Abstract
Healthcare spending varies widely across markets, and previous empirical studies find little evidence that higher spending translates into better health outcomes. The main innovation in this paper exploits this cross-sectional variation in hospital spending in a new way by considering patients who are exposed to healthcare systems not designed for them: patients far from home when a health emergency strikes. Visitors to Florida who become ill in high-spending areas have significantly lower mortality rates compared to visitors in lower-spending areas. The results are robust within groups of similar visitors and within groups of destinations that appear to be close demand substitutes—areas that likely attract similar visitors.
1. Introduction
Healthcare spending amounts to over $2 trillion in the U.S. (Catlin et al., 2007), and there are concerns that continued growth in spending will strain government budgets and limit private-sector profitability (Lee and Skinner, 1999). Further, there is some debate over the returns to healthcare spending. When countries, or regions within the U.S., are compared, large disparities in spending are found yet health outcomes are remarkably similar.1 Fisher et al. (2003) studied Medicare expenditure data and found a 60% difference between high- and low-spending areas in the U.S. Nevertheless, no mortality difference was found following a health event such as a heart attack or hip fracture. This evidence has been cited in support of reducing Medicare spending by 20–30% without adversely affecting health outcomes (Fisher, Bynum and Skinner, 2009). In contrast, instrumental-variable and panel-data evidence suggests that higher spending is associated with significantly lower mortality.2
One issue that arises with cross-country or cross-region comparisons is that greater treatment levels may be chosen for populations in worse health. For example, higher spending is strongly associated with higher mortality rates at the individual level, as more is spent on patients with greater health problems. At the regional level, summary measures of treatment intensity may reflect the underlying health of the population as well.
The main innovation in this paper exploits the large cross-sectional variation in spending intensity in a new way by comparing patients who are exposed to different healthcare systems that were not designed for them: patients who are far from home when a health emergency strikes. These visitors may have an emergency in an area that spends a great deal on patients or one that tends to spend less. To the extent that these health events are unanticipated, patients are unlikely to choose the destination based on the healthcare intensity in the area. Further, close demand substitutes in terms of destinations may attract “close substitutes” in terms of patients with similar lifestyles. As a result, geographic variation in spending practices may be considered plausibly exogenous for this group of patients, and a comparison of health outcomes for similar visitors across these locations can shed light on the returns to healthcare spending, at least in emergency situations.3
The analysis uses the universe of hospital discharges in the state of Florida—one of the most frequently visited states that provides detailed patient characteristics. The results show that patients who have a health emergency in high-spending areas have significantly lower inpatient mortality rates compared to those visiting low-spending areas. The results are less informative with regard to the mechanisms of the decrease in mortality. Suggestive evidence shows that high-spending areas offer a bundle of services, most notably a greater reliance on intensive-care-unit services and a higher likelihood of treatment in a teaching hospital.
Of course, visitors are not randomly assigned to destinations. If relatively healthy individuals were to choose high-spending areas, or if high-spending areas tend to admit relatively healthy visitors into the hospital, then the results would reflect these differences. Much of the results section demonstrates that the estimates are robust within groups of similar patients and that selection into the hospital is unlikely to drive the results.
The outline of the paper is as follows. Section 2 presents the empirical framework. Section 3 describes the data, including a comparison of high- and low-spending areas in terms of patient characteristics. Section 4 presents the main estimates of the relationship between inpatient mortality and local-area healthcare spending. The analysis focuses on heart conditions, although results for other common emergencies are reported as well. Section 5 interprets the results by considering how treatment in local areas that spend more differs from treatment provided in less costly areas. Section 6 concludes.
2. Empirical Framework
A large literature documents the remarkable geographic variation in healthcare spending, as well as relatively similar health outcomes for patients who experience a health problem such as a heart attack. The main estimating equation for such an analysis for patient i treated in geographic area g(i) is:
| (1) |
where M represents mortality, T represents a measure of treatment intensity in the area, and X includes controls for individual characteristics such as age, race, sex, and diagnoses.
End-of-life spending, such as average expenditures in the area for patients’ last hospital stays, is a commonly used proxy for treatment intensity in an area (Fisher et al., 2003). The aim of the measure is to consider similar patients in the calculation; they are all close to death. In the data used below, area rankings of treatment intensity are similar regardless of whether or not they are restricted to end-of-life care. This suggests that end-of-life spending is informative of intensity in general, but also calls into question whether the spending measure is unrelated to treatment decisions for those not close to death.
The main sources of potential bias in estimating equation (1) are due to omitted variables and sample selection. The usual concern in cross-sectional studies is that people who live in different places may differ from one another in ways that can confound estimates. Empirically, patients who receive higher treatment levels have substantially higher mortality rates, even after controlling for observable patient characteristics. Abstracting from iatrogenic effects, this implies that additional care is provided to patients in worse health. When the treatment measure is aggregated, areas with patients in worse health may spend more on patients, which would bias the estimate of β1 upward.4 In contrast, areas that provide greater treatment intensity may admit more patients to the hospital, resulting in healthier patients at the margin and a downward bias.
A key question in health economics considers where the variation in healthcare spending across areas originates. Previous work highlights provider preferences as the remaining explanation (for summaries, see Gold (2004) and Congressional Budget Office (2008)). For example, a number of studies show that greater capacity for care is associated with greater usage, although capacity may be a result of the interaction of both supply and demand factors. Furthermore, observable patient characteristics do not appear to be related to area spending levels (Pilote et al. 1995; O’Connor et al., 1999; Phelps, 2000; Stukel, Fisher et al., 2003; Lucas, and Wennberg, 2005). In particular, areas with higher Medicare spending are not wealthier areas, although they do tend to be more urban. A remaining question is whether geographic variation in spending is associated with the unobserved health characteristics.
This paper attempts to circumvent these concerns by estimating equation (1) for a group of visitors. Visitors are unlikely to impact the treatment intensity policy and practice in their destinations. In the episodes analyzed below, for example, visitors constitute only 5% of the cases. Further, if the incidents were truly shocks, then healthcare intensity in the area would not enter into the travel decision. This should ameliorate the selection bias caused by greater treatment provided to populations in worse health, as the bias disappears when the treatment level in the area is not associated with a group’s gain (Bjorklund and Moffitt, 1987, Heckman, Lalonde, and Smith, 1999). Last, in the extreme of a discrete choice between perfect substitutes, the destination choice may approximate a random assignment, and the treatment intensity of the hospital system in the tourist destinations would be exogenous.
Previous evidence also provides support for the use of visitors as participants in a natural experiment. Visitors with a health shock in an area that tends to spend relatively more on locals should also receive relatively more care compared to visitors in areas that spend less. For example, Fisher et al. (1994) and Stukel, Lucas and Wennberg (2005) demonstrate that treatment intensity in an area tends to be similar across patients in the area. It appears that high-spending areas have a lower short-run marginal cost of providing state-of-the-art treatment following previous investments physical and human capital. Last, the lack of a relationship between area income and healthcare spending intensity suggests that other amenities in high-spending areas are less likely to attract particular types of visitors.
3. Data Description
The patient-level data represent the universe of hospital discharges in the state of Florida from 1996 to 2003. These reports are submitted to the Florida Agency for Healthcare Administration and are available for research purposes. Florida offers three main advantages: it is a top travel destination state, which allows for large samples of visitors; the state provides detailed discharge data; and there is a great deal of variation in spending across the state. Florida has been noted to have large geographic variation in spending, with especially large spending levels in South Florida (Fuchs, 2003, Skinner and Wennberg, 2003). These differences are attributed to differing attitudes about health and healthcare among patients and providers in ways that are difficult to separate, as well as a smaller influence from HMOs in the area (Bertko, 2003).
Available data elements include the patient’s age, race, sex, and ZIP code of residence. Visitors are defined as an out-of-state patient. Procedure and diagnosis codes, primary payer, day of the week, and quarter of the year also describe the episode. To focus on health shocks rather than planned travel for healthcare, the analysis is restricted to patients who are admitted into the hospital from the emergency room with an admission type of “emergency”. Hospital markets are defined at the level of the Health Service Area (HSA), defined by the Dartmouth Atlas of Healthcare. These areas typically encompass one or two hospitals whose acute-care patients come from similar ZIP codes: areas that appear appropriate for the health shocks employed here.
The main measure of resource use is total costs reported in the discharge summary, which is the sum of the list prices for each of the services provided deflated by a cost-to-charge ratio calculated by the Centers for Medicare and Medicaid at the hospital-year level.5
The end-of-life spending measure was calculated as the mean of log costs in the HSA among patients from Florida who were admitted on an emergency basis and who died in the hospital. The mean is weighted by the fraction of visitors who visit each hospital in an HSA to reflect the exposure to spending levels across visitors (similar results are found without these weights). Algebraically, this measure is the HSA fixed effect in a model predicting end-of-life log costs for this sample of locals, weighted by each hospital’s visitor share in the HSA.
The health outcome available in the discharge data is inpatient mortality. While this is a frequent and important outcome, it does not allow an examination of long-run mortality effects. 6 That said, for the visitor group inpatient mortality is tied more directly to the acute care provided by Florida healthcare systems, whereas long-term outcomes may be influenced by the care received once the patient returns home. In addition, an advantage of the discharge data compared to previous studies that use Medicare administrative data is that younger patients can be compared, as well as patients enrolled in Medicare HMOs who are generally not included in Medicare expenditure files.
U.S. Census data from 2000 are used to describe the patient’s ZIP code of residence, including the seven median household income categories, median rent, racial composition, educational composition among individuals older than 25-years old, and the percent rural. One issue is that visitors who are not from the U.S. do not have a ZIP code. In addition, the Census Bureau does not publish data for small ZIP codes due to confidentiality concerns (especially income categories). In total, ZIP code information is missing for 16% of the visitor sample. The main results will retain these observations by filling in the missing information with sample means and including an indicator for missing ZIP code information in the model. Results are similar when these observations are excluded, as shown below. Similar U.S. Census measures for the destination county in Florida are used in some specifications as well.
Prices faced by visitors in particular are used to categorize counties in Florida. These prices come in the form of per-diem rates calculated by the U.S. General Services Administration (GSA) and are based on lodging and meal prices in each county. Given the seasonal variation in these rates, two measures are used: the per diem for January and June.7 Each measure should reflect local-area cost structures, and the difference in the two measures should identify areas that are desirable for winter vacations. Results will be reported with and without these controls.
The 1995 American Travel Survey describes visitors to each of 13 metropolitan areas. These data are used in a specification check that controls for these characteristics on this subset of cities. Last, American Hospital Association data that provide detailed information about each hospital in Florida are used to describe the different areas in terms of staffing ratios.
Main Analysis Sample
The main analysis focuses on common heart-related emergencies: patients who are admitted with a primary diagnosis of acute myocardial infarction (AMI), cardiac dysrhythmias, or heart failure.8 These are among the top-10 diagnoses for emergency admissions with a mortality rate over 3%. They hold the potential to represent health shocks where the patient is less likely to investigate the healthcare spending in the area prior to choosing the destination.9
The sample is restricted to HSAs with at least 30 visitors with a heart-related emergency, for a total of 97. The sample is further limited to visitors from U.S. states with at least five observations or visitors from outside the U.S. to allow comparisons of patients from the same state who travel to different tourist destinations. The sample includes over 37,000 hospitalizations for patients whose residence is outside the state of Florida, representing 5% of heart-related emergency admissions in Florida.
Comparison of Health Service Areas
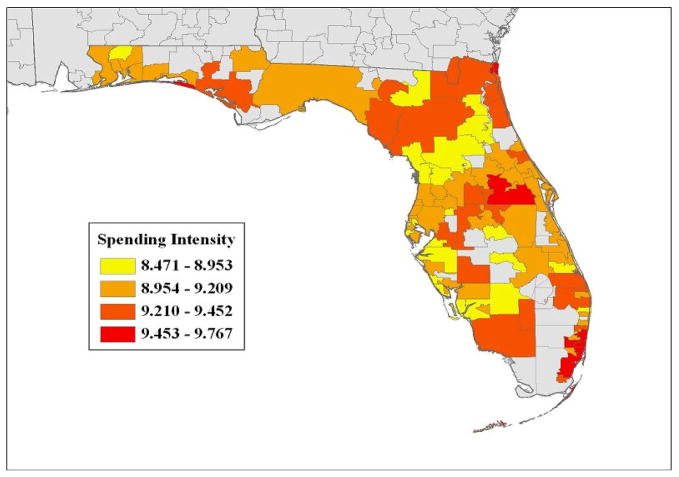
To describe the data further and compare visitors with local patients who had a heart-related emergency across different areas in Florida, Figures 1–4 and Table 1 demonstrate how high-spending areas differ from low-spending ones.
Figure 1.
97 Health Service Areas in Florida
Figure 4.
Age vs. HSA Cost Rank
Table 1.
Selected Characteristics, by Quartile of Spending Intensity
| Patient Group: | Local Floridians | Visitors | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Q1 | Q2 | Q3 | Q4 | Q1 | Q2 | Q3 | Q4 | ||
|
|
|
||||||||
| Area-level | |||||||||
| Intensity Proxy: mean log(costs) | mortality | 8.90 | 9.12* | 9.31* | 9.57* | 8.89 | 9.11* | 9.31* | 9.56* | |
|
|
|||||||||
| Outcome | Mortality | 0.058 | 0.061 | 0.052* | 0.055 | 0.070 | 0.064 | 0.048* | 0.049* |
|
|
|||||||||
| Personal Characteristics | Male | 0.526 | 0.518 | 0.521 | 0.511 | 0.624 | 0.605 | 0.63 | 0.634 |
| Age | 73.5 | 72.4 | 71.3* | 70.4* | 72.5 | 71.2 | 70.1 | 67.0* | |
| White | 0.913 | 0.849* | 0.755 | 0.535* | 0.966 | 0.925* | 0.938 | 0.745* | |
|
|
|||||||||
| ZIP Code of Residence | Median HH Income | 36825 | 38531 | 38792 | 38123 | 47357 | 46572 | 49994 | 45527 |
| Percent White | 0.864 | 0.813* | 0.801* | 0.682* | 0.874 | 0.838* | 0.852 | 0.785* | |
| Percent >65 years old | 0.273 | 0.221* | 0.190* | 0.151* | 0.140 | 0.143 | 0.141 | 0.135 | |
| Percent No HS Degree | 0.198 | 0.188 | 0.226 | 0.260 | 0.161 | 0.173 | 0.158 | 0.186* | |
| Percent Rural | 0.151 | 0.090 | 0.140 | 0.028 | 0.304 | 0.302 | 0.244 | 0.235 | |
|
|
|||||||||
| Payer Categories | Medicare | 0.652 | 0.616 | 0.577 | 0.439* | 0.672 | 0.627 | 0.606 | 0.441* |
| Medicare HMO | 0.126 | 0.124 | 0.111 | 0.186 | 0.053 | 0.043 | 0.045 | 0.045 | |
| Medicaid | 0.026 | 0.035 | 0.052* | 0.070* | 0.006 | 0.012* | 0.009 | 0.022* | |
| Private Insurance | 0.148 | 0.172* | 0.198* | 0.227* | 0.220 | 0.263* | 0.297* | 0.351* | |
|
|
|||||||||
| Comorbidities | No Comorbidities | 0.313 | 0.319 | 0.330* | 0.355* | 0.386 | 0.380 | 0.413 | 0.439* |
| Prior AMI | 0.133 | 0.117 | 0.109* | 0.095* | 0.144 | 0.132 | 0.135 | 0.100* | |
| Congestive Heart Failure | 0.174 | 0.162 | 0.147* | 0.142* | 0.170 | 0.161 | 0.149* | 0.165 | |
| Chronic Obstructive Pulmonary Disease | 0.288 | 0.285 | 0.287 | 0.246* | 0.212 | 0.216 | 0.201 | 0.175* | |
| Diabetes | 0.237 | 0.240 | 0.252 | 0.263* | 0.200 | 0.213 | 0.198 | 0.211 | |
|
|
|||||||||
| Timing | 1st Quarter | 0.286 | 0.278 | 0.270* | 0.266* | 0.522 | 0.458 | 0.498 | 0.399* |
| Weekend | 0.281 | 0.277 | 0.272* | 0.266* | 0.286 | 0.283 | 0.281 | 0.293 | |
|
|
|||||||||
| Area | Per-diem in January | 111 | 119 | 119 | 127* | 109 | 118 | 124 | 127* |
| Prices | Per-diem in July | 99 | 107 | 105 | 115* | 96 | 106* | 102 | 116* |
| Observations | 169575 | 216209 | 144681 | 219297 | 8436 | 10149 | 9655 | 8945 | |
=significantly different from bottom quartile at the 5% level, computed using standard errors clustered at the Health Service Area level. ZIP code characteristics reported for those with ZIP code information.
Figure 1 shows a map of Florida where the 97 HSAs are located, and four quartiles of the end-of-life cost measure are shown. The higher-spending areas are distributed across the state. Perhaps the most striking variation is along the eastern coast, where all four quartiles are represented in popular destination areas.
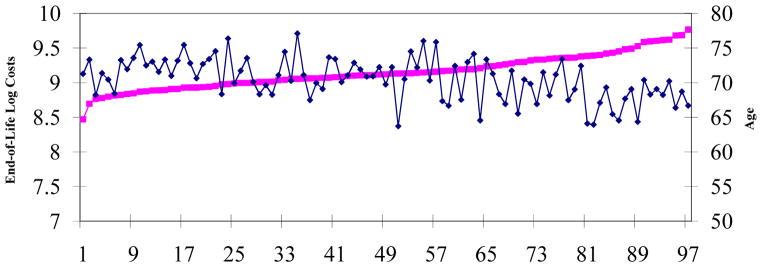
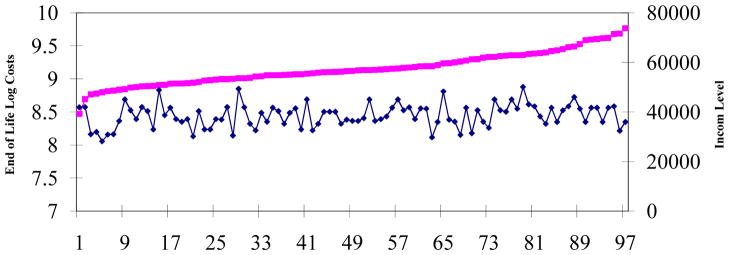
To investigate whether high-cost healthcare markets are more expensive areas in general that happen to attract wealthier (and healthier) visitors, Figures 2 and 3 consider median income levels of the Florida counties and the visiting patients’ ZIP codes. The x-axis in each Figure is the rank of the area in terms of end-of-life spending. The graphs show that while the spending measure increases with its rank, the income measures are not related to it. It does not appear that high-spending areas reflect the income level of residents or travelers.
Figure 2.
Florida County Median HH Income vs. HSA Cost Rank
Figure 3.
ZIP Code Median HH Income vs. HSA Cost Rank
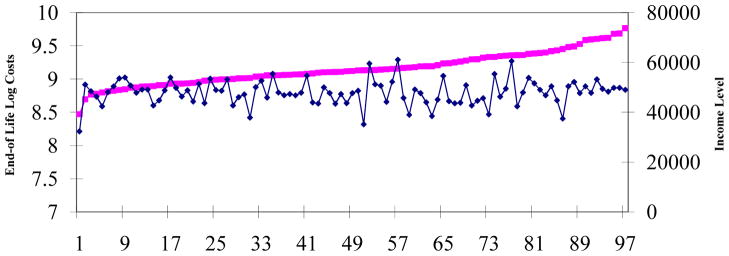
Figure 4 is similar to Figure 3, but reports the average age of the visitors. Age is relatively unrelated to hospital spending for most of the spending distribution. A noticeable decline in age is seen for the top 17 HSAs, where 30% of the visiting patients are found. These areas are more urban, including HSAs in Miami. This decline in age is an important limitation, as age is a strong predictor of mortality, and it is addressed in three ways. First, the analysis flexibly controls for age with indicators for each year of age. Second, results are shown separately by age group. Third, the results are shown to be robust when patients found in these highest-cost HSAs are excluded from the analysis: a subset of HSAs that is shown to have similar observable characteristics (including age) regardless of the healthcare spending level.
Table 1 reports means of the patient characteristics for both local Floridians and visitors.10 The HSAs were divided into quartiles based on the end-of-life spending measure: the first row shows that HSAs in the top quartile have mean end-of-life costs that are over 65 log points (or $7000) greater than the average HSA in the bottom quartile. The next row shows that mortality is lower in the top two quartiles, with an especially steep decline among visitors. As shown in Figure 4, part of this decrease is found in the highest-spending HSAs have somewhat lower average ages. The overall mortality rate is similar between the visitors and locals (5.8% vs. 5.7%), which suggests that results for the visitor group may be informative of returns to spending for the local group as well.
As in the previous cross-sectional evidence, Table 1 shows that patients’ observable characteristics are fairly similar regardless of the spending intensity of the area, at least for the bottom three quartiles. The top quartile, which includes Miami, shows greater differences. The best case in favor of using visitors instead of locals to compare relatively similar patients across markets is in terms of race, where approximately 95% of visitors are white across the bottom three quartiles of spending intensity, falling to 75% in the top quartile. Among locals, these percentages fall across the quartiles (from bottom to top they are 91%, 85%, 76%, and 54%). Income levels of the ZIP codes where the locals and the visitors reside are similar, as in the figures described above. Meanwhile, the younger ages of patients in the top quartile lead to lower Medicare coverage rates and somewhat lower rates of comorbidity. These differences motivate investigation of the main results within subgroups of patients, defined by these characteristics.
Table 1 also shows that locals differ from visitors regardless of the HSA spending level in several ways. Visitors with heart-related emergencies are more likely to be male compared to locals (62% vs. 52%), they are more likely to live in rural areas, and are more likely to be found in the popular travel time of the first quarter of the year.11
In terms of the areas, the per-diem rates are higher for the larger urban areas that comprise higher-spending areas. The analysis controls for these lodging prices and also compares results within destinations with similar lodging prices.12 In addition, the American Travel Survey (ATS) provides summaries of the types of visitors and trips to Florida. While the ATS limits the analysis to 13 metropolitan areas, the evidence suggests that visitors are generally similar across these cities, including the reason for travel and income measures (see Appendix Table A2).13
4. Results
4A. Main Estimates
Following the framework in Section 2, the empirical models consider the outcome of inpatient mortality, M, for patient i hospitalized in the geographic area (defined by the HSA) g, within Florida county c, from ZIP code z in state s, in year t as:
| (3) |
T is the measure of local-area, end-of-life spending in the HSA visited by patient i, as described above; X is a vector of personal characteristics listed in Table 1 with indicators for each age, admission day of the week, an indicator that the patient is white interacted with 5-year age categories, and three-digit diagnosis indicators; W is the set of ZIP code of residence characteristics described above; and P is the vector of county per-diem rates in January and June.14 Home-state fixed effects are used to compare individuals from the same state who visit different HSAs in Florida, and year indicators are used to capture overall changes in survival rates over time.15 The outcome is binary, and the results are shown using a linear probability model to estimate differences in means across HSAs. Results are similar when a probit model is used, as shown below. The standard errors are clustered at the HSA level to reflect variation in the local-area spending measure.
The top panel of Table 2 reports results for the local Florida population. The first two columns show results from a model similar to (3), but with costs accrued by a particular patient, Ti, instead of the local-area treatment measure, Tg(i). Column (1) reports a coefficient of 0.025. The interquartile range of log costs among the local population is 113 log points. The estimated coefficient suggests that such a difference in costs is associated with a 2.8 percentage-point increase in mortality, or nearly 50% of the mean. When the controls are employed, the coefficient decreases to a 0.13 percentage-point increase in mortality. These results are consistent with the hypothesis that more is spent on patients who are in worse health in ways that are not controlled.
Table 2.
Treatment & Health Outcomes for Heart-Related Emergencies
| A. Florida Locals | ||||||
|---|---|---|---|---|---|---|
| Dependent Variable: Mortality | ||||||
| (1) | (2) | (3) | (4) | (5) | (6) | |
|
|
||||||
| log(costs) | 0.025 (0.0020) | 0.013 (0.0020) | ||||
|
|
||||||
| Local area: mean log(costs) | mortality | −0.0061 (0.0043) | 0.0048 (0.0038) | −0.0020 (0.0037) | −0.0030 (0.0039) | ||
|
|
||||||
| Controls for Personal Characteristics | No | Yes | No | Yes | Yes | Yes |
| Controls for Patient ZIP Code Characteristics | No | Yes | No | No | Yes | Yes |
| Controls for Area Prices | No | Yes | No | No | No | Yes |
|
| ||||||
| Observations | 749762 | |||||
| Mean of Dep. Variable | 0.057 | |||||
|
| ||||||
| B. Visitors | ||||||
| Dependent Variable: Mortality | ||||||
| (1) | (2) | (3) | (4) | (5) | (6) | |
|
|
||||||
| log(Costs) | 0.025 (0.0025) | 0.012 (0.0024) | ||||
|
|
||||||
| Local area: mean log(costs) | mortality | −0.035 (0.0094) | −0.029 (0.0082) | −0.028 (0.0081) | -0.028 (0.0082) | ||
|
|
||||||
| Controls for Personal Characteristics | No | Yes | No | Yes | Yes | Yes |
| Controls for Patient ZIP Code Characteristics | No | Yes | No | No | Yes | Yes |
| Controls for Area Prices | No | Yes | No | No | No | Yes |
|
|
||||||
| Observations | 37185 | |||||
| Mean of Dependent Variable | 0.058 | |||||
The models are estimated by OLS and the standard errors are clustered at the Health Service Area level. Personal characteristics include the variables in Table A3, as well as indicators for each age, 5-year age indicators interacted with the white indicator, day of the week, and home state.
When the mean end-of-life spending measure for the HSA, Tg(i), is used to compare healthcare systems, mortality is unrelated to the spending level in the HSA among Florida locals. The coefficient on HSA spending intensity ranges from −0.002 to 0.005 with standard errors on the order of 0.004. These results match findings in the prior literature that higher spending is associated with small, statistically-insignificant differences in mortality.
Panel B shows results using the sample of visitors. The first two columns show nearly identical coefficients as in the Florida sample, which is consistent with providers taking observable factors such as age and comorbidity into account in a similar manner when making treatment decisions, regardless of whether the patient is a visitor or a local. Columns (3)-(6) show that contrary to the previously established result for locals, end-of-life spending is strongly negatively related to mortality, with a coefficient closer to -0.028. A 2 standard deviation increase in spending intensity of roughly 50% is associated with mortality rates that are 1.4 percentage points lower, or 24% lower than the mean.
For context, the estimated coefficients for the control variables are shown in Appendix Table A3. Patients with comorbidities and older patients have higher mortality rates, with 85 year olds having a 4 percentage-point higher mortality rate than 60 year olds, conditional on the other controls. Visitors in the 1st quarter have a one percentage-point lower mortality rate compared visitors at other times of the year. The uninsured have a 1 to 3 percentage-point higher mortality rate compared to insured patients. Meanwhile, the ZIP code characteristics tended not to be related to mortality, most notably the fraction rural—a characteristic that differed between the visitors and locals.
To test the shape of the relationship between local-area costs and mortality, a model that included indicators for the HSA quartiles (described in Table 1) were used rather than the level of the end-of-life spending measure. The bottom quartile appears to have higher mortality rates, with the second least expensive quartile showing a 0.8 percentage-point lower mortality rate and the top two quartiles each showing a 1.7–1.8 percentage-point reduction in mortality. This suggests that the effectiveness of spending intensity may fade for the most expensive areas, although some caution is warranted in the interpretation given that the top quartile appeared somewhat different from the bottom three in Table 1.16
4B. Robustness
The main results suggest that more expensive healthcare systems do achieve lower inpatient mortality rates among visitors, but alternative explanations include the possibility that high-spending areas attract healthier patients, areas that provide better care for heart-related emergencies happen to be high-spending areas overall but not necessarily for cardiac care, or that high-spending areas admit healthier patients into the hospital. The remaining sets of results consider these explanations by estimating the model within similar groups of patients and within similar groups of destinations—areas that are more likely to attract similar patients; considering a wider set of diagnoses; and providing additional evidence on the potential role of sample selection bias.
Patient Characteristics
Section 3 makes clear that there are differences among the patients across the areas. To consider whether these differences are responsible for the main results, and begin to investigate heterogeneous treatment effects, Table 3 explores the robustness of the results across subgroups of patients.
Table 3.
Heart-Related Emergency Results Across Patient Types
| Dependent Variable: Mortality | |||||
|---|---|---|---|---|---|
| A. Age & Business Travelers | Business Destinations:
|
||||
| Age>=65 | Age<65 | Age <65 | Age<65 & Privately Insured | Age <65 & Privately Insured & Quarter 2–4 | |
| (1) | (2) | (3) | (4) | (5) | |
| Local area: mean log(costs) | mortality | −0.036 (0.011) | −0.019 (0.008) | −0.023 (0.013) | −0.034 (0.012) | −0.032 (0.014) |
|
|
|||||
| Observations | 26614 | 10571 | 4722 | 2946 | 1841 |
| Mean of Dep. Var. | 0.068 | 0.033 | 0.037 | 0.036 | 0.035 |
| B. Patient Income Level | ZIP Code Income Quartile
|
ZIP Code Fixed Effects | |||
|---|---|---|---|---|---|
| Bottom | 2nd Quartile | 3rd Quartile | Top | ||
| (6) | (7) | (8) | (9) | (10) | |
| Local area: mean log(costs) | mortality | −0.031 (0.013) | −0.029 (0.016) | −0.025 (0.015) | −0.049 (0.012) | −0.022 (0.010) |
|
|
|||||
| Observations | 7840 | 7848 | 7861 | 7839 | 27356 |
| Mean of Dep. Var. | 0.054 | 0.058 | 0.057 | 0.066 | 0.059 |
| C. Comorbidities | Charlson Index
|
||
|---|---|---|---|
| None | Index = 1 | Index = 2 | |
| (11) | (12) | (13) | |
| Local area: mean log(costs) | mortality | −0.017 (0.009) | −0.039 (0.013) | −0.041 (0.015) |
|
|
|||
| Observations | 15050 | 12764 | 9371 |
| Mean of Dep. Var. | 0.032 | 0.066 | 0.087 |
| D. Quarter of Year | 1st Quarter | 2nd Quarter | 3rd Quarter | 4th Quarter |
|---|---|---|---|---|
| (14) | (15) | (16) | (17) | |
| Local area: mean log(costs) | mortality | −0.024 (0.009) | −0.036 (0.015) | −0.042 (0.018) | −0.035 (0.018) |
| 17439 | 7816 | 4437 | 7493 | |
|
|
||||
| Mean of Dep. Var. | 0.051 | 0.069 | 0.063 | 0.060 |
| E. Top 100 Diagnoses: By Illness Severity | All | P(Mortality|Diagnosis) Quartiles
|
|||
|---|---|---|---|---|---|
| Bottom | 2nd | 3rd | Top | ||
| (18) | (19) | (20) | (21) | (22) | |
| Local area: mean log(costs) | mortality | −0.012 (0.0050)** | 0.0003 (0.0008) | −0.0028 (0.0025) | −0.016 (0.007)** | −0.030 (0.014)** |
|
|
|||||
| Observations | 229110 | 0.002 | 0.011 | 0.034 | 0.118 |
| Mean of Dep. Var. | 0.039 | 57388 | 60335 | 59869 | 51505 |
Each cell represents a separate regression with full controls, including diagnosis fixed effects. The models are estimated by OLS and the standard errors are clustered at the Health Service Area level. Business destinations include the cities where the fraction of visitors whose reason for travel is business in the 1995 American Travel Survey is greater than the median city. ZIP code fixed effects models are estimated for patients with non-missing ZIP code information.
Panel A considers the age and location of the patient. The over-65 group is mostly covered by Medicare (with the exception of foreign visitors). The first two columns show that the results are similar when the group is either older or younger than 65 years old: a 10% increase in end-of-life spending is associated with a 0.36 percentage-point decline in mortality among the 65+ group, or 5.2% of the mean, and such an increase is associated with a 0.19 percentage-point decline in mortality among the younger group available in these hospital discharge data, or 5.8% of its mean.
The next three columns compare the results for patients who are increasingly likely to be business travelers. Business travelers have the advantage of being even less likely to choose the destination based upon its healthcare spending practices. First, the ATS was used to categorize metropolitan areas as business travel destinations. The sample was then divided into two groups based on the median rate of business travel.17 Column (3) shows that for travelers under the age of 65 in these destinations, the coefficient is similar to under-65 subgroup overall, with a coefficient of −0.023. When privately insured individuals are considered, largely dropping those who qualify for disability claims and thereby not likely to be business travelers, the magnitude of the coefficient increases to −0.034. Last, when the first quarter is dropped—the most popular quarter for leisure travel—the coefficient is again qualitatively similar: −0.032. The sample size decreases from 10,571 for all patients under the age of 65 to 1,841 for the most refined category of patients most likely to be business travelers, yet the estimate increases in magnitude.
One concern is that high spending areas will attract wealthier (and healthier) patients. Panel B shows that the results are similar across ZIP code income levels, as well as when the main estimating model includes ZIP code fixed effects. Panel C shows that the results are similar regardless of the comorbidity level, as defined by the Charlson severity index that takes on values of 0, 1, and 2 (Quan et al., 2005): a 10% increase in spending intensity is associated with mortality reductions of 5.3%, 5.9%, and 4.7% compared to the mean mortality rates for the three groups, respectively. Results are also shown to be similar across the quarters of the year in Panel D. This suggests that the results are not due to “snow birds” who winter in Florida and may take more care in choosing the destination. Appendix Table A4 provides additional evidence of the robustness of the results across patient types, including by sex, race, insurance status, and region of primary residence.
Panel E considers the top 100 emergency diagnoses, where the coefficient on end-of-life spending in the HSA is −0.012 (s.e.=0.0050).18 That is, a 2 standard deviation increase in the spending intensity measure is associated with a 0.6 percentage-point reduction in mortality, or 15% of the mean: similar to the heart-related emergency results. Panel E also shows statistically and economically significant reductions in mortality among diagnoses with higher mortality rates. In the top quartile of mortality rates, a 2 standard deviation increase in the spending measure is associated with a 1.5 percentage-point reduction in mortality (13% of the mean). The comparable figure for the third quartile is 24% of the mean. These results suggest that high-spending areas achieve better health outcomes across a wide range of emergency situations. For further disaggregation, Appendix Table A5 reports results for the top 10 most common emergency diagnoses. In particular, the results are similar for stroke patients, with a coefficient of −0.029 compared to a mortality rate of 6.3%.
Comparison of Close Substitutes in Destinations
As in the comparisons across patient types, HSAs that differ by local-area healthcare spending may differ along a number of other dimensions. These differences may attract different types of visitors and different types of hospital staff. To test whether these HSA differences affect the results, Table 4 reports estimates across subsets of similar destinations.19
Table 4.
Heart-Related Emergency Results Across County Types
| Dependent Variable: Mortality | ||||||
|---|---|---|---|---|---|---|
| Destination Demand Substitutes:
|
Spending Dist’n:Exclude Top 30% of HSAs | |||||
| Visitor Price Quartiles
|
1st Quarter &MLB Spring Training Sites | |||||
| Bottom Quartile | 2nd Quartile | 3rd Quartile | Top Quartile | |||
| (1) | (2) | (3) | (4) | (5) | (6) | |
|
|
||||||
| Local area: mean log(costs) | mortality | −0.039 (0.031) | −0.004 (0.023) | −0.049 (0.024) | −0.026 (0.009) | −0.026 (0.010) | −0.026 (0.013) |
|
|
||||||
| Number of Counties | 17 | 10 | 8 | 9 | 13 | 41 |
| Number of HSAs | 23 | 18 | 18 | 38 | 45 | 80 |
| Observations | 4547 | 6848 | 7293 | 18497 | 8611 | 26360 |
| Mean of Dep. Var. | 0.069 | 0.057 | 0.060 | 0.055 | 0.048 | 0.063 |
Each column represents a separate regression with full controls. The models are estimated by OLS and the standard errors are clustered at the Health Service Area level. Visitor prices are per-diem rates calculated by the US General Services Administration. The bottom quartile represents the counties that do not have their own per-diem rate. Major League Baseball (MLB) Spring Training Sites include the 13 counties with a spring training facility.
If hospital-spending levels do not enter the visitor’s decision to choose a destination, then visitors to areas that are close substitutes are likely to be similar to one another as well. In that spirit, Table 4 reports the results for sub-samples defined by quartiles of the per-diem rates to compare destinations with similar prices. This is a coarse categorization given the 97 HSAs studied, although the measures should serve to distinguish relatively expensive areas from less expensive ones. The bottom quartile represents the 17 counties where the per-diem rate is the state-level rate of $80. These counties tend to be visited less frequently. The next three quartiles have per-diem rates that range from $80–99, $100–116, and $117–214, respectively.20 The bulk of the data reside in the top quartile, which also includes Miami, Fort Lauderdale, West Palm Beach, and Tampa Bay. The results are fairly robust across the groups, with the second quartile being one of the few subgroups where no relationship is found.21 That is, the main results are found in popular destinations, even within areas with similar lodging prices.
A related approach considers Spring Training sites for Major League Baseball, where teams train during February and March. The advantage of focusing on these areas is that they tend to be similarly sized cities that attract similar visitors as well. Appendix Table A6 shows that high- and low-spending areas that host the teams are similar in terms of patient age, race, sex, comorbidity levels, and especially lodging and meal prices. Column (5) shows that the result is similar when the analysis focuses on these 13 counties during the first quarter of the year, with an estimated coefficient on local-area, end-of-life spending of −0.026 (s.e. = 0.010).
Recall from Figure 4 that the most expensive HSAs tend to have younger patients, especially for the top 17 HSAs where 30% of the patients are found. When these HSAs were excluded, the observable characteristics are quite similar (see Appendix Table A6), as are the main estimates of interest. The main results do not appear to be due to high-spending areas attracting the youngest, and perhaps healthiest, patients. Last, results were similar when Census data were used to control for characteristics of the destination county and when American Travel Survey data were used to control for characteristics of the typical visitors (Appendix Table A4).
Sample Selection Bias
The hospital discharge data include only patients who were admitted to the hospital. A number of selection biases could result in estimates of returns to healthcare spending that are too large or too small. One explanation for the lower mortality rates in high-spending areas is that these areas may admit healthier patients.22 The focus on health shocks, such as heart attacks (and strokes and hip fractures reported in the Appendix), as well as the similarity of the results for patients with increasing levels of comorbidity shown in Table 3, suggests that the estimates are similar as the probability of admission is approaches 1—where the effects would be identified “at infinity”. In addition, rough estimates of admission rates, and in-hospital death rates as opposed to outside of the hospital, do not appear to be systematically related to area-spending levels, especially among the visitors.23
A number of other robustness checks were carried out as well as those presented above (shown in the Appendix Tables 7–8). For example, the results were similar when the model was estimated using a probit specification and across alternative measures of area-level spending intensity.
5. Interpretation
A. Mechanisms: Treatment Differences Across HSAs
As described in Section 2, a large medical literature describes the types of services provided in high- vs. low-spending areas. The Dartmouth Atlas of Healthcare also shows that surgical interventions are correlated with end-of-life spending (a correlation close to 0.25), and a higher correlation (close to 0.5) with intensive care unit services.24 Meanwhile, differences in prices account for less than 30% of the variation in expenditures.
To compare different types of treatment in the current data and population studied, Table 5 reports results separately for AMI patients, as well as all heart-related emergency patients. Panel A of Table 5 considers spending at the patient level, which is shown to be strongly associated with the spending intensity proxy for the area. In particular, the summary measure of total costs averages $16,400 (in 2003 dollars) for AMI emergency visitors, and a 2 standard deviation increase in area-spending intensity is associated with a $5,840 increase in total costs at the patient level.
Table 5.
Mechanisms
| AMI Emergencies
|
All Heart-Related Emergencies
|
|||||
|---|---|---|---|---|---|---|
| Dependent Variable: | Mean of Dep. Var. | Coeff on Area Intensity | S.E. | Mean of Dep. Var. | Coeff on Area Intensity | S.E. |
| A. Types of hospital costs | ||||||
| Total | 16438 | 11679 | (3080)** | 11557 | 8106 | (1650)** |
| ICU & CCU | 2092 | 2239 | (622)** | 1471 | 1498 | (409)** |
| Diagnostic | 2520 | 1783 | (312)** | 2107 | 1356 | (239)** |
| Surgical | 3924 | 1058 | (1090) | 2201 | 838 | (563) |
| Remaining | 7902 | 6599 | (1540)** | 5778 | 4414 | (835)** |
|
|
|
|||||
| B. Indicator for Top 10 Most Frequent Procedures Among Local AMI Patients | ||||||
| 37.2 Dx procedures on heart and pericardium (catheterization) | 0.54 | 0.155 | (0.129) | 0.28 | 0.099 | (0.069) |
| 88.5 Angiocardiography (catheterization) | 0.52 | 0.156 | (0.134) | 0.26 | 0.093 | (0.067) |
| 36.0 Stent(s) | 0.25 | 0.148 | (0.105) | 0.10 | 0.066 | (0.046) |
| 99.2 Injection prophylactic substance (platelet inhibitor) | 0.15 | 0.057 | (0.046) | 0.06 | 0.02 | (0.020) |
| 96.7 Other continuous mechanical ventilation | 0.11 | 0.007 | (0.016) | 0.07 | 0.010 | (0.011) |
| 36.1 Bypass anastomosis for heart revascularization | 0.10 | 0.110 | (0.060)* | 0.04 | 0.050 | (0.028)* |
| 39.6 Extracorporeal circulation | 0.08 | 0.082 | (0.058) | 0.04 | 0.038 | (0.027) |
| 96.0 Nonoperative intubation of gastrointestinal and respiratory tracts | 0.08 | −0.011 | (0.012) | 0.06 | 0.001 | (0.010) |
| 88.4 Arteriography using contrast material | 0.06 | −0.062 | (0.042) | 0.03 | −0.031 | (0.022) |
| 99.1 Injection prophylactic substance (excludes aspirin) | 0.06 | −0.05 | (0.025)** | 0.02 | −0.021 | (0.011)* |
|
|
|
|||||
| C. Additional Measures of Inputs | ||||||
| Patient treated in Teaching Hospital | 0.09 | 0.36 | (0.163)** | 0.073 | 0.288 | (0.140)** |
| log(Length of Stay) | 1.40 | 0.39 | (0.142)*** | 1.250 | 0.227 | (0.092)** |
| American Hospital Assn: FTE Nurses per 1000 admissions | 27.1 | 9.6 | (3.07)*** | 27.3 | 11.4 | (2.88)*** |
| American Hospital Assn: FTE Total Staff per 1000 admissions | 94.9 | 43.9 | (11.5)*** | 95.9 | 51.7 | (10.6)*** |
|
|
|
|||||
| Mean of Area Spending Intensity Proxy | 9.23 | 9.22 | ||||
| Standard Deviation of Proxy | 0.25 | 0.25 | ||||
| Observations | 15069 | 37185 | ||||
Each coefficient is from a separate regression with full controls. The models are estimated by OLS and the standard errors are clustered at the Health Service Area level. Costs are measured by charges deflated by a cost-to-charge ratio at the hospital x year level and expressed in 2003 dollars. American Hospital Association rows have 37038 and 15034 observations due to missing AHA data.
=10%;
=5%;
=1%.
The types of care provided can also be described by revenue categories available in the discharge data, such as charges for intensive care units or diagnostic tests. One caveat is that these revenue codes may be treated differently across hospitals (and, therefore, across HSAs), and the results should be taken with caution. For comparability to the main results, these categories of charges have been deflated by the hospital’s cost-to-charge ratio in the year of admission. Four representative categories of costs are shown in Table 5: intensive care services, diagnostic services, surgical costs, and other costs (see Appendix Table A9 for each cost category separately). The strongest relationship between patient costs and the local-area spending intensity proxy is found for intensive care services, followed by diagnostic services, and then surgical care. To place the cost categories on the same log scale (dropping patients with zero costs), for AMI patients the coefficient on log(total costs) is 0.61 compared to 0.84 for log(icu costs), 0.65 for log(diagnostic costs), and 0.38 for log(surgical costs).25 This strong relationship between area spending intensity and the use of intensive care units suggests that such care is a driver of the improved outcomes, which is consistent with prior research that intensive care units are associated with significantly higher costs and significantly survival rates as well (Ridley and Morris, 2007).26
Procedure Differences
Third, the main results focus on patient with heart-related emergencies, and an issue when comparing outcomes after heart attacks is that recent evidence suggests that low-cost treatments, such as the use of beta blockers, yield large benefits (Phillips et al., 2000; Heidenreich and McClellan, 2001; Stukel et al., 2005). Results are similar when areas are characterized according to their heart-related-emergency end-of-life spending, however (Appendix Table A7). In addition, to consider quantities of care rather than costs, Panel B shows procedure rates for visitors. Estimates are reported from models that regress an indicator that a common procedure is conducted on the end-of-life spending measure and full controls. The top-10 most frequent three-digit ICD-9 procedures for AMI patients in these data are shown, and high-spending areas generally have higher procedure rates. A 2 standard deviation increase in the spending measure is 0.5, and such a difference is associated with an 8 percentage-point increase in catheterization procedures, compared to a mean of just over 50%; a 7 percentage-point increase in the likelihood of the insertion of a stent, compared to a mean of 25%; and a 6 percentage-point increase in the bypass rate, compared to a mean of only 10%. Similar differences are found for all heart-related emergencies as well.
These estimates tend to be imprecisely measured, however, which is partly due to the disaggregation of procedures. Among the top 25 procedures (not shown), 20 are more common in high-spending areas. Those that are more common in low-spending areas tend to be lower-cost procedures. For example, arteriography is a lower-cost substitute for angiocardiography, and ateriography is more common in low-cost areas whereas angiocardiography is more common in high-cost areas. Taken together, it appears that higher-spending areas do provide a greater quantity of services.
One caveat is that the positive association with surgical intensity, both in terms of costs and quantities, suggests that the inpatient mortality differences may be understated. Surgery carries its own in-hospital mortality risk. Physicians and patients must weigh this risk against potential longer-term benefits.27
Differences in Input Measures Across HSAs
A further exploration of the variation in the types of services provided is shown in Panel C. First, patients who have a medical emergency in a high-spending area are much more likely to be treated in a teaching hospital. A comparison of teaching hospitals and non-teaching hospitals is similar to the main question in this paper of whether a bundle of characteristics associated with higher costs are associated with lower mortality. For example, Taylor et al. (1999) found that teaching hospitals have 20–50% higher costs compared to for-profit and government hospitals, and also had a 25% lower mortality rate overall.28 In fact, a model similar to equation (3), but with mortality regressed on an indicator that the hospital was a teaching hospital reveals lower mortality for these visiting patients (coefficient=−0.013, s.e.=0.006).29 Notably, this result is not found for local patients. These results are consistent with plausibly exogenous exposure to teaching hospitals among visitors but less so among locals who chose to settle in the area permanently and are more likely to know the quality of the hospitals.
Another summary measure of resource use that is related to costs but more straightforward to measure across markets is the length of stay in the hospital. Areas with greater end-of-life treatment intensity are associated with longer stays in the hospital. Among visitors, a 2 standard deviation increase in the spending proxy is associated with a 19 log point longer length of stay for AMI patients and 11 log point longer length of stay for all heart-related emergency patients.30
Last, human capital measures of the staff may explain differences in treatment intensity, possibly due to differences in the quality of care or training styles. While quality measures are part of ongoing research, the number of nurses and staff for each hospital is available from the American Hospital Association (AHA). For each HSA, a staff-to-admission ratio was calculated for the year 2000, weighting each hospital by the number of admissions reported in the AHA data. 31 Table 5 shows that a 2 standard deviation increase in the spending-intensity proxy is associated with a 23% increase in the staff-to patient ratio compared to its mean, and an 18% higher nurse-to-admission ratio.
Locals vs. Visitors
It would be useful to demonstrate why the results differ between the locals and the visitors. As noted above, the result for locals replicates what has been found many times before in the medical literature, including the relative similarity of the observable characteristics across areas. A number of tests were considered to explain the difference, but only suggestive evidence is found that the negative relationship between spending and mortality can be found once selection or other patient characteristics are taken into account.
For example, the data were explored to consider locals who appear more and more similar to visitors. Such a comparison tests whether the returns can be found for similar locals and whether returns are higher for those who are similar to travelers. Using all of the observable characteristics, the propensity of being a visitor was estimated and the sample was divided into deciles. Among visitors, the results were fairly stable across the deciles, again demonstrating the robustness of the main results. Meanwhile, the coefficient on the local-area end-of-life cost measure becomes increasingly negative as the propensity of being a visitor increases, with the top decile associated with a coefficient of −0.008 (s.e.=0.006). In addition, all of the analyses that were done for visitors were conducted for locals as well, and the lack of relationship between spending intensity and inpatient mortality was generally robust. 32
One explanation is that the unobservable characteristics shown to be important when individual-level costs are correlated with higher mortality continue to confound estimates when the cost measures are aggregated to the area level. Another explanation is that tourists—who are relatively unfamiliar to local physicians—have higher returns to intensive-care unit and diagnostic services.
6. Conclusions
Estimates of returns to healthcare spending can be confounded by the fact that individuals in worse health receive more care. In fact, there is a strong positive correlation between spending and mortality at the individual level, even after controlling for observable characteristics such as age and comorbidity levels. Regional measures of spending intensity aggregate the choices made at the individual level, which can again confound comparisons.
When patients who experience an emergency when they are far from home are considered, those in high-spending areas have significantly lower mortality compared to those in low-spending ones. These results were found within similar groups of patients, similar destinations, and across a wide variety of emergency conditions. Areas that spend more are most highly associated with greater levels of intensive care services, as well as treatment in teaching hospitals. Higher staff-to-patient ratios are also found in high-spending areas. The finding that this bundle of characteristics is associated with higher costs and lower mortality is in contrast to prior cross-sectional evidence, but is consistent with prior instrumental-variable estimates that higher intensity care is associated with better health outcomes. While these results may relate in particular to the types of patients who are likely to travel, they suggest that high returns may be present, at least for emergency care.
Supplementary Material
Footnotes
This is a large literature. See, for example, Fisher et al., 1994; Pilote et al., 1995; Kessler and McClellan, 1996; Tu et al., 1997; O’Connor et al., 1999; Baicker and Chandra, 2004; Fuchs, 2004; Stukel, Lucas, and Wennberg, 2005; Sirovich et al., 2006; Garber and Skinner, 2008.
For example, see McClellan, McNeil and Newhouse 1994; Stukel et al., 2007; Cutler 2007; Stukel, Lucas and Wennberg, 2005; Chandra and Staiger, 2007; McClellan and Newhouse, 1997; Cutler, McClellan, Newhouse, and Remler, 1998,; Cutler and McClellan, 2001; Murphy and Topel, 2003; Nordhaus, 2005; Cutler, Rosen and Vijan, 2006; Luce et al., 2006; and Hall and Jones, 2007.
Previous papers considered variation in healthcare inputs due to the distance of patients to services (McClellan, McNeil, and Newhouse 1994; Gowrisankaran and Town 1999; Stukel et al., 2007, Cutler, 2007). This paper also considers patients who use the nearest healthcare system, although the starting point is more likely to be exogenous as the healthcare system is less likely to be designed for visitors. Further, the healthcare market is considered rather than individual hospitals, as the market is also more likely to be exogenous than the particular hospital chosen by a patient or emergency medical services. Results at the hospital level will be shown as well.
For example, if the true model at the individual level were Mi = α0 + α1 Ti + ωi, then taking expectations at the geographic area level: E(Mi|Mi = 1) = 1 = α0 + α1 E(Ti|Mi = 1) + E(ωi|Mi = 1). If α1 < 0, then the area-level proxy for spending, Tg(i) = E(Ti+Mi = 1), is directly related to unobserved illness severity of patients who died in the area. If individuals in an area are similar to one another in unobserved health characteristics, then the between-area variation in end-of-life spending would capture between-area variation in health.
The results here substitute the median cost-to-charge ratio for outliers as suggested by CMS. In particular, the data are replaced when the cost-to-charge ratio for the hospital is in the top or bottom 2%. Results were not sensitive to outlier definitions. Results are also similar when the raw facility charge measure was used.
Future work will consider Medicare Inpatient Claims to examine longer-term mortality. Initial estimates suggest similar results for one-year mortality among the Florida visitors considered here.
1997 is the first year this lodging-rate data are available. 1996 per-diems were computed using a time trend through the 1997–2003 series. Results were similar when only the 1997 per-diem data were used instead.
These are three-digit ICD9-CM primary diagnosis codes of 410, 427, and 428.
Only 0.16% of the AMIs among visitors were the result of a “subsequent episode of care” versus 0.4% among locals, although this is defined by an ICD-9CM code suffix that is generally unrelated to reimbursement and is thought to be unreliable.
Table 1 shows a representative subset of characteristics for ease of display. See Table A1 for a wider set of variables.
The first quarter may have more visitors who spend the entire winter in Florida. These “snow birds” are considered in more detail below.
Fortunately, healthcare spending varies widely even within destinations with similar lodging and meal prices. When counties were broken into quartiles based on the January per-diem rate, the average, end-of-life log spending from the least to most expensive are 9.9, 9.9, 10.2, and 9.9, with standard deviations of 0.24, 0.23, 0.14, and 0.11, respectively.
Given that each metropolitan area contains multiple HSAs, the spending intensity proxy for this table is calculated at the metropolitan-area level, and the comparison is somewhat different from Table 1. The 2nd highest quartile contains cities close to the northern Florida border, and has more visitors coming from the South, which results in somewhat different characteristics than the other quartiles. In terms of patient characteristics along these city-based quartiles, the average age of visiting patients across the quartiles used in Table A2 does not monotonically decrease, with average ages across the quartiles (from bottom to top) of 71.3, 72.2, 69.1 and 67.2.
Individual age categories are used, with the exception of wider categories for patients under the age of 20, between 20 and 30, and above 100 years old.
In addition to indicators for each U.S. state, indicators for Canada, the Americas, and “unknown” state of residence, which is used to describe foreign visitors, are included as well. Estimates are similar when patients from outside the U.S. are excluded, as shown below.
These estimates are reported in Appendix Table A5. This result is less robust, however. When markets were defined at the county level, mortality was found to decrease for each of these quartiles.
A trip was categorized as a business trip if the reason for travel was: business, combined business/pleasure, convention, conference, or seminar, or other reason (i.e., not a vacation). The results were robust to the definition of business travel. In areas that were categorized as business destinations, 28% (range: 19–55%) of the trips were for business reasons, compared to 14% in non-business destinations. Among 40–60 year olds, the business-trip rates ranged from and 8% to 17%.
Similar results are found for all emergency diagnosies (Appendix Table A5). The top 100 include a wide range of conditions ranging from intestinal infections (n=1052) to skull base fracture (n=914).
HSA and county fixed effects were also considered, although the change in hospital-area spending levels within these eight years is not associated with changes in mortality. High-spending areas tend to remain so, with a spending measure defined on a county-by-year basis having a 1-year correlation of 0.95. The idea of this paper is that the large amount of cross-sectional variation in local-area spending can be exploited using a visitor sample where the variation is more likely to be exogenous.
The $214 per-diem rate is for Monroe County, which includes the Florida Keys; the next most expensive county has a per-diem rate of $132.
As shown in the working paper version of this paper, when the quartiles were constructed based on the number of patients in each county, rather than the equal weights shown in Table 4, the coefficients were consistently negative.
Alternatively, high-spending areas may be more likely to keep patients in the hospital until death rather than discharging seriously ill patients to other facilities (Pritchard et al., 1998; Wennberg et al., 2004).
See Appendix Figure A1 that uses American Travel Survey data to estimate the denominator in the visitor admission rate. Further, the detailed mortality file of the National Vital Statistics System provides information on whether deaths occur in the hospital or outside the hospital, and these data have the advantage of listing the home state of the decedent to identify locals and visitors. The fraction of descendants listed as in-hospital is unrelated to spending intensity, although some evidence suggests a positive relationship among locals, consistent with earlier work (Mitchell, 1992; Wennberg, Fisher and Skinner, 2002; Fisher and Wennberg, 2008). Results are shown in Appendix Table A10.
Author’s calculations based on Dartmouth Atlas of Health Care data.
A 2 standard deviation in the spending intensity measure would be associated with $4000 in additional costs, which is also associated with a 1.4 percentage point reduction in mortality. Dividing the two would provide an instrumental variables estimate of the effectiveness of spending at the individual level, and imply a $285,000 cost per statistical life saved (during the initial hospital stay). Similar results are found for the entire sample of emergency patients.
There is a large literature documenting the survival benefits of ICU care. Ridley and Morris (2007) review 8 studies that consider variation in ICU entry due to temporary crowding. The median estimate for the relative risk of death for patients who are denied access to an ICU is 1.68. Another review of 10 similar studies by Sinuff et al. (2004) finds a relative risk of death of 3.04. Chalfin et al. (2007) compared patients who were delayed entry into an ICU to those who were not and found in-hospital mortality rates of 17.4% (delayed) vs. 12.9% (non-delayed), controlling for age, sex, diagnosis, and health evaluation.
In a separate analysis, volumes of coronary artery bypass surgeries and cardiac catheterizations were calculated and counties were broken into quartiles based on these counts. Counties that had particularly high volumes of local-area surgeries were associated with lower mortality rates compared to counties in the 2nd and 3rd quartiles.
The result was found in overall, although it was less robust within specific diagnoses. The paper found that hip fracture was the only one to have a statistically significantly different mortality rate (hazard ratio of 0.54)—the condition where selection bias due to hospital admission is thought to be the least severe.
See Appendix Table A8.
The main results are also robust to using end-of-life length of stay to characterize HSAs rather than costs. In a model of mortality, the coefficient on local-area, end-of-life length of stay is −0.028 (s.e.=0.021).
The AHA data also lists staff expenses (a measure of the wage bill) and the number of physicians directly employed by the hospital (as opposed to physicians with admitting priviledges. The wage bill measure, as well as US Census data on physician and nurse income at the county level, were not related to spending intensity, although these relationships were imprecisely estimated. Results were similar when the number of nurses or physicians was the dependent variable and the number of admissions was included as a control. Further, the presence of a catheterization lab in an HSA or hospital was associated with moderately higher mortality rates, although this result is not statistically significant and may relate to the in-hospital mortality risk of procedures that may follow a catheterization.
Another potential explanation for the lower mortality rate found for visitors in high-spending areas is that they may frequent relatively better hospitals than the locals, and the local-area measures obscure within-HSA differences in treatment intensity. Popular hospitals among locals are popular among visitors, however. When the fraction of visitors that visit a particular hospital in an HSA is regressed on the fraction of locals who visit that hospital, the coefficient is 0.97 (C.I. = 0.93, 1.01).
References
- Baicker Katherine, Chandra Amitabh. Medicare Spending, the Physician Workforce, and the Quality of Care Received by Medicare Beneficiaries. Health Affairs. 2004;W4:184–197. doi: 10.1377/hlthaff.w4.184. [DOI] [PubMed] [Google Scholar]
- Baker Laurence C, Fisher Elliot S, Wennberg John E. Variations in Hospital Resource Use for Medicare and Privately Insured Populations in California. Health Affairs. 2008;27(2):w123–34. doi: 10.1377/hlthaff.27.2.w123. [DOI] [PubMed] [Google Scholar]
- Bertko John M. Perspective: Variation in use of Medical Care Services: Higher Risk or Higher Consumption? Health Affairs Web Exclusive. 2003 Aug 13; doi: 10.1377/hlthaff.w3.363. [DOI] [PubMed] [Google Scholar]
- Bjorklund Anders, Moffitt Robert. The Estimation of Wage Gains and Welfare Gains in Self-Selection Models. The Review of Economics and Statistics. 1987 Feb;69(1):42–49. [Google Scholar]
- Catlin Aaron, Cowan Cathy, Heffler Stephen, Washington Benjamin. National Health Spending In 2005: The Slowdown Continues. Health Affairs. 2007;26(1):142–153. doi: 10.1377/hlthaff.26.1.142. [DOI] [PubMed] [Google Scholar]
- Chalfin Donald B, Trzeciak Stephen, Likourezos Antonios, Baumann Brigitte M, Phillip Dellinger R. Impact of Delayed Transfer of Critically Ill Patients form the Emergency Department to the Intensive Care Unit. Critical Care Medicine. 2007;35(6):1477–1483. doi: 10.1097/01.CCM.0000266585.74905.5A. [DOI] [PubMed] [Google Scholar]
- Chandra Amitabh, Staiger Douglas O. Productivity Spillovers in Healthcare: Evidence from the Treatment of Heart Attacks. Journal of Political Economy. 2007;115(1):103–140. doi: 10.1086/512249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Congressional Budget Office. Geographic Variation in Healthcare Spending. 2008. [Google Scholar]
- Cutler David M. The Lifetime Costs and Benefits of Medical Technology. Journal of Health Economics. 2007;26(6):1081–1100. doi: 10.1016/j.jhealeco.2007.09.003. [DOI] [PubMed] [Google Scholar]
- Cutler David M, McClellan Mark B. Is technological change in medicine worth it? Health Affairs. 2001;20(5):11–29. doi: 10.1377/hlthaff.20.5.11. [DOI] [PubMed] [Google Scholar]
- Cutler David M, McClellan Mark B, Newhouse Joseph P, Remler Dahlia. Are medical prices declining? Evidence for heart attack treatments. Quarterly Journal of Economics. 1998;113(4):991–1024. [Google Scholar]
- Cutler David M, Rosen Allison B, Vijan Sandeep. The Value of Medical Spending in the United States, 1960–2000. New England Journal of Medicine. 2006;355:920–927. doi: 10.1056/NEJMsa054744. [DOI] [PubMed] [Google Scholar]
- Dobkin Carlos. Working Paper. 2003. Hospital Staffing and Inpatient Mortality. [Google Scholar]
- Fisher Elliot S, Bynum Julie P, Skinner Jonathan S. Slowing the Growth of Healthcare Costs—Lessons from Regional Variation. New England Journal of Medicine. 2009;360(9):849–852. doi: 10.1056/NEJMp0809794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher Elliot S, Gilbert Welch H. Avoiding the Unintended Consequences of Growth in Medical Care: How Might More Be Worse? Journal of the American Medical Association. 1999;281:446–453. doi: 10.1001/jama.281.5.446. [DOI] [PubMed] [Google Scholar]
- Fisher E, Wennberg D, Stukel T, Gottlieb D, Lucas F, Pinder E. Implications of regional variations in Medicare spending. part 2: health outcomes and satisfaction with care. Annals of Internal Medicine. 2003;138(4):288–298. doi: 10.7326/0003-4819-138-4-200302180-00007. [DOI] [PubMed] [Google Scholar]
- Fisher Elliott S, Wennberg John E, Stukel Therese A, Sharp Sandra M. Hospital Readmission Rates for Cohorts of Medicare Beneficiaries in Boston and New Haven. New England Journal of Medicine. 1994;331:989–995. doi: 10.1056/NEJM199410133311506. [DOI] [PubMed] [Google Scholar]
- Fuchs Victor R. More Variation in Use of Care, More Flat-of-the-curve Medicine. Health Affairs. 2004;23(6):104–107. doi: 10.1377/hlthaff.var.104. [DOI] [PubMed] [Google Scholar]
- Fuchs Victor R. Florida Exceptionalism. Health Affairs Web Exclusive. 2003 Aug 13; [Google Scholar]
- Fuchs Victor R, McClellan Mark, Skinner Jonathan. NBER Working Paper Series, No 8628. 2001. Area Differences in the Utilization of Medical Care and Mortality Among U.S. Elderly. [Google Scholar]
- Garber Alan M, Skinner Jonathan S. Is American Healthcare Uniquely Inefficient? Journal of Economic Perspectives. 2008;22(4):27–50. doi: 10.1257/jep.22.4.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gold Sharon. Robert Woods Johnson Foundation Research Synthesis Report No 6. 2004. Geographic variation in per capita Medicare spending: Should policy-makers be concerned? [Google Scholar]
- Gowrisankaran Gautam, Town Robert J. Estimating the Quality of Care in Hospitals Using Instrumental Variables. Journal of Health Economics. 1999;18:747– 67. doi: 10.1016/s0167-6296(99)00022-3. [DOI] [PubMed] [Google Scholar]
- Guadagnoli Edward, Hauptman Paul J, Ayanian John Z, Pashos Chris L, McNeil Barbara J, Cleary Paul D. Variation in the Use of Cardiac Procedures after Acute Myocardial Infarction. New England Journal of Medicine. 1995;333:573–578. doi: 10.1056/NEJM199508313330908. [DOI] [PubMed] [Google Scholar]
- Hall Robert E, Jones Charles I. The Value of Life and the Rise in Health Spending. Quarterly Journal of Economics. 2007;122(1):39–72. [Google Scholar]
- Heckman J, LaLonde R, Smith J. The Economics and Econometrics of Active Labor Market Programs,” in O. Ashenfelter and D. Card, Chapter 31. Handbook of Labor Economics. 1999;IV:1865–2073. [Google Scholar]
- Heidenreich PA, McClellan M. Trends in treatment and outcomes for acute myocardial infarction: 1975–1995. American Journal of Medicine. 2001;110:165–174. doi: 10.1016/s0002-9343(00)00712-9. [DOI] [PubMed] [Google Scholar]
- Kessler Daniel, McClellan Mark. Do Doctors Practice Defensive Medicine? The Quarterly Journal of Economics. 1996;111(2):353–390. [Google Scholar]
- Lannon Patrick J. Domicile Planning — Don’t Take it for Granted. The Florida Bar Journal. 2006;80(1):34. [Google Scholar]
- Lee Ronald, Skinner Jonathan. Will Aging Baby Boomers Bust the Federal Budget? The Journal of Economic Perspectives. 1999;13(1):117–140. [Google Scholar]
- Luce BR, Mauskopf J, Sloan FA, Ostermann J, Paramore C. The return on investment in healthcare: from 1980 to 2000. Value in Health. 2006;9 (3):146–156. doi: 10.1111/j.1524-4733.2006.00095.x. [DOI] [PubMed] [Google Scholar]
- McClellan Mark B, McNeil J, Newhouse Joseph P. Does more intensive treatment of acute myocardial infarction in the elderly reduce mortality? Analysis using instrumental variables. Journal of the American Medical Association. 1994;272:859–866. [PubMed] [Google Scholar]
- McClellan Mark B, Newhouse Joseph P. The Marginal Cost-Effectiveness of Medical Technology: A Panel Instrumental-Variables Approach. Journal of Econometrics. 1997;77:39–64. [Google Scholar]
- Mitchell Janet B. Area Variation in Medicare Physician Spending. Health Affairs. 1992;11(1):224–234. doi: 10.1377/hlthaff.11.1.224. [DOI] [PubMed] [Google Scholar]
- Murphy Kevin M, Topel Robert. The Economic Value of Medical Research. In: Murphy Kevin M, Topel Robert H., editors. Measuring the Gains from Medical Research: An Economic Approach. Chicago: University of Chicago Press; 2003. [Google Scholar]
- Nordhaus William D. Irving Fisher and the Contribution of Improved Longevity to Living Standards. American Journal of Economics and Sociology. 2005;64(1):367–392. [Google Scholar]
- O’Connor Gerald T, Quinton Hebe B, Traven Neal D, Ramunno Lawrence D, Dodds T Andrew, Marciniak Thomas A, Wennberg John E. Geographic Variation in the Treatment of Acute Myocardial Infarction: The Cooperative Cardiovascular Project. Journal of the American Medical Association. 1999;281:627–633. doi: 10.1001/jama.281.7.627. [DOI] [PubMed] [Google Scholar]
- Phelps Charles E. Information Diffusion and Best Practice Adoption. In: Culyer AJ, Newhouse JP, editors. Handbook of Health Economics. 1. Vol. 1. Amsterdam: Elsevier; 2000. [Google Scholar]
- Phillips Kathryn A, Shipak Michael G, Coxson Pam, Heidenreich Paul A, Hunink MG Myriam, Goldman Paula A, Williams Lawrence W, Weinstein Milton C, Goldman Lee. Health and Economic Benefits of Increased β-Blocker Use Following Myocardial Infarction. Journal of the American Medical Association. 2000;284:2748–2754. doi: 10.1001/jama.284.21.2748. [DOI] [PubMed] [Google Scholar]
- Pilote Louise, Califf Robert M, Sapp Shelly, Miller Dave P, Mark Daniel B, Weaver W Douglas, Gore Joel M, Armstrong Paul W, Ohman E Magnus, Topol Eric J. Regional Variation across the United States in the Management of Acute Myocardial Infarction. New England Journal of Medicine. 1995;333:565–572. doi: 10.1056/NEJM199508313330907. [DOI] [PubMed] [Google Scholar]
- Pope Gregory, Welch W Pete, Zuckerman Stephen, Henderson Mary G. Cost of Practice and Geographic Variation in Medicare Fees. Health Affairs. 1989 Fall;:117–128. doi: 10.1377/hlthaff.8.3.117. [DOI] [PubMed] [Google Scholar]
- Pritchard Robert S, Fisher Elliott S, Teno Joan M, Sharp Sandra M, Reding Douglas J, Knaus William A, Wennberg Jone E, Lynn Joanne. Influence of Patient Preferences and Local Health System Characteristics on the Place of Death. Journal of the American Geriatrics Society. 1998;46(10):1242–1250. doi: 10.1111/j.1532-5415.1998.tb04540.x. [DOI] [PubMed] [Google Scholar]
- Quan H, Sundararajan V, Halfon P, Fong A, Burnand B, Luthi JC, Saunders LD, Beck CA, Feasby TE, Ghali WA. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Medical Care. 2005;43(11):1073–1077. doi: 10.1097/01.mlr.0000182534.19832.83. [DOI] [PubMed] [Google Scholar]
- Ridley S, Morris S. Cost Effectiveness of Adult Intensive care in the UK. Anaesthesia. 2007;62:547–554. doi: 10.1111/j.1365-2044.2007.04997.x. [DOI] [PubMed] [Google Scholar]
- Sheehan-Connor Damien. Working Paper. Feb, 2007. Traveler Experience as an Instrument to Assess Medical Care Effectiveness. [Google Scholar]
- Sinuff T, Kahnamoui K, Cook DJ, Luce JM, Levy MM. Rationing Critical Care Beds: A Systematic Review. Critical Care Medicine. 2004;32(7):1588–1597. doi: 10.1097/01.ccm.0000130175.38521.9f. [DOI] [PubMed] [Google Scholar]
- Sirovich BE, Gottlieb DJ, Welch HG, Fisher ES. Regional variations in healthcare intensity and physician perceptions of the quality of care. Annals of Internal Medicine. 2006;144:641–649. doi: 10.7326/0003-4819-144-9-200605020-00007. [DOI] [PubMed] [Google Scholar]
- Skinner Jonathan, Fisher Elliott, Wennberg John E. The Efficiency of Medicare. In: Wise David., editor. Analyses in the Economics of Aging. Chicago: University of Chicago Press and NBER; 2005. pp. 129–57. [Google Scholar]
- Skinner Jonathan, Wennberg John E. Regional Inequality in Medicare Spending: The Key to Medicare Reform? Forum for Health Economics & Policy. 2000;3:69–90. [Google Scholar]
- Skinner Jonathan, Wennberg John E. Exceptionalism Or Extravagance? What’s Different About Health Care In South Florida. Health Affairs Web Exclusive. 2003 Aug 13; doi: 10.1377/hlthaff.w3.372. [DOI] [PubMed] [Google Scholar]
- Stukel Therese A, Fisher Elliott S, Wennberg David E, Alter David A, Gottlieb Daniel J, Vermeulen Marian J. Analysis of Observational Studies in the Presence of Treatment Selection Bias: Effects of Invasive Cardiac Management on AMI Survival Using Propensity Score and Instrumental Variable Methods. Journal of the American Medical Association. 2007;297:278–285. doi: 10.1001/jama.297.3.278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stukel Therese A, Lucas F Lee, Wennberg David E. Long-term Outcomes of Regional Variations in Intensity of Invasive vs Medical Management of Medicare Patients With Acute Myocardial Infarction. Journal of the American Medical Association. 2005;293:1329–1337. doi: 10.1001/jama.293.11.1329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor Donald H, Whellan David J, Sloan Frank A. Effects of Admission to a Teaching Hospital on the Cost and Quality of Care for Medicare Beneficiaries. New England Journal of Medicine. 1999;340:293–299. doi: 10.1056/NEJM199901283400408. [DOI] [PubMed] [Google Scholar]
- Tu Jack V, Pashos Chris L, Naylor C David, Chen Erluo, Normand Sharon-Lise, Newhouse Joseph P, McNeil Barbara J. Use of Cardiac Procedures and Outcomes in Elderly Patients with Myocardial Infarction in the United States and Canada. New England Journal of Medicine. 1997;336:1500–1505. doi: 10.1056/NEJM199705223362106. [DOI] [PubMed] [Google Scholar]
- Wennberg John E, Fisher Elliot S, Skinner Jonathan S. Geography and the Debate Over Medicare Reform. Health Affairs. 2002 doi: 10.1377/hlthaff.w2.96. Web Exclusive. [DOI] [PubMed] [Google Scholar]
- Wennberg John E, Fisher Elliot S, Stuke Therese A, Skinner Jonathan S, Sharp Sandra M, Bronner Kristen K. Use of hospitals, physician visits, and hospice care during last six months of life among cohorts loyal to highly respected hospitals in the United States. British Medical Journal. 2004;328:607–612. doi: 10.1136/bmj.328.7440.607. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.