Abstract
♦ Background: Pre-dialysis education can guide the choice of the dialysis modality best tailored to meet the needs and preferences of individual patients with chronic kidney disease.
♦ Methods: In a retrospective single-center cohort study, we evaluated the impact of a pre-dialysis education program on the incidence rates of patients using hemodialysis (HD) and peritoneal dialysis (PD) in our unit. The frequency distribution of dialysis modalities between people attending our education program and people not attending the program (control group) was analyzed for the 4-year period 2004 - 2008.
♦ Results: From among all the incident chronic kidney disease 5D patients presenting during the 4-year period, we analyzed 227 who started dialysis either with an arteriovenous fistula or a PD catheter. In that cohort, 70 patients (30.8%) took part in the education program, and 157 (69.2%) did not receive structured pre-dialysis counseling. In the group receiving education, 38 patients (54.3%) started with PD, and 32 (45.7%), with HD. In the standard-care group not receiving education, 44 patients (28%) started with PD, and 113 (72%), with HD (p < 0.001).
♦ Conclusions: Our multidisciplinary pre-dialysis program had a significant impact on the frequency distribution of dialysis modalities, increasing the proportion of patients initiating dialysis with PD.
Key words: Dialysis modalities, integrated care concept, pre-dialysis education
The prevalence of end-stage renal disease (ESRD) is steadily increasing worldwide, with annual dialysis growth rates of about 6% - 8% (1). In the United States, as of 31 December 2007, in-center hemodialysis (HD) was being used by more than 90% of ESRD patients as renal replacement therapy (RRT), and peritoneal dialysis (PD), by only 7.2% (1). There is broad consensus that PD is an underutilized method, and yet its benefits, especially in the early phases of treatment, have led to the integrated care concept of starting with PD first (2-4). Besides the structural barriers, the financial reimbursement issues, and the negative attitudes of some nephrologists, a lack of patient awareness is another prominent reason for the low use of home-based RRTs such as PD (5,6).
To date, several studies have shown that pre-dialysis education for chronic kidney disease (CKD) patients might help to increase the proportion of patients using self-care dialysis (6-9). In contrast, a recently published registry study did not show that patients with early awareness of the method (10) were more likely to select PD. A pre-dialysis education program gives patients the opportunity to choose the RRT most suitable to their needs and fosters timely referral to dialysis, thus preventing urgent dialysis, which is associated with high mortality (11-13).
In the present study, we retrospectively evaluated the impact of the multidisciplinary pre-dialysis INDIAL (“Information on Dialysis”) education program on the choice of dialysis modality (HD or PD) at our center over a 4-year period. We compared annual incidence rates for the dialysis modalities of INDIAL participants with the modalities of a standard-care patient group (controls).
Methods
Patients
Patients with CKD attending the nephrology outpatient clinic at the Medical University of Graz who had an estimated glomerular filtration rate of 15 mL/min/1.73 m2 or less and an anticipated progression to CKD5D within the following year were offered the INDIAL pre-dialysis education program. Although current guidelines suggest starting pre-dialysis education at an estimated glomerular filtration rate of 30 mL/min or less (14), our threshold was pragmatically chosen given that the large number of CKD patients with an estimated glomerular filtration rate of 30 mL/min or less in our unit would have exceeded the capacity of the program.
The impact of pre-dialysis education was retrospectively evaluated for the 4-year period 2004 - 2008. During that time, we compared the annual incidence rates of PD and HD for patients receiving pre-dialysis education with rates for the standard-care group. Incidence rates were defined as the number of new patients starting with either HD or PD in a given year. The first-ever start with the treatment modality was used for the analysis. The INDIAL participants and the standard-care patients both started their RRT on an inpatient basis, because that was the facility protocol in our unit at the time the patients were enrolled. Patients in the standard-care group did not receive structured education, and they served as controls. In both groups, patients starting dialysis with a central venous catheter (CVC) were excluded, thus eliminating late referrals and emergency starts from the analysis.
Indial Multidisciplinary Pre-dialysis Education Program
In November 2003, the INDIAL structured pre-dialysis education program was implemented in the clinical division of Nephrology of the Medical University of Graz. The program was created by the nurses and nephrologists of the unit to improve awareness among patients of ESRD and its treatment options. This tailor-made and commercially unavailable program has since then become an essential component of our integrative care approach for CKD patients at our center.
On 2 consecutive days, groups of patients (maximum 6) with CKD5 and their relatives receive information concerning the basic pathophysiologic principles of CKD and RRTs including HD, PD, and kidney transplantation. For technical—and more importantly, regional reimbursement—reasons, home HD is infrequently used in Austria; thus, we cannot offer it and do not present it in our program as an option for RRT. The interactive INDIAL program is presented by a multidisciplinary team, including nurses, dieticians, and nephrologists. In a 2-hour session on the first day, patients are given basic information about medical, dietary, and lifestyle issues. The 2-hour session on the second day features practical demonstrations of HD and PD.
Statistical Analyses
Differences between the study groups were tested using the Mann-Whitney U-test. Differences in the relative frequencies between the groups were tested using the Pearson chi-square test. A logistic regression model was used to correct for the effect of age on the choice of initial therapy. The odds ratio and its confidence interval (CI) constitute the effect measure used for the logistic regression. Values of p less than 0.05 were considered statistically significant. The R 2.14.0 (http://www.r-project.org) and SPSS 19 (http://www.spss.com) statistical software applications were used for the analysis.
Results
Study Group, Control Group, and Patient Characteristics
During 2004 - 2008, 460 incident CKD5D patients (38.6% women) were treated in our unit. Of those 460 patients, 296 (36% women), together with 141 relatives (72% women), took part in the INDIAL program, and 116 (35% women) had to start dialysis within 1 year after attending the program. In parallel, a standard-care group of 344 CKD5D patients (40.1% women) did not receive structured pre-dialysis counseling. The patients who received education were significantly younger than those in the standard-care group (p = 0.007), but the groups did not differ with respect to sex or causes of CKD5D.
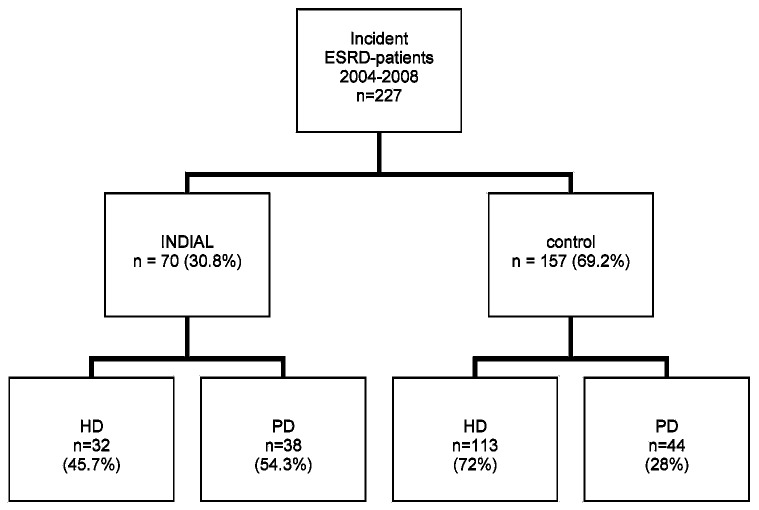
Subjects starting dialysis with a CVC were excluded from the overall group of 460 incident CKD5D patients, leaving 70 patients who received pre-dialysis education and 157 standard-care patients for the ultimate analysis (Figure 1). Table 1 shows the characteristics of the study groups. Elimination of all patients with a CVC minimized the bias of late referral and emergency starts. In the INDIAL group, 38 patients (54.3%) started with PD, and 32 (45.7%), with HD. In the control group, who received no formal pre-dialysis education, 44 patients (28%) started with PD, and 113 (72%), with HD (p < 0.001). As a consequence, the odds of starting with PD were 1.19 in the INDIAL group and 0.73 in the control group. Hence, the odds ratio of INDIAL with respect to standard treatment was 3.05 (95% CI: 1.70 to 4.58).
Figure 1.
— Flowchart of incident end-stage renal disease (ESRD) patients with chronic kidney disease stage 5 on dialysis during 2004 - 2008, after exclusion of patients starting dialysis with a central venous catheter. INDIAL = Information on Dialysis program; HD = hemodialysis; PD = peritoneal dialysis.
TABLE 1.
Characteristics of Incident Patients with Chronic Kidney Disease Stage 5 Starting Dialysis During 2004 - 2008a
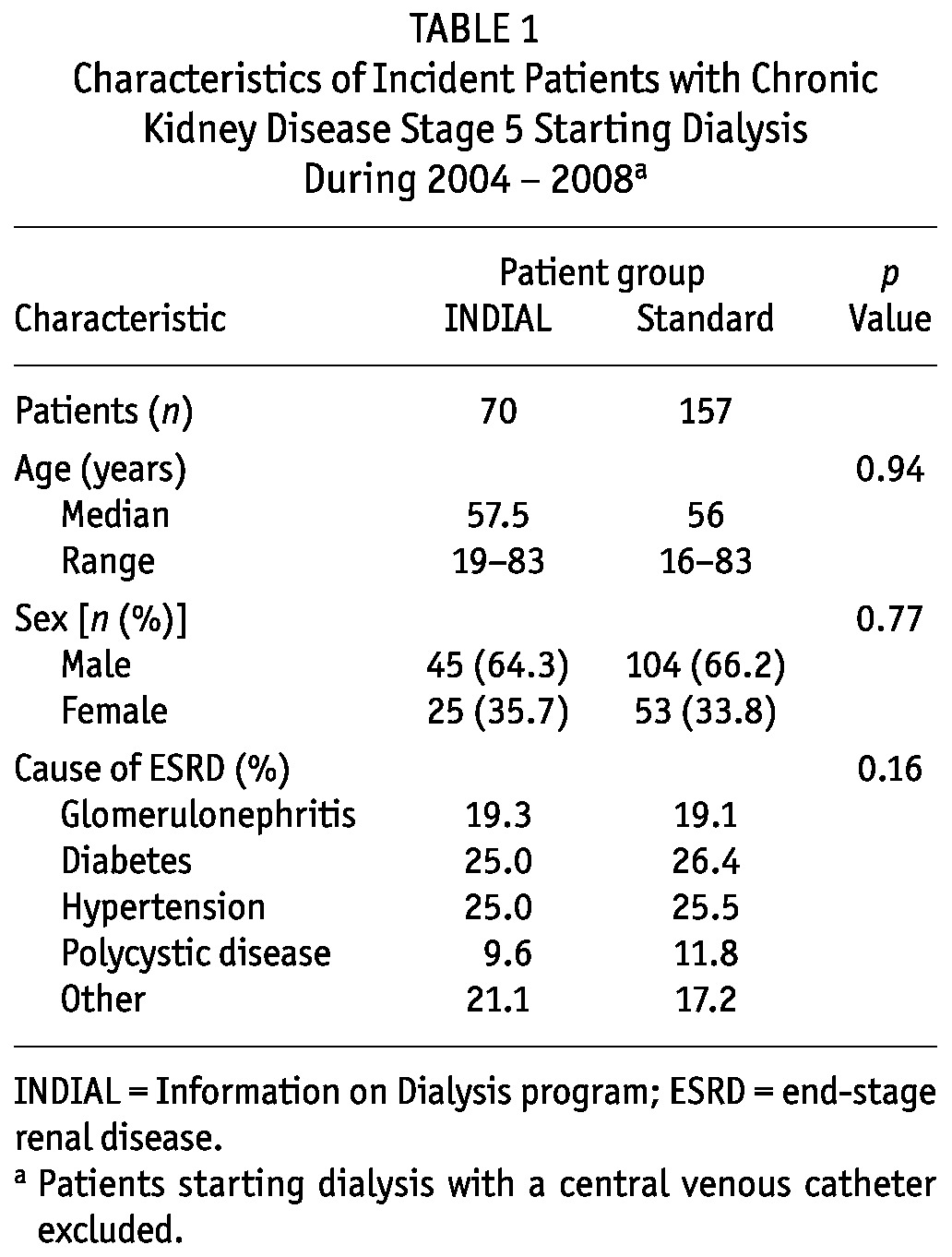
Median age was 57.5 years in the INDIAL group, and 56 years in the standard-care group (p = 0.93). Older patients chose PD significantly less often: the odds ratio for each 10 additional years of age was 0.73 (95% CI: 0.60 to 0.89; p < 0.001). However, after INDIAL, patients opted preferentially for PD even after correction for the influence of age. The age-corrected odds ratio was 3.35 (95% CI: 1.82 to 6.14; p < 0.001).
Discussion
Pre-dialysis education helps to overcome fears about dialysis and helps patients to choose a dialysis modality. In the present study we saw that the INDIAL multidisciplinary pre-dialysis education program had a significant impact on the frequency distribution of dialysis modalities. After excluding all emergency starts and late-referral patients, the educated CKD5 patients started significantly more often with PD (54.3%) than did patients in the control group, of whom only 28% initiated PD. This marked difference persisted after adjustment for age, although older patients started significantly less often with PD.
Our results accord with findings in previous studies, emphasizing the importance of pre-dialysis counseling on the choice of dialysis treatment. According to a British report, 45% of CKD5 patients who received information about their illness and available dialysis modalities chose PD as their RRT (8). Similar results were obtained in the National Pre-ESRD Education Initiative, among whose 15 000 enrolled patients, 55% chose HD and 45% chose PD after being educated about kidney disease and RRTs (15). Manns et al. (7) showed that a patient-centered education intervention significantly increased the proportion of patients opting for self-care dialysis.
In contrast to those optimistic studies of 10 years ago, a recently published survey on patient awareness of PD for the Comprehensive Dialysis Study revealed that 61% of surveyed patients reported hearing a discussion about PD, but only 10.9% initiated PD. In contrast, just 1.6% of patients not informed about the PD treatment option started with PD. The authors ascribe these somewhat surprising results to a lack of information about the content and duration of, or the patient satisfaction with, PD information and to variability in the selection of PD in the 18 participating ESRD Network areas (10).
The dialysis patients in our study who received education were significantly younger than those in the control group, although the difference was no longer detectable after all patients with a CVC had been excluded. Nevertheless, in our cohort, the chance of starting with PD declined significantly with increasing age. Younger patients have fewer comorbidities, are more self-determined, and are more often employed. As such, they are more likely to join an education program and to choose PD as a modality more suited to their needs, in that it offers more flexibility and personal freedom (16-18). Not all of the patients in our study might have started with their chosen dialysis modality after attending INDIAL. Additional factors (for example, medical or social factors) might have influenced their ultimate choice of a dialysis modality. On the other hand, it is clear that patients cannot be forced to start with a therapy that they refuse. Home-based treatments especially call for motivated and adherent patients who are committed to their therapy. In that respect, we think that our education program indeed had an impact not only on awareness, but also on choice of a dialysis modality.
A multidisciplinary pre-dialysis education program such as INDIAL gives patients the opportunity to make an informed choice of their preferred dialysis modality and implies further advantages. Patients who receive timely education have a higher probability of starting dialysis in a structured setting and of avoiding urgent dialysis because of late referral, a situation associated with high mortality (19). Pre-dialysis education improves access to PD and home HD. There is broad consensus in the nephrology community that PD is an underutilized method when its benefits are taken into account (20).
Overall survival and infectious complications are similar for PD and HD, but health care costs are lower, quality of life is better, and satisfaction with care is higher with PD (21-25). An investigation in our own unit revealed that the average daily costs for medication for 1 PD patient totaled to €32.5 compared with €49.5 for 1 HD patient. The cost difference was attributable mainly to the higher use of erythropoiesis-stimulating agents in the HD group (data not shown). The advantages of PD, especially during the early phases of treatment, have led to the concept of integrated care (3,26), and a pre-dialysis education program is a valuable component of that approach. It must be borne in mind that success is closely related to the time spent with patients during such a program, as Levin et al. (19) already showed in their study more than 10 years ago. Our results suggest that the INDIAL program fulfills those prerequisites, because a multidisciplinary team deals with a small group of patients and their relatives in a 2-day course, facilitating adequate education quality.
Because of its observational design, our study has limitations, and our findings cannot be generalized. Group allocation was not performed in a randomized controlled setting, and so confounding cannot be ruled out. It must be noted that the INDIAL program was designed not for a scientific trial, but to introduce pre-dialysis education into our clinical routine. Another drawback of the study is that during 2004 - 2008, only 25% of incident ESRD patients took part in INDIAL. This relatively small number can be traced back to the voluntary character of the program and to the fact that patients were also being referred to dialysis in an urgent setting. Our study therefore unveils the problem of recruiting patients for such a pre-dialysis education program in daily clinical practice. That problem has not yet been addressed in studies dealing with pre-dialysis patient education, and it is certainly one that deserves particular attention in the future.
Conclusions
In general, the present study suggests that a predialysis education program has an impact on the choice of dialysis modality, underlining the importance of such a program in the effort to further increase the number of PD patients treated using an integrated care approach. Furthermore, our study also points to the challenge of motivating patients to attend an education program. Implementation of pre-dialysis counseling programs is undoubtedly valuable, but future research should look for ways to assure that as many patients as possible take part in them.
Disclosures
WR receives an unrestricted research grant from Baxter Healthcare Austria.
Acknowledgments
We thank Mrs. Monika Wagner and Mrs. Karin Pfeffer for their commitment to implementing the INDIAL program. We also thank Dr. Reinhard Kramar from the Austrian Dialysis and Transplant Registry for his support in data collection.
References
- 1. United States, Department of Health and Human Services, National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, US Renal Data System (USRDS) USRDS 2009 Annual Data Report: Atlas of Chronic Kidney Disease and End-Stage Renal Disease in the United States. Bethesda, MD: USRDS; 2009. [Google Scholar]
- 2. Heaf J. Underutilization of peritoneal dialysis. JAMA 2004; 291:740–2 [DOI] [PubMed] [Google Scholar]
- 3. Van Biesen W, Vanholder RC, Veys N, Dhondt A, Lameire NH. An evaluation of an integrative care approach for end-stage renal disease patients. J Am Soc Nephrol 2000; 11:116–25 [DOI] [PubMed] [Google Scholar]
- 4. Mendelssohn DC, Pierratos A. Reformulating the integrated care concept for the new millennium. Perit Dial Int 2002; 22:5–8 [PubMed] [Google Scholar]
- 5. Golper TA. Learning about the practice of peritoneal dialysis. Kidney Int 2009; 76:12–14 [DOI] [PubMed] [Google Scholar]
- 6. Mehrotra R, Marsh D, Vonesh E, Peters V, Nissenson A. Patient education and access of ESRD patients to renal replacement therapies beyond in-center hemodialysis. Kidney Int 2005; 68:378–90 [DOI] [PubMed] [Google Scholar]
- 7. Manns BJ, Taub K, Vanderstraeten C, Jones H, Mills C, Visser M, et al. The impact of education on chronic kidney disease patients’ plans to initiate dialysis with self-care dialysis: a randomized trial. Kidney Int 2005; 68:1777–83 [DOI] [PubMed] [Google Scholar]
- 8. Little J, Irwin A, Marshall T, Rayner H, Smith S. Predicting a patient’s choice of dialysis modality: experience in a United Kingdom renal department. Am J Kidney Dis 2001; 37:981–6 [DOI] [PubMed] [Google Scholar]
- 9. Lo WK, Kwan TH, Ho YW, Lee M, Cheng YY, Ng SY, et al. Preparing patients for peritoneal dialysis. Perit Dial Int 2008; 28(Suppl 3):S69–71 [PubMed] [Google Scholar]
- 10. Kutner NG, Zhang R, Huang Y, Wasse H. Patient awareness and initiation of peritoneal dialysis. Arch Intern Med 2011; 171:119–24 [DOI] [PubMed] [Google Scholar]
- 11. Yeoh HH, Tiquia HS, Abcar AC, Rasgon SA, Idroos ML, Daneshvari SF. Impact of predialysis care on clinical outcomes. Hemodial Int 2003; 7:338–41 [DOI] [PubMed] [Google Scholar]
- 12. Winkelmayer WC, Owen WF, Jr, Levin R, Avorn J. A propensity analysis of late versus early nephrologist referral and mortality on dialysis. J Am Soc Nephrol 2003; 14:486–92 [DOI] [PubMed] [Google Scholar]
- 13. Marrón B, Martínez Ocaña JC, Salgueira M, Barril G, Lamas JM, Martín M, et al. Analysis of patient flow into dialysis: role of education in choice of dialysis modality. Perit Dial Int 2005; 25(Suppl 3):S56–9 [PubMed] [Google Scholar]
- 14. Hemodialysis Adequacy 2006 Work Group Clinical practice guidelines for hemodialysis adequacy, update 2006. Am J Kidney Dis 2006; 48(Suppl 1):S2–90 [DOI] [PubMed] [Google Scholar]
- 15. Golper T. Patient education: can it maximize the success of therapy? Nephrol Dial Transplant 2001; 16(Suppl 7):20–4 [DOI] [PubMed] [Google Scholar]
- 16. Julius M, Kneisley JD, Carpentier-Alting P, Hawthorne VM, Wolfe RA, Port FK. A comparison of employment rates of patients treated with continuous ambulatory peritoneal dialysis vs in-center hemodialysis (Michigan End-Stage Renal Disease Study). Arch Intern Med 1989; 149:839–42 [PubMed] [Google Scholar]
- 17. Merkus MP, Jager KJ, Dekker FW, Boeschoten EW, Stevens P, Krediet RT. Quality of life in patients on chronic dialysis: self-assessment 3 months after the start of treatment. The NECOSAD Study Group. Am J Kidney Dis 1997; 29:584–92 [DOI] [PubMed] [Google Scholar]
- 18. Wuerth DB, Finkelstein SH, Schwetz O, Carey H, Kliger AS, Finkelstein FO. Patients’ descriptions of specific factors leading to modality selection of chronic peritoneal dialysis or hemodialysis. Perit Dial Int 2002; 22:184–90 [PubMed] [Google Scholar]
- 19. Levin A, Lewis M, Mortiboy P, Faber S, Hare I, Porter EC, et al. Multidisciplinary predialysis programs: quantification and limitations of their impact on patient outcomes in two Canadian settings. Am J Kidney Dis 1997; 29:533–40 [DOI] [PubMed] [Google Scholar]
- 20. Chaudhary K, Sangha H, Khanna R. Peritoneal dialysis first: rationale. Clin J Am Soc Nephrol 2011; 6:447–56 [DOI] [PubMed] [Google Scholar]
- 21. Mehrotra R, Chiu YW, Kalantar-Zadeh K, Bargman J, Vonesh E. Similar outcomes with hemodialysis and peritoneal dialysis in patients with end-stage renal disease. Arch Intern Med 2011; 171:110–18 [DOI] [PubMed] [Google Scholar]
- 22. Aslam N, Bernardini J, Fried L, Burr R, Piraino B. Comparison of infectious complications between incident hemodialysis and peritoneal dialysis patients. Clin J Am Soc Nephrol 2006; 1:1226–33 [DOI] [PubMed] [Google Scholar]
- 23. Shih YC, Guo A, Just PM, Mujais S. Impact of initial dialysis modality and modality switches on Medicare expenditures of end-stage renal disease patients. Kidney Int 2005; 68:319–29 [DOI] [PubMed] [Google Scholar]
- 24. Kutner NG, Zhang R, Barnhart H, Collins AJ. Health status and quality of life reported by incident patients after 1 year on haemodialysis or peritoneal dialysis. Nephrol Dial Transplant 2005; 20:2159–67 [DOI] [PubMed] [Google Scholar]
- 25. Rubin HR, Fink NE, Plantinga LC, Sadler JH, Kliger AS, Powe NR. Patient ratings of dialysis care with peritoneal dialysis vs hemodialysis. JAMA 2004; 291:697–703 [DOI] [PubMed] [Google Scholar]
- 26. Blake PG. Integrated end-stage renal disease care: the role of peritoneal dialysis. Nephrol Dial Transplant 2001; 16(Suppl 5):61–6 [DOI] [PubMed] [Google Scholar]