Abstract
Behavioral dysregulation is a common and detrimental consequence of traumatic brain injury (TBI) in children that contributes to poor academic achievement and deficits in social development. Unfortunately, behavioral dysregulation is difficult to predict from either injury severity or early neuropsychological evaluation. The uncinate fasciculus (UF) connects orbitofrontal and anterior temporal lobes, which are commonly implicated in emotional and behavioral regulation. Using probabilistic diffusion tensor tractography (DTT), we examined the relationship between the integrity of the UF 3 months post-injury and ratings of executive functions 12 months post-injury in children with moderate to severe TBI and a comparison group with orthopedic injuries. As expected, fractional anisotropy of the UF was lower in the TBI group relative to the orthopedic injury group. DTT metrics from the UF served as a biomarker and predicted ratings of emotional and behavior regulation, but not metacognition. In contrast, the Glasgow Coma Scale score was not related to either UF integrity or to executive function outcomes. Neuroanatomical biomarkers like the uncinate fasciculus may allow for early identification of behavioral problems and allow for investigation into the relationship of frontotemporal networks to brain-behavior relationships.
Keywords: Diffusion tensor imaging, Executive function, Neuropsychology, Child, Anisotropy, Behavior
INTRODUCTION
Children who sustain moderate to severe traumatic brain injury (TBI) often demonstrate changes in social and behavioral functioning (Ganesalingam, Sanson, Anderson, & Yeates, 2006; Levin et al., 2004); however, the severity of these difficulties is often not fully appreciated until the child re-enters school and community environments. Dysfunction in neural networks involved in executive processes regulating cognition and behavior may contribute significantly to difficulties in social and behavioral functioning in everyday contexts (Anderson & Catroppa, 2005; Ewing-Cobbs, Prasad, Landry, Kramer, & DeLeon, 2004; Hanten et al., 2008; Levin et al., 2004; Sesma, Slomine, Ding, & McCarthy, 2008).
Executive functions (EF) refers to the self-regulatory processes that direct cognitive activity, emotional responses, and overt goal-directed behavior (Dennis, 1991; Gioia & Isquith, 2004). Fuster (1991) proposed a general subdivision of executive processes into metacognitive versus emotion and behavior regulation. Metacognition refers to establishing a goal and monitoring progress, and modifying one's strategies to meet the goal. Behavioral regulation refers to modulation of emotions and inhibition of inappropriate behaviors. Orbital and medial prefrontal cortex (PFC) were regarded as the substrate for emotional regulation while the dorsolateral PFC was the substrate for metacognitive functions involving the temporal organization of behavior. Fuster's (1991) subdivision of EFs has received support from functional MRI studies that have identified activation of distributed networks involving specific regions of orbital and medial PFC with a variety of emotion and emotion-regulation tasks (Kober et al., 2008; Ochsner et al., 2009; Wager, Davidson, Hughes, Lindquist, & Ochsner, 2008) and activation in dorsal PFC-striatal networks with tasks tapping metacognitive functions, including aspects of working memory, attentional control, and shifting (Bunge & Wright, 2007; Rubia et al., 2006; Somerville & Casey, 2010).
Despite the high rate of occurrence of EF deficits following childhood TBI (Dennis, Guger, Roncadin, Barnes, & Schachar, 2001; Mangeot, Armstrong, Colvin, Yeates, & Taylor, 2002), it has proven challenging to predict which children will develop difficulties and what difficulties they will develop (Anderson & Catroppa, 2005). There is substantial variability in symptom expression across individual children. This variability is likely due to several factors, including differences in pre-injury functioning, extent of focal and diffuse injury, and degree of involvement of the prefrontal regions and related networks. The full effect of TBI on EF may not be appreciable immediately following injury, but may develop later, especially in response to increased demands on the executive system (Gioia & Isquith, 2004). Identification of a neuroanatomical marker capable of predicting likely executive dysfunction would permit early, targeted intervention for children at elevated risk for decline in metacognition or behavioral regulation.
TBI may differentially impact emotional and behavior regulation versus metacognitive processes. The orbitofrontal and anterior temporal lobes are commonly implicated in EF involving behavioral regulation, as well as inhibitory control, reward and punishment analysis, and social cognition (Amodio & Firth, 2006; Bechara, Damasio, & Damasio, 2000; Castellanos, Sonuga-Barke, Milham, & Tannock, 2006; Damasio, 1994). The uncinate fasciculus (UF) has bilateral connectivity of the uncus of the temporal lobe and amygdala with the orbitofrontal cortex (Goldman-Rakic, 1988; Croxson et al., 2005). Key anatomical substrates for metacognition and behavioral regulation, the prefrontal and anterior temporal lobes, are highly vulnerable to focal and diffuse damage following TBI (Bigler, 2007; Levin, 1993; Wilde et al., 2005). The location of the UF makes it particularly susceptible to both immediate impact and shearing injuries. Therefore, TBI may affect both white and gray matter components and the connectivity of networks involved in behavioral and emotional regulation.
Diffusion tensor imaging (DTI) is a promising approach to examining microstructural changes in white and gray matter following TBI and their relations with behavioral outcomes. DTI quantifies macro- and micro-structural changes in both gray matter and white matter through examination of the degree and directionality of the diffusion of water in tissues (Basser, 1997; Eluvathingal, Hasan, Kramer, Fletcher, & Ewing-Cobbs, 2007). DTI provides metrics of diffusivity and anisotropy. The diffusion of water is restricted by several variables, including myelin, cell membranes, intracellular microtubules, and axonal packing (Barkovich, 2005; Le Bihan, 2003; Moseley, Bammer, & Illes, 2002). Fractional anisotropy (FA) reflects the degree of diffusion anisotropy within a voxel, which is related to microstructural tissue characteristics (Pierpaoli & Basser, 1996). Microstructural changes occurring in neurodegenerative disorders, including demyelination or the loss of axonal integrity, are likely to decrease FA (Moseley et al., 2002). Although clarification of the microstructural correlates of these metrics is ongoing, FA is believed to index the integrity and degree of fiber organization. Mean diffusion (MD) has been related to expansion of extracellular space, possibly attributed to neuronal or glial loss (Pierpaoli et al., 2001; Rugg-Gunn, Symms, Barker, Greenwood, & Duncan, 2001; Tasker, 2006). In relation to comparison groups, DTI metrics revealed lower FA and higher mean diffusion in multiple pathways following pediatric TBI. (Ewing-Cobbs et al., 2008; Wilde et al., 2006; Wilde et al., 2010)
Diffusion tensor tractography (DTT) is the mapping of white matter pathways based on the voxel-based values of DTI metrics. Extrapolating directional information from the acquired diffusion metrics, DTT reconstructs large white pathways by creating fibers of likely direction, allowing for full reconstruction of the white matter pathway integrity, rather than relying on individual regions of interest. This method allows investigators to relate the integrity of white matter pathways to cognitive and behavioral outcomes, creating a powerful means for measuring the impact of an injury within a specific neural substrate. However, DTI and DTT have rarely been evaluated in relation to limbic system pathways and to measures of EFs.
The process of determining whether voxels belong to a pathway and the orientation of the fibers can be accomplished using either deterministic or probabilistic methods. Deterministic tractography uses specific algorithms on the nature of the pathway in question to identify the structure of the pathway and define it. Conversely, probabilistic methods of tractography rely on the values at each voxel to determine if and where a tract continues. While deterministic methods produce excellent reconstructions of the intact brain, due to the dysmorphic processes of TBI, assumptions about the structure of pathways and relationship to surrounding brain matter may not hold. Therefore, we chose a probabilistic approach due to its flexibility in accommodating the tight curvature in tracts such as the UF and disruption of tissue integrity and diffusion due to injury (Cook et al., 2005). Probabilistic DTT is also well suited for addressing questions of connectivity between cortical regions and was used to determine connectivity of the UF with regard to two target cortical regions, the anterior temporal pole and the orbitofrontal cortex (Mori & van Zijl, 2002; Johansen-Berg & Behrens, 2006).
In the present study, we evaluated whether probabilistic DTT of the UF obtained 3 months after moderate to severe TBI predicts ratings of metacognition or behavioral regulation at 12 months after injury. The following hypotheses were examined: (1) Using DTT, the UF will show reduced FA and elevated mean diffusion in the TBI group relative to an orthopedic injury comparison group. (2) The DTI metrics derived from tracking of the UF will act as a biomarker, predicting later, specific EF ratings. The DTI metrics will predict ratings of behavioral regulation, but not meta-cognition, at 12 months post-injury due to the specificity of the orbitofrontal and anterior temporal regions in emotional control functions. (3) Probabilistic tractography of the UF will demonstrate superior prognostic capabilities over the Glasgow Coma Scale (GCS) score in predicting EF outcomes.
METHOD
Participants
Participants included children between the ages of 6 and 15 who were hospitalized following a TBI (n = 15) or an orthopedic injury not involving head trauma (n = 15). The severity of TBI was classified as moderate (n = 3) or severe (n = 12) based on the post-resuscitation Glasgow Coma Scale score (Teasdale & Jennett, 1974). Children with preexisting psychiatric diagnoses were excluded from the study. TBI and comparison groups were comparable on age at testing (n(28) = 0.23, ns) and sex (χ2 = 0.56, ns). Additional demographic and injury information is presented in Tables 1 and 2.
Table 1.
Demographic information
| Demographic variables | TBI (n = 15) | Orthopedic (n = 15) |
|---|---|---|
| Years of age at scan (M (SD)) | 10.9 (3.7) | 11.2 (2.7) |
| Gender (% male) | 53 | 67 |
| Handedness (% right) | 100 | 80 |
| Injury Severity Score (M (SD)) | 22.5 (9.1) | 6.5 (2.6) |
| Glasgow Coma Scale score at time of hospital admission (n) | ||
| 3–8 | 9 | — |
| 9–12 | 5 | — |
| 13–15 | 1 | — |
| Radiological characteristics (n) | ||
| Diffuse axonal injury | 12 | — |
| Encephalomalacia | 6 | — |
| Shear injury | 11 | |
| Mechanism of injury (n) | ||
| Motor vehicle accident | 4 | — |
| Pedestrian struck by auto | 5 | — |
| Fall | 6 | — |
Table 2.
Clinical characteristics and radiological findings of TBI group imaged 3 months post-injury
| Age at MRI | Gender | Trauma type | GCS Low | GCS admit | Presence of shear/location | Presence of encephalomalacia/location |
|---|---|---|---|---|---|---|
| 6.8 | F | MVA | 3 | 3 | Bilateral FT | R frontal |
| 13.3 | M | Fall | 3 | 8 | R Temporal | None |
| 13.5 | M | Fall | 9 | 10 | None | None |
| 16.4 | M | PED | 3 | 14 | R Frontal | None |
| 7.9 | M | PED | 3 | 3 | Bilateral Frontal | None |
| 7.4 | F | PED | 3 | 12 | L Temporal | None |
| 7.9 | F | MVA | 3 | 3 | None | None |
| 10.7 | F | MVA | 12 | 12 | L Frontal | None |
| 15.7 | M | Fall | 3 | 12 | None | Bilateral frontal, R temporal |
| 10.4 | M | Fall | 3 | 8 | R Frontal | L temporal |
| 15.6 | M | PED | 3 | 7 | Bilateral FT | L FT |
| 6.5 | M | Fall | 12 | 12 | L FT | None |
| 11.5 | M | MVA | 6 | 6 | L FT | None |
| 11.9 | M | PED | 3 | 3 | Bilateral Frontal | Bilateral frontal |
| 16.3 | F | Fall | 3 | 3 | None | Bilateral frontal |
MVA = motor vehicle accident; PED = pedestrian struck; FT = frontotemporal.
Procedure
All recruitment and testing procedures were approved by the University of Texas Health Science Center at Houston's Committee for the Protection of Human Subjects. Children in both groups received neuropsychological evaluations, including parent rating of behavioral competencies at 12 months after injury and structural MRI an average of 3 months after injury as part of a longitudinal study. All scans were reviewed clinically by a board certified radiologist; all scans of the orthopedic injury and two of the TBI group were read as normal. Written parental consent and child assent were completed for behavioral testing and MRI. For the TBI group, 239 individuals were screened in the emergency room. Of that group, 189 did not meet inclusion criteria. Of the remaining 50, 13 did not wish to participate in the study and 5 could not be approached before discharge. Of the 32 individuals who participated in the study, 17 either failed to complete the neuropsychological testing follow-up at 12 months or had incomplete imaging data. The orthopedic injury group was recruited from the same emergency room as the TBI group. For the orthopedic injury group, 303 individuals were screened in the emergency room. One hundred seventy of those individuals did not meet inclusion criteria. Of the remaining 133 individuals, 62 elected not to participate in the study and 38 were not approached before being discharged from the hospital. Finally, of the 33 individuals who were enrolled in the study, 18 either did not complete the neuropsychological testing at 12 months or had incomplete imaging data. GCS scores for the TBI group were obtained through chart review from the participating hospital. To minimize artificial lowering of GCS scores in children treated pharmacologically, the child's hourly GCS scores were reviewed and the best level of response was coded for each 24-hr period. The lowest post-resuscitation GCS score was the lowest of the “best response” scores obtained.
Executive Function Measure
The Behavior Rating Inventory of Executive Function (BRIEF; Gioia, Isquith, Guy, & Kenworthy, 2000) is an 86-item parental questionnaire assessing everyday EF competencies. The BRIEF has been used to reliably assess TBI outcomes in children up to 5 years post-injury (Gioia & Isquith, 2004; Mangeot et al., 2002). The BRIEF generates eight subscales which combine to form behavioral regulation and metacognition index scores. Index scores allow dissociation of behavior regulation, generally associated with the orbitofrontal cortex from metacognition, which is more closely associated with the dorsolateral prefrontal cortex (Fuster, 1991). The BRIEF has demonstrated greater ecological validity for measuring EF deficits related to activities of daily life, including school performance, than performance-based measures in children with TBI (Gioia & Isquith, 2004; Vriezen & Pigott, 2002). Higher T scores (M = 50, SD = 10) indicate greater difficulty. The BRIEF was administered at 12 months post-injury with standard instructions to rate behavior over the past 6 months. A pre-injury estimate was also collected at the 3-month time point by asking parents to report on behavior for the 6 months before injury.
MR Image Acquisition
All MRIs were performed on a Philips 3T scanner with SENSE (Sensitivity Encoding) technology using an eight-channel phase array head coil. After conventional scout and T2-weighted sequences, a three-dimensional isotropic T1-weighted sequence (MPRAGE) was performed in the coronal plane. Acquisition parameters of the isotropic 3D MPRAGE sequence were as follows: repetition time/echo time = 8.5/4.0 ms; flip angle = 6°; field of view = 240 × 240; matrix = 256 × 256; slice thickness = 0.94 mm; in-plane pixel dimensions (x,y) = 0.94,0.94 mm; number of excitations (NEX) = 1; scan time ~6 min. The DTI sequence consisted of a single-shot spin-echo diffusion sensitized echo-planar imaging sequence with the following parameters: 21 non-collinear equally distributed diffusion encoding directions (e.g., Icosa21; Hasan and Narayana, 2003); repetition time/echo time = 6100/84 ms; b = 0, and 1000 s/mm2; field-of-view = 240 × 240 mm2; matrix = 256 × 256; slice thickness = 3.0 mm; in-plane pixel dimensions (x,y) = 0.94,0.94; SENSE acceleration factor = 2; sequence repeated and averaged twice; scan time ~7 min.
MR Image Analysis
The current method of isolating DTI metrics of the UF involved reconstructing the UF pathway via probabilistic tracking methods from the anterior temporal pole to the orbitofrontal cortex. Once reconstructed, the mean FA and MD values were derived from the resulting tract. This produced more reliable estimates of the DTI metrics than region of interest or single seed methods by being fully computerized and produced more valid estimates of tract integrity by using values from the entire tract rather than a small sample of voxels.
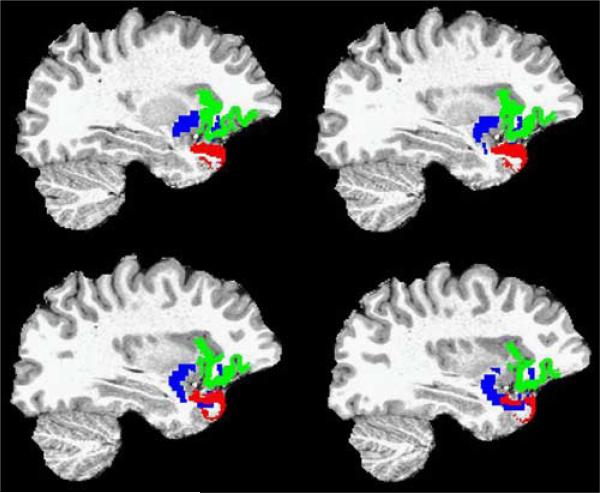
Using Freesurfer v4.1.0 software (www.surfer.nmr.mgh.harvard.edu) on a 64-bit Linux-based computer, whole brain segmentation was performed using the recon-all functionality of Freesurfer (Fischl et al., 2004) to segment the brain into three classes of tissue types: gray matter (GM), white matter (WM), and cerebrospinal fluid (CSF). These cortical areas were subsequently parcellated in Freesurfer according to the Desikan-Killiany parcellation scheme (Desikan et al., 2006), which generates a total of 35 gyral-based regions in each hemisphere, including the anterior temporal pole, lateral and medial orbitofrontal regions. Each subject's high resolution T1-weighted image set and respective Freesurfer generated cortical masks were subsequently co-registered with corresponding non–diffusion-weighted volume using an affine linear registration option included with FSL-FLIRT (fMRI Software Library Linear Image Registration Tool; Smith et al., 2004). This transformation matrix (and its inverse) provided the means to bring the Freesurfer masks from T1-space to DTI space where all tractography functions were conducted to avoid the introduction of normalization based error to the analyses (Allen et al., 2008; Chao et al., 2008; Wallis, Widjaja, Wignall, Wilkinson, & Griffiths, 2006). Probability tracking was then performed between the temporal pole mask (e.g., seed mask) and orbitofrontal mask (e.g., termination mask) using FSL's ProbtrackX package. A total of 5000 samples were initiated from each voxel in the seed mask to the termination mask with a curvature threshold set to 0.2, limiting curvature to approximately 80 degrees or less. Due to between-subjects variability in volumes of the temporal pole seed mask, it was necessary to account for this variability. Therefore, each voxel was divided by the value of waytotal, a value calculated by FSL as the total number of successful streamlines drawn from the seed to the target. This created a voxel over waytotal quotient from which common probability across subjects could be compared to a threshold, set at 1% of all streamlines. Tractography was then limited by fractional anisotropy at 0.2 to minimize the influence of neighboring gray matter. Finally, the seed and target masks were subtracted away from the thresholded tractography mask. The resulting gray matter masks and white matter tract are illustrated for a single subject in four sagittal slices in Figure 1. Mean FA and MD of the tracts were then calculated from the tractography mask using command-line tools included with FSL.
Fig. 1.
Sagittal images demonstrating the gray matter masks for the orbitofrontal cortex (green), anterior temporal pole (red), and the resulting uncinate fasciculus (blue).
Statistical Analyses
The composite scores for the metacognition index, composed of items relating to working memory, initiation, planning, self-monitoring, and organization of materials, and the behavioral regulation index, composed of items relating to emotional control, inhibitory control, and cognitive shifting, were compared between groups via t test to investigate anticipated behavioral differences between the orthopedic injury and TBI groups. Similarly, mean FA and MD values were compared between groups to ascertain if UF metrics on both the left and right varied between the groups. t-tests and χ2 were also used to determine if age or sex differences existed between groups. Differences between pre-injury BRIEF estimates and 12-month outcome scores were compared within each group to examine post-injury changes to executive functioning.
Correlations between left and right UF metrics of both FA and MD were high enough to justify combining hemispheres for analysis. However, to ensure that no hemisphere effect was lost, a preliminary assessment of hemisphere differences in FA and MD as predictors of BRIEF scores was completed. No effect of hemisphere was identified for FA, F(1,26) = 0.01; p = .96, or MD, F(1,26) = 0.01; p = .96, in predicting behavioral regulation scores. Similarly, no effect of hemisphere was identified for FA, F(1,26) = 0.75; p = .39, or MD, F(1,26) = 0.15; p = .70, in predicting metacognition scores.
An analysis of covariance (ANCOVA) was used to evaluate the relationships between UF metrics and the two indices of EF from the BRIEF, including additional independent factors for age and group, as well as interactions between metrics of UF integrity and group membership (TBI vs. orthopedic injury) while covarying for pre-injury estimates. Follow-up analysis involved decomposing the EF composites into component subscales to determine underlying characteristics of the scales which might account for relationships between structure and function.
Within the TBI group, Pearson correlations were used to determine if there was a relationship between GCS at admission and metrics of the UF. These analyses were followed up with an ANOVA exploring the additional variance explained by incorporating UF DTI metrics to predict behavioral regulation after accounting for any variance due to GCS score to determine if additional information about behavioral outcomes could be derived from these metrics. This analysis was replicated with the lowest post-resuscitation GCS score.
RESULTS
Relative to the orthopedic injury group, the TBI group had significantly less favorable ratings on BRIEF behavioral regulation and metacognition index scales (see Table 3). The TBI group demonstrated significant increases in executive dysfunction from pre-injury estimates on scales of emotional control and organization of materials (see Table 4). Neither FA nor MD differed by group in the right UF. Conversely, in the left UF, FA but not MD was significantly lower in the TBI group (see Table 5). No age or sex effects were identified for any of the metrics.
Table 3.
Group differences on BRIEF scales
| BRIEF scales | TBI | Orthopedic | t(28) | η 2 | p |
|---|---|---|---|---|---|
| Behavior regulation | 52.7 (8.6) | 47.0 (6.5) | 2.06 | 0.13 | 0.05 |
| Metacognition | 52.4 (6.4) | 46.1 (6.6) | 2.64 | 0.20 | 0.01 |
| Global Executive | 52.8 (7.2) | 46.3 (6.2) | 2.66 | 0.20 | 0.01 |
Note. Standard deviations presented in parentheses.
Table 4.
Change in BRIEF scores from pre-injury estimate to 12 months post-injury by group
| TBI |
Orthopedic |
|||||||
|---|---|---|---|---|---|---|---|---|
| BRIEF Scales | Pre-injury | 12 month | t(28) | p | Pre-injury | 12 month | t(28) | p |
| Behavioral Regulation Index | 48.3 (9.9) | 52.7 (8.6) | 1.47 | 0.16 | 46.7 (8.7) | 47.0 (6.5) | 0.12 | 0.91 |
| Inhibit | 49.5 (7.0) | 51.1 (8.1) | 0.71 | 0.49 | 47.5 (8.6) | 50.2 (8.6) | 1.27 | 0.23 |
| Shift | 52.1 (14.6) | 52.3 (8.9) | 0.08 | 0.94 | 47.7 (9.3) | 47.3 (6.3) | –0.17 | 0.87 |
| Emotional Control | 46.1 (8.1) | 53.7 (11.5) | 2.12 | 0.05 | 46.5 (8.0) | 44.9 (7.8) | –0.6 | 0.56 |
| Metacognitive Index | 49.7 (9.3) | 52.4 (6.4) | 1.3 | 0.21 | 45.5 (9.3) | 46.1 (6.6) | 0.33 | 0.75 |
| Initiate | 51.4 (8.16) | 53.2 (7.3) | 0.67 | 0.51 | 47.1 (8.9) | 46.0 (7.4) | –0.57 | 0.58 |
| Working Memory | 50.8 (11.0) | 53.7 (7.3) | 1.12 | 0.28 | 46.1 (6.6) | 47.2 (5.3) | 0.53 | 0.6 |
| Plan/Organize | 50.4 (11.4) | 50.7 (6.9) | 0.14 | 0.88 | 45.9 (7.6) | 48.0 (6.6) | 1.06 | 0.31 |
| Organization of Materials | 47.2 (9.0) | 51.1 (8.4) | 2.23 | 0.04 | 46.7 (10.8) | 45.3 (8.5) | –0.93 | 0.37 |
| Monitor | 48.9 (8.9) | 52.7 (7.8) | 1.66 | 0.12 | 44.5 (11.9) | 46.0 (6.1) | 0.53 | 0.61 |
| Global Executive Composite | 49.3 (9.8) | 52.9 (7.2) | 1.47 | 0.16 | 45.5 (9.2) | 46.3 (6.2) | 0.38 | 0.71 |
Table 5.
Group differences on DTI metrics
| TBI | Orthopedic | t(28) | η 2 | p | |
|---|---|---|---|---|---|
| Right uncinate | |||||
| Fractional anisotropy | 0.399 (0.043) | 0.418 (0.030) | 1.44 | 0.07 | 0.16 |
| Mean diffusivity (×1000) | 0.830 (0.035) | 0.812 (0.038) | –1.30 | 0.06 | 0.20 |
| Left uncinate | |||||
| Fractional anisotropy | 0.386 (0.031) | 0.419 (0.033) | 2.87 | 0.23 | 0.01 |
| Mean diffusivity (×1000) | 0.834 (0.031) | 0.820 (0.036) | –1.14 | 0.04 | 0.26 |
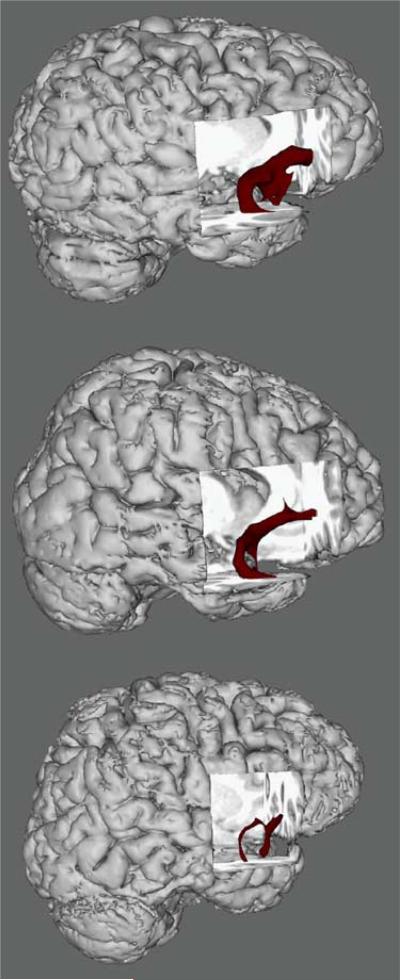
An ANCOVA revealed that UF FA predicted 12 month behavioral regulation, F(1,24) = 6.00; p = .02, but not metacognition, F(1,24) = 0.34; p = .56, after covarying for pre-injury estimates of function. No interaction was found between group and UF FA, but there was a trend toward significance in predicting behavioral regulation, F(1,24) = 3.20; p = .86. Decomposing the behavioral regulation index into component subscales (Emotional Control, Shift, and Inhibit) revealed that the relationship between behavioral regulation and right UF FA was primarily driven by its relationship to emotional control, F(1,26) = 7.96; p = .009. Neither the Shift, F(1,26) = 0.06; p = .82, nor Inhibit, F(1,26) = 1.23; p = .28, subscales were related to uncinate FA. Figure 2 illustrates the relationship between BRIEF outcome scores and white matter integrity between three of the individuals, demonstrating that behavioral regulation score was associated with the integrity of the UF rather than just presence of TBI.
Fig. 2.
Three-dimensional reconstructions of the uncinate fasciculus in three 15-year-old participants (clockwise from top left): (a) orthopedic control participant with good outcome on the Behavioral Regulation Index (T score = 43); (b) traumatic brain injury participant with good outcome on the Behavioral Regulation Index (T = 52), and (c) traumatic brain injury participant with poor outcome on the Behavioral Regulation Index (T = 63).
No significant correlations could be identified between GCS score at hospital admission and UF DTI metrics within the TBI group. Neither FA, r(15) = 0.40; p = .14, nor MD r(15) = −0.45; p = .09, was correlated with GCS admission score. Additionally, UF FA predicted behavioral regulation beyond that accounted for by admission GCS, F(1,12) = 6.45; p = .026. The model including only GCS predicted little of the variance in behavioral regulation, R2 = 0.026, while a model including FA was much more predictive, R2 = 0.366.
Similarly, no significant correlations could be identified between lowest recorded GCS score and UF DTI metrics within the TBI group. Neither FA, r(15) = 0.15; p = .60, nor MD r(15) = −0.02; p = .94 was correlated with lowest recorded GCS score. Additionally, UF FA predicted behavioral regulation beyond that accounted for by lowest recorded GCS, F(1,12) = 6.38; p = .027. The model including only GCS predicted little of the variance in behavioral regulation, R2 = 0.104, while a model including FA was much more predictive, R2 = 0.415.
DISCUSSION
TBI is associated with long-term cognitive and behavioral sequelae. Due to the heterogeneous nature of TBI, the outcomes of a specific injury are difficult to predict (Schwartz et al., 2003; Taylor et al., 2002). The tremendous variability in the severity of injury and degree of diffuse and multifocal injury to cortical and subcortical structures is paralleled by variable cognitive and behavioral outcomes. The current study demonstrated the utility of probabilistic gray matter target connectivity based analyses of DTI obtained at 3 months following moderate to severe TBI or orthopedic injury for predicting specific EF outcomes assessed 1 year after injury. As predicted, DTT metrics from the UF indicated reduced FA in the TBI group relative to the orthopedic injury group. This effect was only seen in the left UF and is possibly a result of the vagaries of a small sample with more left sided injuries. DTT metrics from the UF served as a biomarker and predicted ratings of EF obtained 1 year after brain injury. The pattern of findings supported our hypothesis that elevated behavioral dysregulation would be predicted specifically by FA from the UF. Within the behavioral regulation factor score, the emotional control subscale was strongly related to measures of FA from the UF. As expected, metacognitive difficulties were not predicted by DTT metrics from the UF. Additionally, UF MD was not predictive of behavioral regulation score on the BRIEF, in contrast to one of our hypotheses. However, this finding is not wholly unexpected as MD is less sensitive to the effects of TBI in white matter pathways and FA is more associated with cognitive functions (Ewing-Cobbs, Hasan, Prasad, Kramer, & Bachevalier, 2006; Huisman et al., 2004; Levin et al., 2008). The lack of change in MD is informative despite its lack of relation to cognitive changes because dramatic decreases in MD might suggest global alterations in the diffusion characteristics of the brain, limiting the utility of FA as a predictor (Hasan, 2006). FA predicted EF outcomes above and beyond either the GCS score obtained at admission or the lowest post-resuscitation score. Clearly, DDT metrics were strongly related to behaviors affected by moderate to severe TBI and were differentially related to specific EF outcomes.
DTT as a Biomarker of UF Disruption
Commonly used measures of injury severity, such as the GCS score, are useful for predicting global outcomes in groups of patients but are not particularly sensitive predictors of specific outcomes. Given the limitations of the GCS score in predicting outcome after TBI, there is increasing interest in using pathoanatomic variables derived from neuroimaging studies in multivariate prognostic modeling to more precisely characterize injury severity, predict outcomes, and classify patients into more homogeneous groups for intervention protocols (Saatman et al., 2008; Steyerberg et al., 2008).
DTT has great potential for serving as a biomarker of integrity of frontotemporal connectivity. The UF is a candidate pathway for investigation of prognosis following TBI because TBI often involves injury to frontotemporal gray and white matter (Bigler, 2007; Wilde et al., 2005), and is often associated with cognitive and behavioral dysregulation. We found evidence of UF disruption that was not always identifiable on structural MRI. Additionally, GCS was a poor predictor of both UF disruption and EF dysfunction. The UF has previously been identified as a pathway not associated with GCS despite GCS predicting other major white matter pathways (Bendlin et al., 2008).
At the level of predicting individual outcome domains, inclusion of neuroimaging variables can also enhance prediction of outcomes following pediatric TBI. Inclusion of presence/absence of lesions in the frontal lobes and related functional networks has significantly improved predictions of some outcomes. For example, unilateral lesions of the frontal lobes, but not extrafrontal lesions, were associated with less favorable socialization and greater maladaptive behaviors (Levin et al., 2004). The likelihood of developing secondary attention-deficit/hyperactivity disorder was significantly greater in children with focal lesions in the orbital frontal lobes (Max et al., 2005), thalamus, or basal ganglia (Gerring et al., 2000; Herskovits, Gerring, Bavatzikos, & Bryan, 1999). Frontal lobe lesion volume, but not hippocampal volume, was associated with learning and memory performance following severe TBI (Di Stefano et al., 2000). DTI has advantages over measures of regional tissue volume or lesion volume in predicting outcomes. DTI can quantify tissue integrity as well as the connectivity of specific circuitry in relation to specific cognitive and behavioral EF outcomes. Unlike lesion volumes that can only be evaluated in a subset of study participants, DTI metrics can be obtained in both healthy participants and in those with TBI of all severities. This allows investigation of the contribution of components of frontotemporal networks to brain behavioral relationships across populations and across the range of injury severity.
The use of DTT to identify changes to specific pathways after TBI may allow for behavioral interventions to be introduced before the appearance of significant cognitive or behavioral disturbances. At present, most injuries require a “wait-and-see” approach in which significant sequelae are only identified after performance begins to decline in school or on repeated neuropsychological evaluations over a period of time. Children with TBI must first demonstrate a deficit before interventions can be implemented. If more specific predictors of emotional and behavioral regulation could be identified shortly after injury, then targeted interventions could be introduced substantially earlier to children at greatest risk.
DTT of the UF in Relation to Executive Function Outcomes
The importance of frontotemporal connections to adequate social functioning has been emphasized in several clinical populations, including autism spectrum disorders (Bachevalier & Loveland, 2006; Barnea-Goraly et al., 2004; Lee et al., 2007; Pugliese et al., 2009), schizophrenia (Highley, Walker, Esiri, Crow, & Harrison, 2002; Kubicki et al., 2002), temporal lobe epilepsy (Diehl et al., 2008; Lin, Riley, Juranek, & Cramer, 2008), and early socioemotional deprivation (Eluvathingal et al., 2006). Additional investigation of similarities and differences in cognitive and behavioral dysregulation identified in these populations in relation to specific DTI metrics will provide refinement of theories of orbitofrontal connectivity with temporal and amygdalar regions. Tractography and connectivity studies hold much promise for clarifying relations between limbic system components and their unique contribution to emotion regulation.
LIMITATIONS AND FUTURE DIRECTIONS
Probabilistic tractography is, by its very nature, an exclusionary process. Due to the selective nature of tracking, the identified tract represents only areas of certain, intact, well-organized, fiber bundles. Specifically, the step-by-step filtering of the uncinate pathway by probability, FA, and grey matter borders reduces the data to a pathway that could be defined as almost certainly intact white matter that is part of the UF. However, DTT makes no inference about the microstructural characteristics of surrounding fibers or the strength of connectivity of the pathway with gray matter.
Additional limitations of the present study include the small sample size which precludes evaluation of other variables, such as gender, that might influence both DTI metrics and behavioral outcomes. Like many TBI studies, the small sample size also allows for great variation between injury characteristics as can be seen in Table 2. The presence of more left than right sided injuries explains the significant effect of TBI on left UF FA and weak trend toward significance on right UF FA in the current sample. Identification of pathways that predict specific components of metacognition would contribute significantly to the emergent literature relating specific EF to networks of specific gray matter regions and pathways. Moreover, in the present study, both behavior and DTT were evaluated at one time point. Following additional participants in a longitudinal design will allow for more specific investigation of the behavioral correlates of injury to the UF. Recent longitudinal investigation of diffusion tensor metrics following TBI suggests a reduction in FA by 2 months post-injury and a further reduction by 1 year post-injury (Bendlin et al., 2008). This suggests that TBI results in traumatic axonal injury that can be measured via FA values shortly after injury, with continued reductions likely due to secondary effects such as Wallerian degeneration and gliosis. While the finding that DTI metrics better predicted specific behavioral outcomes than GCS scores provides valuable information as to the power of diffusion tensor methods, it would be useful to compare the utility of DTI metrics of the UF to a better predictor of outcome, such as length of post-traumatic amnesia. Additionally, the range of GCS was restricted to a small amount of variation within this small sample and GCS may be more predictive of outcome within a greater range of coma symptoms. However, the number of severe scores does still suggest that within more severe TBIs GCS is not a powerful predictor of behavioral outcome.
In children, characterization of consequences of frontal lobe injury can be further complicated by the protracted development of these substrates and their associated functions. Therefore, the full extent of functional deficits may not become apparent until further maturation has occurred and the child fails to develop cognitive and behavioral control at an age-appropriate rate or to an age-appropriate level (Goldman, 1974; Eslinger, Grattan, Damasio, & Damasio, 1992). Due to these factors, it is essential to examine how interrelationships among behavioral changes, white matter integrity, and strength of connectivity of key white and gray matter regions evolve over time.
ACKNOWLEDGMENTS
This work was funded by NIH-NINDS-R01-NS046308 awarded to LEC. Portions of this study were awarded the Phillip M. Rennick award when presented as a poster at the 38th Annual Meeting of the International Neuropsychological Society in Acapulco.
Footnotes
No conflicts of interest exist.
REFERENCES
- Allen JS, Brusss J, Mehta S, Grabowski T, Brown CK, Damasio H. Effects of spatial transformation on regional brain volume estimates. Neuroimage. 2008;42:535–547. doi: 10.1016/j.neuroimage.2008.05.047. doi:10.1016/j.neuroimage.2008.05.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amodio DM, Firth CD. Meeting of minds: The medial frontal cortex and social cognition. Nature Reviews Neuroscience. 2006;7:268–277. doi: 10.1038/nrn1884. doi:10.1038/nrn1884. [DOI] [PubMed] [Google Scholar]
- Anderson V, Catroppa C. Recovery of executive skills following paediatric traumatic brain injury (TBI): A 2 year follow-up. Brain Injury. 2005;19:459–470. doi: 10.1080/02699050400004823. doi:10.1080/02699050400004823. [DOI] [PubMed] [Google Scholar]
- Bachevalier J, Loveland KA. The orbitofrontalamygdala circuit and self-regulation of social-emotional behavior in autism. Neuroscience & Biobehavioral Review. 2006;30:97–117. doi: 10.1016/j.neubiorev.2005.07.002. doi:10.1016/j.neubiorev.2005.07.002. [DOI] [PubMed] [Google Scholar]
- Barkovich AJ. Pediatric neuroimaging. Lippincott Williams & Wilkins; Baltimore: 2005. [Google Scholar]
- Barnea-Goraly N, Kwon H, Menon V, Eliez S, Lotspeich L, Reiss AL. White matter structure in autism: Preliminary evidence from diffusion tensor imaging. Biological Psychiatry. 2004;55:323–326. doi: 10.1016/j.biopsych.2003.10.022. doi:10.1016/j.biopsych.2003.10.022. [DOI] [PubMed] [Google Scholar]
- Basser PJ. New histological and physiological stains derived from diffusion-tensor MR images. Annals of the New York Academy of Sciences. 1997;820:123–138. doi: 10.1111/j.1749-6632.1997.tb46192.x. doi:10.1111/j.1749-6632.1997.tb46192.x. [DOI] [PubMed] [Google Scholar]
- Bechara A, Damasio H, Damasio AR. Emotion, decision making, and the orbitofrontal cortex. Cerebral Cortex. 2000;10:295–307. doi: 10.1093/cercor/10.3.295. doi:10.1093/cercor/10.3.295. [DOI] [PubMed] [Google Scholar]
- Bendlin BB, Ries ML, Lazar M, Alexander AL, Dempsey RJ, Rowley HA, Johnson SC. Longitudinal changes in patients with traumatic brain injury assessed with diffusion-tensor and volumetric imaging. Neuroimage. 2008;42:503–514. doi: 10.1016/j.neuroimage.2008.04.254. doi:10.1016/j.neuroimage.2008.04.254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bigler ED. Anterior and middle cranial fossa in traumatic brain injury: Relevant neuroanatomy and neuropathology in the study of neuropsychological outcome. Neuropsychology. 2007;21:515–531. doi: 10.1037/0894-4105.21.5.515. doi:10.1037/0894-4105.21.5.515. [DOI] [PubMed] [Google Scholar]
- Bunge SA, Wright SB. Neurodevelopmental changes in working memory and cognitive control. Current Opinion in Neurobiology. 2007;17:243–250. doi: 10.1016/j.conb.2007.02.005. doi:10.1016/j.conb.2007.02.005. [DOI] [PubMed] [Google Scholar]
- Castellanos FX, Sonuga-Barke EJS, Milham MP, Tannock R. Characterizing cognition in ADHD: Beyond executive dysfunction. Trends in Cognitive Science. 2006;10:117–123. doi: 10.1016/j.tics.2006.01.011. doi:10.1016/j.tics.2006.01.011. [DOI] [PubMed] [Google Scholar]
- Chao YP, Chen JH, Cho KH, Yeh CH, Chou KH, Lin CP. A multiple streamline approach to high angular resolution diffusion tractography. Medical Engineering & Physics. 2008;30:989–996. doi: 10.1016/j.medengphy.2008.01.010. [DOI] [PubMed] [Google Scholar]
- Cook PA, Zhang H, Avants BB, Yushkevich P, Alexander DC, Gee JC, Thompson AJ. An automated approach to connectivity-based partitioning of brain structures. Lecture Notes in Computer Science. 2005;3749:164–171. doi: 10.1007/11566465_21. doi:10.1007/11566465_21. [DOI] [PubMed] [Google Scholar]
- Croxson PL, Johansen-Berg H, Behrens TEJ, Robson MD, Pinsk MA, Gross CG, Rushworth MFS. Quantitative investigation of connections of the prefrontal cortex in the human and macaque using probabilistic diffusion tractography. The Journal of Neuroscience. 2005;25:8854–8866. doi: 10.1523/JNEUROSCI.1311-05.2005. doi:10.1523/JNEUROSCI.1311-05.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Damasio AR. Descartes’ error: Emotion, reason, and the human brain. Putnam; New York: 1994. [Google Scholar]
- Dennis M. Frontal lobe function in childhood and adolescence: A heuristic for assessing attention regulation, executive control, and the intentional states important for social discourse. Developmental Neuropsychology. 1991;7:327–358. [Google Scholar]
- Dennis M, Guger S, Roncadin C, Barnes M, Schachar R. Attentional-inhibitory control and social-behavioral regulation after childhood closed head injury: Do biological, developmental, and recovery variables predict outcome? Journal of the International Neuropsychological Society. 2001;7:683–692. doi: 10.1017/s1355617701766040. [DOI] [PubMed] [Google Scholar]
- Desikan RS, Segonne F, Fischl B, Quinn BT, Dickerson BC, Blacker D, Killiany RJ. An automated labeling system for subdividing the human cerebral cortex on MRI scans into gyral based regions of interest. Neuroimage. 2006;31:968–980. doi: 10.1016/j.neuroimage.2006.01.021. doi:10.1016/j.neuroimage.2006.01.021. [DOI] [PubMed] [Google Scholar]
- Di Stefano G, Bachevalier J, Levin HS, Song J, Scheibel RS, Fletcher JM. Volume of focal brain lesions and hippocampal formation in relation to memory function after closed head injury in children. Journal of Neurology, Neurosurgery, and Psychiatry. 2000;69:210–216. doi: 10.1136/jnnp.69.2.210. doi:10.1136/jnnp.69.2.210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diehl B, Busch RM, Duncan JS, Piao Z, Tkach J, Luders HO. Abnormalities in diffusion tensor imaging of the uncinate fasciculus relate to reduced memory in temporal lobe epilepsy. Epilepsia. 2008;49:1409–1418. doi: 10.1111/j.1528-1167.2008.01596.x. doi:10.1111/j.1528-1167.2008.01596.x. [DOI] [PubMed] [Google Scholar]
- Eslinger PJ, Grattan LM, Damasio H, Damasio AR. Developmental consequences of childhood frontal lobe damage. Archives of Neurology. 1992;49:764–769. doi: 10.1001/archneur.1992.00530310112021. [DOI] [PubMed] [Google Scholar]
- Eluvathingal TJ, Chugani HT, Behen ME, Juhasz C, Muzik O, Maqbool M, Makki M. Abnormal brain connectivity in children after early severe socioemotional deprivation: A diffusion tensor imaging study. Pediatrics. 2006;117:2093–2100. doi: 10.1542/peds.2005-1727. doi:10.1542/peds.2005-1727. [DOI] [PubMed] [Google Scholar]
- Eluvathingal TJ, Hasan KM, Kramer L, Fletcher JM, Ewing-Cobbs L. Quantitative diffusion tensor tractography of association and projection fibers in normally developing children and adolescents. Cerebral Cortex. 2007;17:2760–2768. doi: 10.1093/cercor/bhm003. doi:10.1093/cercor/bhm003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ewing-Cobbs L, Hasan KM, Prasad MR, Kramer L, Bachevalier J. Corpus callosum diffusion anisotropy correlates with neuropsychological outcomes in twins disconcordant for traumatic brain injury. American Journal of Neuro-radiology. 2006;27:879–881. [PMC free article] [PubMed] [Google Scholar]
- Ewing-Cobbs L, Prasad MR, Landry SH, Kramer L, DeLeon R. Executive functions following traumatic brain injury in young children: A preliminary analysis. Developmental Neuropsychology. 2004;26:487–512. doi: 10.1207/s15326942dn2601_7. doi:10.1207/s15326942dn2601_7. [DOI] [PubMed] [Google Scholar]
- Ewing-Cobbs L, Prasad MR, Swank P, Kramer L, Cox CS, Fletcher JM, Hasan KM. Arrested development and disrupted callosal microstructure following pediatric traumatic brain injury. Neuroimage. 2008;42:1305–1315. doi: 10.1016/j.neuroimage.2008.06.031. doi:10.1016/j.neuroimage.2008.06.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fischl B, van der Kouwe A, Destrieux C, Halgren E, Ségonne F, Salat DH, Dale AM. Automatically parcellating the human cerebral cortex. Cerebral Cortex. 2004;14:11–22. doi: 10.1093/cercor/bhg087. doi:10.1093/cercor/bhg087. [DOI] [PubMed] [Google Scholar]
- Fuster JM. The prefrontal cortex and its relation to behavior. Progress in Brain Research. 1991;87:201–211. doi: 10.1016/s0079-6123(08)63053-8. doi:10.1016/S0079-6123(08)63053-8. [DOI] [PubMed] [Google Scholar]
- Ganesalingam K, Sanson A, Anderson V, Yeates KO. Self-regulation and social and behavioral functioning following childhood traumatic brain injury. Journal of the International Neuropsychological Society. 2006;12:609–621. doi: 10.1017/S1355617706060796. doi:10.1017/S1355617706060796. [DOI] [PubMed] [Google Scholar]
- Gerring J, Brady K, Chen A, Quinn C, Herskovits E, Bandeen-Roche K, Bryan RN. Neuroimaging variables related to development of secondary attention deficit hyperactivity disorder after closed head injury in children and adolescents. Brain Injury. 2000;14:205–218. doi: 10.1080/026990500120682. [DOI] [PubMed] [Google Scholar]
- Gioia GA, Isquith PK. Ecological assessment of executive function in traumatic brain injury. Developmental Neuropsychology. 2004;25:135–158. doi: 10.1080/87565641.2004.9651925. [DOI] [PubMed] [Google Scholar]
- Gioia GA, Isquith PK, Guy SC, Kenworthy L. Behavior rating inventory of executive function. Psychological Assessment Resources; Odessa, FL: 2000. [Google Scholar]
- Goldman PS. An alternative to developmental plasticity: Heterology of CNS structures in infants and adults. In: Stein DG, Rosen JJ, Butters N, editors. Plasticity and recovery of function in the central nervous system. Academic; New York: 1974. pp. 149–174. [Google Scholar]
- Goldman-Rakic PS. Topography of cognition: Parallel distributed networks in primate association cortex. Annual Review of Neuroscience. 1988;11:137–156. doi: 10.1146/annurev.ne.11.030188.001033. doi:10.1146/annurev.ne.11.030188.001033. [DOI] [PubMed] [Google Scholar]
- Hanten G, Wilde EA, Menefee DS, Li X, Lane S, Vasquez C, Levin HS. Correlates of social problem solving during the first year after traumatic brain injury in children. Neuropsychology. 2008;22:357–370. doi: 10.1037/0894-4105.22.3.357. doi:10.1037/0894-4105.22.3.357. [DOI] [PubMed] [Google Scholar]
- Hasan KM. Diffusion tensor eigenvalues or both mean diffusivity and fractional anisotropy are required in quantitative clinical diffusion tensor MR reports: Fractional anisotropy alone is not sufficient. Radiology. 2006;236:221–230. doi: 10.1148/radiol.2392051172. doi:10.1148/radiol.2392051172. [DOI] [PubMed] [Google Scholar]
- Hasan KM, Narayana PA. DTI parameter optimization at 3.0T: Potential application in entire normal human brain mapping and multiple sclerosis research. Medicamundi. 2003;49:30–45. [Google Scholar]
- Herskovits E, Gerring JP, Davatzikos C, Bryan RN. Is the spatial distribution of brain lesions associated with closed-head injury in children predictive of subsequent development of posttraumatic stress disorder? Radiology. 1999;224:345–351. doi: 10.1148/radiol.2242011439. doi:10.1148/radiol.2242011439. [DOI] [PubMed] [Google Scholar]
- Highley JR, Walker MA, Esiri MM, Crow TJ, Harrison PJ. Asymmetry of the uncinate fasciculus: A postmortem study of normal subjects and patients with schizophrenia. Cerebral Cortex. 2002;12:1218–1224. doi: 10.1093/cercor/12.11.1218. doi:10.1093/cercor/12.11.1218. [DOI] [PubMed] [Google Scholar]
- Huisman TA, Schwann LH, Schaefer PW, Koroshetz WJ, Shetty-Alva N, Ozsunar OW, Sorensen AG. Diffusion tensor imaging as potential biomarker of white matter injury in diffuse axonal injury. AJNR American Journal of Neuroradiology. 2004;25:370–376. [PMC free article] [PubMed] [Google Scholar]
- Kober H, Barrett LF, Joseph J, Bliss-Moreau E, Lindquist K, Wager TD. Functional grouping and cortical-subcortical interactions in emotion: A meta-analysis of neuroimaging studies. Neuroimage. 2008;42:998–1031. doi: 10.1016/j.neuroimage.2008.03.059. doi:10.1016/j.neuroimage.2008.03.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kubicki M, Westin CF, Maier SE, Mamata H, Frumin M, Ersner-Hershfield H, Shenton ME. Diffusion tensor imaging and its application to neuropsychiatric disorders. Harvard Review of Psychiatry. 2002;10:324–336. doi: 10.1080/10673220216231. doi:10.1080/10673220216231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johansen-Berg H, Behrens TEJ. Just pretty pictures? What diffusion tractography can add in clinical neuroscience. Current Opinion in Neurology. 2006;19:379–385. doi: 10.1097/01.wco.0000236618.82086.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Le Bihan D. Looking into the functional architecture of the brain with diffusion MRI. Nature Reviews Neuroscience. 2003;4:469–480. doi: 10.1038/nrn1119. doi:10.1016/j.ics.2006.04.006. [DOI] [PubMed] [Google Scholar]
- Lee JE, Bigler ED, Alexander AL, Lazar M, DuBray MB, Chung MK, Lainhart JE. Diffusion tensor imaging of white matter in the superior temporal gyrus and temporal stem in autism. Neuroscience Letters. 2007;424:127–132. doi: 10.1016/j.neulet.2007.07.042. doi:10.1016/j.neulet.2007.07.042. [DOI] [PubMed] [Google Scholar]
- Levin HS. Head trauma. Current Opinion in Neurology. 1993;6:841–846. doi: 10.1097/00019052-199312000-00003. [DOI] [PubMed] [Google Scholar]
- Levin HS, Wilde EA, Chu Z, Yallampalli R, Hanten GR, Li X, Hunter JV. Diffusion tensor imaging in relation to cognitive and functional outcome of traumatic brain injury. Journal of Head Trauma Rehabilitation. 2008;23:197–208. doi: 10.1097/01.HTR.0000327252.54128.7c. doi:10.1097/01.HTR.0000327252.54128.7c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levin HS, Zhang L, Dennis M, Ewing-Cobbs L, Schachar R, Max J, Hunter JV. Psychosocial outcome of TBI in children with unilateral frontal lesions. Journal of the International Neuropsychological Society. 2004;10:305–316. doi: 10.1017/S1355617704102129. doi:10.1017/S1355617704102129. [DOI] [PubMed] [Google Scholar]
- Lin JJ, Riley JD, Juranek J, Cramer SC. Vulnerability of the frontal-temporal connections in temporal lobe epilepsy. Epilepsy Research. 2008;82:162–170. doi: 10.1016/j.eplepsyres.2008.07.020. doi:10.1016/j.eplepsyres.2008.07.020. [DOI] [PubMed] [Google Scholar]
- Mangeot S, Armstrong K, Colvin AN, Yeates KO, Taylor HG. Long-term executive function deficits in children with traumatic brain injuries: Assessment using the Behavior Rating Inventory of Executive Function (BRIEF). Child Neuro-psychology. 2002;8:271–284. doi: 10.1076/chin.8.4.271.13503. doi:10.1076/chin.8.4.271.13503. [DOI] [PubMed] [Google Scholar]
- Max JE, Schachar RJ, Levin HS, Ewing-Cobbs L, Chapman SB, Dennis M, Landis J. Predictors of attention-deficit/hyperactivity disorder within 6 months after pediatric traumatic brain injury. Journal of the American Academy of Child & Adolescent Psychiatry. 2005;44:1032–1040. doi: 10.1097/01.chi.0000173293.05817.b1. doi:10.1097/01.chi.0000173293.05817.b1. [DOI] [PubMed] [Google Scholar]
- Mori S, van Zijl PCM. Fiber tracking: Principles and strategies – a technical review. NMR in Biomedicine. 2002;15:468–480. doi: 10.1002/nbm.781. doi:10.1002/nbm.781. [DOI] [PubMed] [Google Scholar]
- Moseley M, Bammer R, Illes J. Diffusion-tensor imaging of cognitive performance. Brain and Cognition. 2002;50:396–413. doi: 10.1016/s0278-2626(02)00524-9. doi:10.1016/S0278-2626(02)00524-9. [DOI] [PubMed] [Google Scholar]
- Ochsner KN, Ray RR, Hughes B, McRae K, Cooper JC, Weber J, Gross JJ. Bottom-up and top-down processes in emotion generation: Common and distinct neural mechanisms. Psychological Science. 2009;20:1322–1331. doi: 10.1111/j.1467-9280.2009.02459.x. doi:10.1111/j.1467-9280.2009.02459.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pierpaoli C, Barnett A, Pajevic S, Chen R, Penix L, Virta A, Basser P. Water diffusion changes in Wallerian degeneration and their dependence on white matter architecture. Neuroimage. 2001;13:1174–1185. doi: 10.1006/nimg.2001.0765. doi:10.1006/nimg.2001.0765. [DOI] [PubMed] [Google Scholar]
- Pierpaoli C, Basser PJ. Toward a quantitative assessment of diffusion anisotropy. Magnetic Resonance in Medicine. 1996;36:893–906. doi: 10.1002/mrm.1910360612. doi:10.1002/mrm.1910360612. [DOI] [PubMed] [Google Scholar]
- Pugliese L, Catani M, Ameis S, Dell'Acqua F, de Schotten MT, Murphy C, Murphy DGM. The anatomy of extended limbic pathways in Asperger syndrome: A preliminary diffusion tensor imaging tractography study. Neuroimage. 2009;47:427–434. doi: 10.1016/j.neuroimage.2009.05.014. doi:10.1016/j.neuroimage.2009.05.014. [DOI] [PubMed] [Google Scholar]
- Rubia K, Smith AB, Woolley J, Nosarti C, Heyman I, Taylor E, Brammer M. Progressive increase of frontostriatal brain activation from childhood to adulthood during event-related tasks of cognitive control. Human Brain Mapping. 2006;27:973–993. doi: 10.1002/hbm.20237. doi:10.1002/hbm.20237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rugg-Gunn FJ, Symms MR, Barker GJ, Greenwood R, Duncan JS. Diffusion imaging shows abnormalities after blunt head trauma when conventional magnetic resonance imaging is normal. Journal of Neurology, Neurosurgery, & Psychiatry. 2001;70:530–533. doi: 10.1136/jnnp.70.4.530. doi:10.1136/jnnp.70.4.530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saatman KE, Duhaime AC, Bullock R, Maas AI, Valadka A, Manley GT. Classification of traumatic brain injury for targeted therapies. Journal of Neurotrauma. 2008;25:719–738. doi: 10.1089/neu.2008.0586. doi:10.1089/neu.2008.0586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz L, Taylor HG, Drotar D, Yeates KO, Wade SL, Stancin T. Long term behavior problems following pediatric traumatic brain injury: Prevalence, predictors, and correlates. Journal of Pediatric Psychology. 2003;28:251–263. doi: 10.1093/jpepsy/jsg013. doi:10.1093/jpepsy/jsg013. [DOI] [PubMed] [Google Scholar]
- Sesma HW, Slomine BS, Ding R, McCarthy ML. Executive functioning in the first year after pediatric traumatic brain injury. Pediatrics. 2008;121:e1686–1695. doi: 10.1542/peds.2007-2461. doi:10.1542/peds.2007-2461. [DOI] [PubMed] [Google Scholar]
- Smith SM, Jenkinson M, Woolrich MW, Beckmann CF, Behrens TE, Johansen-Berg H, Matthews PM. Advances in functional and structural MR image analysis and implementation as FSL. Neuroimage. 2004;23:S208–S219. doi: 10.1016/j.neuroimage.2004.07.051. doi:10.1016/j.neuroimage.2004.07.051. [DOI] [PubMed] [Google Scholar]
- Somerville LH, Casey BJ. Developmental neuro-biology of cognitive control and motivational systems. Current Opinions in Neurobiology. 2010;20:236–241. doi: 10.1016/j.conb.2010.01.006. doi:10.1016/j.conb.2010.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steyerberg EW, Mushkudiani N, Perel P, Butcher I, Lu J, McHugh GS, Maas AIR. Predicting outcome after traumatic brain injury: Development and international validation of prognostic scores based on admission characteristics. Public Library of Science Medicine. 2008;5:e165. doi: 10.1371/journal.pmed.0050165. doi:10.1371/journal.pmed.0050165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tasker RC. Changes in white matter late after severe traumatic brain injury in childhood. Developmental Neuroscience. 2006;28:302–308. doi: 10.1159/000094156. doi:10.1159/000094156. [DOI] [PubMed] [Google Scholar]
- Taylor HG, Yeates KO, Wade SL, Drotar D, Stancin T, Minich N. A prospective study of short- and long-term outcomes after traumatic brain injury in children: Behavior and achievement. Neuropsychology. 2002;16:15–27. doi: 10.1037//0894-4105.16.1.15. doi:10.1037//0894-4105.16.1.15. [DOI] [PubMed] [Google Scholar]
- Teasdale G, Jennett B. Assessment of coma and impaired consciousness: A practical scale. The Lancet. 1974;304:81–84. doi: 10.1016/s0140-6736(74)91639-0. doi:10.1016/S0140-6736(74)91639-0. [DOI] [PubMed] [Google Scholar]
- Vriezen ER, Pigott SE. The relationship between parental report on the BRIEF and performance-based measures of executive function in children with moderate to severe traumatic brain injury. Child Neuropsychology. 2002;8:296–303. doi: 10.1076/chin.8.4.296.13505. doi:10.1076/chin.8.4.296.13505. [DOI] [PubMed] [Google Scholar]
- Wager TD, Davidson ML, Hughes BL, Lindquist MA, Ochsner KN. Prefrontal-subcortical pathways mediating successful emotion regulation. Neuron. 2008;59:1037–1050. doi: 10.1016/j.neuron.2008.09.006. doi:10.1016/j.neuron.2008.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wallis LI, Widjaja E, Wignall EL, Wilkinson ID, Griffiths PD. Misrepresentation of surface rendering of pediatric brain malformations performed following spatial normalization. Acta Radiologica. 2006;47:1094–1099. doi: 10.1080/02841850600979048. doi:10.1080/02841850600979048. [DOI] [PubMed] [Google Scholar]
- Wilde EA, Chu Z, Bigler ED, Hunter JV, Fearing MA, Hanten G, Levin HS. Diffusion tensor imaging in the corpus callosum in children after moderate to severe traumatic brain injury. Journal of Neurotrauma. 2006;23:1412–1426. doi: 10.1089/neu.2006.23.1412. doi:10.1089/neu.2006.23.1412. [DOI] [PubMed] [Google Scholar]
- Wilde EA, Hunter JV, Newsome MR, Scheibel RS, Bigler ED, Johnson JL, Levin HS. Frontal and temporal morphometric findings on MRI in children after moderate to severe traumatic brain injury. Journal of Neurotrauma. 2005;22:333–344. doi: 10.1089/neu.2005.22.333. doi:10.1089/neu.2005.22.333. [DOI] [PubMed] [Google Scholar]
- Wilde EA, Ramos MA, Yallampali R, Bigler ED, McCauley SR, Chu Z, Levin HS. Diffusion tensor imaging of the cingulum bundle in children after traumatic brain injury. Developmental Neuropsychology. 2010;35:333–351. doi: 10.1080/87565641003696940. doi:10.1080/87565641003696940. [DOI] [PMC free article] [PubMed] [Google Scholar]