Abstract
Background
Communication with family members of Intensive Care Unit (ICU) patients is challenging and fraught with dissatisfaction.
Objectives
We hypothesized that family attendance at structured interdisciplinary Family Rounds would enhance communication and facilitate end-of-life planning (when appropriate).
Methods
The study was conducted at the 26-bed medical ICU of a tertiary care, academic, medical center from April through October 2006. Implementation of Family Rounds occurred in July 2006, after which families were invited to attend daily interdisciplinary rounds while the medical team discussed the plan for care. Family members were surveyed at least one month following the ICU stay using the validated “Family Satisfaction in ICU (FS-ICU)” tool prior to and after implementation of Family Rounds.
Results
Of 227 patients enrolled, 187 patients survived and 40 died. Among families of survivors, participation in Family Rounds was associated with higher family satisfaction regarding frequency of communication with physicians (p=0.004) and support during decision making (p=0.005). Participation decreased satisfaction regarding time for decision making (p=0.02). There was no difference in overall satisfaction scores. For families of patients who died, participation in Family Rounds did not significantly change satisfaction.
Conclusions
In the context of this pilot Family Rounds study, certain elements of satisfaction were improved but not overall satisfaction. The findings pointed out that structured interdisciplinary Family Rounds can be viewed as an improvement in some families’ opinions while others feel rushed to make decisions. More work is needed to optimize communication between ICU personnel and patients’ families, their comprehension, and the affects on ICU team workload.
Keywords: critical care, intensive care, communication, end-of-life, palliative care, family research, family satisfaction, family distress, medical rounds
INTRODUCTION
Comprehensive state-of-the-art care of patients in the intensive care unit (ICU) involves not only excellent medical treatment but also optimal communication and interaction with the healthcare team. Family members, who frequently must act as the surrogates for ICU patients, suffer significant distress in the setting of poor communication and interpersonal interactions (1–6). For many patients and their families, this becomes especially important when the transition from anticipation of cure to the realization of non-survivability must be negotiated in the ICU, making the ICU team responsible for providing a quality end-of-life (EOL) experience for the patient and his/her family members (7).
While much attention has been given to the family conference separate from rounds (5, 8–11), communication may also be enhanced through routine incorporation of families into daily interdisciplinary ICU rounds. Studies in pediatric (12–14) and trauma populations (15, 16) have suggested a positive impact from family inclusion in interdisciplinary rounds, and exploration of the related practice of bedside rounds shows the practice to be positively received by patients as well (17, 18). Studies of families’ experiences with EOL in the ICU indicate a need for better communication, as the deficit results in family anxiety and depression (1, 3, 5, 6), increased risk of contradictory information from multiple physicians (19), and potential family mistrust of physicians (5). Families desire more frequent communication with nurses and physicians (6), and access to and comprehension of information often is lacking (3, 20). Failure to comprehend a diagnosis, prognosis, or treatment occurs in 35–50% of family members (21, 22). It is thought that improved comprehension is a base from which overall satisfaction can arise (1), making this deficit in understanding a significant impediment to optimal care. Thus, a “family rounds” approach, with nurses inviting and bringing the family into daily rounds, might facilitate the earliest possible and most regular form of communication for all patients, not just those in whom problems arise, such as the need for EOL discussions. On the other hand, such an approach of hearing the actual medical discussions on rounds could increase fear, confusion, and doubts about care.
We conducted this pilot investigation to explore the effect of consistent, early communication through the addition of a family component to interdisciplinary rounds in the medical ICU, a setting in which there are few previous reports of this type of communication intervention. This intervention will be referred to as “Family Rounds” to focus on this one aspect of interdisciplinary rounds. Constructing this study, we noted the importance of including families of patients who both survive their ICU stay and who die during or shortly after an ICU stay. The needs of the survivors and their families for communication can be neglected due to focus on communication in the EOL setting (23). We hypothesized that implementation of family rounds would enhance communication and facilitate end-of-life planning (when appropriate) between families and the medical team, leading to improved family satisfaction, especially with aspects of communication.
MATERIALS AND METHODS
Study Design
We conducted a before-after study during which family satisfaction in the ICU was assessed prior to implementation of a Family Rounds component as well as after implementation.
Patient Population
Two study investigators (NJ, AD) conducted phone interviews of family members designated as primary contacts for all patients admitted longer than 24 hours to the Vanderbilt University Medical Center medical ICU, a 26-bed unit, prior to and after the implementation of Family Rounds on July 7, 2006. The study period included April 24, 2006 through October 31, 2006. Patients without a primary contact or whose primary contact did not understand English sufficiently to complete the survey were excluded. Family members of patients enrolled prior to implementation of Family Rounds comprised the Baseline group. Family attendance post-implementation of Family Rounds comprised the Family Rounds group. Upon admission to the ICU, patients’ families received a letter describing the study and the phone surveys. For patients discharged from the unit, surveys were completed within 1 month following discharge. For patients who died in the unit, surveys were completed between 3 and 5 months following the death, respecting a grieving period for the families. At the time of the phone call, the purpose of the survey was described again, families were informed that the survey was voluntary and anonymous, and verbal consent was obtained. Only one respondent was interviewed per patient, and no patient included in the baseline group was readmitted during the family rounds period. This study was reviewed by the Vanderbilt IRB and granted expedited review and approval with verbal consent obtained at the time of interview.
Survey Development and Administration
The previously refined and validated Family Satisfaction in the ICU (FS-ICU) survey (24) was used in this study. The survey consisted of two sub-domains: care and decision making, which consisted of 13 and 10 questions, respectively. The Cronbach’s α coefficient for the two sub-scales were .92 and .88, respectively, and the two sub-scales showed good correlation with each other (Spearman’s ρ 0.73, p<.001), supporting their combination into a single scale with a Chronbach’s α coefficient of .94. The survey’s validity was demonstrated by a significant correlation to the previously established Family-Quality of Death and Dying survey. Respondents rated their satisfaction with multiple aspects of the patient’s care in the ICU and the respondent’s experience during that time on a 1–5 scale, with higher values indicating increased satisfaction. In keeping with prior studies, responses were converted to a 0–100 score per question (25). The average of the 13 questions and 10 questions provided the total score for each sub-domain. The average of these two sub-scores provided the total score.
Family Rounds Process
The structure of Family Rounds as a family communication component of daily interdisciplinary rounds was developed through multiple discussions with the physicians and nurses of the ICU, settling on the following format. Family Rounds added to the existing structure of interdisciplinary rounds in the medical ICU, which occurred before regular visiting hours and consisted of: 1) nurse presentation of vital signs and relevant events from the previous 24-hours, 2) intern presentation of 24-hour events to complement information provided by the nurse, 3) upper level residents’ and fellows’ refinement of 24-hour goals and treatment plan, and 4) teaching provided by the attending physician to the treatment team. Two additional steps, which we define as Family Rounds, were added: 5) the attending physician provided a summary for the family using understandable, lay language and 6) the family was offered an opportunity to ask questions of the team. To limit extension of the time of rounds, each patient was allowed up to two family members at the bedside and if questions exceeded a few minutes, the team invited the family to meet with them again after rounds for further discussion. More extended family conferences did not occur for every patient, but the standard medical ICU procedure was to arrange such conferences as needed due to complexity of illness or to facilitate decision making. Families received an explanatory letter and verbal explanation from the nurse upon admission, orienting them to these procedures as well. It was essential that the nurses embraced the concept of family rounds, as they would be the ones helping bring families in and out of the ICU in the morning and also would have the most frequent interactions with families, making them a primary influence to encourage their patients’ families to attend Family Rounds.
Data Entry and Statistical Analysis
For this pilot study, sample size was determined by available resources. Thus, we sought to enroll all eligible patients during the specified period of study. Since our goal for this study was to assess the efficacy of Family Rounds as a source of improved satisfaction via better communication, we focused our analysis on specific items in the FS-ICU that we deemed most relevant (Table 1). These questions had a primary focus on communication with members of the ICU team, family member understanding and decision making, and frequency of contact with the ICU team. Although less specific to this study, the summative scores for decision making and overall satisfaction were evaluated as well, in keeping with prior research (25). We also stratified all analyses according to whether the patient survived to ICU discharge or died in the ICU, because we hypothesized that family members of patients who died would have different interactions with ICU staff than those of patients who survived, and therefore the effect of family rounds on satisfaction may differ according to survival status of the patient.
Table 1.
Family Satisfaction in the ICU (FS-ICU) survey items related to communication
| Item |
|---|
| How often nurses communicated to you about your family member’s condition. |
| How often doctors communicated to you about your family member’s condition. |
| Willingness of ICU staff to answer your questions. |
| How well ICU staff provided you with explanations that you understood. |
| The honesty of information provided to you about your family member’s condition. |
| How well ICU staff informed you what was happening to your family member and why things were being done. |
| The consistency of information provided to you about your family member’s condition. |
| Did you feel included in the decision making process? |
| Did you feel supported during the decision making process? |
| When making decisions, did you have adequate time to have your concerns addressed and questions answered? |
Baseline characteristics are presented using median and interquartile range for continuous variables and proportions for categorical variables. We used chi-squared tests to compare categorical variables between the study groups, and the Wilcoxon-Mann-Whitney two-sample rank-sum test to compare continuous variables, including individual items on the FS-ICU and summary scores. Because responses on individual survey items were strongly skewed (i.e., most respondents rated their experiences “good” or “excellent”), we also reduced each item to a dichotomous variable representing the highest level of satisfaction (e.g., “excellent” or “very supported”) vs. less than the highest level of satisfaction and compared these variables using the chi-squared test. To explore potential interactions between the effect of family rounds and patient survival in the ICU, we included interaction terms in proportional odds logistic regression models with individual FS-ICU items as the dependent variables. In keeping with authoritative recommendations on the topic (26, 27), no adjustments were made to our results to account for multiple comparisons. Though this may increase the likelihood of a type I error, our approach of not making such adjustments avoids an unnecessary inflation of type II errors. STATA version 10.0 (StataCorp, College Station, TX, USA), and SPSS version 15 (SPSS Inc., Chicago, IL, USA) were used for data analysis, and a two-sided 5% significance level was used for all statistical inferences.
RESULTS
Demographics and Clinical Characteristics
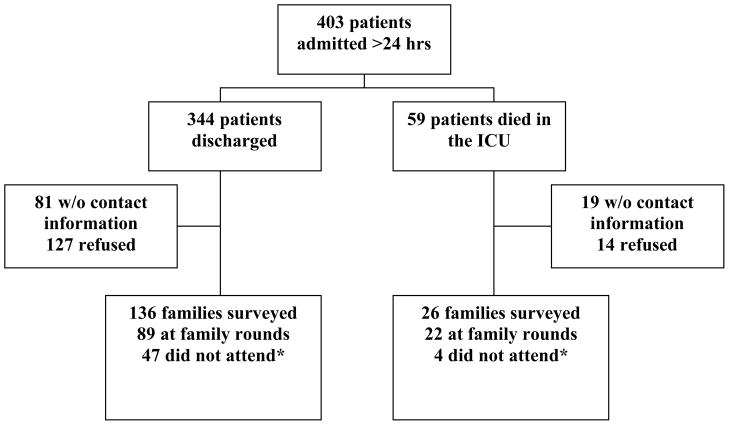
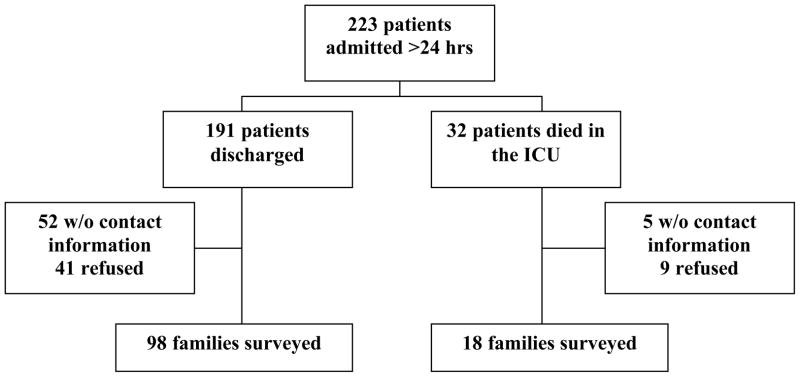
Among 402 families of survivors for whom contact information was available, 234 (58%) respondents completed the survey; among 67 families of deceased patients for whom contact information was available, 44 (66%) respondents completed the survey. After eliminating those who did not attend any Family Rounds despite this intervention’s availability at the time of their family member’s ICU admission, 227 survey interviews of family members remained to be analyzed. Of these families, 187 were of patients discharged from the ICU and 40 were of patients who died in the ICU. The breakdown of those interviews is seen in Figures 1 and 2. For patients who survived and those who died in the ICU, survey respondents during the baseline phase were similar to respondents who attended family rounds, without significant differences in age, race, or relationship to the patient (Table 2). Patients enrolled during the two study periods were similar except that patients who survived during the family rounds phase had longer stays in the ICU than patients who survived prior to implementation of Family Founds.
Figure 1. Flowchart of family member interviews: Baseline Phase.
This flowchart demonstrates the numbers of surveys conducted during the baseline phase, with detailed listing of whether or not the family was associated with an ICU patient who had been discharged alive or dead (designated as end-of-life, EOL).
Figure 2. Flowchart of family member interviews: Intervention Phase.
This flowchart demonstrates the numbers of surveys conducted after incipience of Family Rounds, with detailed listing of whether or not the family was associated with an ICU patient who had been discharged alive or dead (designated as end-of-life, EOL) and attendance of family rounds.
Table 2.
Demographics and Clinical Characteristics
| Characteristics | Patient Survived
|
Patient Died
|
||||
|---|---|---|---|---|---|---|
| Baseline (n=98) | Family Rounds (n=89) | p value | Baseline (n=18) | Family Rounds (n=22) | p value | |
| Patient | ||||||
| Age, yrs* | 57 [46–66] | 55 [37–66] | 0.45 | 62 [51–68] | 56 [49–71] | 0.94 |
| Female, % | 49 | 42 | 0.31 | 56 | 50 | 0.73 |
| Race, % | 0.61 | 0.97 | ||||
| White | 79 | 85 | 82 | 82 | ||
| Black | 12 | 10 | 18 | 18 | ||
| Other | 9 | 5 | 0 | 0 | ||
| Admission Diagnosis, % | 0.11 | 0.36 | ||||
| Cardiovascular | 11 | 8 | 17 | 9 | ||
| Respiratory | 21 | 33 | 50 | 27 | ||
| Neurological | 11 | 16 | 6 | 9 | ||
| Sepsis | 14 | 10 | 0 | 18 | ||
| Gastroenterological | 12 | 18 | 6 | 9 | ||
| Other | 31 | 15 | 21 | 28 | ||
| ICU length of stay, days* | 3 [2–5] | 4 [3–8] | 0.001 | 4 [2–6] | 4 [3–9] | 0.46 |
| Full code status, % | 97 | 93 | 0.33 | 65 | 76 | 0.23 |
| Respondent | ||||||
| Age, % | 0.41 | 0.23 | ||||
| ≥80 yrs | 0 | 1 | 0 | 4 | ||
| 60–79 yrs | 30 | 21 | 47 | 18 | ||
| 40–59 yrs | 53 | 57 | 35 | 55 | ||
| 20–39 yrs | 16 | 20 | 18 | 23 | ||
| <20 yrs | 1 | 1 | ||||
| Female, % | 69 | 80 | 0.10 | 61 | 77 | 0.27 |
| Race, % | 0.56 | 0.97 | ||||
| White | 79 | 87 | 82 | 82 | ||
| Black | 13 | 10 | 18 | 18 | ||
| Other | 8 | 3 | ||||
| Relationship to pt, % | 0.66 | 0.33 | ||||
| Spouse/Partner (1,2) | 49 | 49 | 72 | 50 | ||
| Child (3) | 28 | 23 | 11 | 36 | ||
| Parent (4) | 11 | 17 | 6 | 5 | ||
| Other (5–9) | 12 | 11 | 11 | 9 | ||
Median [interquartile range]
Follow-Up Family Evaluations: Discharged Patients’ Families
When families of discharged patients were asked to rate “How often doctors communicated to you about your family member’s condition,” there was a significant improvement (p=.004) in the number of families who were able to rate this central aspect of communication as “excellent” after the implementation of Family Rounds. Families also were asked about support received via the question: “Did you feel supported during the decision making process?” There was a significant increase (p=.005) in families reporting “very supported,” the top value on the Likert scale, after families had the opportunity to attend Family Rounds.. In contrast, the percentage of family members who responded that they had “more than enough time to have concerns addressed and questions answered” during decision making declined with Family Rounds (p = 0.02). When all potential responses to this item were compared pre- and post-Family Rounds, there was no significant difference between groups (p = 0.19) according to the Wilcoxon rank-sum test. All other items were rated similarly prior to and after implementation of Family Rounds.
Follow-Up Family Evaluations: Deceased Patients’ Families
Among families of patients who died in the ICU, none of the FS-ICU items pertaining to communication were rated significantly better by respondents who participated in Family Rounds (Table 3). There was a trend of more families of deceased patients reporting the highest level of satisfaction regarding “How often nurses communicated to you about your family member’s condition” in the Family Rounds group (p = 0.11). Similarly, the number of family members of deceased who reported the highest level of satisfaction regarding “willingness of ICU staff to answer your questions” increased after implementation of Family Rounds (p = 0.18).
Table 3.
Effect of family rounds on family satisfaction
| Outcome | Patient Survived
|
Patient Died
|
||||
|---|---|---|---|---|---|---|
| Historical (n=98) | Family Rounds (n=89) | p value | Historical (n=18) | Family Rounds (n=22) | p value | |
| Individual Items, % excellent* | ||||||
| Frequency of RN communication | 64 | 57 | 0.30 | 33 | 59 | 0.11 |
| Frequency of MD communication | 38 | 60 | 0.004 | 50 | 43 | 0.66 |
| Willingness to answer questions | 55 | 59 | 0.58 | 33 | 55 | 0.18 |
| Understandable explanations | 54 | 54 | 0.98 | 39 | 41 | 0.90 |
| Honesty of information | 61 | 58 | 0.74 | 53 | 48 | 0.74 |
| Informative regarding treatment | 56 | 56 | 0.95 | 39 | 52 | 0.40 |
| Consistency of information | 51 | 53 | 0.81 | 33 | 55 | 0.18 |
| Included in decision making | 66 | 76 | 0.12 | 77 | 82 | 0.71 |
| Supported in decision making | 49 | 69 | 0.005 | 61 | 73 | 0.44 |
| Adequate time for questions | 40 | 23 | 0.02 | 39 | 41 | 0.90 |
| Summary Scores, median [IQR] | ||||||
| Decision Making subscore | 83 [65–93] | 85 [74–93] | 0.67 | 75 [63–88] | 78 [73–90] | 0.18 |
| Total Survey score | 85 [70–95] | 88 [75–95] | 0.65 | 74 [62–92] | 82 [72–94] | 0.26 |
”% excellent” indicates the proportion of respondents who gave the survey item the highest rating, i.e., expressed the highest level of satisfaction.
Overall Measures of Satisfaction and Interactions
Neither the Decision making subscore nor the total FS-ICU score was significantly different among respondents who attended Family Rounds compared with respondents prior to implementation of Family Rounds (Table 3). Additionally, there were no significant interactions noted between the effect of Family Rounds on family satisfaction and patient survival in the ICU.
DISCUSSION
In this pilot before-after study, a Family Rounds component during interdisciplinary rounds in the medical ICU did not impact the global measure of family satisfaction and, in fact, resulted in significant improvements in some aspects of family satisfaction related to communication. Specifically, families of discharged patients reported an increased frequency of communication. Additionally, while conceived as efficient use of time for both families and the medical team, the results also showed that more families reported a perception of inadequate time for decision making after implementation of Family Rounds.
Past research that has evaluated patient perspectives of similar interventions such as bedside case presentations that brought the patient and family into the midst of rounds. The majority of patients preferred such bedside presentations (17, 18). There have been limited studies of family inclusion in ICU rounds (15, 16), but those that exist demonstrated that families appreciated the scheduled opportunity to receive information and answers to questions. Past studies also have revealed a link between family satisfaction and psychological health (1, 3, 5, 6). Hospitalization of a loved one in the ICU is a very stressful event for family members, with nearly 3 out of every 4 family members struggling with anxiety and 1 in 3 showing signs of depression (6, 28). A proactive approach to bereavement and implementation of a proactive communication strategy has been shown to lead to decreased PTSD, anxiety, and depressive symptoms (5). In our Family Rounds pilot study, this communication began from admission, congruent with the reported increased satisfaction with communication when prognostic information is provided within a shorter time interval (29). By addressing some of these key components of family satisfaction, Family Rounds has the potential to minimize the psychological distress in the stressful ICU environment (especially if those who feel rushed by such an approach are encouraged to have family conferences later in the day to allow more time for decision making). Simultaneously, subsequent study of family inclusion should consider the potential for families to feel intimidated or overwhelmed in the setting of daily rounds and should explore family comfort in that setting and any potential impact on families’ levels of stress and anxiety. This important balance, which is developed more in the following paragraph, must be explored in future research.
This pilot highlights that family satisfaction with communication may hinge on receipt of adequate knowledge to improve their comprehension and aid in surrogate decision making (1, 5, 20, 21, 25, 28, 30, 31). Reports of inadequate comprehension range from 30% to 50% of families (21, 22, 28), which we felt necessitated that the structure of Family Rounds included having the physician provide the families with a 1–2 minute summary in lay language for maximal benefit of Family Rounds. Family Rounds initiated brief, structured, and consistent communication within the first 24 hours of admission, providing families a realistic, real-time format and frequently updated picture of their loved one’s condition (13, 15). These rounds also helped prepare families for more in-depth discussions that were sometimes necessary at a later time point in the day to meet their reported need for more time in decision making than might be present on rounds. However, the effect of Family Rounds on knowledge and comprehension was not studied in this investigation beyond families’ summary statements about access to and satisfaction with information. As this is a central aspect of good communication, it warrants more extensive attention in future studies.
Studies of families of patients with EOL experiences have documented a need to provide information early and often (7, 22), and inadequacies of information and communication may impede removal of support, leading to drawn out deaths and longer patient stays (32). Interdisciplinary inclusion of the ICU medical care team during Family Rounds may reduce communication obstacles by fostering more cohesive care with better integration of palliative care (33), yet the pace of these rounds and the inclusion of medical terminology amid the discussions between doctors and nurses could also increase communication problems. This must be tested. Our study included only English-speaking patients, necessitating further study of the application of Family Rounds with non-English speaking families as alterations in translation during interpreted interactions can negatively impact communication, complicating both the transmission of knowledge and emotional support (34). In addition to examining the success of transmission of content in these conversations, studies of patient-physician relationships have shown that styles of interpersonal communication influence satisfaction (35, 36). Studies in the ICU also have identified a need to improve the quality of communication (9, 10). Though not examined in our study, future research should evaluate influence of the style and nature of the communication itself on family satisfaction.
From the perspective of the ICU nurses, one of the most significant obstacles to providing EOL care is multiple physicians with discordant opinions about the plan of care as well as multiple family members contacting the staff instead of communicating with one designated team member (19). From the perspective of the ICU care team, attention to communication and palliative care can lead to improved nurse-assessed quality of death in the ICU (37). In the case of EOL care, nurses experienced distress and decreased satisfaction with quality of care when they perceived care to be overly aggressive given the patient’s expected prognosis (38, 39), and the Critical Care Medicine Task Force 2004–2005 identified poor communication as a major source of stress for staff (40). Though not explored formally in this study, Family Rounds may be a forum to address these issues, providing components of suggested interventions (41), including a systemic framework to support palliative care integration and attitudinal change regarding communication given the increased, regular interaction with families.
Why did this study not show global improvements in family members’ satisfaction? There are important considerations that address this intriguing question. As seen in other studies using the FS-ICU (4, 25, 31, 42), family members in the baseline group reported high satisfaction in general, thus improvements in satisfaction with Family Rounds may have been difficult to detect because of these high baseline ratings causing a possible ceiling effect. Combined with a limited number of FS-ICU questions targeting aspects likely to be affected by Family Rounds, our study likely had limited sensitivity to detect a difference in the pre vs. post periods. Additionally, the study size—determined by restricted resources and time available to conduct this pilot study—was small, especially regarding patients with EOL experiences, and may have impaired the ability to observe overall changes in satisfaction. There was not enough power to assess for differences between family members of living vs. deceased patients. The refusal rate of families in study participation warrants exploration. High baseline levels of satisfaction may point to a selection bias, since family members without contact information or who refused to participate likely are different than those who responded to the survey, and the latter may represent a population most likely to attend and benefit from Family Rounds, even though demographically there were not significant differences between attendees and non-attendees. Since Vanderbilt serves a diverse population, other factors probably influenced ability and willingness to attend Family Rounds, such as socioeconomic status, availability to be at the hospital at the time of rounds, geographic factors (many patients and their families live hours away from the hospital), and comfort and experience with the medical system. As the rate of non-attendance is a limitation to this study, these factors should be explored. Attention also should be given to the level of nurse engagement in Family Rounds and nurse-perceived barriers to successful Family Rounds since the level of family participation may depend on how well families are informed about and encouraged to attend Family Rounds by their bedside nurse with whom they interact during the day.
Other limitations of this study should be discussed. As this was a single-center study, future multicenter work is needed to assess the impact of Family Rounds in other settings. Though no other major changes were noted in our routine ICU practices during the course of the study, it is possible that improvements in satisfaction were confounded by unmeasured factors such as time spent in further communications during the rest of the day. Particular attention in future work should be given to the time nurses and physicians spend communicating medical updates to families as well as the effect on nursing work flow and productivity during the day. Regarding their reactions to Family Rounds, the perspectives of different ICU team members have been shown to differ (38, 43), necessitating exploration of the effects on all members of the team.
CONCLUSIONS
ICU patients’ and families’ satisfaction and comprehension of the course of critical illness increasingly are recognized as relevant measures of outcome and benchmarks of high quality ICU care. Family members participate in decision making, representing the voice of the patient, and suffer significant distress when inadequately educated and supported during a loved one’s ICU care. In this pilot investigation, including a family component in daily interdisciplinary rounds appeared to be a potential means by which to improve some elements of satisfaction, including support during decision making and frequency of communication with physicians. Yet, for an important minority it was perceived that this process tended to provide inadequate time for decision making. Global satisfaction was not changed by the implementation of family rounds in this study, and concern was raised about a potential negative perception regarding having adequate time for decision-making. There remains a need to explore further the impact of Family Rounds on family members’ psychological outcomes, family rounds’ ability to affect family members’ comprehension and knowledge, the use and impact of differing physician communication styles and approaches, factors influencing family attendance, and the effect on an ICU team’s workload.
Key Points.
Family members of ICU patients suffer significant distress and anxiety when inadequately informed and poorly supported by the ICU team.
Incorporating family members into rounds has the potential to improve communication and family satisfaction, yet this pilot study showed improvements in only certain domains among families of survivors and for some it made them feel rushed in decision making.
Optimal communication with and support of families is becoming an important outcome measure of high quality ICU care.
Based on this pilot study, including a family component, Family Rounds, in daily interdisciplinary rounds is a potential mechanism by which to improve some elements of satisfaction including decision making, frequency of communication with physicians, and coordination of care.
Acknowledgments
During the course of this research, Dr. Girard was supported in part by the National Institutes of Health (AG034257), the Hartford Geriatrics Health Outcomes Research Scholars Award Program, the Vanderbilt Physician Scientist Development Program, and the Veterans Affairs Tennessee Valley Geriatrics Research, Education and Clinical Center. Dr. Ely was supported in part by the National Institutes of Health (AG027472) and the Veterans Affairs Tennessee Valley Geriatrics Research, Education and Clinical Center.
We thank the director of the Medical Intensive Care Unit, Art Wheeler, MD, and the nurse manager of the Medical Intensive Care Unit, Julie Foss, MSN, RN, for their support in the implementation of this research. Additionally, we thank Andrea Dugas, MD for her assistance in conducting phone surveys of family members.
ABBREVIATIONS
- EOL
End of Life
- FS-ICU
Family Satisfaction in the ICU
- ICU
Intensive Care Unit
Footnotes
The authors have no conflicts of interest.
Authors’ Contributions:
NJ conceived of the study, participated in study design, study implementation, survey conduction, and database creation, and drafted the manuscript. TG participated in data analysis and helped draft the manuscript. JM involved in conceiving the study and participated in study design. WEE involved in conceiving the study and participated in study design, study implementation, and helped draft the manuscript. All authors have reviewed the final manuscript.
References
- 1.Azoulay E, Pochard F, Chevret S, et al. Impact of a Family Information Leaflet on Effectiveness of Information Provided to Family Members of Intensive Care Unit Patients. American Journal of Respiratory and Critical Care Medicine. 2002;165:438–442. doi: 10.1164/ajrccm.165.4.200108-006oc. [DOI] [PubMed] [Google Scholar]
- 2.Azoulay E, Pochard F, Chevret S, et al. Meeting the needs of intensive care unit patient families: a multicenter study. American Journal of Respiratory and Critical Care Medicine. 2001;163(1):135–139. doi: 10.1164/ajrccm.163.1.2005117. [DOI] [PubMed] [Google Scholar]
- 3.Azoulay E, Sprung cL. Family-Physician Interactions in the Intensive Care Unit. Critical Care Medicine. 2004;32(11):2323–2328. doi: 10.1097/01.ccm.0000145950.57614.04. [DOI] [PubMed] [Google Scholar]
- 4.Heyland D, Cook D, Rocker G, et al. Decision-making in the ICU: perspectives of the substitute decision-maker. Intensive Care Medicine. 2003;29(1):75–82. doi: 10.1007/s00134-002-1569-y. [DOI] [PubMed] [Google Scholar]
- 5.Lautrette A, Darmon M, Megarbane B, et al. A communication strategy and brochure for relatives of patients dying in the ICU. New England Journal of Medicine. 2007;356(5):469–478. doi: 10.1056/NEJMoa063446. [DOI] [PubMed] [Google Scholar]
- 6.Pochard F, Darmon M, Fassier T, et al. Symptoms of anxiety and depression in family members of intensive care unit patients before discharge or death. A prospective multicenter study. Journal of Critical Care. 2005;20:90–96. doi: 10.1016/j.jcrc.2004.11.004. [DOI] [PubMed] [Google Scholar]
- 7.Mosenthal AC. Palliative care in the surgical ICU. Surgical Clinics of North America. 2005;85:303–313. doi: 10.1016/j.suc.2005.01.001. [DOI] [PubMed] [Google Scholar]
- 8.Azoulay E. The end-of-life family conference: communication empowers. American Journal of Respiratory and Critical Care Medicine. 2005;171(8):803–804. doi: 10.1164/rccm.2501004. [DOI] [PubMed] [Google Scholar]
- 9.Curtis JR, Engelberg RA, Wenrich MD, et al. Studying Communication about End-of-Life Care During the ICU Family Conference: Developing a Framework. Journal of Critical Care. 2002;17(3):147–160. doi: 10.1053/jcrc.2002.35929. [DOI] [PubMed] [Google Scholar]
- 10.Curtis JR, Engelberg RA, Wenrich MD, et al. Missed Opportunities during Family Conferences about End-of-Life Care in the Intensive Care Unit. American Journal of Respiratory and Critical Care Medicine. 2005;171:844–849. doi: 10.1164/rccm.200409-1267OC. [DOI] [PubMed] [Google Scholar]
- 11.White DB, Engelberg RA, Wenrich MD, Lo B, Curtis JR. Prognostication during physician-family discussions about limiting life support in intensive care units. Critical Care Medicine. 2007;2007(35):442–448. doi: 10.1097/01.CCM.0000254723.28270.14. [DOI] [PubMed] [Google Scholar]
- 12.Latta L, Dick R, Parry C, Tamura G. Parental responses to involvement in rounds on a pediatric inpatient unit at a teaching hospital: a qualitative study. Academic Medicine. 2008;83(3):292–297. doi: 10.1097/ACM.0b013e3181637e21. [DOI] [PubMed] [Google Scholar]
- 13.Lewis C, Knopf D, Chastain-Lorber K, et al. Patient, parent, and physician perspectives on pediatric oncology rounds. Journal of Pediatrics. 1988;112(3):378–384. doi: 10.1016/s0022-3476(88)80316-0. [DOI] [PubMed] [Google Scholar]
- 14.Muething SE, Kotagal UR, Schoettker PJ, Gonzalez del Rey J, DeWitt TG. Family-centered bedside rounds: a new approach to patient care and teaching. Pediatrics. 2007;119:829–832. doi: 10.1542/peds.2006-2528. [DOI] [PubMed] [Google Scholar]
- 15.Mangram A, Mccauley T, Villarreal D, et al. Families’ perception of the value of timed daily “family rounds” in a trauma ICU. American Surgeon. 2005;71(10):886–891. [PubMed] [Google Scholar]
- 16.Schiller WR, Anderson BF. Family as a member of the trauma rounds: a strategy for maximized communication. Journal of Trauma Nursing. 2003;10(4):93–99. doi: 10.1097/00043860-200310040-00001. [DOI] [PubMed] [Google Scholar]
- 17.Lehmann LL, Brancati FL, Chen M-C, Roter D, Dobs AS. The effect of bedside case presentations on patients’ perceptions of their medical care. New England Journal of Medicine. 1997;336(16):1150–1155. doi: 10.1056/NEJM199704173361606. [DOI] [PubMed] [Google Scholar]
- 18.Wang-Cheng R, Barnsas G, Sigmann P, Riendl P, Young M. Bedside case presentations: why patients like them but learner’s don’t. Journal of General Internal Medicine. 1989;4(4):284–287. doi: 10.1007/BF02597397. [DOI] [PubMed] [Google Scholar]
- 19.Beckstrand RL, Kirchhoff KT. Providing end-of-life care to patients: critical care nurses’ perceived obstacles and supportive behaviors. American Journal of Critical Care. 2005;14(5):395–403. [PubMed] [Google Scholar]
- 20.Azoulay E, Pochard F. Communication with family members of patients dying in the intensive care unit. Current Opinions in Critical Care. 2003;9:545–550. doi: 10.1097/00075198-200312000-00014. [DOI] [PubMed] [Google Scholar]
- 21.Azoulay E, Chevret S, Leleu G, et al. Half the families of intensive care unit patients experience inadequate communication with physicians. Critical Care Medicine. 2000;28(8):3116–3117. doi: 10.1097/00003246-200008000-00061. [DOI] [PubMed] [Google Scholar]
- 22.Azoulay E, Pochard F, Chevret S, Arich C, et al. Family paricipation in care to the critically ill: opinions of families and staff. Intensive Care Medicine. 2003;29:1498–1504. doi: 10.1007/s00134-003-1904-y. [DOI] [PubMed] [Google Scholar]
- 23.Curtis JR, White DB. Practical Guidelines for Evidence-Based ICU Family Conferences. Chest. 2008;134:835–843. doi: 10.1378/chest.08-0235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wall RJ, Engelberg RA, Downey L, Heyland D, Curtis JR. Refinement, scoring, and validation of the Family Satisfaction in the ICU (FS-ICU) survey. Critical Care Medicine. 2007;35(1):271–279. doi: 10.1097/01.CCM.0000251122.15053.50. [DOI] [PubMed] [Google Scholar]
- 25.Heyland D, Rocker G, Dodeck P, et al. Family satisfaction with care in the intensive care unit: results of a multiple center study. Critical Care Medicine. 2002;30(7):1413–1418. doi: 10.1097/00003246-200207000-00002. [DOI] [PubMed] [Google Scholar]
- 26.Perneger T. What’s wrong with Bonferroni adjustments. BMJ. 1998;316(7139):1236–1238. doi: 10.1136/bmj.316.7139.1236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rothman K. No adjustments are needed for multiple comparisons. Epidemiology. 1990;1(1):43–46. [PubMed] [Google Scholar]
- 28.Azoulay E, Pochard F, Chevret S, et al. Half the family members of intensive care unit patients do not want to share in the decision-making process: a study in 78 French intensive care units. Critical Care Medicine. 2004;32(9):1832–1838. doi: 10.1097/01.ccm.0000139693.88931.59. [DOI] [PubMed] [Google Scholar]
- 29.LeClaire M, Oakes J, Weinert C. Communication of prognostic information for critically ill patients. Chest. 2005;128(3):1728–1735. doi: 10.1378/chest.128.3.1728. [DOI] [PubMed] [Google Scholar]
- 30.Cohen S, Sprung cL, Sjokvist P, et al. Communication in end-of-life decisions in European intensive care units. Intensive Care Medicine. 2005;31:1215–1221. doi: 10.1007/s00134-005-2742-x. [DOI] [PubMed] [Google Scholar]
- 31.Heyland D, Rocker G, O’Callaghan C, Dodeck P, Cook D. Dying in the ICU: perspectives of family members. Chest. 2003;124(1):392–397. doi: 10.1378/chest.124.1.392. [DOI] [PubMed] [Google Scholar]
- 32.Gerstel E, Engelberg RA, Koepsell T, Curtis JR. Duration of Withdrawal of Life Support in the Intesive Care Unit and Association with Family Satisfaction. American Journal of Respiratory and Critical Care Medicine. 2008;178:798–804. doi: 10.1164/rccm.200711-1617OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Curtis JR. Caring for patients with critical illness and their families: the value of an integrated team. Respiratory Care. 2008;53(4):480–7. [PubMed] [Google Scholar]
- 34.Pham K, Thornton J, Engelberg RA, Jackson J, Curtis JR. Alterations during medical interpretation of ICU family conference that interfere with or enhance communication. Chest. 2008;134(1):106–116. doi: 10.1378/chest.07-2852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cooper-Patrick L, Gallo JJ, Gonzales JJ, et al. Race, gender, and partnership in the patient-physician relationship. JAMA. 1999;282(6):583–589. doi: 10.1001/jama.282.6.583. [DOI] [PubMed] [Google Scholar]
- 36.Napoles AMN, Gregorich SE, Santoyo-Olsson J, O’Brien H, Stewart AL. Interpersonal processes of care and patient satisfaction: do associations differ by race, ethnicity, and language? Health Services Research. 2009;44(4):1326–1344. doi: 10.1111/j.1475-6773.2009.00965.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Curtis JR, Treecy PD, Nielsen EL, et al. Integrating palliative and critical care: evaluation of a quality-improvement intervention. American Journal of Respiratory and Critical Care Medicine. 2008;178:269–275. doi: 10.1164/rccm.200802-272OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hamric AB, Blackhall LJ. Nurse-physician perspectives on the care of dying patients in intensive care units: Collaboration, moral distress, and ethical climate. Critical Care Medicine. 2007;35(2):422–429. doi: 10.1097/01.CCM.0000254722.50608.2D. [DOI] [PubMed] [Google Scholar]
- 39.Ho KM. The involvement of intensive care nurses in end-of-life decisions: a nationwide survey. Intensive Care Medicine. 2005;31:668–673. doi: 10.1007/s00134-005-2613-5. [DOI] [PubMed] [Google Scholar]
- 40.Davidson JE, Powers K, Hedayat KM, et al. Clinical practice guidelines for support of the family in the patient-centered intensive care unit: American College of Crticial Care Medicine taskforce. Critical Care Medicine. 2007;35(2):605–622. doi: 10.1097/01.CCM.0000254067.14607.EB. [DOI] [PubMed] [Google Scholar]
- 41.Treece PD, Engelberg RA, Shannon SE, et al. Integrating palliative and critical care: description of an intervention. Critical Care Medicine. 2008;34(11 Suppl):2380–7. doi: 10.1097/01.CCM.0000237045.12925.09. [DOI] [PubMed] [Google Scholar]
- 42.Gries CJ, Curtis JR, Wall RJ, Engelberg RA. Family member satisfaction with end-of-life decision making in the ICU. Chest. 2008;133:704–712. doi: 10.1378/chest.07-1773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Levy CR, Ely EW, Payne K, et al. Quality of Death and Dying in Two Medical ICUs: Perceptions of Family and Clinicians. Chest. 2005;127(5):1775–1783. doi: 10.1378/chest.127.5.1775. [DOI] [PubMed] [Google Scholar]