writing.
Dr Colón-Semidey: contributed to data collection and manuscript writing.
Dr Canino: contributed to the study design, data collection, data analysis, and manuscript writing.
Dr Apter: contributed to data analysis and manuscript writing.
Dr Celedón: contributed to study design, data collection, data analysis, and manuscript writing.
Financial/nonfinancial disclosures: The authors have reported to CHEST the following conflicts of interest: Dr Apter works on a research project supported by AstraZeneca/Bristol-Myers Squibb Company unrelated to this manuscript. Dr Celedón served as a consultant for Genentech, Inc in 2011 on a topic unrelated to this manuscript. Drs Rosas-Salazar, Ramratnam, Brehm, Han, Acosta-Pérez, Alvarez, Colón-Semidey, and Canino have reported that no potential conflicts of interest exist with any companies/organizations whose products or services may be discussed in this article.
Role of sponsors: The sponsors had no role in the design of the study, the collection of the data, the data analysis, or in the preparation of the manuscript.
Other contributions: We thank all participating children and their families for their invaluable participation in the study.
Additional information: The e-Tables can be found in the “Supplemental Materials” area of the online article.
Abbreviations
- ANQ
Asthma Numeracy Questionnaire
- ICS
inhaled corticosteroid
Footnotes
Funding/Support: This work was supported by the US National Institutes of Health (NIH) [Grant HL079966]. Dr Brehm’s contribution was supported by the NIH [Grant HD052892], and Dr Apter’s contribution was supported by the NIH [Grants HL088469 and HL099612].
Reproduction of this article is prohibited without written permission from the American College of Chest Physicians. See online for more details.
References
- 1.Forno E, Celedon JC. Asthma and ethnic minorities: socioeconomic status and beyond. Curr Opin Allergy Clin Immunol. 2009;9(2):154-160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hunninghake GM, Weiss ST, Celedón JC. Asthma in Hispanics. Am J Respir Crit Care Med. 2006;173(2):143-163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cohen RT, Canino GJ, Bird HR, Shen S, Rosner BA, Celedón JC. Area of residence, birthplace, and asthma in Puerto Rican children. Chest. 2007;131(5):1331-1338 [DOI] [PubMed] [Google Scholar]
- 4.Lara M, Rosenbaum S, Rachelefsky G, et al. Improving childhood asthma outcomes in the United States: a blueprint for policy action. Pediatrics. 2002;109(5):919-930 [DOI] [PubMed] [Google Scholar]
- 5.Moorman JE, Zahran H, Truman BI, Molla MT; Centers for Disease Control and Prevention (CDC) Current asthma prevalence - United States, 2006-2008. MMWR Surveill Summ. 2011;60(Suppl):84-86 [PubMed] [Google Scholar]
- 6.Stingone JA, Claudio L. Disparities in the use of urgent health care services among asthmatic children. Ann Allergy Asthma Immunol. 2006;97(2):244-250 [DOI] [PubMed] [Google Scholar]
- 7.U.S. Department of Health and Human Services Office of Disease Prevention and Health Promotion. Healthy People 2010. Washington, DC: US Government Printing Office; 2000 [Google Scholar]
- 8.Apter AJ, Paasche-Orlow MK, Remillard JT, et al. Numeracy and communication with patients: they are counting on us. J Gen Intern Med. 2008;23(12):2117-2124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nielsen-Bohlman L, Panzer AM, Kindig DA. Institute of Medicine. Committee on Health Literacy. Health literacy: a prescription to end confusion. Washington, DC: The National Academies Press; 2004. http://www.iom.edu/Reports/2004/Health-Literacy-A-Prescription-to-End-Confusion.aspx. Accessed October 15, 2012. [Google Scholar]
- 10.National Center for Education Statistics National Assessment of Adult Literacy (NAAL): A First Look at the Literacy of America’s Adults in the 21st Century. Washington, DC: National Center for Education Statistics; 2005 [Google Scholar]
- 11.National Center for Education Statistics The Health Literacy of America’s Adults: Results from the 2003 National Assessment of Adult Literacy. Washington, DC: National Center for Education Statistics; 2006 [Google Scholar]
- 12.Berkman ND, Sheridan SL, Donahue KE, Halpern DJ, Crotty K. Low health literacy and health outcomes: an updated systematic review. Ann Intern Med. 2011;155(2):97-107 [DOI] [PubMed] [Google Scholar]
- 13.DeWalt DA, Dilling MH, Rosenthal MS, Pignone MP. Low parental literacy is associated with worse asthma care measures in children. Ambul Pediatr. 2007;7(1):25-31 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shone LP, Conn KM, Sanders L, Halterman JS. The role of parent health literacy among urban children with persistent asthma. Patient Educ Couns. 2009;75(3):368-375 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Apter AJ, Cheng J, Small D, et al. Asthma numeracy skill and health literacy. J Asthma. 2006;43(9):705-710 [DOI] [PubMed] [Google Scholar]
- 16.Apter AJ, Wang X, Bogen D, et al. Linking numeracy and asthma-related quality of life. Patient Educ Couns. 2009;75(3):386-391 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bird HR, Canino GJ, Davies M, et al. A study of disruptive behavior disorders in Puerto Rican youth: I. Background, design, and survey methods. J Am Acad Child Adolesc Psychiatry. 2006;45(9):1032-1041 [DOI] [PubMed] [Google Scholar]
- 18.Blumenthal MN, Banks-Schlegel S, Bleecker ER, Marsh DG, Ober C. Collaborative studies on the genetics of asthma–National Heart, Lung and Blood Institute. Clin Exp Allergy. 1995;25(suppl 2):29-32 [DOI] [PubMed] [Google Scholar]
- 19.Fuhlbrigge A, Peden D, Apter AJ, et al. Asthma outcomes: exacerbations. J Allergy Clin Immunol. 2012;129(suppl 3):S34-S48 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Reddel HK, Taylor DR, Bateman ED, et al. ; American Thoracic Society/European Respiratory Society Task Force on Asthma Control and Exacerbations An official American Thoracic Society/European Respiratory Society statement: asthma control and exacerbations: standardizing endpoints for clinical asthma trials and clinical practice. Am J Respir Crit Care Med. 2009;180(1):59-99 [DOI] [PubMed] [Google Scholar]
- 21.Centers for Disease Control and Prevention National Asthma Control Program state profiles: asthma in Puerto Rico. Center for Disease Control and Prevention website. www.cdc.gov/asthma/stateprofiles/Asthma_in_PR.pdf Accessed October 12, 2012.
- 22.American Thoracic Society Standardization of Spirometry, 1994 Update. Am J Respir Crit Care Med. 1995;152(3):1107-1136 [DOI] [PubMed] [Google Scholar]
- 23.Pérez-Perdomo R, Pérez-Cardona C, Disdier-Flores O, Cintrón Y. Prevalence and correlates of asthma in the Puerto Rican population: Behavioral Risk Factor Surveillance System, 2000. J Asthma. 2003;40(5):465-474 [DOI] [PubMed] [Google Scholar]
- 24.Kuczmarski RJ, Ogden CL, Grummer-Strawn LM, et al. CDC growth charts: United States. Adv Data. 2000;(314):1-27 [PubMed] [Google Scholar]
- 25.US Census Bureau Household income for states: 2008 and 2009. US Census Bureau website. http://www.census.gov/prod/2010pubs/acsbr09-2.pdf Accessed September 19, 2012. [Google Scholar]
- 26.Freeman NC, Schneider D, McGarvey P. Household exposure factors, asthma, and school absenteeism in a predominantly Hispanic community. J Expo Anal Environ Epidemiol. 2003;13(3):169-176 [DOI] [PubMed] [Google Scholar]
- 27.Ancker JS, Senathirajah Y, Kukafka R, Starren JB. Design features of graphs in health risk communication: a systematic review. J Am Med Inform Assoc. 2006;13(6):608-618 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lipkus IM. Numeric, verbal, and visual formats of conveying health risks: suggested best practices and future recommendations. Med Decis Making. 2007;27(5):696-713 [DOI] [PubMed] [Google Scholar]
- 29.Wood MR, Price JH, Dake JA, Telljohann SK, Khuder SA. African American parents’/guardians’ health literacy and self-efficacy and their child’s level of asthma control. J Pediatr Nurs. 2010;25(5):418-427 [DOI] [PubMed] [Google Scholar]
- 30.Reyna VF, Nelson WL, Han PK, Dieckmann NF. How numeracy influences risk comprehension and medical decision making. Psychol Bull. 2009;135(6):943-973 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lipkus IM, Peters E. Understanding the role of numeracy in health: proposed theoretical framework and practical insights. Health Educ Behav. 2009;36(6):1065-1081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rosas-Salazar C, Apter AJ, Canino G, Celedón JC. Health literacy and asthma. J Allergy Clin Immunol. 2012;129(4):935-942 [DOI] [PubMed] [Google Scholar]
- 33.Jandasek B, Ortega AN, McQuaid EL, et al. Access to and use of asthma health services among Latino children: the Rhode Island-Puerto Rico asthma center study. Med Care Res Rev. 2011;68(6):683-698 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Canino G, Vila D, Cabana M, et al. Barriers to prescribing controller anti inflammatory medication among Puerto Rican asthmatic children with public insurance: results of national survey of pediatricians. Pediatr Allergy Immunol Pulmonol. 2010;23(3):169-174 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.McQuaid EL, Vasquez J, Canino G, et al. Beliefs and barriers to medication use in parents of Latino children with asthma. Pediatr Pulmonol. 2009;44(9):892-898 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Online Supplement