Abstract
♦ Background: Transfer to hemodialysis (HD) is a frequent cause of peritoneal dialysis (PD) cessation. In the present study, we set out to describe the transition period between PD and HD.
♦ Methods: All patients in 4 centers of Basse-Normandie who had been treated with PD for more than 90 days and who were permanently transferred to HD between 1 January 2005 and 31 December 2009 were retrospectively reviewed. The rate of unplanned HD start was evaluated.
♦ Results: In the 60 patients (39 men, 21 women) included in the study, median score on the Charlson comorbidity index at PD initiation was 5 [interquartile range (IQR): 3 - 7], median age at HD initiation was 62 years (IQR: 54 - 76 years), and median duration on PD was 22 months (IQR: 12 - 36 months). Among the 60 patients, 37 had an unplanned HD initiation. Peritonitis was the most frequent cause of unplanned HD start (n = 20), and dialysis inadequacy (n = 11), the main cause of planned HD start. During the transition period, all patients were hospitalized. Median duration of hospitalization was 4.5 days (IQR: 0 - 25.5 days). Within 2 months after HD initiation, 9 patients died. Two months after starting HD, 6 of the remaining 51 patients were being treated in a self-care HD unit and only 23 patients had a mature fistula.
♦ Conclusions: Unplanned HD start is a common problem in patients transferred from PD. Further studies are needed to improve the rate of planned HD start in PD patients transferred to HD.
Key words: Technique failure, transition
It is well-established that technique failure is one of the main reasons for peritoneal dialysis (PD) cessation (1). Theoretically, the transfer to hemodialysis (HD) should be a particular point in a gradual process that should start with PD and finish with HD (2,3). The term “transition” has recently been used to refer to the movement between PD and HD. Because unplanned HD initiation is associated with mortality, the so-called transition period between dialysis modalities must be anticipated and planned (4,5). In addition, compared with an unplanned HD start, planned HD initiation would have a lesser psychological effect and therefore a lesser impact on a patient’s quality of life. Nevertheless, sudden PD failure may jeopardize the gradual move to HD and affect patient outcome.
To attempt to prevent unplanned HD initiation, patients who are likely to fail PD should be prepared for HD. Although clinical advice and guidelines about transfer from PD to HD have been issued, predicting PD failure is still a matter of concern for clinicians (6,7). Models that might predict technique survival in the clinical setting are expected (8,9), but data about unexpected HD transfer and unplanned HD start in PD patients are lacking. The main objective of the present descriptive study was to provide information about the circumstances of HD initiation in PD patients switched to HD. A secondary object was to evaluate rates of unexpected transfer to HD and outcomes during the transition period.
Methods
Study Population
This retrospective study assessed patients transferred from PD to HD in one French region (Basse-Normandie). Among the 6 dialysis centers of Basse-Normandie, 5 are members of the French Peritoneal Dialysis Registry (RDPLF). Of those 5 centers, 4 agreed to participate in the study.
In the RDPLF, each transfer to HD must be categorized by the nephrologist as a permanent switch to HD or a temporary transfer to HD. In the RDPLF, transfer category is a declarative covariate, and a permanent switch to HD is defined as a transfer lasting more than 2 months. In an attempt to validate the transfer category, the time spent on HD is calculated using a new RDPLF registration date when a subject restarts PD.
We identified all incident PD patients in the RDPLF database who were categorized as permanently transferred to HD between 1 January 2005 and 31 December 2009. We then selected all patients who had been treated with PD for more than 90 days. From the RDPLF, we extracted patient sex, age at PD start, underlying nephropathy, diabetes status, and Charlson comorbidity index (CCI) score at PD initiation. In an attempt to evaluate the role of the comorbidities independent of patient age, we calculated a modified CCI score by subtracting the age sub-score. By French legislation, data collection about ethnic origin is not authorized, and therefore data on race were not collected.
We also extracted patient age, type of PD (continuous ambulatory PD or automated PD), modality of assistance (assisted PD or self-care PD), and the reasons for stopping PD at PD cessation. Cause of PD cessation is a declarative covariate, and details about the origin of PD failure are not collected by the RDPLF. Peritonitis episodes during PD were also extracted from the database.
For evaluation of the hospital stay during transition, additional information was extracted from the administrative database of each hospital. Data about HD start were obtained by an extensive review of patient files (as described shortly). In addition, HD transfer and HD transfer duration were checked during the chart review to confirm the transfer category.
Definition of the Transition Period
In most registries, it is accepted that an event occurring within 2 months after a PD patient’s transfer to HD can be attributed to PD. Because of both surgical delay and fistula maturation, the total time between surgeon referral and first vascular access cannulation in incident HD patients is close to 3 months (10). Furthermore, late referral before HD start is defined as a nephrology follow-up of less than 3 months before dialysis initiation (5). The known benefits of arteriovenous fistula imply that PD patients should be converted to HD with a mature vascular access. That understanding emphasizes the fact that a decision to switch a PD patient to HD should theoretically be made at least 3 months before the transfer. Even though transfer to HD is often not a sudden event, there is, to our knowledge, no clear definition of the transition period available. We therefore arbitrarily defined the transition period as a period beginning 3 months before and ending 2 months after HD initiation.
Definition of the Events
Evoked Transfer to HD: To examine the rate of evoked transfer to HD, we looked in the patient’s file for any physician’s note that was made more than 3 months before HD initiation and that evoked the need for HD conversion. This “evoked transfer” information was collected for each patient transferred to HD.
Unplanned HD Initiation: It is well recognized that, in incident dialysis patients, starting HD through a HD catheter is associated with an increased risk of mortality. In addition, a HD catheter increases the workload of the dialysis nurses and has an impact on the organization of the dialysis center. However, permanent catheters are commonly used in patients in whom a fistula cannot be created because of medical problems or patient refusal. Thus, unplanned HD initiation was defined as starting HD with a temporary HD catheter. It is important to note that the unplanned transfer to HD could, in some cases, be explained by the cause of the transfer itself. However, use of a temporary catheter also highlights the fact that the transfer is unplanned, whatever the cause happens to be.
Urgent HD Initiation: Urgent-start HD was defined as a requirement to start HD because of severe overhydration, pericarditis, neurologic disorder, hyperkalemia, or severe acidosis fewer than 24 days after the beginning of management by a nephrologist.
Outcome During the Transition Period
To assess patient outcomes, we studied the occurrence of hospitalization during the transition period. Hospitalization at the time of a patient’s transfer to HD was recorded, as was the duration of the hospital stay. In addition, the number of hospitalizations and the hospitalization durations before and after the transfer to HD were collected. The type of vascular access (fistula, tunneled catheter, temporary catheter) at the end of the transition period (2 months after HD initiation) was noted. The vascular access was considered to be a HD catheter when HD was performed through a HD catheter while awaiting fistula maturation. The dialysis facility (in-center HD, self-care HD) when a patient was switched to HD was obtained. Also, the dialysis facility at the end of the transition period was noted. We examined serum albumin, hemoglobin, and serum creatinine at the beginning and end of the transition period.
Statistical Analysis
Continuous variables are expressed as means and standard deviations, or median with first and third quartiles [interquartile range (IQR)]. Categorical variables are expressed as proportions. A bivariate analysis using the Fisher exact test was performed for categorical variables, and an unpaired t-test or Mann-Whitney test, when required, was used for continuous variables. In addition, a logistic regression analysis was used to estimate the strength of the association between each covariate and unplanned HD initiation. Subsequently, a multivariate logistic regression analysis for unplanned HD initiation was performed. Only 95% confidence intervals (CIs) were used for statistical inference and to represent the uncertainty of the odds ratio. Statistical differences were considered significant at p < 0.05. Statistical analyses were performed using the R 2.13.1 software application (The R Foundation for Statistical Computing, Vienna, Austria).
Results
Patient Characteristics
During the study period, 60 PD patients (39 men, 21 women; 12 with diabetes; 37 on automated PD, 23 on continuous ambulatory PD) were switched to HD. At PD initiation, the median age of these patients was 60 years (IQR: 51 - 74 years), the median CCI score was 5 (IQR: 3 - 7), and the median modified CCI score was 3 (IQR: 2 - 4). The underlying nephropathies were glomerulonephritis (n = 16), vascular (n = 12), chronic interstitial nephritis (n = 9), diabetic (n = 7), congenital (n = 5), miscellaneous (n = 2), and unknown (n = 9). Of the 60 patients, 21 received assisted PD. Median duration on PD was 22 months (IQR: 12 - 36 months). The group experienced 115 peritonitis episodes during a cumulative 1532 months on PD (0.97 ± 0.96 episodes per patient-year on PD).
Causes of Technique Failure
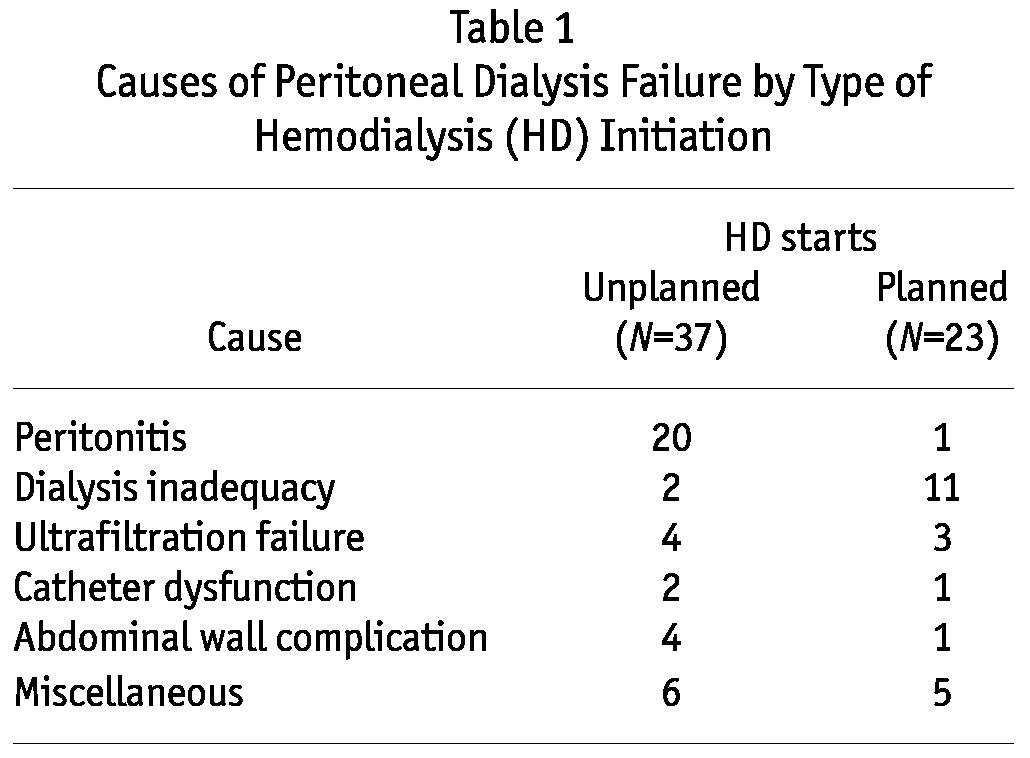
The most common reasons for technique failure were peritonitis (n = 21) and dialysis inadequacy (n = 13). Ultrafiltration failure led to 7 patients being transferred to HD. Of the 19 remaining patients, 6 were transferred because of abdominal surgery, 5 because of abdominal wall complications, and 3 because of catheter dysfunction. Malnutrition and patient burnout were responsible for 3 and 2 PD failures respectively. Peritonitis was the most frequent cause of PD failure in the unplanned HD start group; dialysis inadequacy was the main cause of PD cessation in the planned HD start group (Table 1).
Table 1.
Causes of Peritoneal Dialysis Failure by Type of Hemodialysis (HD) Initiation
Evoked Hemodialysis Transfer
Based on the notes written by nephrologists in the charts, we found that patient transfer to HD was evoked for 16 of the 60 patients switched to HD (26%). In the evoked transfer group, the reasons for stopping PD were dialysis inadequacy (n = 7), peritonitis (n = 2), ultrafiltration failure (n = 2), malnutrition (n = 2), abdominal wall complications (n = 1) catheter dysfunction (n = 1), and patient burnout (n = 1). In the non-evoked transfer group, the causes of PD cessation were peritonitis (n = 19), dialysis inadequacy (n = 6), ultrafiltration failure (n = 5), abdominal surgery (n = 6), abdominal wall complications (n = 4), catheter dysfunction (n = 2), malnutrition (n = 1), and patient burnout (n = 1).
Unplanned HD Initiation
Among the 60 patients switched from PD to HD, 37 had an unplanned HD initiation. The rate of urgent HD initiation was similar in the unplanned and planned HD start groups (6 vs 1 respectively). The rate of evoked HD transfer was greater in the planned HD start group than in the unplanned HD start group (3 vs 13 respectively, p < 0.01, Figure 1). We observed no significant differences between the unplanned HD starters and the planned HD starters with respect to median age, median CCI score, and median modified CCI score at dialysis initiation (Table 2).
Figure 1.
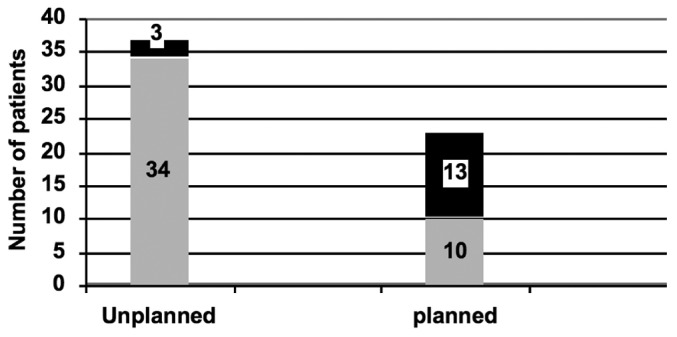
— Rate of unplanned hemodialysis (HD) initiation. Transfer to HD not planned 3 months before HD initiation (gray bars); transfer to HD planned 3 months before HD initiation (black bars).
Table 2.
Factors Associated With Unplanned Hemodialysis (HD) Initiation, Bivariate Analysis
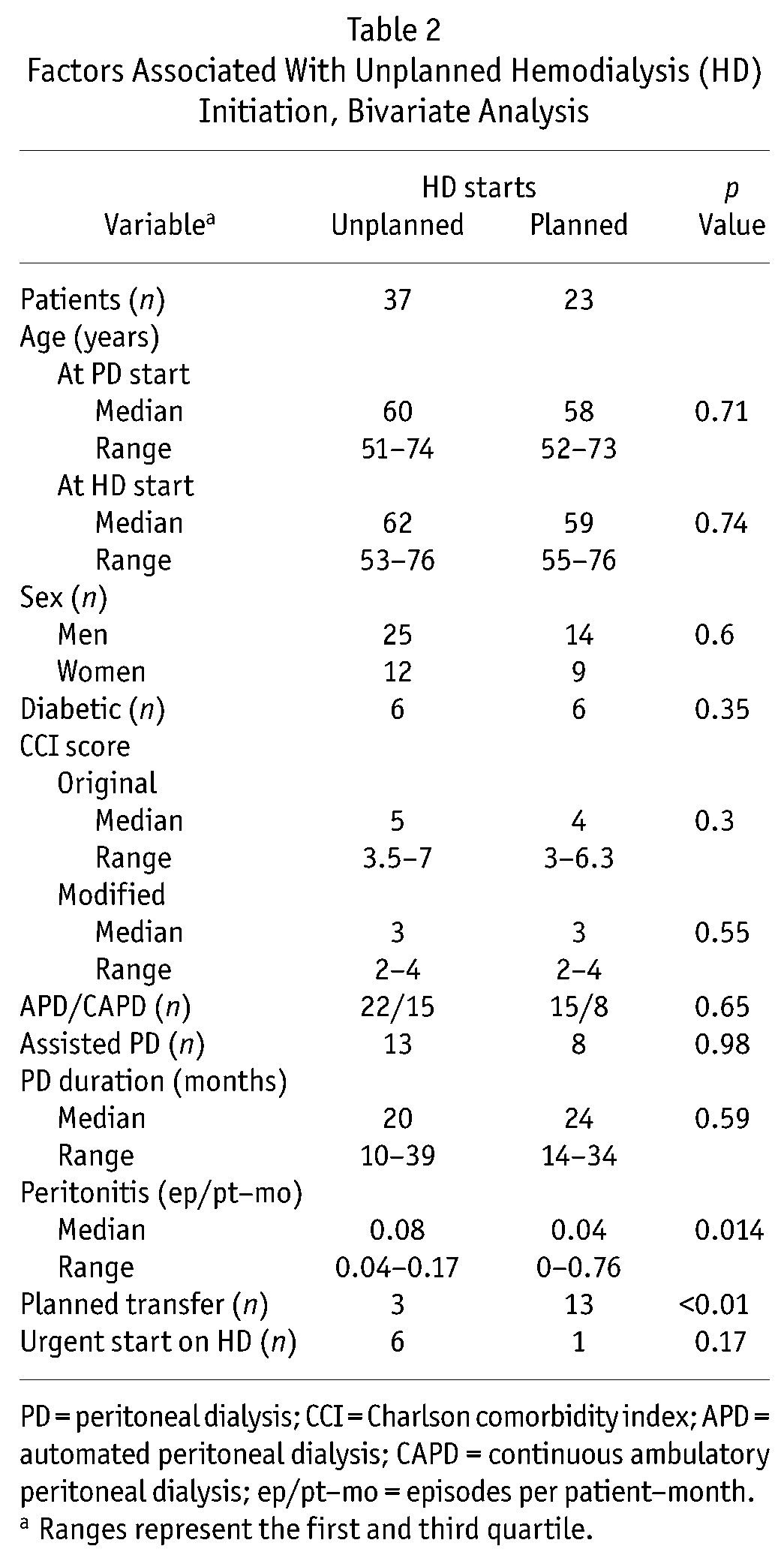
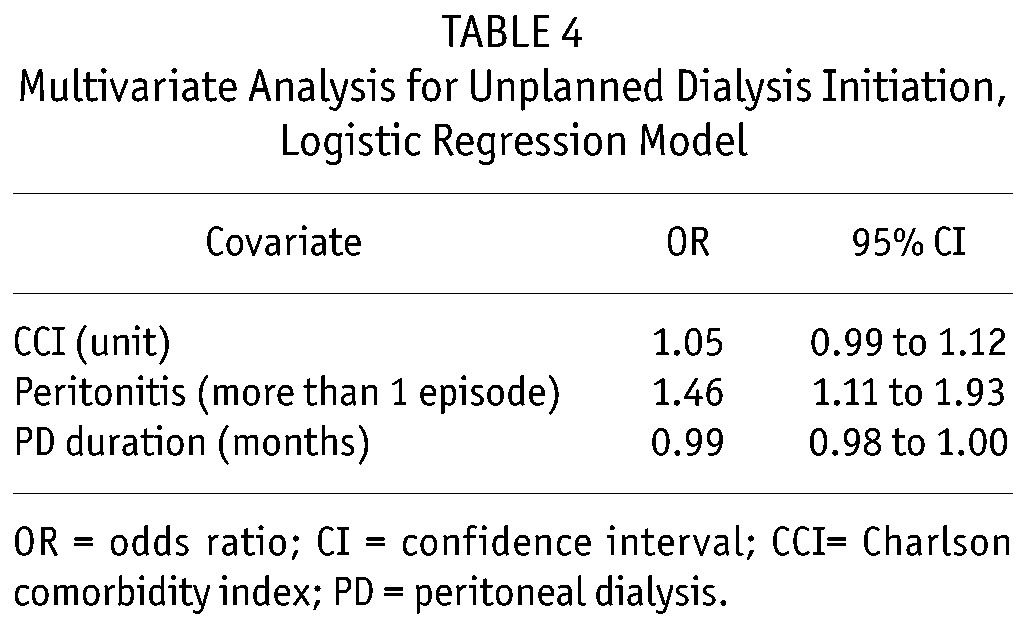
In the bivariate logistic regression analysis, the peritonitis rate was associated with a higher risk of unplanned HD start. Patient age, comorbidities, diabetes, dialysis assistance, PD dialysis modality, PD duration, and center were not associated with unplanned HD start (Table 3). In the multivariate logistic regression analysis (Table 4), after adjustment both for CCI score and PD duration, experience of more than 2 peritonitis episodes was associated with a higher risk of unplanned HD start (odds ratio: 1.46; 95% CI: 1.11 to 1.93).
Table 3.
Bivariate Analysis for Unplanned Hemodialysis (HD) Initiation, Logistic Regression
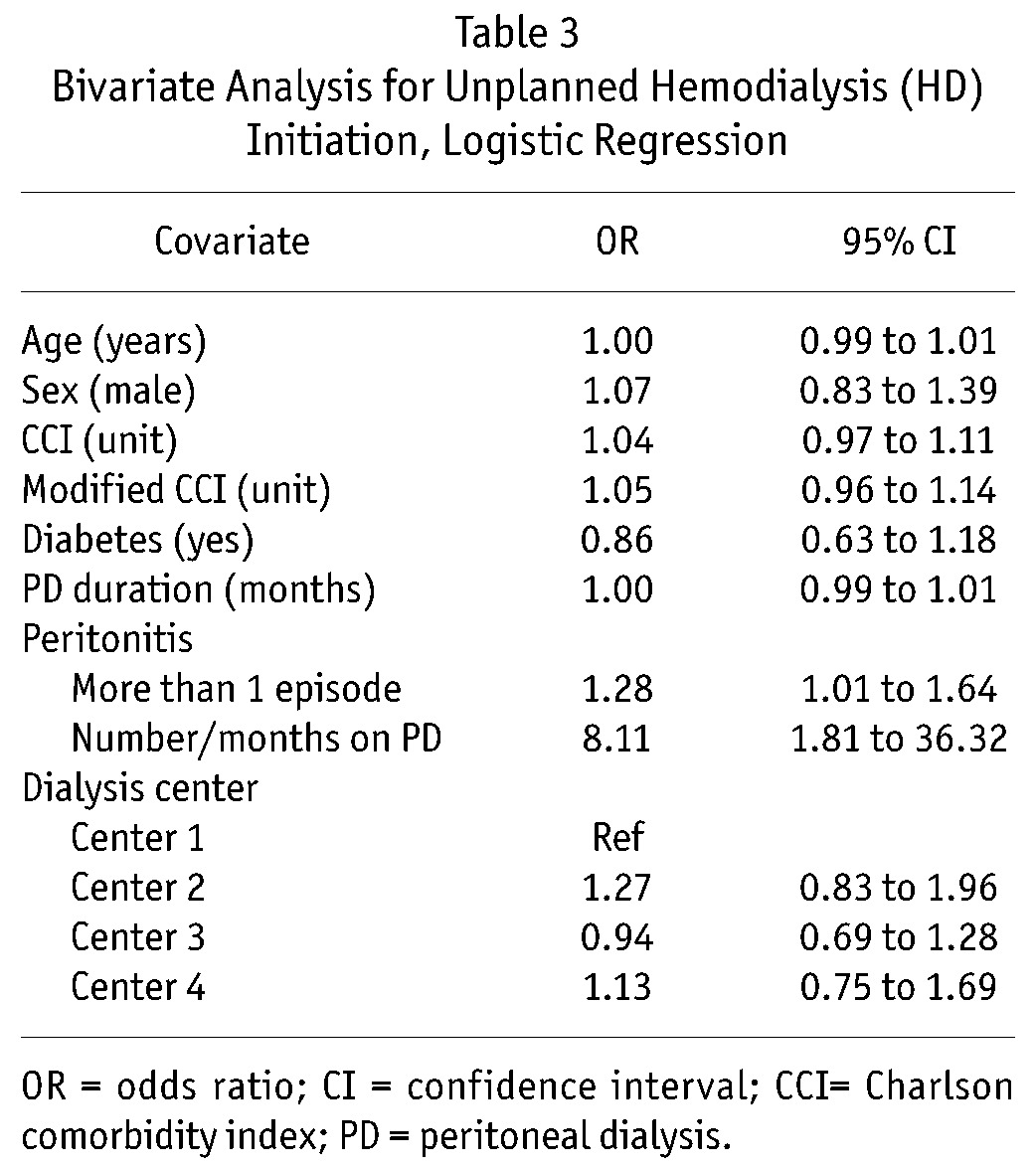
TABLE 4.
Multivariate Analysis for Unplanned Dialysis Initiation, Logistic Regression Model
Outcome During the Transition Period
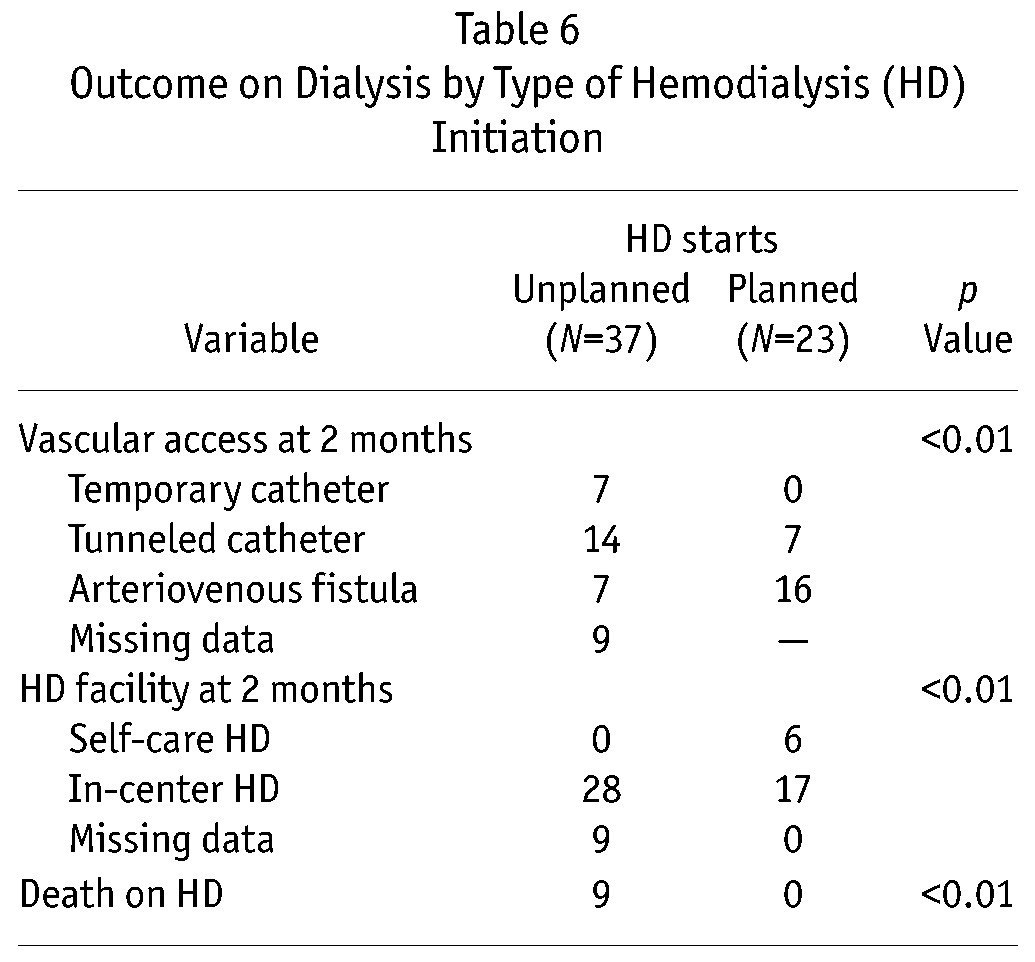
Compared with the planned HD starters, unplanned HD starters were more frequently hospitalized during the first HD session (37 of 37 unplanned vs 7 of 23 planned, p < 0.01; Figure 2; Table 5). The mean number of hospitalizations during the transition period was higher for the unplanned HD starters than for the planned HD starters. Compared with the planned HD starters, the unplanned HD starters experienced longer hospitalization periods during the transition period. At the end of the transition period, a mature fistula was available in only 7 patients of the unplanned HD group compared with 16 patients of the planned HD group (Table 6). No patient in the unplanned HD start group was treated in a self-care HD unit; 6 of 23 patients in the planned HD start group were so treated (Table 6). Except for serum albumin, we observed no significant difference between the unplanned and planned HD start groups with respect to biologic value.
Figure 2.
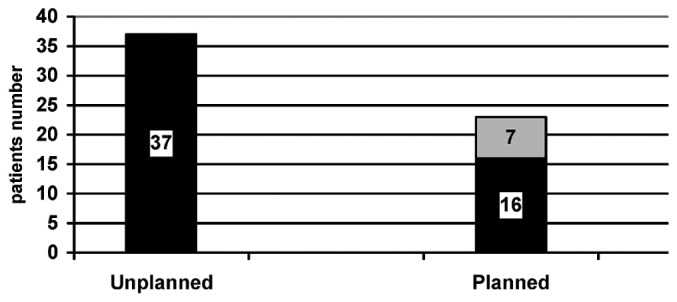
— Hospitalization rate during transition. Patients hospitalized during transition (black bars); patients not hospitalized during transition (gray bars).
TABLE 5.
Hospitalization by Type of Hemodialysis (HD) Initiation
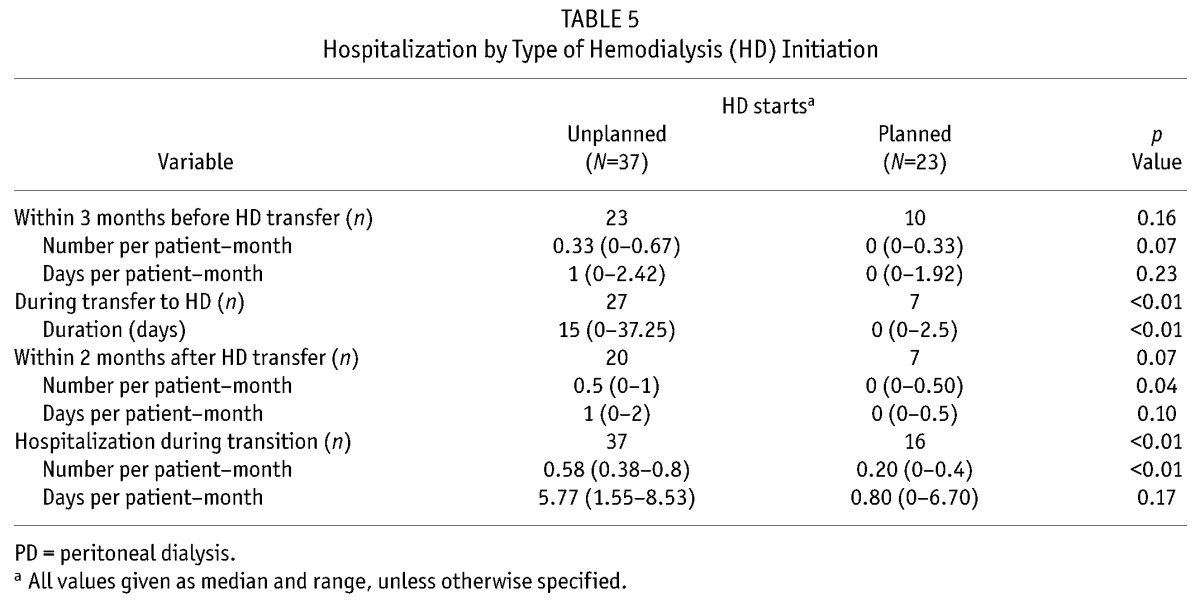
Table 6.
Outcome on Dialysis by Type of Hemodialysis (HD) Initiation
Discussion
Although several reports have underlined the fact that PD can be used for a long duration, technique survival remains a main concern for nephrologists in charge of PD patients (1). In a report from the Netherlands Cooperative Study on the Adequacy of Dialysis, the 2-year technique survival in Netherlands PD patients who started renal replacement therapy on PD was 64% (11). Data from the Australian and New Zealand Dialysis and Transplantation Registry showed that death-censored median technique survival was 3.7 years in incident PD patients. In France, the median time on PD of patients transferred to HD in 2009 was 19 months (12). Therefore, transfer of PD patients to HD must be taken into account in the patient trajectory. It has been suggested that an integrative care approach based on an appropriate on-time transfer from PD to HD could improve outcomes in patients on dialysis (2,13-15). Furthermore, it has recently been emphasized that transition between PD and HD should be planned and anticipated (4,16). However, little is known about HD initiation in patients transferred from PD.
One of the main concerns in transition is the timely creation of a vascular access in PD patients switching from PD to HD (17). Preemptive fistula is not recommended in patients starting PD (18,19). At the same time, because PD failure is not easily predictable, PD patients could undergo HD initiation using a temporary HD catheter. For patients entering into dialysis, a higher mortality risk is associated with unplanned HD initiation than with planned dialysis start (5,20,21). The worse outcomes of unplanned HD starters is partly explained by the complications associated with HD catheters (22,23). To our knowledge, no data about the impact of unplanned HD start in PD patients are available. However, it is obvious that unplanned HD start in PD patients would have a negative effect on patient outcomes.
In our study, 37 of 60 patients experienced an unplanned HD initiation. Unplanned HD start could have been avoided in at least 6 of the 37 (16%). Those findings are consistent with the results of a recent study from Hong Kong, in which a temporary HD catheter was more often required in patients who transferred from PD than in incident HD patients (16). Because pre-emptive fistula creation is not recommended in incident PD patients, it is understandable that most of the early transfers to HD may occur in patients with no vascular access (24-26).
In an attempt to study late PD failure, only patients who remained on PD for more than 3 months were included in our study. Our report shows that, in the unplanned HD start group, the main cause for PD cessation was peritoneal infection. In the multivariate analysis, experiencing more than 2 peritonitis episodes was associated with a higher risk of unplanned HD start. To increase the number of PD patients with a mature fistula at HD start, predictive models are awaited that could help the clinician make a decision about fistula creation in PD patients (9,17). It is important to note that peritonitis caused by enteric micro-organisms is associated with a higher frequency of technique failure than is peritonitis caused by other agents (27). It might therefore be argued that vascular access creation should be considered in patients with a higher risk of enteric peritonitis.
The term “transition” was introduced in the last European Renal Best Practice clinical advisory to describe a smooth conversion between PD and HD (6). Unfortunately, based on the hospitalization requirement during the period of our study and on the rate of unplanned HD starts, it might be argued that transfer from PD to HD needs significant improvement.
Even though PD is considered a method of home therapy, it is important to note that, in our study, most of the patients transferring from PD to HD were treated at in-center HD units 2 months after their dialysis modality conversion. Those findings also highlight the increase in demand that PD transfer places on in-center HD units and the effort that must be made to provide self-care HD or home HD for PD patients transferred to HD (28). Like others, we therefore believe that a pre-emptive education program for self-care HD, dedicated to PD with a planned transfer to HD, should be implemented.
Our study, conducted in only one French region, has limitations not only because of the sample size, but also because of the definition of the transition period and the demographics and comorbidities of the population. At the same time, our region has had the highest rate of PD utilization in France for many years (29). Because the study was conducted in only one country, generalization of the results requires caution. Our results raise the problem of unplanned HD initiation in patients transferred from PD to HD. To lower the rate of unplanned dialysis initiation, further studies are needed to determine when and for whom a vascular access for HD should be created in PD patients. The current concept of PD “failure” leading to transfer to HD could become obsolete, to be replaced by the idea of a smooth transition from one dialysis modality to another as a normal stage in the trajectory of end-stage renal disease patients.
Disclosures
The authors have no financial conflicts of interest with respect to this study.
References
- 1. Davies SJ, Phillips L, Griffiths AM, Russell LH, Naish PF, Russell GI. What really happens to people on long-term peritoneal dialysis? Kidney Int 1998; 54:2207–17 [DOI] [PubMed] [Google Scholar]
- 2. Van Biesen W, Vanholder RC, Veys N, Dhondt A, Lameire NH. An evaluation of an integrative care approach for end-stage renal disease patients. J Am Soc Nephrol 2000; 11:116–25 [DOI] [PubMed] [Google Scholar]
- 3. Mendelssohn DC, Pierratos A. Reformulating the integrated care concept for the new millennium. Perit Dial Int 2002; 22:5–8 [PubMed] [Google Scholar]
- 4. Fluck R. Transitions in care: what is the role of peritoneal dialysis? Perit Dial Int 2008; 28:591–5 [PubMed] [Google Scholar]
- 5. Lorenzo V, Martn M, Rufino M, Hernández D, Torres A, Ayus JC. Predialysis nephrologic care and a functioning arteriovenous fistula at entry are associated with better survival in incident hemodialysis patients: an observational cohort study. Am J Kidney Dis 2004; 43:999–1007 [DOI] [PubMed] [Google Scholar]
- 6. Covic A, Bammens B, Lobbedez T, Segall L, Heimbürger O, van Biesen W, et al. Educating end-stage renal disease patients on dialysis modality selection: a clinical advice from the European Renal Best Practice (ERBP) Advisory Board. Nephrol Dial Transplant 2010; 25:1757–9 [DOI] [PubMed] [Google Scholar]
- 7. Haute Autorité de santé Indications and non-indications for chronic peritoneal dialysis in adults [French, Web page]. Saint-Denis La Plaine, France: Haute authorité de Santé; 2007. [Available at: http://www.has-sante.fr/portail/jcms/c_702927/indications-et-non-indications-de-la-dialyse-peritoneale-chronique-chez-ladulte?xtmc=&xtcr=3; accessed 1 January 2011] [Google Scholar]
- 8. Jaar BG, Plantinga LC, Crews DC, Fink NE, Hebah N, Coresh J, et al. Timing, causes, predictors and prognosis of switching from peritoneal dialysis to hemodialysis: a prospective study. BMC Nephrol 2009; 10:3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Tangri N, Ansell D, Naimark D. Predicting technique survival in peritoneal dialysis patients: comparing artifical neural networks and logistic regression. Nephrol Dial Transplant 2008; 23:2972–81 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Lobbedez T, Lecouf A, Ficheux M, Henri P, Hurault de Ligny B, Ryckelynck JP. Is rapid initiation of peritoneal dialysis feasible in unplanned dialysis patients? A single-centre experience. Nephrol Dial Transplant 2008; 23:3290–4 [DOI] [PubMed] [Google Scholar]
- 11. Jager KJ, Merkus MP, Dekker FW, Boeschoten EW, Tijssen JG, Stevens P, et al. Mortality and technique failure in patients starting chronic peritoneal dialysis: results of the Netherlands Cooperative Study on the Adequacy of Dialysis. Kidney Int 1999; 55:1476–85 [DOI] [PubMed] [Google Scholar]
- 12. Le Registre de Dialyse Péritonéale de Langue Française (RDPLF) Causes and types of dropout (Metropolitan France)—2009 [French, Web page]. Pontoise, France: RDPLF; 2010. [http://www.rdplf.org/sorties/70-sortie-2009.html; accessed 1 January 2011] [Google Scholar]
- 13. Panagoutsos S, Kantartzi K, Passadakis P, Yannatos E, Mourvati E, Theodoridis M, et al. Timely transfer of peritoneal dialysis patients to hemodialysis improves survival rates. Clin Nephrol 2006; 65:43–7 [DOI] [PubMed] [Google Scholar]
- 14. Blake PG. Integrated end-stage renal disease care: the role of peritoneal dialysis. Nephrol Dial Transplant 2001; 16(Suppl 5):61–6 [DOI] [PubMed] [Google Scholar]
- 15. Van Biesen W, Dequidt C, Vijt D, Vanholder R, Lameire N. Analysis of the reasons for transfers between hemodialysis and peritoneal dialysis and their effect on survivals. Adv Perit Dial 1998; 14:90–4 [PubMed] [Google Scholar]
- 16. Szeto CC, Kwan BC, Chow KM, Pang WF, Kwong VW, Leung CB, et al. Outcome of hemodialysis patients who had failed peritoneal dialysis. Nephron Clin Pract 2010; 116:c300–6 [DOI] [PubMed] [Google Scholar]
- 17. Chiarelli G, Beaulieu M, Cozzolino M, Singh S, Kiaii M, Taylor P, et al. Vascular access planning in peritoneal dialysis patients. Perit Dial Int 2008; 28:585–90 [PubMed] [Google Scholar]
- 18. Beckingham IJ, O’Rourke JS, Bishop MC, Blamey RW. Are backup arteriovenous fistulae necessary for patients on continuous ambulatory peritoneal dialysis? Lancet 1993; 341:1384–6 [DOI] [PubMed] [Google Scholar]
- 19. Clinical practice guidelines and clinical practice recommendations for vascular access, update 2006. Am J Kidney Dis 2006; 48(Suppl 1):S176–276 [DOI] [PubMed] [Google Scholar]
- 20. Kessler M, Frimat L, Panescu V, Briançon S. Impact of nephrology referral on early and midterm outcomes in ESRD: Epidémiologie de l’Insuffisance Renale chronique terminale en Lorraine (EPIREL): results of a 2-year, prospective, community-based study. Am J Kidney Dis 2003; 42:474–85 [DOI] [PubMed] [Google Scholar]
- 21. Astor BC, Eustace JA, Powe NR, Klag MJ, Fink NE, Coresh J. Type of vascular access and survival among incident hemodialysis patients: the Choices for Healthy Outcomes in Caring for ESRD (CHOICE) Study. J Am Soc Nephrol 2005; 16:1449–55 [DOI] [PubMed] [Google Scholar]
- 22. Pastan S, Soucie JM, McClellan WM. Vascular access and increased risk of death among hemodialysis patients. Kidney Int 2002; 62:620–6 [DOI] [PubMed] [Google Scholar]
- 23. Dhingra RK, Young EW, Hulbert-Shearon TE, Leavey SF, Port FK. Type of vascular access and mortality in U.S. hemodialysis patients. Kidney Int 2001; 60:1443–51 [DOI] [PubMed] [Google Scholar]
- 24. Kolesnyk I, Dekker FW, Boeschoten EW, Krediet RT. Time-dependant reasons for peritoneal dialysis technique failure and mortality. Perit Dial Int 2010; 30:170–7 [DOI] [PubMed] [Google Scholar]
- 25. Quinn RR, Ravani P, Hochman J. Technique failure in peritoneal dialysis patients: insights and challenges. Perit Dial Int 2010; 30:161–2 [DOI] [PubMed] [Google Scholar]
- 26. Descoeudres B, Koller MT, Garzoni D, Wolff T, Steiger J, Schaub S, et al. Contribution of early failure to outcome on peritoneal dialysis. Perit Dial Int 2008; 28:259–67 [PubMed] [Google Scholar]
- 27. Jarvis EM, Hawley CM, McDonald SP, Brown FG, Rosman JB, Wiggins KJ, et al. Predictors, treatment, and outcomes of non-Pseudomonas gram-negative peritonitis. Kidney Int 2010; 78:408–14 [DOI] [PubMed] [Google Scholar]
- 28. Wong JH, Pierratos A, Oreopoulos DG, Mohammad R, Benjamin-Wong F, Chan CT. The use of nocturnal home hemodialysis as salvage therapy for patients experiencing peritoneal dialysis failure. Perit Dial Int 2007; 27:669–74 [PubMed] [Google Scholar]
- 29. Renal Epidemiology and Information Network: 2008 REIN report [French]. Nephrol Ther 2010; 6(Suppl 2):S25–183 [DOI] [PubMed] [Google Scholar]


