Abstract
Anaplastic thyroid carcinoma (ATC) is an extremely aggressive malignancy with undifferentiated features, for which conventional treatments, including radioactive iodine ablation, are usually not effective. Recent evidence suggests that the Notch1 pathway is important in the regulation of thyroid cancer cell growth and expression of thyrocyte differentiation markers. However, drug development targeting Notch1 signaling in ATC remains largely underexplored. Previously, we have identified resveratrol out of over 7,000 compounds as the most potent Notch pathway activator using a high-throughput screening method. In this study, we showed that resveratrol treatment (10–50 μM) suppressed ATC cell growth in a dose-dependent manner for both HTh7 and 8505C cell lines via S phase cell cycle arrest and apoptosis. Resveratrol induced functional Notch1 protein expression and activated the pathway by transcriptional regulation. In addition, the expression of thyroid-specific genes including TTF1, TTF2, Pax8 and sodium iodide symporter (NIS) were up-regulated in both ATC cell lines with resveratrol treatment. Notch1 siRNA interference totally abrogated the induction of TTF1 and Pax8 but not of TTF2. Moreover, Notch1 silencing by siRNA decreased resveratrol-induced NIS expression. In summary, our data indicate that resveratrol inhibits cell growth and enhances re-differentiation in ATC cells dependent upon the activation of Notch1 signaling. These findings provide the first documentation for the role of resveratrol in ATC re-differentiation, suggesting that activation of Notch1 signaling could be a potential therapeutic strategy for ATC patients, and thus warrants further clinical investigation.
Keywords: Resveratrol, Notch1, differentiation, thyroid cancer, and anaplastic thyroid carcinoma
Introduction
Anaplastic thyroid carcinoma (ATC) represents less than 2% of all thyroid cancers, but it is responsible for around 50% of thyroid cancer mortality (1). The mean survival time for ATC is only about 6 months (2). One major challenge to the current treatment modality for ATC is the extremely fast-growing and aggressive nature of the tumor. For this reason, most ATCs are classified as stage IV diseases, making the majority of ATC patients ineligible for surgery (3). In addition, ATCs lose thyroid-specific gene expression during the dedifferentiation process, which impairs the capacity for concentrating or absorbing iodine. The conventional treatments for well-differentiated thyroid cancers, including radioactive iodine ablation, are therefore not effective for ATC patients (4,5). The inhibition of tumor growth and induction of re-differentiation in ATC have been the major goals in the development of a novel treatment (6).
Recently, the Notch1 pathway has been reported as an important signaling cascade that determinates thyroid cell fate and directly regulates thyroid-specific gene expression (7). Notch1, a multifunctional trans-membrane receptor, is activated upon two sequential proteolytic cleavages. The second cleavage within the trans-membrane domain allows the release and translocation of the intracellular domain of Notch1 (NICD) into the nucleus where it associates with DNA binding proteins to assemble a transcriptional complex that activates downstream target genes (8). Since Notch1 activation implements cellular differentiation, development, proliferation and survival in variety of contexts, it is not surprising that the aberrant gain or loss of Notch1 signaling has been directly linked to various kinds of cancers (9–12). For epithelial thyroid cancers, it has been found that the expression level of activated Notch1 (NICD) is much lower in human thyroid cancer tissue compared with normal thyroid tissue which has abundant NICD (13). Similar findings have been reported in another study, which shows that the down-regulation of Notch1 signaling in thyroid tumors is associated with the dedifferentiated phenotype of ATC. Furthermore, overexpression of Notch1 restores the differentiated phenotype of thyroid cancer cells (7). Based on the above findings, Notch1 pathway activating compounds could be worthy of study as a potential therapeutic for ATC.
Previously, we identified 27 compounds from over 7,000 via a high-throughput screening method. The 27 compounds were selected because they revealed over 300% pan-Notch activation in a carcinoid cell system. Among these positive hits, resveratrol showed the strongest Notch activation (14). Resveratrol is a polyphenol phytoalexin contained naturally in grapes, berries and several medicinal plants. It has been well-known for its chemopreventive and antineoplastic activity since first documented in late 1990s (15–19). However, little is known about the antitumor effect of resveratrol on ATC cells. A recent study has shown that resveratrol induces the expression of sodium iodide symporter (NIS) and increases iodide trapping in the rat thyrocyte cell line FRTL-5, though the molecular mechanisms for these findings are not fully elucidated (20). Given the role of Notch1 in cell differentiation, we hypothesized that resveratrol could activate Notch1 in ATC cells and thereby induce ATC re-differentiation.
In the present study, we aimed to evaluate the effects of resveratrol in ATC cells and obtain new insights about the responsible mechanisms. Our results showed that resveratrol was very potent at inhibiting ATC cell growth by inducing both cell cycle arrest and apoptosis. Additionally, resveratrol enhanced the thyroid-specific gene expression in ATC dependent upon Notch1 activation. These findings suggest, for the first time, that Notch1 activating compounds could be further investigated as a potential therapy for ATC patients.
Materials and Methods
Cell culture
The human ATC cell line HTh7 was kindly provided by Dr. Rebecca Schweppe (University of Colorado Denver, CO), and 8505C was provided by Dr. Daniel Ruan (Brigham and Women’s Hospital, Boston, MA). HTh7 and 8505C have been well documented as unique ATC-derived cell lines genotyped using a short tandem repeat profiling method (21). Both of the cell lines were authenticated. The cell lines were maintained in RPMI-1640 (Invitrogen Life Technologies, Carlsbad, CA) medium supplemented with 10% fetal bovine serum (Sigma-Aldrich, St Louis, MO), and were grown at 37 °C in a humidified atmosphere containing 5% CO2.
Resveratrol
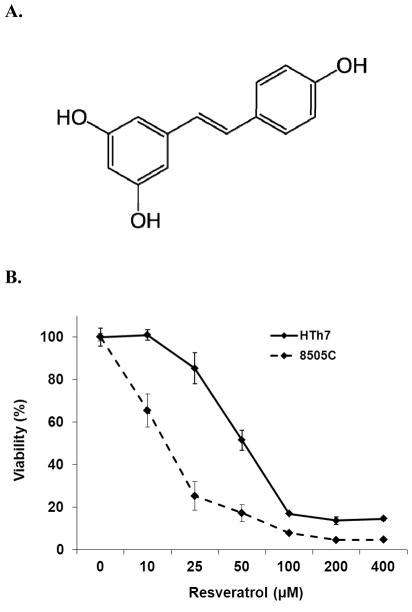
Resveratrol, also named as trans-3,4′,5-trihydroxystilbene (chemical structure shown in Fig. 1A), was obtained from Enzo Life Sciences, Inc. (Farmingdale, NY).
Figure 1.
Effect of resveratrol on ATC cell viability. A, Skeletal chemical structure of resveratrol, which is also named as trans-3,4′,5-trihydroxystilbene. B, Resveratrol treatment resulted in dose-dependent reduction of cell growth in both ATC lines. ATC cell lines, HTh7 and 8505C, were cultured for 72 hours in the presence of various concentration of resveratrol. Cell viability was measured by MTT assay and expressed as mean± SD (representative of four experiments).
Cell viability assay
Drug sensitivity of ATC cells growing in a monolayer was determined by the methylthiazolyldiphenyl-tetrazolium bromide (MTT) assay (Sigma-Aldrich) as previously described (22). Briefly, cells were plated at a density of 15,000 cells per well on 24-well plates in quadruplicate and incubated overnight under standard conditions to allow cell attachment. Resveratrol was added in serial dilutions in fresh medium and the plates were incubated for another 72 hours. After the treatment medium was removed, 250μL of serum-free medium containing 0.5 mg/mL MTT was added to each well and incubated for 4 hours at 37°C. MTT formazan crystals were dissolved by adding 750 μL of dimethyl sulphoxide (DMSO) (Fischer Scientific, Pittsburg, PA) in each well and the absorbance was measured at 540nm in a spectrophotometer (μQuant; Bio-Tek Instruments, Winooski, VT).
Western blot analysis
ATC cells were treated with resveratrol at various concentrations for 48 hours. Then, the cells were washed twice with PBS before the lysis buffer was added. The protein lysates were prepared as previously described (23). Protein concentration was quantified using the BCA Protein Assay Kit (Thermo Scientific, Waltham, MA) following the manufacturer’s instructions. Equal amounts of denatured protein were resolved by electrophoresis on 4%–15% Criterion TGX precast gels (Bio-Rad Laboratories, Hercules, CA), transferred onto nitrocellulose membranes (Bio-Rad Laboratories), blocked in 5% nonfat milk solution, then immunoblotted with the following primary antibodies overnight at 4°C: p21 (1:2000), cyclin B1 (1:1000), cleaved Poly-ADP ribose polymerase (PARP) (1:3000) caspase-3 (1:1000), Bcl-2(1:1000), Bcl-xL (1:1000), β-actin (1:2000, all from Cell Signaling Technology, Danvers, MA) and Notch1 (1:1000, Santa Cruz Biotechnology, Santa Cruz, CA). Membranes were washed the other day and incubated for one hour at room temperature with horseradish peroxidase-conjugated secondary antibodies (1:2000, Cell Signaling Technology). The immunoreactive protein bands were visualized by the detection systems of Immunstar (Bio-Rad Laboratories), SuperSignal West Pico, or SuperSignal West Femto (Pierce Biotechnology, Rockford, IL). Immunoblot analyses were repeated at least twice and the expression levels of β-actin were used as the loading control.
Analysis of cell cycle distribution by flow cytometry
Cell cycle distribution was detected by flow cytometry analysis using APC BrdU Flow Kit (BD Pharmingen, San Diego, CA) according to manufacturer’s instructions. In brief, ATC cells were seeded in 6-well plate and treated with resveratrol at different concentrations for 24 hours in the medium. After labeling cells with 10 μM of BrdU for 2 hours at 37°C, cells were washed, fixed and permeabilized. Next, the cells were incubated with 100μL of DNase (300μg/mL) at 37 °C for one hour then stained with anti-BrdU antibody and 7-AAD. Samples were acquired by FACSCalibur (Becton Dickinson, San Jose, CA) and data was analyzed by FlowJo software (Tree Star, Inc., Ashland, OR).
Detection of cell apoptosis by flow cytometry
Cell apoptosis was detected by flow cytometry analysis using PE Annexin V Apoptosis Detection Kit I (BD Pharmingen) according to manufacturer’s instructions. In brief, ATC cell lines were seeded in 6-well plate and treated with resveratrol at different concentrations for 24 or 48 hours. Cells were harvested and resuspended in binding buffer (10 mM HEPES/NaOH, pH=7.4, 140 mM NaCl, and 2.5 mM CaCl2) at a concentration of 1 × 106 cells/mL. Then Annexin V-FITC (5 μL) and 7-AAD (10 μL) were added to 100 μL of each samples. Cells were gently mixed and incubated for 15 minutes at room temperature in the dark followed by the addition of another 400 μL of binding buffer. Stained cells were acquired within 1 hour on FACSCalibur (Becton Dickinson) and data were analyzed by FlowJo software (Tree Star).
Luciferase reporter assay
To determine the functional activity of Notch1, ATC cells were transiently transfected with luciferase constructs as previously described (13). Cells were plated onto 6-well plates in triplicate and allowed to adhere overnight. Wild-type CBF-1 luciferase reporter plasmid (a generous gift from Dr. Diane Hayward, Johns Hopkins University, Baltimore, MD) were cotransfected with cytomegalovirus β-galactosidase (CMV-β-gal; 0.5 μg) utilizing Lipofectamine 2000 Transfection Reagent (Invitrogen). Twenty hours after transfection, cells were treated with different concentrations of resveratrol for another 48 hours. Cells were then harvested and lysed. Luciferase and β-galactosidase assays (Promega, Madison, WI) were performed in accordance with the manufacturer’s instructions. Luciferase level was measured using a Monolight 2010 Luminometer (Analytical Luminescence Laboratory, San Diego, CA) and β-galactosidase activity was measured using a spectrophotometer at 420 nm (μQuant; Bio-Tek Instruments). Luciferase activity was determined relative to β-galactosidase activity.
Quantitative real-time PCR
Total RNA was isolated from cultured cells 48 hours after resveratrol treatment using silica-gel membrane-based spin-column technology (Qiagen Inc., Valencia, CA). Each RNA sample was examined by electrophoresis on a formaldehyde agarose gel and was quantified by NanoDrop (Thermo Scientific) to ensure the purity and integrity of RNA. Total RNA (2μg) was reverse transcribed using the iScript cDNA Synthesis Kit (Bio-Rad Laboratories). Sequences for each pair of PCR primers were listed in Supplementary Table S1. The quantitative real-time PCR reactions were performed on MyiQ Thermal Cycler (Bio-Rad Laboratories). Target gene expression was normalized to GAPDH levels in respective samples as an internal standard, and the comparative cycle threshold (ΔCt) method was used to calculate relative expression levels of target genes.
Immunofluorescence
ATC cells were plated on 8-well chamber slides (Nalge Nunc, Rochester, NY) in RPMI medium containing 10% FBS. After incubation overnight, cells were treated with or without resveratrol (25μM) for another 48 hours. Cells were then rinsed and fixed in 4% paraformaldehyde for 30 minutes at room temperature. After permeabilization in 0.2% Triton X-100 for 10 min at 4°C and blocking with 5% bovine serum albumin and 3% donkey serum in PBS for one hour at room temperature, the cells were incubated with mouse monoclonal anti-Pax8 antibody (10 μg/mL; Abcam, Cambridge, MA) and rabbit polyclonal anti-TTF1 antibody (2 μg/mL; Santa Cruz Biotechnology) at 4°C overnight. Antigens were visualized using Alexa-488-conjugated donkey anti-mouse and Alexa-555-conjugated donkey anti-rabbit (1:300, 30 minutes) secondary antibodies (Invitrogen). Nuclear staining was performed with DAPI (Invitrogen). Images were acquired with a Nikon Eclipse E800 upright microscope and attached RetigaEXi CCD digital camera. Images were processed and analyzed using Adobe Photoshop 7.0.
Notch1 siRNA interference assay
Desalted siRNA duplex targeting Notch1 and non-specific siRNA (NS siRNA; Santa Cruz Biotechnology) were delivered into ATC cells using Lipofectamine RNAiMAX (Invitrogen) according to manufacturer’s protocol. After 24 hours, the cells were treated either with or without resveratrol (25μM) for another 48 hours followed by protein and mRNA isolation for Western blot and real-time PCR analyses, respectively.
Subcutaneous Xenograft Tumor Model and Resveratrol Administration
Animal studies were performed in compliance with our animal experiment protocol approved by the University of Wisconsin Madison Animal Care and Use Committee. HTh7 cells (2×106 per 200μL for each mouse) or 8505C cells (8×106 per 200μL for each mouse) were mixed 1:1 with Matrigel (BD Biosciences) and injected subcutaneously (s.c) into the right flanks of 20 6-week old male athymic mice (Harlan Laboratories, Madison, WI). Ten days after inoculation, mice with palpable tumors were randomly divided into two groups for equal tumor size distribution (10 in each group for each cell line). Animals were treated daily for 5 weeks with either resveratrol (50mg/kg) or control DMSO administrated by oral gavage. Fresh dilutions of resveratrol were made with DMSO and Neobee M5 oil (Spectrum Chemical MFG Corp., New Brunswick, NJ) before each treatment. We further tested the drug effect by local administration using peri-tumor injections. HTh7 cells (2 × 106) were injected s.c. in 10 athymic mice. After 10-day inoculation, the mice were divided into two groups of five animals each. Peri-tumor injections were given every four days for 20 days of 2 mg of resveratrol in 100 μL DMSO (treatment) or DMSO alone (vehicle control). All 50 mice were weighed every four days during the study period. The volume of the xenograft tumor was measured every four days using digital calipers and calculated according to the following formula: tumor volume = length × (width)2 × π/6. The relative tumor volume was defined as the fold change of tumor volume for each time point compared to the initial volume when treatment started.
Statistical analysis
Continuous data were expressed as mean ± SD. One-way ANOVA or two-tailed Student’s t test was used to determine statistical significance using the Statistical Package for the Social Sciences (SPSS, version 17, IBM SPSS). P < 0.05 was considered significant.
Results
Resveratrol Suppressed Cell Growth in ATC by Both Cell Cycle Arrest and Apoptosis
To determine the effective dose on ATC, MTT assay was carried out to measure cell viability 72 hours after resveratrol treatment of different concentrations up to 400μM. Both cell lines, HTh7 and 8505, showed a profound dose-dependent growth inhibition by resveratrol (Fig. 1B, p<0.05). The average IC50 values for HTh7 and 8505C from four experiments were 49.9 and 10.2 μM, respectively.
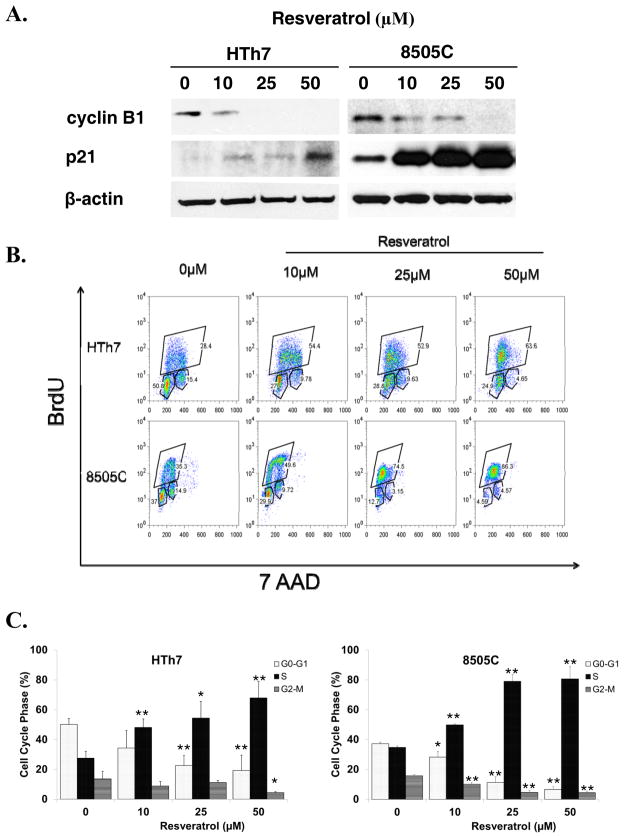
The possible mechanisms responsible for ATC growth suppression by resveratrol were then investigated. The levels of representative cell cycle regulators were assessed 48 hours after resveratrol treatment of 10, 25 and 50 μM, which covered the effective dose range for both of the ATC cell lines. Resveratrol treatment resulted in an increase in protein levels of cyclin-dependent kinase inhibitor p21, while the levels of cell cycle promoter of cyclin B1 were decreased (Fig. 2A). To further determine the associated changes in cell cycle distribution, the ATC cells were labeled with BrdU 24 hours after resveratrol treatment for flow cytometry analysis. Resveratrol treatment induced S phase accumulation in both cell lines. Accordingly, the cell numbers in both G0-G1 and G2-M phases were diminished (one representative result shown in Fig. 2B). The mean percentage of cells in S phase increased between control cells and cells treated with 25 μM resveratrol from 27.5% to 54.5% in HTh7 and from 34.7% to 79.1% in 8505C (p<0.05). In contrast, the percentage of the cells in both G0-G1 and G2-M phases dropped significantly with the increasing doses of resveratrol treatment (p<0.05, all data from repeats were summarized in Fig. 2C).
Figure 2.
Cell cycle arrest in ATC caused by resveratrol treatment. A, Detection of cyclinB1and p21 protein expression by Western blot in HTh7 and 8505C cells treated with three different concentrations of resveratrol (10, 25, 50μM) or vehicle control. Equal loading was confirmed with β-actin. B, Resveratrol caused S phase arrest in both HTh7 and 8505C cells. ATC cells were exposed to different concentrations of resveratrol for 24 hours before they were labeled with BrdU and 7 AAD for flow cytometry analysis. Percentages denote the cells in each cell cycle phase from total single cell population. Results of one representative experiment. Data from three repeated experiments are summarized in bar graph (C). ATC cells with resveratrol treatment were accumulated in S phase while diminished in both G0-G1 and G2-M phases. Data are shown as mean ± SD (n=3, *P<0.05, **P<0.01 vs. control cells without resveratrol treatment).
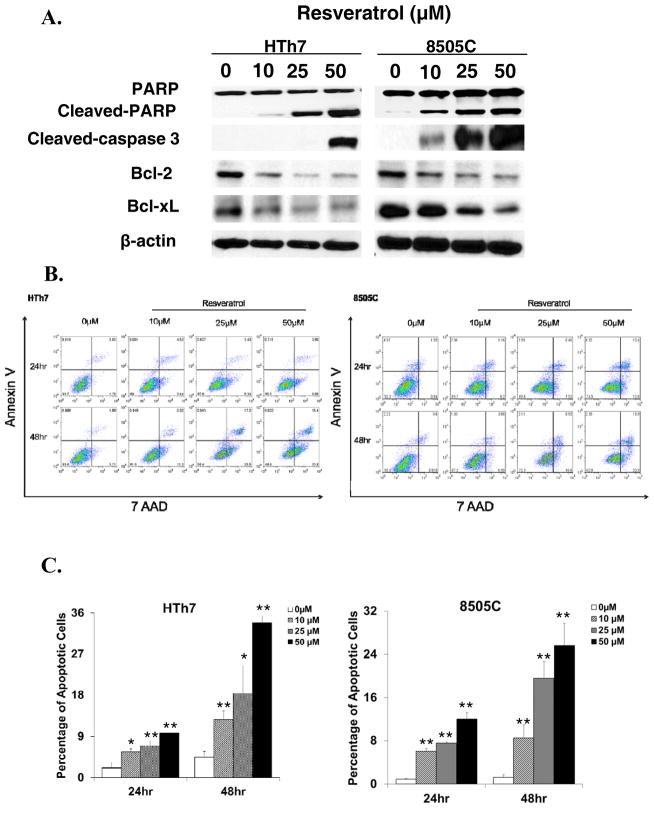
It was also found that the cleavages of Poly (ADP-ribose) polymerase (PARP) and caspase-3, both of which are pro-apoptotic markers in the execution phase of cell apoptosis, were greatly induced along with the resveratrol treatment. At the same time, the anti-apoptotic markers including Bcl-2 and Bcl-xL were reduced (Fig. 3A). To quantify the number of cells undergoing apoptosis, ATC cells were double stained with Annexin V and 7 AAD after 24 hours or 48 hours treatment with different concentrations of resveratrol. Early apoptotic cells were positive for Annexin V and negative for 7 AAD when analyzed by flow cytometry. Resveratrol triggered ATC cell apoptosis in a dose- and time-dependent manner. As shown in Fig. 3B, the number of apoptotic cells increased with time as well as increasing doses of resveratrol (p<0.05, all data from repeats were summarized in Fig. 3C). The above observations strongly suggested that the resveratrol suppressed ATC cell growth by both cell cycle arrest and induction of apoptosis.
Figure 3.
Apoptosis in ATC induced by resveratrol treatment. A, Detection of apoptotic markers including cleaved-PARP, cleaved-caspase 3, Bcl2 and Bcl-xL by Western blot in HTh7 and 8505C cells treated with three different concentrations of resveratrol (10, 25, 50μM) or vehicle control. Equal loading was confirmed with β-actin. B, Resveratrol induced apoptosis in a time-and dose-dependent manner. ATC cells were exposed to different concentrations of resveratrol for 24 hours and 48 hours before they were double stained with Annexin V and 7 AAD for flow cytometry analysis. Percentages at right lower quadrant denote the cells in early apoptotic phase. Results of one representative experiment. Data from three repeated experiments are summarized in bar graph (C), and are shown as mean ± SD (n=3, *P<0.05, **P<0.01 vs. control cells without resveratrol treatment).
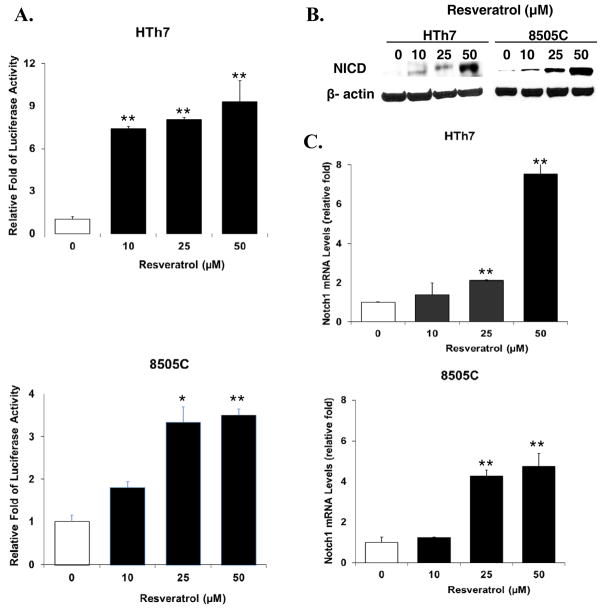
Resveratrol Activated Notch1 Signaling in ATC
In order to determine if resveratrol acts as a functional Notch1 activating compound in an ATC context, a luciferase reporter assay using the CBF-1 binding site was carried out. CBF-1 was used because it is the primary nuclear effector of the Notch signaling pathway. The interaction between active Notch isoforms and CBF-1 allows for the generation of a transcriptional activation complex. Resveratrol treatment of 25 μM on HTh7 and 8505C cells transfected with the luciferase construct resulted in a greater than 8- and 3-fold increase of relative luciferase activity, respectively (p<0.05, Fig. 4A).
Figure 4.
Resveratrol activated Notch1 signaling in both HTh7 and 8505C cell lines. A, Resveratrol treatment resulted in significant increase of luciferase activity in ATC cells transfected with luciferase reporter plasmid containingCBF-1 binding site. Luciferase activity was first normalized to β-galactosidase unit, and data were expressed relative to control cells without resveratrol treatment. B, Notch1 intracellular domain (NICD) expression levels detected by western blot in ATC cells treated with different concentrations of resveratrol or vehicle control. Equal loading was confirmed with β-actin. C, Notch1 mRNA levels in resveratrol treated ATC cells were assessed by real-time RT-PCR, and data were plotted relative to control cells without resveratrol treatment. All values were expressed as mean± SD (n=3, *P<0.05 and **P<0.01 compared with control).
The luciferase reporter assay demonstrated that the Notch pathway was functionally active due to resveratrol treatment. To determine which of the Notch isoforms were affected by resveratrol, we performed Western blot analysis. As shown in Figure 4B, resveratrol led to an increased expression of Notch1 intracellular domain (NICD) in both ATC cell lines in a dose-dependent manner. However, the levels of both Notch2 and Notch3 intracellular domains showed no difference between control and the treated cells (data not shown here). Furthermore, the mRNA level of Notch1 was also elevated by resveratrol treatment of 25 and 50 μM (Fig. 4C), indicating that resveratrol activated Notch1 signaling mainly by transcriptional up-regulation of Notch1.
Resveratrol Induced Expression of Thyroid-Specific Genes in ATC
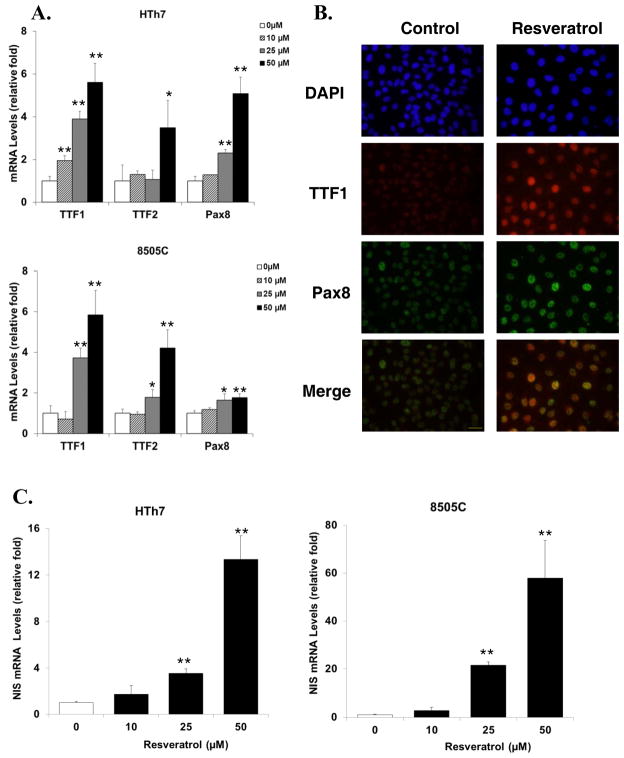
To investigate the effects of resveratrol on cell differentiation, thyroid-specific genes including thyroid transcription factor 1 (TTF1), thyroid transcription factor 2 (TTF2), and paired box gene 8 (Pax8) were examined. Treatment of resveratrol resulted in a profound induction of TTF1 mRNA level, which increased 4-fold at 25 μM and 6-fold at 50 μM from control levels in both cell lines. Significant elevation of TTF2 expression levels was observed at 50 μM treatment for both cell lines. Pax8 level in HTh7 cells increased by 5-fold at 50 μM treatment, while induced by less than 2-fold in 8505C cells (shown in Fig. 5A).
Figure 5.
Resveratrol enhanced the expression of differentiation markers in ATC cells. A, The mRNA levels of differentiation markers including TTF1, TTF2 and Pax8 were quantified by real-time RT-PCR in ATC cell lines treated with different concentrations of resveratrol or vehicle control. B, Immunofluorescence double staining of TTF1 and Pax8 in 8505C cells with resveratrol treatment (25μM) or vehicle control. Strong positive staining of both TTF1 (red) and Pax8 (green) was localized to the nucleus of ATC cells treated with resveratrol compared with faint positive staining in control cells, thoughTTF1 and Pax8 were not co-localized to each other (shown in the merge figure). DAPI (blue) was used as a nuclear counterstain. Scale bar: 50μm. C, The mRNA level of NIS was assessed by real-time RT-PCR in ATC cell lines with or without resveratrol treatment. All data were plotted relative to cells treated with vehicle control. All values were expressed as mean± SD (n=3, *P<0.05 and **P<0.01 compared with control).
Since TTF1 and Pax8 are both contained in the regulatory region of the NIS promoter/enhancer (24), the expression and localization of these two proteins were studied. ATC cells (8505C) treated with 25 μM of resveratrol presented with a much stronger signal of TTF1 than the control cells. A slight induction was seen for Pax8, which was consistent with the mRNA level reported above. Both TTF1 and Pax8 were localized in the cell nucleus, but they were not co-localized with one another (Fig. 5B). HTh7 and 8505C cells have minimal to no detectable endogenous NIS. However, NIS mRNA levels increased markedly along with the induction of TTF1 and Pax8 by resveratrol treatment (Fig. 5C).
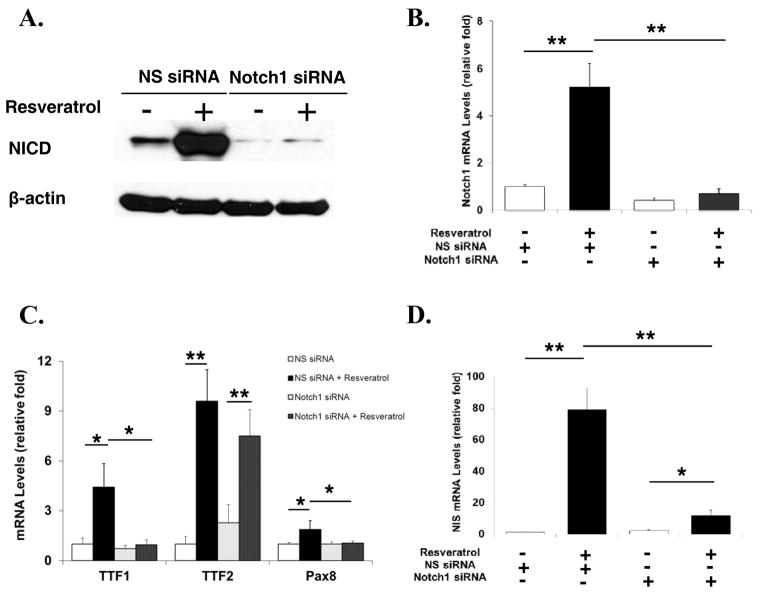
Re-differentiation by Resveratrol was Mainly Dependent upon Notch1 Activation
To determine the role of Notch1 activation in cell re-differentiation of ATC cells, 8505C cells were transiently transfected with siRNA against Notch1 or non-specific siRNA, then treated with or without resveratrol. Notch1 siRNA effectively silenced Notch1 on both protein (Fig. 6A) and mRNA (Fig. 6B) levels despite resveratrol treatment, when compared to non-specific siRNA transient transfection. The mRNA levels of TTF1, TTF2 and Pax8 were elevated in resveratrol treated 8505C cells with non-specific siRNA, which was similar to those levels in absence of siRNA(as previously shown in Fig. 5A). The abrogation of resveratrol-mediated Notch1 induction by Notch1 siRNA resulted in unchanged expression levels of TTF1 and Pax8 in ATC cells with resveratrol treatment while TTF2 levels were still seen to increase (Fig. 6C). This suggested that the induction of TTF1 and Pax8 by resveratrol was dependent upon Notch1 activation, but TTF2 induction was Notch1 independent. In addition, the changes of NIS mRNA levels with resveratrol treatment were partially reversed by Notch1 targeted siRNA, indicating that NIS induction was mainly mediated through Notch1 activation but not completely (Fig. 6D).
Figure 6.
Differentiation markers expression in ATC cells was dependent upon Notch1 signaling. A, NICD protein expression levels detected by western blot in 8505C cells, as well as Notch1 mRNA levels quantified by real-time RT-PCR (B). The cells were first exposed to non-specific siRNA (NS siRNA) or Notch1 siRNA and then treated with resveratrol or vehicle control. Notch1 siRNA was effective to block the induction of Notch1 by resveratrol treatment. Equal loading of protein lysate was confirmed with β-actin. C, The quantified mRNA levels of differentiation markers including TTF1, TTF2 and Pax8, as well as the levels of NIS (D)in 8505C cells by real-time RT-PCR. All data were plotted relative to cells treated NS siRNA and vehicle control. All values were expressed as mean± SD (n=3, *P<0.05 and **P<0.01 compared with control).
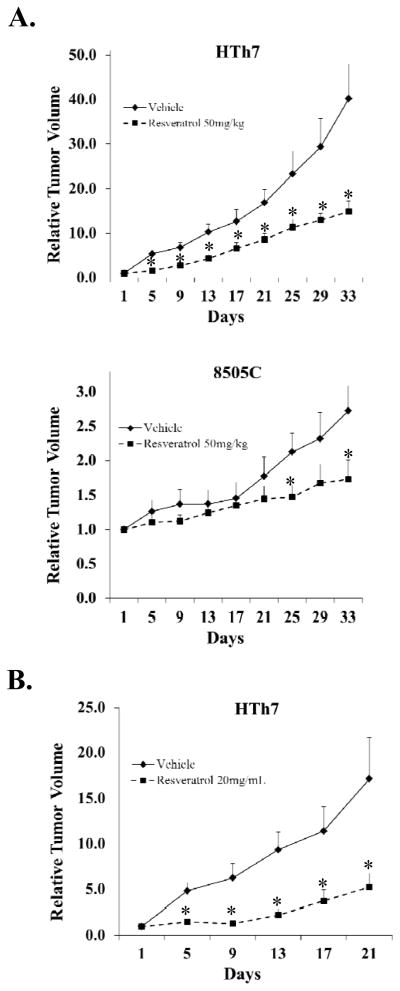
Resveratrol Suppressed ATC Tumor Growth in vivo
Next, we evaluated the impact of resveratrol in vivo using ATC xenograft model. Nude mice bearing subcutaneous HTh7 or 8505C cell xenografts were treated with either resveratrol by oral gavage (n=10, 50/kg/day) or DMSO as a vehicle control (n=10). None of the mice in the groups with resveratrol treatment exhibited any weight loss or overt toxicity compared to the controls. As shown in Fig. 7A, both HTh7 and 8505C xenografts were progressively suppressed in the resveratrol treatment group. The tumor volume of HTh7 xenografts in resveratrol treatment group reduced by an average of 63% compared with the vehicle control group 33 days after the first treatment (P<0.01). Similarly, resveratrol suppressed the growth of 8505C xenografts by an average of 36% by the end of the experiment (P=0.042). Local delivery of resveratrol by peri-tumor injection efficiently inhibited the HTh7 tumor growth. Tumor volume significantly reduced by 69% after 5 injections of resveratrol (Fig. 7B, P=0.036).
Figure 7.
Resveratrol suppressed ATC tumor growth in vivo. A, Tumor growth kinetics of HTh7 and 8505C xenografts treated with resveratrol of 50 mg/kg (n=10) or vehicle control (n=10) by oral gavage. B, Tumor growth curves of HTh7 xenografts treated with resveratrol of 20mg/mL (n=5) or vehicle control (n=5) by peri-tumor injection. All values were plotted as the average of the relative tumor volume in each group.*, P<0.05.
Discussion
ATC is characterized by extremely fast growing and undifferentiated features, which pose a major challenge to the current treatment modality for ATC patients. Despite multimodal approaches, ATC still carries a dismal prognosis and the median overall survival has not been improved during the last 50 years (25). To tackle this uniformly lethal disease, innovative strategies beyond conventional methods need to be developed (26). Here, we reported the Notch1 signaling pathway as a potential target of a new therapeutic strategy against ATC. In addition, resveratrol, a red wine polyphenol, was first documented here as a Notch1 signaling pathway activator capable of restoring cell differentiation in an ATC context.
Resveratrol was initially discovered as a potential cancer chemoprevention agent and has been documented to have chemotherapeutic activity in both hematological and solid tumors during the last decade (27–29). However, there is a lack of information about the effect of resveratrol on ATC. In the current study, we found that resveratrol inhibited ATC cell growth by both cell cycle arrest and induction of apoptosis at concentrations between 10–50μM. These finding are consistent with previous studies but with relatively lower effective doses than which was found before in other human malignancies including leukemia, breast and colon cancers (27,28,30,31). Furthermore, we observed that resveratrol treatment of 50mg/kg/day effectively suppressed ATC tumor growth in vivo with minimal side effect. Most of the in vivo studies using xenograft models showed the effective doses of resveratrol ranged from 2mg/kg to 100mg/kg (32,33). Serum resveratrol levels, documented in a mouse neuroblastoma model, were in the low micro-molar range (2–10 μM) after oral administration of 50mg/kg of the drug (33). Though plasma level of resveratrol in human after repeated administration of high doses is around micro-molar concentrations (17), the effective treatment doses in human could be achieved with enhanced drug bioavailability. We showed in our study that local administration of the drug by peri-tumor injection was very effective to reduce the tumor volume, suggesting the necessity to modify or engineer resveratrol into a more targeted formulation.
We observed a dynamic ATC cell death process corresponding to increasing resveratrol treatment at multiple time points. S-G2 transition arrest was a significant effect of treatment and was first noted around 24 hours after resveratrol treatment. Importantly, less than 15% of the cells underwent apoptosis even when treated with the highest dose 24 hours after treatment. The percentage of apoptotic cells significantly increased after 48 hours of the treatment, suggesting the failure of DNA repair and irreversible transition to apoptosis. This was reflected by the induction of the pro-apoptotic markers cleaved-PARP and cleaved-caspase3 with the concomitant decrease in anti-apoptotic markers Bcl-2 and Bcl-xL. Previously, resveratrol has been shown to induce cell cycle arrest or/and apoptosis in different cell lines including colon carcinoma, breast carcinoma, esophageal squamous carcinoma and neuroblastoma (29,33). Another study has revealed the dose- and treatment duration-dependent effect of resveratrol on DNA synthesis using a prostate cancer model. The prostate cancer cells were induced to enter S phase by resveratrol, but subsequent progression through S phase was limited by the inhibitory effect of resveratrol on DNA synthesis (34). Our observations were consistent with these studies while provided more detailed evidences on how resveratrol causes cell death in ATC.
Various pathways have been reported to be responsible for the cell death induced by resveratrol treatment (35). In our study, it was found that resveratrol activated Notch1 signaling in the ATC context. Consistent with two other studies (36,37), this indicates that the Notch1 pathway could be another important signaling cascade involved in resveratrol-induced cell growth inhibition. In one of our previous studies, genetic induction of Notch1in the thyroid cancer xenografts profoundly suppressed tumor growth (38). Notch1 signaling has been reported to suppress growth and induce apoptosis in B cell malignancies by targeting PARP1 (39,40). Other studies have also reported various mechanisms regarding how Notch1 is involved in apoptotic processes, which may occur through either direct interaction with members of the IAP family or via indirect crosstalk with other signaling pathways like the p53 pathway (41,42). Additionally, it has been shown that cell cycle arrest is also responsible for the Notch1-mediated growth suppression of cancer cells. Up-regulation of p21 and down-regulation of cyclin D1 were observed when NICD was over-expressed in well-differentiated thyroid cancer (13). Resveratrol is well-known for having a wide spectrum of targets including tyrosine kinases, MAPK family and SIRT signaling. One previous study has shown that resveratrol induces apoptosis in well-differentiated thyroid cancer cell lines via a MAPK- and p53-dependent mechanism (43). Therefore, the potent anti-tumor effect of resveratrol demonstrated here in ATC could be a result of the activation of Notch1 signaling together with other pathways, which can be either linked to Notch1 by crosstalk or capable of generating synergetic effects with Notch1. This was further evidenced by our current in vivo study. Resveratrol treatment was effective to suppress the tumor growth in both HTh7 and 8505C xenograft, considering the basal expression of Notch1 was different between these two cell lines.
Though Notch1 signaling may not be the only pathway responsible for ATC growth inhibition by resveratrol, it has been shown to be significantly involved in ATC cell re-differentiation. We showed that the expression of thyroid-specific genes including TTF1, TTF2, Pax8 and NIS were up-regulated in both ATC cell lines with resveratrol treatment. Similar finding has been demonstrated in a rat thyroid cell line, showing that resveratrol increases NIS expression and enhances iodide trapping, though the mechanisms are not fully elucidated (20). In our study, Notch1 siRNA totally abrogated the induction of TTF1 and Pax8 but not of TTF2. The up-regulation of NIS by resveratrol was also partially blocked in ATC cells by Notch1 siRNA. This evidence strongly suggests that resveratrol regulates thyrocyte re-differentiation through Notch1 signaling. It was found in a previous study that Notch1 pathway activation was required for appropriate morphogenesis and differentiation during mouse thyroid gland development (7,44). Moreover, over-expression of Notch1 in thyroid cancer cells restored thyroid-specific differentiation markers (7). These findings have also been corroborated by the fact that other Notch1 activating compounds like valproic acid (13,45), induced NIS expression in a variety of thyroid cancer cell lines (46,47). Importantly, we also found that resveratrol induced re-differentiation in those ATC cells that survived the treatment and escaped the cell death process, which implied that resveratrol could still be a treatment option for the drug-resistant ATCs in combination with either radioactive iodine ablation or traditional chemotherapy.
Taken together, resveratrol inhibits ATC cell growth via apoptosis and S phase cell cycle arrest with a relative low concentration. More importantly, resveratrol enhances re-differentiation in ATC cells, which is dependent upon the activation of Notch1 signaling. Our findings provide the first documentation for the role of resveratrol in ATC re-differentiation, suggesting that activation of Notch1 signaling could be a potential therapeutic strategy for ATC patients. Therefore, Notch1 activating compounds including resveratrol should be subjected to further clinical investigations.
Supplementary Material
Acknowledgments
Grant Support: American Cancer Society Research Scholar Grant (H. Chen); American Cancer Society MEN2 Thyroid Cancer Professorship (H. Chen); NIH RO1 CA109053 and RO1 CA121115 (H. Chen).
We would like to thank Jacob Eide for his help in reviewing initial drafts of this paper.
Footnotes
There were no potential conflicts of interest in preparing this manuscript.
References
- 1.Hundahl SA, Fleming ID, Fremgen AM, Menck HR. A National Cancer Data Base report on 53,856 cases of thyroid carcinoma treated in the U.S. 1985–1995 [see commetns] Cancer. 1998;83:2638–48. doi: 10.1002/(sici)1097-0142(19981215)83:12<2638::aid-cncr31>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- 2.Kitamura Y, Shimizu K, Nagahama M, Sugino K, Ozaki O, Mimura T, et al. Immediate causes of death in thyroid carcinoma: clinicopathological analysis of 161 fatal cases. J Clin Endocrinol Metab. 1999;84:4043–9. doi: 10.1210/jcem.84.11.6115. [DOI] [PubMed] [Google Scholar]
- 3.Greene FL, Page DL, Flemming ID. AJCC cancer staging manual. 6. New York: Springer-Verlag; 2002. Thyroid. [Google Scholar]
- 4.Ros P, Rossi DL, Acebron A, Santisteban P. Thyroid-specific gene expression in the multi-step process of thyroid carcinogenesis. Biochimie. 1999;81:389–96. doi: 10.1016/s0300-9084(99)80086-8. [DOI] [PubMed] [Google Scholar]
- 5.Pasieka JL. Anaplastic thyroid cancer. Curr Opin Oncol. 2003;15:78–83. doi: 10.1097/00001622-200301000-00012. [DOI] [PubMed] [Google Scholar]
- 6.Park JW, Clark OH. Redifferentiation therapy for thyroid cancer. Surg Clin North Am. 2004;84:921–43. doi: 10.1016/j.suc.2004.01.005. [DOI] [PubMed] [Google Scholar]
- 7.Ferretti E, Tosi E, Po A, Scipioni A, Morisi R, Espinola MS, et al. Notch signaling is involved in expression of thyrocyte differentiation markers and is down-regulated in thyroid tumors. J Clin Endocrinol Metab. 2008;93:4080–7. doi: 10.1210/jc.2008-0528. [DOI] [PubMed] [Google Scholar]
- 8.Kopan R, Ilagan MX. The canonical Notch signaling pathway: unfolding the activation mechanism. Cell. 2009;137:216–33. doi: 10.1016/j.cell.2009.03.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ellisen LW, Bird J, West DC, Soreng AL, Reynolds TC, Smith SD, et al. TAN-1, the human homolog of the Drosophila notch gene, is broken by chromosomal translocations in T lymphoblastic neoplasms. Cell. 1991;66:649–61. doi: 10.1016/0092-8674(91)90111-b. [DOI] [PubMed] [Google Scholar]
- 10.Murtaugh LC, Stanger BZ, Kwan KM, Melton DA. Notch signaling controls multiple steps of pancreatic differentiation. Proc Natl Acad Sci U S A. 2003;100:14920–5. doi: 10.1073/pnas.2436557100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kunnimalaiyaan M, Vaccaro AM, Ndiaye MA, Chen H. Overexpression of the NOTCH1 intracellular domain inhibits cell proliferation and alters the neuroendocrine phenotype of medullary thyroid cancer cells. J Biol Chem. 2006;281:39819–30. doi: 10.1074/jbc.M603578200. [DOI] [PubMed] [Google Scholar]
- 12.Hanlon L, Avila JL, Demarest RM, Troutman S, Allen M, Ratti F, et al. Notch1 functions as a tumor suppressor in a model of K-ras-induced pancreatic ductal adenocarcinoma. Cancer Res. 2010;70:4280–6. doi: 10.1158/0008-5472.CAN-09-4645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Xiao X, Ning L, Chen H. Notch1 mediates growth suppression of papillary and follicular thyroid cancer cells by histone deacetylase inhibitors. Mol Cancer Ther. 2009;8:350–6. doi: 10.1158/1535-7163.MCT-08-0585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pinchot SN, Jaskula-Sztul R, Ning L, Peters NR, Cook MR, Kunnimalaiyaan M, et al. Identification and validation of Notch pathway activating compounds through a novel high-throughput screening method. Cancer. 2011;117:1386–98. doi: 10.1002/cncr.25652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jang M, Cai L, Udeani GO, Slowing KV, Thomas CF, Beecher CW, et al. Cancer chemopreventive activity of resveratrol, a natural product derived from grapes. Science. 1997;275:218–20. doi: 10.1126/science.275.5297.218. [DOI] [PubMed] [Google Scholar]
- 16.Belleri M, Ribatti D, Savio M, Stivala LA, Forti L, Tanghetti E, et al. alphavbeta3 Integrin-dependent antiangiogenic activity of resveratrol stereoisomers. Mol Cancer Ther. 2008;7:3761–70. doi: 10.1158/1535-7163.MCT-07-2351. [DOI] [PubMed] [Google Scholar]
- 17.Brown VA, Patel KR, Viskaduraki M, Crowell JA, Perloff M, Booth TD, et al. Repeat dose study of the cancer chemopreventive agent resveratrol in healthy volunteers: safety, pharmacokinetics, and effect on the insulin-like growth factor axis. Cancer Res. 2010;70:9003–11. doi: 10.1158/0008-5472.CAN-10-2364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Oi N, Jeong CH, Nadas J, Cho YY, Pugliese A, Bode AM, et al. Resveratrol, a red wine polyphenol, suppresses pancreatic cancer by inhibiting leukotriene Ahydrolase. Cancer Res. 70:9755–64. doi: 10.1158/0008-5472.CAN-10-2858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Subramanian L, Youssef S, Bhattacharya S, Kenealey J, Polans AS, van Ginkel PR. Resveratrol: challenges in translation to the clinic--a critical discussion. Clin Cancer Res. 16:5942–8. doi: 10.1158/1078-0432.CCR-10-1486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sebai H, Hovsepian S, Ristorcelli E, Aouani E, Lombardo D, Fayet G. Resveratrol increases iodide trapping in the rat thyroid cell line FRTL-5. Thyroid. 20:195–203. doi: 10.1089/thy.2009.0171. [DOI] [PubMed] [Google Scholar]
- 21.Schweppe RE, Klopper JP, Korch C, Pugazhenthi U, Benezra M, Knauf JA, et al. Deoxyribonucleic acid profiling analysis of 40 human thyroid cancer cell lines reveals cross-contamination resulting in cell line redundancy and misidentification. J Clin Endocrinol Metab. 2008;93:4331–41. doi: 10.1210/jc.2008-1102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Phan T, Yu XM, Kunnimalaiyaan M, Chen H. Antiproliferative effect of chrysin on anaplastic thyroid cancer. J Surg Res. 2011;170:84–8. doi: 10.1016/j.jss.2011.03.064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sippel RS, Carpenter JE, Kunnimalaiyaan M, Lagerholm S, Chen H. Raf-1 activation suppresses neuroendocrine marker and hormone levels in human gastrointestinal carcinoid cells. Am J Physiol Gastrointest Liver Physiol. 2003;285:G245–54. doi: 10.1152/ajpgi.00420.2002. [DOI] [PubMed] [Google Scholar]
- 24.Kogai T, Taki K, Brent GA. Enhancement of sodium/iodide symporter expression in thyroid and breast cancer. Endocr Relat Cancer. 2006;13:797–826. doi: 10.1677/erc.1.01143. [DOI] [PubMed] [Google Scholar]
- 25.Smallridge RC, Copland JA. Anaplastic thyroid carcinoma: pathogenesis and emerging therapies. Clin Oncol (R Coll Radiol) 2010;22:486–97. doi: 10.1016/j.clon.2010.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Are C, Shaha AR. Anaplastic thyroid carcinoma: biology, pathogenesis, prognostic factors, and treatment approaches. Ann Surg Oncol. 2006;13:453–64. doi: 10.1245/ASO.2006.05.042. [DOI] [PubMed] [Google Scholar]
- 27.Clement MV, Hirpara JL, Chawdhury SH, Pervaiz S. Chemopreventive agent resveratrol, a natural product derived from grapes, triggers CD95 signaling-dependent apoptosis in human tumor cells. Blood. 1998;92:996–1002. [PubMed] [Google Scholar]
- 28.Ahmad N, Adhami VM, Afaq F, Feyes DK, Mukhtar H. Resveratrol causes WAF-1/p21-mediated G(1)-phase arrest of cell cycle and induction of apoptosis in human epidermoid carcinoma A431 cells. Clin Cancer Res. 2001;7:1466–73. [PubMed] [Google Scholar]
- 29.Joe AK, Liu H, Suzui M, Vural ME, Xiao D, Weinstein IB. Resveratrol induces growth inhibition, S-phase arrest, apoptosis, and changes in biomarker expression in several human cancer cell lines. Clin Cancer Res. 2002;8:893–903. [PubMed] [Google Scholar]
- 30.Schneider Y, Vincent F, Duranton B, Badolo L, Gosse F, Bergmann C, et al. Anti-proliferative effect of resveratrol, a natural component of grapes and wine, on human colonic cancer cells. Cancer Lett. 2000;158:85–91. doi: 10.1016/s0304-3835(00)00511-5. [DOI] [PubMed] [Google Scholar]
- 31.Nakagawa H, Kiyozuka Y, Uemura Y, Senzaki H, Shikata N, Hioki K, et al. Resveratrol inhibits human breast cancer cell growth and may mitigate the effect of linoleic acid, a potent breast cancer cell stimulator. J Cancer Res Clin Oncol. 2001;127:258–64. doi: 10.1007/s004320000190. [DOI] [PubMed] [Google Scholar]
- 32.Tseng SH, Lin SM, Chen JC, Su YH, Huang HY, Chen CK, et al. Resveratrol suppresses the angiogenesis and tumor growth of gliomas in rats. Clin Cancer Res. 2004;10:2190–202. doi: 10.1158/1078-0432.ccr-03-0105. [DOI] [PubMed] [Google Scholar]
- 33.van Ginkel PR, Sareen D, Subramanian L, Walker Q, Darjatmoko SR, Lindstrom MJ, et al. Resveratrol inhibits tumor growth of human neuroblastoma and mediates apoptosis by directly targeting mitochondria. Clin Cancer Res. 2007;13:5162–9. doi: 10.1158/1078-0432.CCR-07-0347. [DOI] [PubMed] [Google Scholar]
- 34.Kuwajerwala N, Cifuentes E, Gautam S, Menon M, Barrack ER, Reddy GP. Resveratrol induces prostate cancer cell entry into s phase and inhibits DNA synthesis. Cancer Res. 2002;62:2488–92. [PubMed] [Google Scholar]
- 35.Pirola L, Frojdo S. Resveratrol: one molecule, many targets. IUBMB Life. 2008;60:323–32. doi: 10.1002/iub.47. [DOI] [PubMed] [Google Scholar]
- 36.Lin H, Xiong W, Zhang X, Liu B, Zhang W, Zhang Y, et al. Notch-1 activation-dependent p53 restoration contributes to resveratrol-induced apoptosis in glioblastoma cells. Oncol Rep. 2011;26:925–30. doi: 10.3892/or.2011.1380. [DOI] [PubMed] [Google Scholar]
- 37.Davis RJ, Pinchot S, Jarjour S, Kunnimalaiyaan M, Chen H. Resveratrol-Induced Notch Activation Potentially Mediates Autophagy in Human Follicular Thyroid Cancer Cells. J Surg Res. 2010;158:331. [Google Scholar]
- 38.Jaskula-Sztul R, Pisarnturakit P, Landowski M, Chen H, Kunnimalaiyaan M. Expression of the active Notch1 decreases MTC tumor growth in vivo. J Surg Res. 2011;171:23–7. doi: 10.1016/j.jss.2011.03.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zweidler-McKay PA, He Y, Xu L, Rodriguez CG, Karnell FG, Carpenter AC, et al. Notch signaling is a potent inducer of growth arrest and apoptosis in a wide range of B-cell malignancies. Blood. 2005;106:3898–906. doi: 10.1182/blood-2005-01-0355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kannan S, Fang W, Song G, Mullighan CG, Hammitt R, McMurray J, et al. Notch/HES1-mediated PARP1 activation: a cell type-specific mechanism for tumor suppression. Blood. 2011;117:2891–900. doi: 10.1182/blood-2009-12-253419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Liu WH, Hsiao HW, Tsou WI, Lai MZ. Notch inhibits apoptosis by direct interference with XIAP ubiquitination and degradation. EMBO J. 2007;26:1660–9. doi: 10.1038/sj.emboj.7601611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Yang X, Klein R, Tian X, Cheng HT, Kopan R, Shen J. Notch activation induces apoptosis in neural progenitor cells through a p53-dependent pathway. Dev Biol. 2004;269:81–94. doi: 10.1016/j.ydbio.2004.01.014. [DOI] [PubMed] [Google Scholar]
- 43.Shih A, Davis FB, Lin HY, Davis PJ. Resveratrol induces apoptosis in thyroid cancer cell lines via a MAPK- and p53-dependent mechanism. J Clin Endocrinol Metab. 2002;87:1223–32. doi: 10.1210/jcem.87.3.8345. [DOI] [PubMed] [Google Scholar]
- 44.Carre A, Rachdi L, Tron E, Richard B, Castanet M, Schlumberger M, et al. Hes1 is required for appropriate morphogenesis and differentiation during mouse thyroid gland development. PLoS One. 2011;6:e16752. doi: 10.1371/journal.pone.0016752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Greenblatt DY, Cayo MA, Adler JT, Ning L, Haymart MR, Kunnimalaiyaan M, et al. Valproic acid activates Notch1 signaling and induces apoptosis in medullary thyroid cancer cells. Ann Surg. 2008;247:1036–40. doi: 10.1097/SLA.0b013e3181758d0e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Fortunati N, Catalano MG, Arena K, Brignardello E, Piovesan A, Boccuzzi G. Valproic acid induces the expression of the Na+/I- symporter and iodine uptake in poorly differentiated thyroid cancer cells. J Clin Endocrinol Metab. 2004;89:1006–9. doi: 10.1210/jc.2003-031407. [DOI] [PubMed] [Google Scholar]
- 47.Puppin C, Passon N, Hershman JM, Filetti S, Bulotta S, Celano M, et al. Cooperative effects of SAHA and VPA on NIS gene expression and proliferation of thyroid cancer cells. J Mol Endocrinol. 2012;48:217–27. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.