Abstract
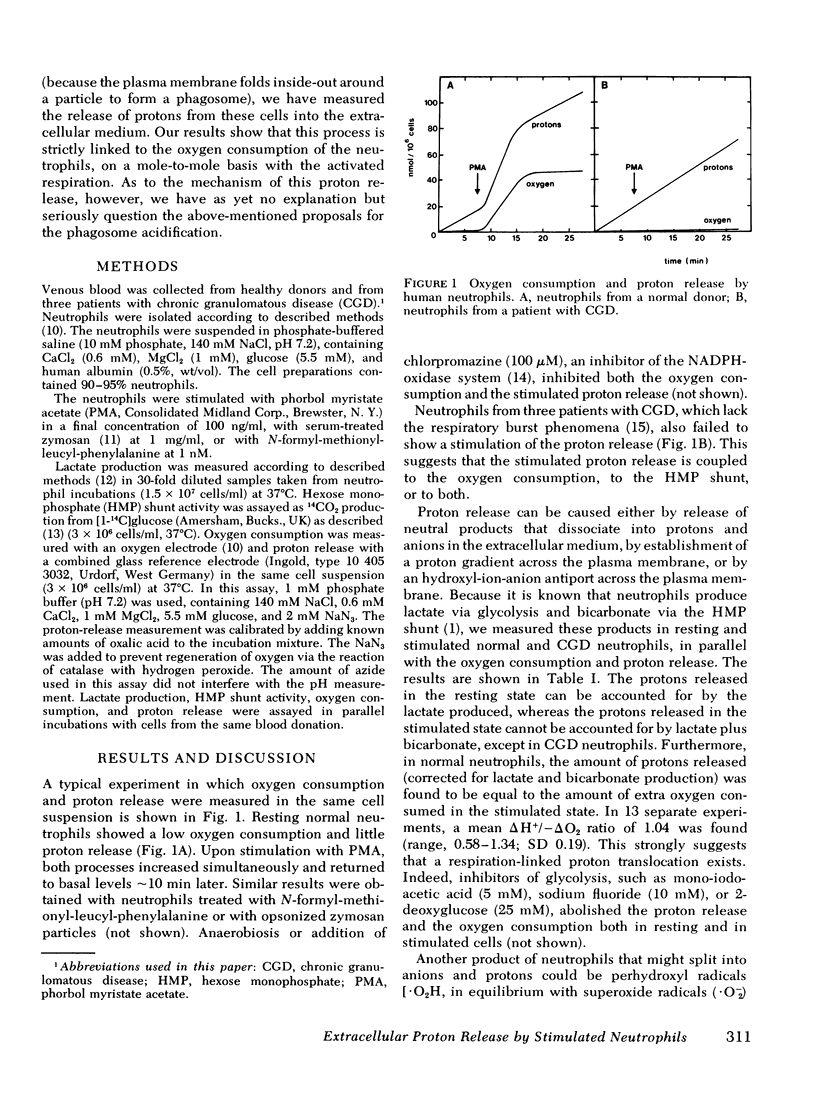
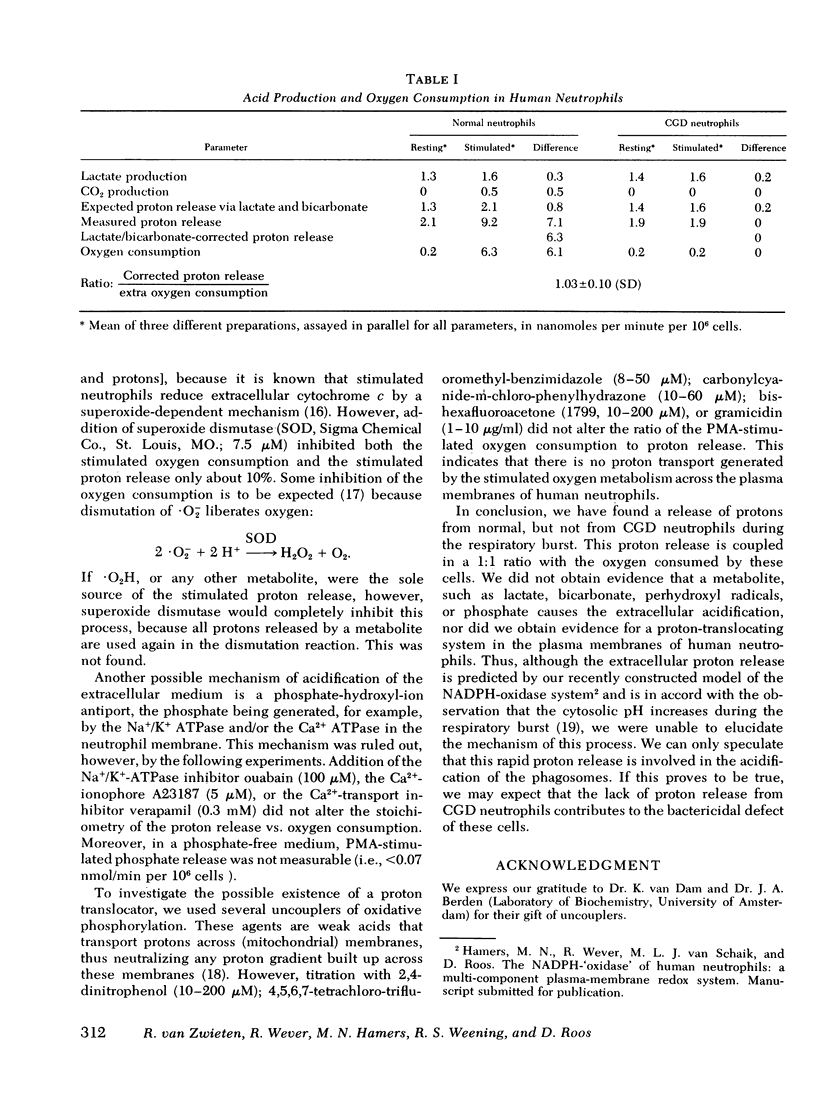
We have tried to elucidate the mechanism of phagosome acidification in human neutrophils. Assuming that phenomena occurring at the plasma membrane reflect reactions in the phagocytic vacuoles, we have stimulated human neutrophils with agents that induce a "respiratory burst," and we have measured the release of protons into the extracellular medium. Phorbol myristate acetate, N-formyl-methionyl-leucyl-phenylalanine and serum-opsonized zymosan particles each caused a rapid release of protons, concomitant with the increase in oxygen consumption. The stimulated release of protons was strictly coupled to the increase respiration of the cells, because inhibition of the respiration of either anaerobiosis, chlorpromazine, or glycolytic inhibitors also inhibited the release of protons. Also, in the presence of the above-mentioned stimulating agents, neutrophils from three patients with chronic granulomatous disease enhanced neither respiration not proton release. In normal cells, the ratio of deltaH+/-deltaO2 was 1.04 +/- 0.19 (mean +/ SD, n = 13). The mechanism of this proton release is not clear. The amount of lactic and carbonic acid produced by stimulated neutrophils was inadequate to explain the amount of protons released. Perhydroxyl radicals were also ruled out as the source of the protons. Because the cells did not release measurable amounts of phosphate ions, a phosphate-hydroxyl-ion antiport was also excluded. Finally, the lack of any effect of uncouplers renders it unlikely that a respiration-driven proton gradient is built up across the plasma membrane.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Babior B. M., Kipnes R. S., Curnutte J. T. Biological defense mechanisms. The production by leukocytes of superoxide, a potential bactericidal agent. J Clin Invest. 1973 Mar;52(3):741–744. doi: 10.1172/JCI107236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Babior B. M. Superoxide production by phagocytes. Another look at the effect of cytochrome c on oxygen uptake by stimulated neutrophils. Biochem Biophys Res Commun. 1979 Nov 14;91(1):222–226. doi: 10.1016/0006-291x(79)90606-5. [DOI] [PubMed] [Google Scholar]
- Cohen H. J., Chovaniec M. E., Ellis S. E. Chlorpromazine inhibition of granulocyte superoxide production. Blood. 1980 Jul;56(1):23–29. [PubMed] [Google Scholar]
- Dewald B., Baggiolini M., Curnutte J. T., Babior B. M. Subcellular localization of the superoxide-forming enzyme in human neutrophils. J Clin Invest. 1979 Jan;63(1):21–29. doi: 10.1172/JCI109273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldstein I. M., Roos D., Kaplan H. B., Weissmann G. Complement and immunoglobulins stimulate superoxide production by human leukocytes independently of phagocytosis. J Clin Invest. 1975 Nov;56(5):1155–1163. doi: 10.1172/JCI108191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmes B., Page A. R., Good R. A. Studies of the metabolic activity of leukocytes from patients with a genetic abnormality of phagocytic function. J Clin Invest. 1967 Sep;46(9):1422–1432. doi: 10.1172/JCI105634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacques Y. V., Bainton D. F. Changes in pH within the phagocytic vacuoles of human neutrophils and monocytes. Lab Invest. 1978 Sep;39(3):179–185. [PubMed] [Google Scholar]
- Jensen M. S., Bainton D. F. Temporal changes in pH within the phagocytic vacuole of the polymorphonuclear neutrophilic leukocyte. J Cell Biol. 1973 Feb;56(2):379–388. doi: 10.1083/jcb.56.2.379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klebanoff S. J. Myeloperoxidase-halide-hydrogen peroxide antibacterial system. J Bacteriol. 1968 Jun;95(6):2131–2138. doi: 10.1128/jb.95.6.2131-2138.1968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loos J. A., Prins H. K. A mechanized system for the determination of ATP + ADP, 2,3-diphosphoglycerate, glucose 1,6-diphosphate and lactate in small amounts of blood cells. Biochim Biophys Acta. 1970 Feb 24;201(2):185–195. doi: 10.1016/0304-4165(70)90292-8. [DOI] [PubMed] [Google Scholar]
- Mandell G. L. Intraphagosomal pH of human polymorphonuclear neutrophils. Proc Soc Exp Biol Med. 1970 Jun;134(2):447–449. doi: 10.3181/00379727-134-34810. [DOI] [PubMed] [Google Scholar]
- Molski T. F., Naccache P. H., Volpi M., Wolpert L. M., Sha'afi R. I. Specific modulation of the intracellular pH of rabbit neutrophils by chemotactic factors. Biochem Biophys Res Commun. 1980 May 30;94(2):508–514. doi: 10.1016/0006-291x(80)91260-7. [DOI] [PubMed] [Google Scholar]
- Pachman L. M., Jayanetra P., Rothberg R. M. Rheumatoid sera and soluble complexes: nitroblue tetrazolium dye test and hexose monophosphate shunt activation. Pediatrics. 1973 Dec;52(6):823–830. [PubMed] [Google Scholar]
- SBARRA A. J., KARNOVSKY M. L. The biochemical basis of phagocytosis. I. Metabolic changes during the ingestion of particles by polymorphonuclear leukocytes. J Biol Chem. 1959 Jun;234(6):1355–1362. [PubMed] [Google Scholar]
- Weening R. S., Roos D., Loos J. A. Oxygen consumption of phagocytizing cells in human leukocyte and granulocyte preparations: a comparative study. J Lab Clin Med. 1974 Apr;83(4):570–577. [PubMed] [Google Scholar]



