Abstract
Purpose
South African adolescents have high HIV risk, yet few prevention interventions are effective. Parents play a pivotal role in youths’ healthy sexual development and may be at-risk themselves. We tested whether Let’s Talk!, a worksite-based parenting program, improves parent-child communication about HIV and sexual health, and parent condom use self-efficacy and behavior.
Methods
We culturally adapted Let’s Talk! in two languages, drawing on formative research and community stakeholder input. We then conducted a small randomized test at a large public worksite in Cape Town. The intervention consisted of five weekly two-hour group sessions for parents of youth aged 11–15. Sixty-six parents [64% female] and their 64 adolescents [41% female] completed surveys before and 1–2 weeks post-intervention; surveys assessed comfort with talking about sex, communication about 16 HIV- and sex-related topics, and parents’ condom use self-efficacy and behavior. Thirty-four Black-African (Xhosa-language) and 32 Coloured (mixed-race; Afrikaans-language) parent-child dyads participated. Parents were randomized to intervention (n=34) and control (n=32) groups; randomization was stratified by language.
Results
Multivariate regressions indicated that the intervention significantly increased parents’ comfort with talking to their adolescent about sex, b(SE)=0.98(0.39), p=0.02, and the number of sex- and HIV-related topics discussed with their adolescent, b(SE)=3.26(1.12), p=0.005. Compared to control parents, intervention parents were more likely to discuss new sex- and HIV-related topics not discussed before the intervention, b(SE)=2.85(0.80), p<.001. The intervention significantly increased parents’ self-efficacy for condom use, b(SE)=0.60(0.21), p=0.007.
Conclusions
Let’s Talk! holds promise for improving parent-child communication, a critical first step in preventing HIV among youth.
Keywords: South Africa, HIV, adolescents, parents, communication
Introduction
HIV prevalence in South Africa is among the highest in the world, with young people especially affected. About 17% of 15–49-year-olds in South Africa are living with HIV,1 with significant disparities between races. Rates are highest among Black Africans (14% overall prevalence, 33% antenatal prevalence) compared with those who are Coloured (i.e., mixed race; 2% overall prevalence, 7% antenatal prevalence) and White (<1% overall prevalence, 3% antenatal prevalence).2,3 HIV prevalence is relatively low among 10–14-year-olds, but increases sharply among older youth and young adults, particularly females.4 On average, South African adolescents initiate sexual intercourse at age 16.7 years; less than 5% have had sex before age 15.5
HIV prevention interventions for young adolescents could help teach safer sexual habits prior to sexual debut. However, many efforts to reduce HIV among South African youth—via national campaigns and school education—have had limited success.6–8 In South Africa, only one middle school intervention showed effects on reducing unprotected vaginal intercourse 12-months post-intervention in a randomized controlled trial.9
Parents can play a pivotal role in promoting adolescents’ sexual health and reducing risk behaviors; specifically, they can engage in ongoing communication about sex, which has been associated with lower sexual risk in some sub-Saharan African studies.10–12 However, efforts to prevent HIV among youth in South Africa and globally generally have not included parents,13 and many parents in South Africa avoid addressing sexual issues,11,14 especially condom use.11,15 When communication occurs, it is commonly perceived to be prescriptive and judgmental.11 One community-based parenting intervention in South Africa (CHAMP, the Collaborative HIV Prevention and Adolescent Mental Health Program), led to improvements in parent-reported frequency and comfort in discussing HIV and sex with adolescents.16 Such work shows promise in involving parents in prevention efforts.
Worksites are a promising yet untested setting in which to develop HIV prevention parenting programs. School-based interventions do not reach parents or truant adolescents (who may be most at-risk); and community interventions may not readily reach employed parents, who may have challenges with transport, scheduling, and childcare. Worksite programs overcome common challenges for reaching and engaging parents, who must make a special effort to attend programs in community settings. Moreover, in South Africa, the Department of Labour recommends that all worksites provide educational HIV programs for employees–and many employers, including almost all large worksites, already provide such programs.17,18 An additional motivation for employers to implement prevention programs is that workers with HIV have decreased productivity, and increased absenteeism, medical costs, and replacement costs.19,20 Despite the potential positive impact, worksite programs have not been rigorously evaluated,17 and no such programs have targeted parents.
A parenting program could have beneficial effects for parents as well as their adolescents. South African adults are often reluctant to attend HIV prevention programs because of the associated stigma, although they may still be at high risk: HIV prevalence among the employed in South Africa is estimated to be 10–25%.20–22 A program focused on adolescents and family relationships may be more attractive to parents than a program solely focused on adult HIV prevention, thereby promoting the health of both generations.
We conducted a randomized pilot test to examine whether Let’s Talk!, a worksite-based HIV prevention program for parents, could improve parent-child communication about HIV and sexual health. We hypothesized that Let’s Talk! would enhance parent-child communication, including prompting more parent-child conversations about HIV and sex. We also hypothesized that the program could lead to changes in parents themselves, including encouraging greater self-efficacy for condom use and greater condom use behavior.
Methods
Intervention Setting and Community Partnership
This study was conducted in the municipal Cape Town City Council (hereafter referred to as “City”) worksites in the Western Cape province, which is 27% Black African, 54% Coloured, and 18% White. Official City languages are English, isiXhosa (spoken by the majority of Black Africans in the Western Cape), and Afrikaans (spoken by people who are Coloured). The City is Cape Town’s largest employer, with a workforce of ~22,000 across multiple locations. We trained study facilitators from the City’s pool of HIV peer educators.23
Consistent with principles of community-based participatory research (CBPR),24 the City was an engaged and equal partner throughout the research process, from formative intervention development research to intervention implementation. The community-academic study team also partnered with a community advisory board (CAB) composed of worksite representatives and staff at community-based organizations that emphasized adolescent, parent, and/or family social services, and HIV prevention. The CAB met at key points during the project to contribute to culturally relevant intervention adaptation, help interpret results, and provide feedback regarding intervention acceptability, feasibility, and sustainability.
Study Design
We evaluated Let’s Talk! with two intervention and two wait-list control groups of parents/caregivers (hereafter referred to as “parents”), stratified by language (Afrikaans vs. isiXhosa). Randomization was conducted following baseline assessment at the individual parent level, within worksite; parents entered the intervention ~one-week post-baseline. Parents and adolescents were surveyed at baseline and ~two-months post-baseline (one-to-two weeks after the end of the five week-intervention).
Intervention Protocol
The intervention consisted of five weekly two-hour group sessions for parents of adolescents aged 11–15; each group consisted of ~15 parents. As is standard for the City’s HIV prevention programming for employees, parents were released from work for the sessions. The program was standardized and manualized across groups, and each group was led by a trained facilitator and co-facilitator who were City peer HIV educators.
Training consisted of two five-day workshops led by a doctoral-level clinical psychologist who modeled the program sessions and taught motivational interviewing principles25 (i.e., a nonconfrontational style emphasizing open-ended questions, and reflective listening, as well as exploration of ambivalence about communication with adolescents about sex), for facilitators to use when interacting with and teaching parents.
Using formative qualitative research, worksite partner and CAB input, and data from a pretest-posttest process evaluation of one pilot intervention group, the program’s content and structure were culturally adapted from Talking Parents, Healthy Teens (TPHT), a successful US-based program that led to improved parent-child communication about sex.26,27 For example, to fit into the basic structure of HIV prevention worksite workshops, the sessions were reorganized into weekly two-hour sessions over five weeks, rather than the eight one-hour lunchtime sessions that were better-suited to US worksites. A session was added on HIV (to replace part of a session on sexually transmitted infections in the US), and assertiveness skills were emphasized, given South Africa’s high sexual violence rates.28 To accommodate lower-literacy employees, program material was primarily conveyed verbally, fewer written materials were disseminated, pictures were added to written materials, and take-home activities were modified to allow children to scribe written portions. In addition, didactic material was shortened and discussion time was lengthened. Overall, all of the original US program skills were maintained because stakeholders felt that they were transferable to the South African context. Moreover, community stakeholders universally agreed that an HIV prevention parenting intervention was critically needed and culturally acceptable.
Table 1 shows a program description. In each of the first four sessions, parents learned two new communication skills. Parents had opportunities to practice each skill in a role play with another parent and in a take-home activity with their child. Parents also engaged in a facilitator-led group discussion on a topic relevant to that week’s content. In the fifth session, parents practiced all skills using role-plays.
Table 1.
Let’s Talk! Program Session Outline
| Session | Communication Skill | Weekly Take-Home Activities |
|---|---|---|
|
1. Building Your Relationship with Your Child Focus: Teaching parents the importance of communication; learning new skills to promote open dialogue with adolescents. |
Five Strategies to Encourage Adolescents to Talk. Facilitating communication with adolescents using verbal and nonverbal techniques. Catching Your Child Doing Something Good. Reinforcing adolescents’ strengths by noticing and commenting on a positive behavior. Also covered: Reinforcing appropriate supervision |
Parents 1. Use five strategies to encourage child to talk. 2. Catch child doing two things that parent likes. |
|
2. Talking about Sensitive Topics Focus: Identifying personal attitudes regarding conversations about sex; overcoming fears of talking to adolescents about sex and HIV. |
Thinking of Your Opening Line Ahead of Time. Practicing how to start conversations about sex in advance. Overcoming Your Adolescent’s Reluctance to Talk about Sex. Surmounting roadblocks to positive communication about sex. Also covered: Using teaching moments to begin conversations about sex & HIV; Thinking from the teen’s perspective: reasons for and against having sex. |
Parents: 1. Use teaching moments and opening lines to start a conversation about a sensitive topic with child. 2. Have a conversation with child about reasons for and against having sex. |
|
3. Talking about HIV & Condoms Focus: Understanding and discussing HIV stigma and empathy; reviewing the steps of proper condom use. |
How to Use a Condom. Reviewing the steps of correct condom use and learning how to teach child these steps. Also covered: Facts and myths about HIV; Learning about HIV stigma and empathy; Tips for talking with adolescents about HIV. |
Parents:1. Play and discuss an HIV facts game with child. 2. Play a game about proper condom use and related obstacles to condom use with child. |
|
4. Building Assertiveness Skills Focus: Learning ways to empower adolescents to firmly exercise their view-points and respect the view-points of others. |
Teach Your Child Alternative Actions and Delay Tactics. Learning to teach child how to exit a pressure situation by offering a different activity and cooling down a situation. Avoiding Sex Without Condoms. Discussing strategies for applying assertiveness skills sexual situations to ensure condom use partner. Also covered: Help your child say “no” peer pressure; Teaching respect. |
Parents: 1. Teach assertiveness skills to child through role- play exercise and follow-up questions. 2. Ask child questions to stimulate discussion about what “no” means and how to respect that decision. |
|
5. Putting It All Together & Staying Motivated Focus: Reviewing skills learned and exploring barriers & motivators for using the skills. |
Review. Parents review and role-play all of the skills taught in the program, and identify the next conversation they will have with their child on sex and HIV; parents are encouraged to stay in touch with one another. |
One observer, as well as the facilitator and co-facilitator, rated the coverage of manual topics in each session; across ratings and sessions, facilitators averaged 97% (SD=5%) of topics covered in the Afrikaans sessions and 89% (SD=16%) of topics covered in the Xhosa sessions. On a feedback form given to parents after each session, parents rated the session on a scale from 1, thumbs down, to 5, thumbs up; average ratings were high across Afrikaans (M=4.96, SD=0.19) and isiXhosa (M=4.87, SD=0.58) sessions. Across all sessions, parents provided 103 general comments in response to an open-ended question on the form. Nearly all (n=94; 91%) comments were favorable (“educational,” “excellent,” “engaging”), two were negative (“[teaching about condoms] can make a child think he is supposed to do sex”), and the remainder were neutral (“I’m thinking of doing [the skill] today”).
Translation
Study materials (manual, surveys, handouts, etc.) were translated by one isiXhosa and one Afrikaans-speaking team member experienced with regional variations in language use and colloquialisms. Other native-speaking team members reviewed all final documents to ensure linguistic and cultural accuracy. Facilitators suggested additional revisions to the wording.
Participant Recruitment
Parents of 11–15-year-olds were recruited from five City departments (Solid Waste, Roads and Stormwater, Municipal Libraries, Electricity Maintenance, Parks and Recreation) across seven worksite regions (Crossroads, Delft, Gugulethu, Mitchells Plain, Nyanga, Phillipi, Strandfontein) via on-site informational sessions provided by the study team, as well as fliers and emails disseminated by site managers. Employees were eligible if they had ≥1 child aged 11–15-years-old who resided with them ≥2 days per week. Interested parents contacted the study team and were screened for eligibility; eligible parents provided written informed consent for themselves and written permission for their adolescent to be interviewed at home or by phone; adolescents provided assent.
Sixty-six parents [64% male, mean age 43 years (SD=7), range 23–59] and their 66 adolescents [44% girls; mean age 13 years (SD=1), range 11–15] participated, which included 34 isiXhosa-speaking and 32 Afrikaans-speaking parent-child dyads; seven parents were non-biological (four step-parents, three relatives). Thirty-four parents were randomized to the intervention group and 32 parents to the control group. Of those assigned to the intervention group, 68% of parents attended session 1, 76% session 2, 74% session 3, 71% session 4, and 82% session 5. In addition, 73% attended 4–5 sessions, 15% attended 2–3 sessions, 3% attended 1 session, and 9% attended no sessions.
Data Collection
Most parents (n=52) completed audio-computer-assisted self-interviews (ACASI) at the worksite; 14 completed surveys at home, due to scheduling difficulties. Study staff conducted face-to-face interviews with 63 adolescents whom parents had selected to participate in the assessment; due to scheduling issues, 3 were interviewed by telephone. All 66 parents, and 64 of the 66 adolescents, responded to the follow-up survey; two adolescents could not be reached at follow-up.
Parents and adolescents could choose to be surveyed in English or their native language (Afrikaans or Xhosa). Parents received 100 Rand (~US $15) and adolescents selected a small gift (e.g., soccer ball) for participation in each survey. Boston Children’s Hospital and Stellenbosch University institutional review boards approved the research.
Survey Content
Adaptation
Survey content was based on constructs used in TPHT. Prior to translation, we adapted, added, or dropped items based on qualitative interviews with parents and adolescents, as well as a pretest-posttest process evaluation of one intervention group. South African team members, including native isiXhosa and Afrikaans speakers, reviewed the final survey for cultural relevance and acceptability.
Socio-demographic covariates
Parents reported their age, gender, education (highest completed grade), occupation (job title), whether they lived with a partner (as married or unmarried), and their relationship to the child (e.g., biological parent, grandparent). Parents also reported age and gender of the target child whom they selected to participate in the assessment. We used the Hollingshead four factor social status index to assess socio-economic status (SES) 29; lower scores on its range of 8–66 indicate lower social status. It has been significantly correlated with the Household Economic and Social Status Index, a measure validated for South Africa.30 The Hollingshead index typically includes parents’ and co-parents’ occupation; due to insufficient information, we used index parent occupation only.
Communication about HIV and sex
Parents reported whether they had ever discussed each of 16 topics related to HIV and sex with the target child (see Table 4); adolescents reported whether they had ever discussed these topics with the index parent. Topics were drawn from Let’s Talk!’s session content and modeled after a similar TPHT measure. Responses were summed and coded as number of topics discussed at baseline and follow-up, and number of new topics discussed at follow-up that had not been discussed at baseline. Baseline internal reliabilities were strong (parent α=92; adolescent α=.86).
Comfort talking about sex
Let’s Talk! aims to increase parents’ comfort in talking with their child about sex, by providing practice through role plays and suggesting strategies (e.g., how to open the conversation using “opening lines” and identifying “teaching moments,” such as a dating scene in a television show). To examine this aspect of Let’s Talk!, we adapted one item from the Speaking Extent and Comfort Scale (SPEACS)31, which assesses general comfort with conversations with different people in one’s network; we adapted the SPEACS to measure comfort with talking about sex with one’s adolescent (for parents) and with one’s parent (for adolescents): “Please indicate the number that best describes how comfortable you feel, in general, when you talk with this child/parent about sex” with response options 1, not at all comfortable to 7, very comfortable.
Parents’ self-efficacy for condom use and condom use behaviors
We used a 7-item scale32 to assess condom use self-efficacy, or parents’ confidence in being able to use a condom in a variety of situations (α=.80). A sample item is: “How sure are you that you would be able to use a condom every time that you had sexual intercourse?” with response options 1=not at all sure, 2=a little sure, 3=somewhat sure, 4=pretty sure, and 5=very sure. Parents were also asked the number of times that they had vaginal and anal sex in the past three months, and of those times, the number of times that a condom was used; we derived a dichotomous variable of no condom use vs. any condom use across sexual acts. Similar sexual behaviour measures have been used in prior South African research.33
Statistical Analysis
For each continuous parent and child outcome, we conducted a multivariate linear regression predicting the outcome with intervention group (intervention vs. control), baseline value of the outcome variable, and language (isiXhosa vs. Afrikaans). For condom use, a dichotomous outcome, we used logistic regression. To test for covariates, we added each socio-demographic characteristic one at a time to this basic model; socio-demographic characteristics that were significantly (p<.05) associated with any of the outcomes were added to the basic model.
In follow-up exploratory analyses, we used logistic regression models to test whether parent-child communication on each of the 16 discussion topics changed as a result of the intervention (i.e., whether any of the topics were more likely to be discussed post-intervention in the intervention vs. control group); models predicted whether each topic was discussed post-intervention with intervention group (intervention vs. control), baseline value of whether the topic was discussed, and language.
Because none of the child outcomes significantly changed as a result of the intervention (as shown in Table 3), they will not be discussed further.
Results
Participants
All 66 parents who expressed interest after the worksite presentations about eligibility criteria were found to be eligible. All parents gave consent to contact their adolescent for the study, and all 66 adolescents participated at baseline. The intervention and control groups did not significantly differ on socio-demographic characteristics (Table 2).
Table 2.
Baseline Participant Characteristics by Treatment Group
| Intervention (n=34) | Control (n=32) | Total (n=66) | |
|---|---|---|---|
| Parent gender (Female) | 35% | 38% | 36% |
| Child gender (Female) | 38% | 50% | 44% |
| Live with Partner | 71% | 66% | 68% |
| Biological Parent | 88% | 91% | 89% |
| Parent Age | M=43.9, SD=6.5 | M=42.8, SD=8.0 | M=43.3, SD=7.2 |
| Child Age | M=12.7, SD=1.1 | M=12.8, SD=1.4 | M=12.8, SD=1.3 |
| Socio-economic Status1 | M=27.8, SD=10.9 | M=25.7, SD=12.4 | M=26.8, SD=11.6 |
Note: Based on Fisher's exact tests (for dichotomous characteristics) and t-tests (for continuous characteristics), no significant differences emerged in baseline demographic data between groups (all p-values>0.05).
Socio-economic status as assessed by the Hollingshead Index29
Communication about Sex and HIV
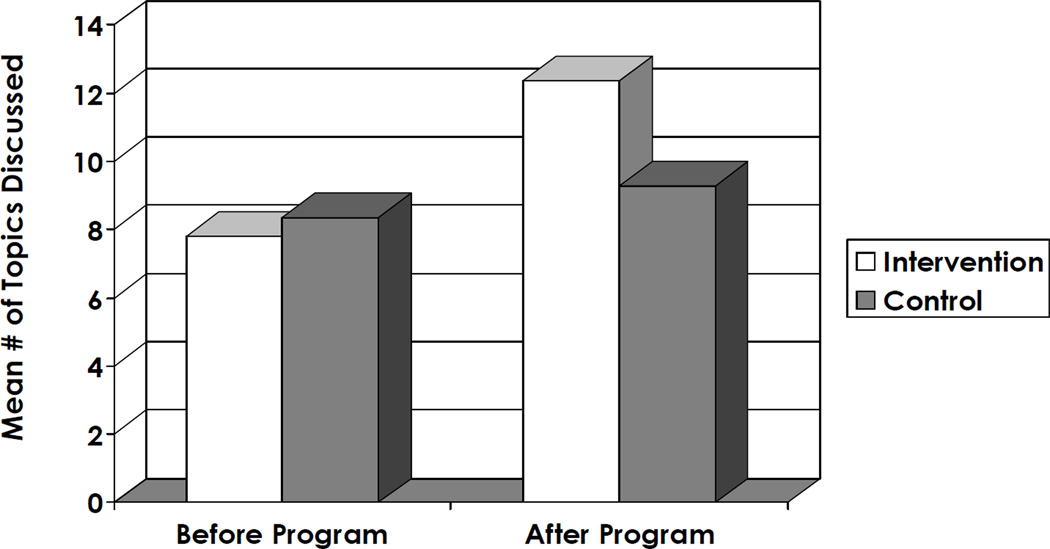
Sum of topics discussed
Table 3 shows the coefficients for the intervention indicator for number of topics discussed, and Figure 1 depicts the average number of topics discussed at both time-points in the intervention and control groups. A significant intervention effect indicated that the number of topics discussed since baseline was significantly larger for intervention parents than for control parents. At baseline, means did not differ between intervention parents (M=7.8, SD=4.8) and control parents (M=8.3, SD=5.7), p=.34. After the intervention, intervention parents reported discussing an average of 12.4 (SD=4.3) topics with their adolescent, while control parents reported an average of 9.3 (SD=5.7) topics. The difference between the pre-to-post increases in the intervention means versus the control means was significant (p = .005). The number of new topics discussed since baseline–that had not been discussed before the start of the intervention–was greater among intervention parents (M=5.9, SD=4.7) than control parents (M=2.8, SD=3.6), p<.001.
Table 3.
Effects of Let's Talk! on Parent-Child Communication and Parent Condom Use Self-Efficacy (n=66 parents)
| Intervention (n=34) | Control (n=32) | Adjusted Coefficient |
Effect Size | ||||
|---|---|---|---|---|---|---|---|
| Pre M(SD) |
Post M(SD) |
Pre M(SD) |
Post M(SD) |
b(SE) | SD | P | |
| Parent Outcomes | |||||||
| Comfort Talking to Child about Sex | 3.4(1.8) | 5.0(1.7) | 4.1(2.1) | 4.3(1.9) | 1.0(0.4) | 0.5 | .015 |
| Number of Sex and HIV Topics Discussed | 7.8(4.8) | 12.4(4.3) | 8.3(5.7) | 9.3(5.7) | 3.3(1.1) | 0.6 | .005 |
| Number of New Sex and HIV Topics Discussed at Follow-Up | — | 5.9(4.7) | — | 2.8(3.6) | 2.9(0.8) | 0.6 | <001 |
| Self-Efficacy for Condom Use | 3.8(1.0) | 4.6(0.8) | 4.1(1.0) | 4.1(1.0) | 0.6(0.2) | 0.6 | .007 |
| Child Outcomes | |||||||
| Comfort Talking to Parent about Sex | 4.1(1.9) | 4.6(1.8) | 3.7(1.9) | 4.2(1.8) | 0.2(0.4) | 0.1 | .60 |
| Number of Sex and HIV Topics Discussed | 7.2(4.7) | 9.2(4.8) | 9.4(4.0) | 9.2(5.1) | 1.3(1.1) | 0.3 | .24 |
| Number of New Sex and HIV Topics Discussed at Follow-Up | — | 3.5(3.3) | — | 2.6(2.7) | 0.3(0.7) | 0.1 | .66 |
Note: Multivariate tests controlled for participants' primary language (Afrikaans vs. Xhosa) and for baseline value of the outcome. Models controlling for other parent and child socio-demographics (e.g., socio-economic status, age) yielded similar results.
Figure 1.
Parent Report of Number of Sex- and HIV-related Topics discussed with Adolescent at Baseline and Follow-up (n = 66 parents)
Specific topics discussed
As shown in Table 4, the intervention increased discussion on a number of topics. For example, intervention parents were nearly five times more likely to discuss the steps of condom use than were control parents; at baseline 35% of intervention parents and 34% of control parents had ever discussed the steps of condom use with their child, whereas 71% of intervention parents versus 38% of control parents did so after the baseline survey, p=.006.
Table 4.
Effect of Let's Talk! on Individual Topics Discussed by Parent with Child (n=66 parents)
| Control Group | Intervention Group | ||||
|---|---|---|---|---|---|
| Topic | % Discussed (Pre) |
% Discussed (Post) |
% Discussed (Pre) |
% Discussed (Post) |
Odds Ratio (95% Confidence Interval) |
| How children's bodies change physically as they grow up | 56 | 69 | 53 | 79 | 2.1(0.6,8.4) |
| How women get pregnant | 53 | 59 | 50 | 74 | 2.2(0.7,7.0) |
| How child will make decisions about whether or not to have sex | 47 | 50 | 35 | 79 | 4.3(1.4,13.2)* |
| What sex is | 56 | 66 | 38 | 76 | 2.1(0.7,6.8) |
| How to prevent pregnancy | 53 | 63 | 53 | 85 | 3.9(1.1, 13.7)* |
| How condoms can prevent HIV | 66 | 56 | 62 | 74 | 2.2(0.8,6.3) |
| Steps of how to use a condom | 34 | 38 | 35 | 71 | 5.0(1.6, 15.8)** |
| How to prevent getting HIV | 63 | 75 | 71 | 91 | 3.3(0.8,14.0) |
| What to do if partner doesn't want to use a condom | 41 | 47 | 47 | 74 | 3.1(1.1,9.0)* |
| Importance of not pressuring others to have sex | 38 | 63 | 44 | 85 | 3.6(1.0,12.9)* |
| Reasons why people like to have sex | 34 | 50 | 32 | 79 | 4.6(1.4, 15.0)* |
| Reasons why child should not have sex | 56 | 56 | 50 | 79 | 4.7(1.3, 17.6)* |
| How to say no if someone wants to have sex and your child doesn't want to | 56 | 53 | 38 | 71 | 3.3(1.0,10.8)* |
| Consequences of alcohol & drug use | 72 | 75 | 62 | 79 | 1.7(0.5,5.8) |
| How to recognize violence and abuse in relationships | 59 | 63 | 62 | 71 | 1.4(0.5,4.2) |
| Homosexuality/people being gay | 50 | 47 | 47 | 71 | 3.42(1.1, 10.9)* |
p<05
p<01
p<001
Note: results based on logistic regressions predicting discussion after baseline, controlling for language and whether the topic had ever been discussed prior to baseline.
Comfort talking about sex
As shown in Table 3, intervention parents felt more comfortable than control parents talking with their child about sex after, versus before, the intervention. On average, intervention parents (M=3.39, SD=1.84) and control parents (M=4.1, SD=2.2) had similar comfort ratings at baseline (p=.17), whereas intervention parents showed increased comfort (M=5.0, SD=1.7) post-intervention and control parents did not (M=4.3, SD=1.9), p=.02.
Condom use self-efficacy and behavior
The intervention led to greater self-efficacy for condom use among intervention parents, but not among control parents. Intervention parents showed increased self-efficacy from baseline (M=3.8, SD=1.0) to follow-up (M=4.6, SD=0.8), whereas control parents remained similar at both time points (baseline M=4.1, SD=1.0 vs. follow-up M=4.1, SD=1.0), p=.007. Results for condom use behavior were not significant, p=.30.
Discussion
Our randomized study – the first worksite-based HIV prevention intervention for parents in sub-Saharan Africa – suggests that Let’s Talk! had beneficial effects on parent-child communication. On average, parents in Let’s Talk! reported that they had broached an average of six new HIV- and sex-related topics with their adolescent following the intervention. Moreover, the intervention increased discussions specifically about condom use, a topic that has been reported to be uncommon in parent-adolescent conversations in sub-Saharan Africa.11 Although we did not measure long-term effects, our intervention increased parent-child communication – a protective factor that has been associated with lower sexual risk among adolescents in some studies in sub-Saharan Africa11 – and thus has the potential to reduce adolescents’ long-term risk.
Parents’ own self-efficacy for condom use increased following the intervention, showing that Let’s Talk!’s effects extend to parents as well as the parent-child relationship. Numerous studies, including in South Africa, have shown a significant relationship between self-efficacy for condom use and condom use behavior34,35; thus, these results are encouraging. However, our follow-up period was too short to assess whether the intervention’s effects on self-efficacy in turn led to greater condom use. In South Africa, both adults and adolescents are at high HIV risk, yet adults are reluctant to attend prevention programs or to get tested due to associated high stigma.36,37 A program for parents can help to de-stigmatize HIV by focusing parents on the need to protect their children, while simultaneously educating parents.
Importantly, our research was conducted as a partnership with the City’s peer educator program. We drew program facilitators from the worksite’s existing pool of peer HIV educators, and thus built worksite capacity for new HIV prevention programming, increasing the likelihood of sustainability. Worksite peer educators play a unique and promising grassroots role in the South African HIV epidemic:23 peer educators operate within worksite social networks to impart HIV knowledge into informal and formal exchanges.
Consistent with prior parenting intervention research in sub-Saharan Africa, our intervention had an effect on parents’ perceptions of parent-child communication11,16 but did not show an effect on adolescents’ perceptions. Due to the pilot nature of our study, the nonsignificant results are likely due to insufficient statistical power. A greater number of worksites, parents, and adolescents would be needed for a full effectiveness test. Moreover, adolescents received a weaker dose of the intervention compared to parents, as they did not directly participate in program sessions; thus a larger number of adolescents and a longer follow-up would be needed to show an effect. Intervention effects also may have been diluted by children talking with other adults (and not only the index parent), including close relatives, and by parents talking with other children (not only the index child). We also recognize the potential for parent perceptions to be influenced by social desirability: parents who took the program were likely to recognize the topics on the survey as ones covered in the sessions and may have wanted to show that they learned from the program. A larger randomized controlled trial is needed to measure effects of the intervention among all adolescents in the family; to determine whether youths’ close relationships with other adults weaken effects for parental communication; and to assess whether the findings for parents hold over time, when social desirability effects are likely to weaken.
Due to the generalized nature of the HIV epidemic in South Africa and the multiple factors that contribute to risk behaviors and biological transmission, any single approach to HIV prevention is unlikely to be sufficient. Multi-pronged, multi-level approaches are needed, which involve national, community, and school efforts alongside family-based interventions.38 Promising approaches have already been developed for schools, community agencies, and faith-based organizations.9,39,40 We believe that worksite-based parenting interventions should be added as one more strategy for the HIV prevention toolkit. A family-oriented worksite parenting approach can be valuable in complementing other efforts, through strengthening the home environment.
Acknowledgments
This research was supported by National Institute of Mental Health R34 MH090790 (LM Bogart, Principal Investigator). We would like to thank Rosalie Corona, PhD, Annemie Stewart, Nombeko Mpongo, Rebecca Nelwamondo, Hilton Redman, Ernest Daniels, Nomafu Jayiya, Riaan Keown, Paul Sheldon, Herman van der Watt, and Madeline Wachman for their contributions to the study.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Implications and Contribution: South African adolescents have high HIV risk, yet few interventions have been effective. We found that Let’s Talk!, a culturally tailored worksite-based HIV prevention parenting program, increased parents’ communication with their child about sex and HIV when tested in a large municipal South African worksite – a critical first step in preventing youths’ risk behavior.
Some of these data were presented at an oral poster discussion session at the XIX International AIDS Conference, July 2012, Washington DC.
References
- 1.Statistics South Africa. Mid-year population estimates. Pretoria, South Africa: 2011. [Google Scholar]
- 2.Shisana O, Rehle T, Simbayi LC, et al. South African national HIV prevalence, incidence, behaviour and communication survey 2008: A turning tide among teenagers? Cape Town, South Africa: HSRC Press; 2009. [Google Scholar]
- 3.Department of Health (South Africa) The 2010 National Antenatal Sentinel HIV and Syphilis Prevalence Survey in South Africa. Pretoria: South Africa; 2011. [Google Scholar]
- 4.UNAIDS. Global AIDS Response Progress Report 2012, Republic of South Africa. UNAIDS. 2012 [Google Scholar]
- 5.Pettifor AE, Levandowski BA, Macphail C, et al. A tale of two countries: rethinking sexual risk for HIV among young people in South Africa and the United States. J Adolesc Health. 2011;49(3):237–243. e1. doi: 10.1016/j.jadohealth.2010.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pettifor AE, MacPhail C, Bertozzi S, Rees HV. Challenge of evaluating a national HIV prevention programme: The case of loveLife, South Africa. Sex Transm Infect. 2007;83(suppl 1):i70–i74. doi: 10.1136/sti.2006.023689. [DOI] [PubMed] [Google Scholar]
- 7.Harrison A, Newell ML, Imrie J, Hoddinott G. HIV prevention for South African youth: which interventions work? A systematic review of current evidence. BMC Public Health. 2010;10:102. doi: 10.1186/1471-2458-10-102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jewkes R, Nduna M, Levin J, et al. Impact of stepping stones on incidence of HIV and HSV-2 and sexual behaviour in rural South Africa: cluster randomised controlled trial. BMJ. 2008;337:a506. doi: 10.1136/bmj.a506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jemmott JB, 3rd, Jemmott LS, O'Leary A, et al. School-based randomized controlled trial of an HIV/STD risk-reduction intervention for South African adolescents. Arch Pediatr Adolesc Med. 2010;164(10):923–929. doi: 10.1001/archpediatrics.2010.176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Peltzer K. Early sexual debut and associated factors among in-school adolescents in eight African countries. Acta Paediatr. 2010;99(8):1242–1247. doi: 10.1111/j.1651-2227.2010.01874.x. [DOI] [PubMed] [Google Scholar]
- 11.Bastien S, Kajula LJ, Muhwezi WW. A review of studies of parent-child communication about sexuality and HIV/AIDS in sub-Saharan Africa. Reprod Health. 2011;8:25. doi: 10.1186/1742-4755-8-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Biddlecom A, Awusabo-Asare K, Bankole A. Role of parents in adolescent sexual activity and contraceptive use in four African countries. Int Perspect Sex Reprod Health. 2009;35(2):72–81. doi: 10.1363/ipsrh.35.072.09. [DOI] [PubMed] [Google Scholar]
- 13.Lightfoot M. HIV prevention for adolescents: Where do we go from here? Am Psychol. 2012;67(8):661–671. doi: 10.1037/a0029831. [DOI] [PubMed] [Google Scholar]
- 14.Lebese RT, Davhana-Maselesele M, Obi CL. Sexual health dialogue between parents and teenagers: an imperative in the HIV/AIDS era. Curationis. 2010;33(3):33–42. doi: 10.4102/curationis.v33i3.5. [DOI] [PubMed] [Google Scholar]
- 15.Namisi FS, Flisher AJ, Overland S, et al. Sociodemographic variations in communication on sexuality and HIV/AIDS with parents, family members and teachers among in-school adolescents: a multi-site study in Tanzania and South Africa. Scand J Public Health. 2009;37(Suppl 2):65–74. doi: 10.1177/1403494808086986. [DOI] [PubMed] [Google Scholar]
- 16.Bell CC, Bhana A, Petersen I, et al. Building protective factors to offset sexually risky behaviors among black youths: a randomized control trial. J Natl Med Assoc. 2008;100(8):936–944. doi: 10.1016/s0027-9684(15)31408-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mahajan AP, Colvin M, Rudatsikira J-B, Ettl D. An overview of HIV/AIDS workplace policies and programmes in southern Africa. AIDS. 2007;21(suppl 3):S31–S39. doi: 10.1097/01.aids.0000279692.54029.a1. [DOI] [PubMed] [Google Scholar]
- 18.International Labour Organization. Department of Labour Employment Equity Act, Act No. 55 of 1998: Code of Good Practice on Key Aspects of HIV/AIDS and Employment. Geneva, Switzerland: 2000. [Google Scholar]
- 19.Mishra V, Medley A, Hong R, et al. Levels and spread of HIV seroprevalence and associated factors: Evidence from national household surveys. Calverton, MD: Macro International Inc.; 2009. [Google Scholar]
- 20.Rosen S, Feeley F, Connelly P, Simon J. The private sector and HIV/AIDS in Africa: taking stock in 6 years of applied research. AIDS. 2007;21(suppl 3):S41–S51. doi: 10.1097/01.aids.0000279693.61652.2d. [DOI] [PubMed] [Google Scholar]
- 21.Colvin M, Connolly C, Madurai L. The epidemiology of HIV in South African workplaces. AIDS. 2007;21(suppl 3):S13–S19. doi: 10.1097/01.aids.0000279690.69276.c9. [DOI] [PubMed] [Google Scholar]
- 22.Stevens W, Apostolellis A, Napier G, et al. HIV/AIDS prevalence testing -- merits, methodology and outcomes of a survey conducted at a large mining organisation in South Africa. S Afr Med J. 2006;96(2):134–139. [PubMed] [Google Scholar]
- 23.Dickinson D. Changing the Course of AIDS: Peer Education in South Africa and its Lessons for the Global Crisis. Ithaca, NY: Cornell University Press; 2009. [Google Scholar]
- 24.Bogart LM, Uyeda KE. Community-based participatory research: partnering with communities for effective and sustainable behavioral health interventions. Health Psychol. 2009;28(4):391–393. doi: 10.1037/a0016387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Miller W, Rollnick S. Motivational Interviewing: Preparing People for Change. 2nd ed. New York, NY: Guilford Press; 2002. [Google Scholar]
- 26.Schuster MA, Corona R, Elliott MN, et al. Evaluation of Talking Parents, Healthy Teens, a new worksite based parenting programme to promote parent-adolescent communication about sexual health: randomised controlled trial. BMJ. 2008;337(a308) doi: 10.1136/bmj.39609.657581.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Eastman KL, Corona R, Schuster MA. Talking Parents, Healthy Teens: A worksite-based program for parents to promote adolescent sexual health. Prev Chronic Dis. 2006;3(4):A126. [PMC free article] [PubMed] [Google Scholar]
- 28.Schleifer R, Csete J. Deadly delay: South Africa's efforts to prevent HIV in survivors of sexual violence. Human Rights Watch. 2004;16(3A):1–75. [Google Scholar]
- 29.Hollingshead AB. Four Factor Index of social status. New Haven, CT: Yale University, Department of Sociology; 1975. [Google Scholar]
- 30.Barbarin OA, Khomo N. Indicators of Economic Status and Social Capital in South African Townships: What Do They Reveal About the Material and Social Conditions in Families of Poor Children? Childhood. 1997;4(2):193–222. [Google Scholar]
- 31.Lyons AC, Spicer J. A new measure of conversational experience: the Speaking Extent and Comfort Scale (SPEACS) Assessment. 1999;6:189–202. doi: 10.1177/107319119900600206. [DOI] [PubMed] [Google Scholar]
- 32.Cecil H, Pinkerton SD. Reliability and validity of a self-efficacy instrument for protective sexual behaviors. J Am Coll Health. 1998;47(3):113–121. doi: 10.1080/07448489809595631. [DOI] [PubMed] [Google Scholar]
- 33.Weinhardt LS, Skinner DH, Glasman L, et al. Baseline behavior interviews impact observed outcomes of a HIV risk reduction intervention: Experimental analysis of assessment reactivity. AIDS Behav. Under revision. [Google Scholar]
- 34.Hendriksen ES, Pettifor A, Lee SJ, et al. Predictors of condom use among young adults in South Africa: the Reproductive Health and HIV Research Unit National Youth Survey. Am J Public Health. 2007;97(7):1241–1248. doi: 10.2105/AJPH.2006.086009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bogart LM, Delahanty DL. Psychosocial models. In: Frank RG, Baum A, Wallander JL, editors. Handbook of Clinical Health Psychology, Vol 3: Models and Perspectives in Health Psychology. Washington, DC: American Psychological Association; 2004. pp. 201–248. [Google Scholar]
- 36.Young SD, Hlavka Z, Modiba P, et al. HIV-related stigma, social norms, and HIV testing in Soweto and Vulindlela, South Africa: National Institutes of Mental Health Project Accept (HPTN 043) J Acquir Immune Defic Syndr. 2010;55(5):620–624. doi: 10.1097/QAI.0b013e3181fc6429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Heunis JC, Wouters E, Norton WE, et al. Patient- and delivery-level factors related to acceptance of HIV counseling and testing services among tuberculosis patients in South Africa: a qualitative study with community health workers and program managers. Implement Sci. 2011;6:27. doi: 10.1186/1748-5908-6-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Cowan F, Pettifor A. HIV in adolescents in sub-Saharan Africa. Curr Opin HIV AIDS. 2009;4(4):288–293. doi: 10.1097/COH.0b013e32832c7d10. [DOI] [PubMed] [Google Scholar]
- 39.Bhana A, McKay MM, Mellins C, et al. Family-based HIV prevention and intervention services for youth living in poverty-affected contexts: the CHAMP model of collaborative, evidence-informed programme development. J Int AIDS Soc. 2010;13(suppl 2):S8. doi: 10.1186/1758-2652-13-S2-S8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mash R, Mash RJ. A quasi-experimental evaluation of an HIV prevention programme by peer education in the Anglican Church of the Western Cape, South Africa. BMJ Open. 2012;2(2):e000638. doi: 10.1136/bmjopen-2011-000638. [DOI] [PMC free article] [PubMed] [Google Scholar]