Abstract
This study was conducted to investigate the association between the chronic obstructive pulmonary disease (COPD) assessment test (CAT) and depression in COPD patients. The Korean versions of the CAT and patient health questionnaire-9 (PHQ-9) were used to assess COPD symptoms and depressive disorder, respectively. In total, 803 patients with COPD were enrolled from 32 hospitals and the prevalence of depression was 23.8%. The CAT score correlated well with the PHQ-9 score (r=0.631; P<0.001) and was significantly associated with the presence of depression (β±standard error, 0.452±0.020; P<0.001). There was a tendency toward increasing severity of depression in patients with higher CAT scores. By assessment groups based on the 2011 Global Initiative for Chronic Obstructive Lung Disease guidelines, the prevalence of depression was affected more by current symptoms than by airway limitation. The area under the receiver operating characteristic curve for the CAT was 0.849 for predicting depression, and CAT scores ≥21 had the highest accuracy rate (80.6%). Among the eight CAT items, energy score showed the best correlation and highest power of discrimination. CAT scores are significantly associated with the presence of depression and have good performance for predicting depression in COPD patients.
Keywords: Pulmonary Disease, Chronic Obstructive; COPD Assessment Test; Depression
INTRODUCTION
Depression is a major comorbidity in COPD and is associated with higher rates of acute exacerbation, re-admission, and 30-day mortality (1-4). Clinical depression has a reported prevalence of 10% to 42% in COPD patients (4-6) and can be a high economic burden to society (1, 2). Therefore, early detection of depression and appropriate intervention are important (3, 7).
In previous studies, severe dyspnea, low body mass index, female gender, low lung function, poor performance status, and current smoking were identified as risk factors for depression in COPD patients (5, 6, 8). Additionally, several well-known parameters, including an index reflecting the body mass index, airflow obstruction, dyspnea, and exercise capacity (BODE index), the short-form 36 health survey, and the St. George's Respiratory Questionnaire, have been shown to be associated with depression (3, 6, 9-11). Although these composite markers can be used to screen COPD patients for depression, they are not convenient in out-patient settings because of their complexity and time requirements.
Recently, the COPD assessment test (CAT) was developed and shown to be useful for assessing the impact of COPD on patients' quality of life (12). It is a fairly simple and quick questionnaire to use in an out-patient setting (13, 14). To date, limited data exist regarding the association between CAT scores and depression. Therefore, through a multi-center study, we investigated the predictive role of CAT scores for the presence of depression in COPD patients and determined which items of the CAT are the strongest indicators of depression.
MATERIALS AND METHODS
Study design
The present study was performed between August and September 2010; and the data are part of ongoing prospective observational cohort study of COPD patients by the Korean COPD Study Group. Thirty-two hospitals (22 tertiary referral hospitals and 10 secondary referral hospitals) participated in the current survey. Patients with a current diagnosis of COPD and a post-bronchodilator forced expiratory volume in 1 second (FEV1)/forced vital capacity (FVC) ratio of less than 70% of the predicted value at their hospital visit were eligible. All enrolled patients completed both the Patient Health Questionnaire-9 (PHQ-9) and the CAT. Exclusion criteria were as follows: 1) acute exacerbation within the previous 6 months, 2) bronchial asthma or an increase in FEV1 of more than 12% of the predicted value with the use of 400 µg of albuterol, 3) other lung diseases such as bronchiectasis, interstitial lung disease, and tuberculosis-destroyed lungs, and 4) patients who refused consent. Some parts of the results of the present study were previously reported as an abstract form (15).
Depression
To assess the presence of depression in COPD patients, the PHQ-9 was used. It is a validated screening questionnaire for depression, and the Korean version was recently validated (16-19). The PHQ-9 is a self-administered questionnaire composed of nine questions that are based on the Diagnostic and Statistical Manual of Mental Disorders, 4th edition (DSM-IV) criteria for a major depressive episode (17). Each question asks patients about the occurrence of symptoms of depression over the previous 2 weeks, and scores for each item range from 0 (not at all) to 3 (nearly every day). As in the study by Kroenke et al. (18), a total score ≥10 indicated the presence of depression in the present study; total scores of 0-4, 5-9, 10-14, 15-19, and ≥20 represented minimal, mild, moderate, moderate-to-severe, and severe depression, respectively.
COPD assessment test
The CAT is a validated and patient-completed questionnaire comprising eight items: cough, phlegm, chest tightness, breathlessness going up hills/stairs, activity limitation at home, confidence leaving home, sleep, and energy. The score for each CAT item ranges from 0 to 5. The CAT score is known to be well correlated with the St. George's Respiratory Questionnaire score (12, 13, 20). The 2011 Global Initiative for Chronic Obstructive Lung Disease (GOLD) recommends that clinicians use the CAT to assess current symptoms and assign patients to treatment groups based on a CAT scores <10 vs ≥10. The Korean version of the CAT has recently been validated (21).
Data analysis
To evaluate the predictive usefulness of the CAT for depression in COPD patients, correlation analysis, multiple linear regression analysis, and receiver operating characteristics (ROC) curve analysis were performed. The sensitivity, specificity, positive predictive value (PV), and negative PV of CAT scores for predicting depression were calculated. The frequency of depression was determined according to age; the GOLD classification of airway limitation based on FEV1 as a percentage of the predicted value (FEV1% ≥80% vs 50% to <80% vs 30% to <50% vs <30%); and the CAT score groups (≤9 vs 10-20 vs 21-30 vs ≥31). Depression severity was compared using multi-nominal logistic regression analysis. We also compared the frequency of depression among the assessment groups (Groups A, B, C, and D) based on the 2011 GOLD guidelines (i.e., CAT scores [<10 vs ≥10] for symptoms and FEV1% [≥50% vs <50%] for future risk) (14).
Correlation analysis, ROC curve analysis, and logistic regression analysis were performed to determine which items of the CAT are the best predictors of depression in COPD patients. Continuous data are expressed as means±standard deviation, and categorical data are expressed as the number (percentage). Chi-square test was used for the comparison of categorical data. P values<0.05 indicated statistical significance. All statistical analyses were performed using SAS statistical software, EG version (SAS Institute, Inc., Cary, NC, USA).
Ethics statement
The study protocol was approved by the institutional review board at each participating hospital (Hallym University Sacred Heart Hospital, IRB No. 2010-I061). Written informed consent was obtained from each patient.
RESULTS
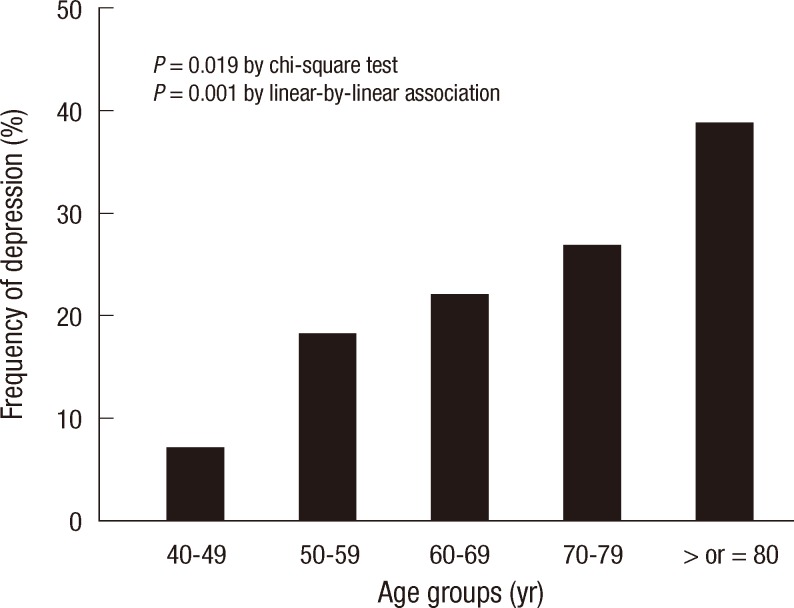
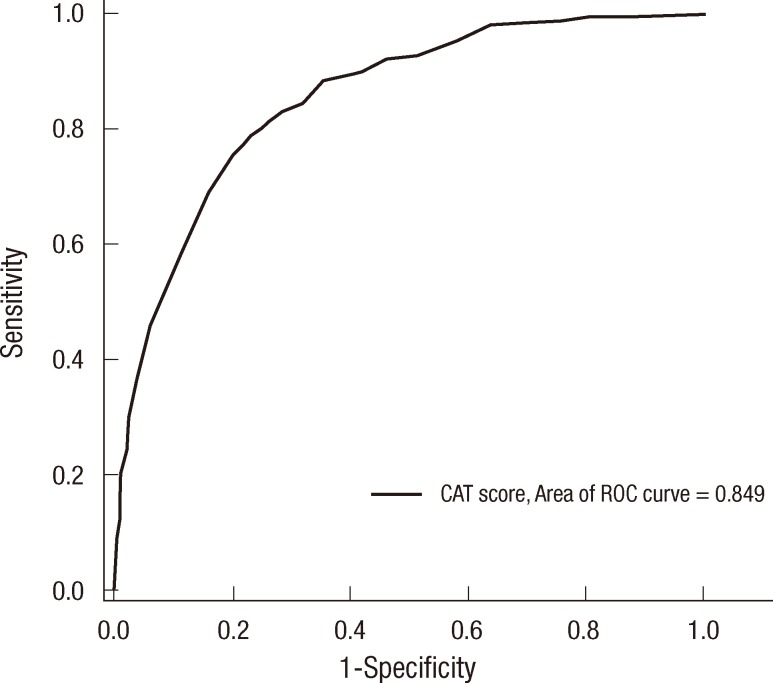
A total of 803 patients were enrolled during the study period, and 91.4% were male. The mean age was 68.2±8.2 yr, and the mean FEV1% was 52.0±19.4% (Table 1). The prevalence of depression, defined as a PHQ-9 score ≥10, was 23.8%. The mean CAT score was 16.2±8.4. Female patients experienced depression more often than male patients, but the difference was not statistically significant. The prevalence of depression was significantly higher in elderly patients than in young patients (P=0.019; Fig. 1).
Table 1.
Patient demographics and clinical characteristics
Data is presented as mean±standard deviation or number (percentage). CAT, COPD assessment test; FEV1, forced expiratory volume in 1 second; GOLD, global initiative for chronic obstructive lung disease; PHQ-9, Patient Health Questionnaire-9.
Fig. 1.
Frequency of depression by age group.
Prevalence of depression according to treatment groups by the 2011 GOLD guidelines
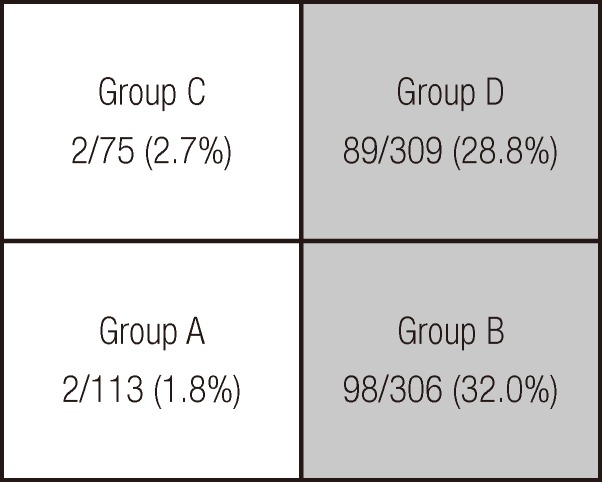
For the assessment and treatment of COPD patients, the 2011 GOLD recommends that patients should be divided into four groups: Group A (low risk and less symptoms), Group B (low risk and more symptoms), Group C (high risk and less symptoms), and Group D (high risk and more symptoms). In the present study, the prevalence rates of depression were 1.8%, 32.0%, 2.7%, and 28.8% in Groups A, B, C, and D, respectively (Fig. 2). The prevalence differed according to current symptoms (Groups A and C vs Groups B and D; P<0.001), but not future risk (Groups A and B vs Groups C and D; P=0.955).
Fig. 2.
Frequency of depression among the four assessment groups recommended by the 2011 GOLD guidelines. The frequency of depression did not differ significantly (P = 0.955) between high-risk patients (Groups C and D; FEV1 < 50% of predicted) and low-risk patients (Groups A and B; FEV1 ≥ 50% of predicted). Frequency of depression was significantly different (P < 0.001) between patients with more symptoms (Groups B and D; CAT score ≥10) and those with less symptoms (Groups A and C; CAT score < 10). CAT, COPD assessment test; FEV1, forced expiratory volume in 1 second.
Associations of CAT score and GOLD classification of airway limitation with depression
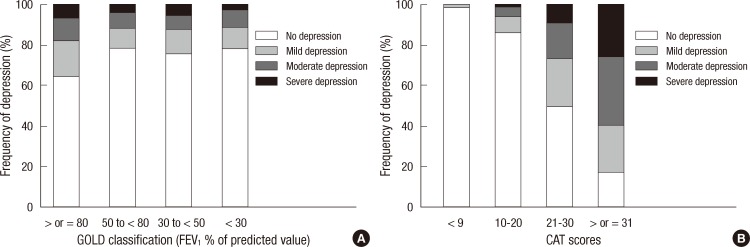
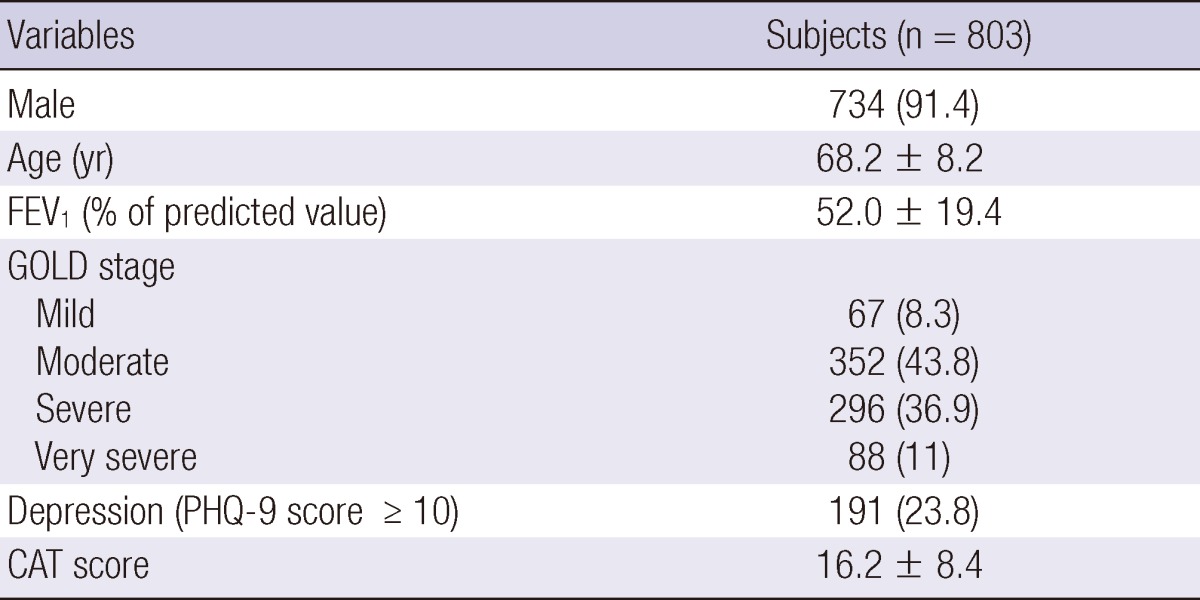
As shown in Fig. 3, the prevalence of depression did not differ among the four groups based on the GOLD classification of airway limitation. Among groups stratified by CAT score (≤9 vs 10-20 vs 21-30 vs ≥31), the frequency of depression was significantly higher in the group with higher CAT scores (P<0.001 and P<0.001 by chi-square test and linear-by-linear association, respectively), and patients with higher CAT scores tended to have more severe depression (Table 2).
Fig. 3.
Frequency and severity of depression according to the GOLD classification of airway limitation (A) and the COPD assessment test (CAT) groups (B). Depression frequency did not differ significantly by airway limitation (A; P = 0.087 and P = 0.283 by chi-square test and linear-by-linear association, respectively). Depression frequency was significantly different between CAT groups (B; P < 0.001 and P < 0.001 by chi-square test and linear-by-linear association). FEV1, forced expiratory volume in 1 second.
Table 2.
Odds ratio of GOLD classification and CAT groups for each severity of depression
*Depression is defined as a PHQ-9 score of ≥10 in the present study; †By multi-nominal logistic regression analyses; ‡Goodness-of-fit test: Chi-square=2.913 and P=0.820. CAT, COPD assessment test; CI, confidence interval; GOLD, global initiative for chronic obstructive lung disease; OR, odds ratio; PHQ-9, Patient Health Questionnaire-9.
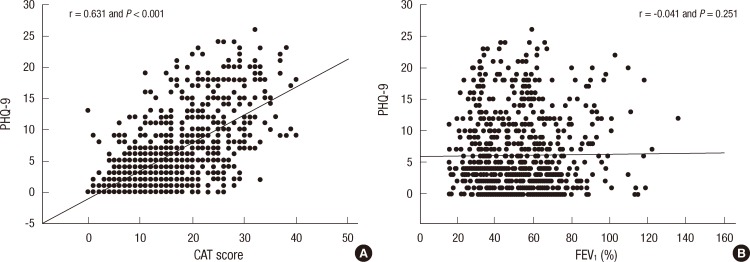
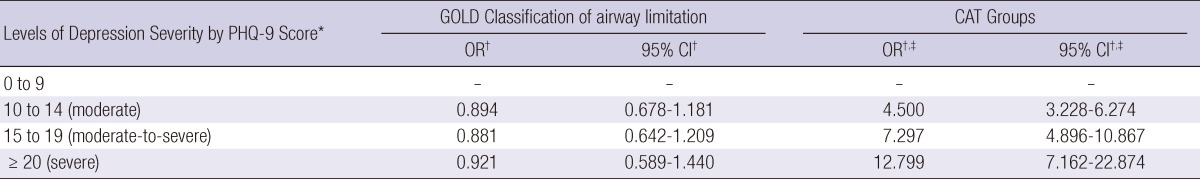
In the correlation analysis, a significant correlation was found between the PHQ-9 and CAT scores (r=0. 631 and P<0.001), but not between the PHQ-9 and GOLD classification of airway limitation (Fig. 4). In the multiple linear regression analysis with age, gender, FEV1, and CAT score as covariates, the CAT score had a significant association with the depression score (β±standard error, 0.452±0.020; P<0.001; Table 3).
Fig. 4.
Scatter diagrams showing the correlations between two parameters. (A) Correlation between Patient Health Questionnaire-9 (PHQ-9) and COPD assessment test (CAT). (B) Correlation between PHQ-9 and forced expiratory volume in 1 second (FEV1).
Table 3.
Multiple linear regression analysis of the association between CAT score and depression
CAT, COPD assessment test; FEV1, forced expiratory volume in 1 second; SE, standard error.
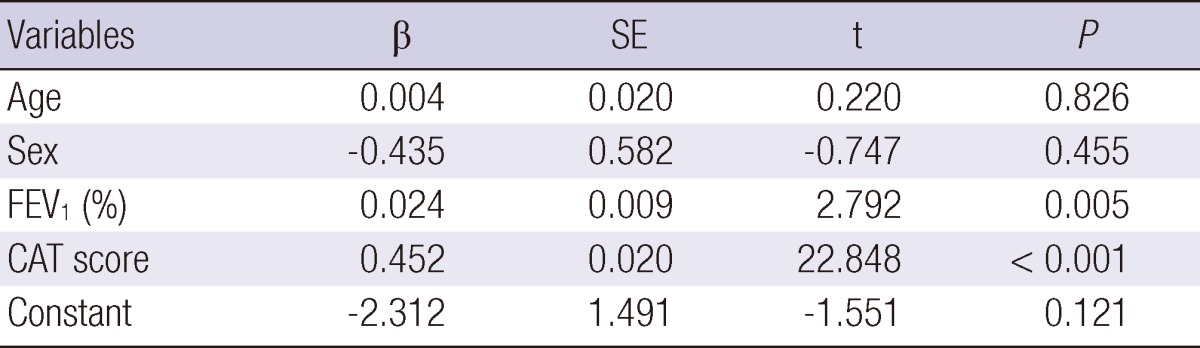
Ability of the sum of CAT scores to predict depression
The ability of the CAT scores to predict the presence of depression was investigated using ROC curve analysis (Fig. 5). The AUC for the CAT score was 0.849 (95% confidence interval, 0.819 to 0.880), and the optimal cutoff value was ≥19.0. The sensitivity, specificity, (+) PV, (-) PV, and accuracy are shown in Table 4. The sensitivity and specificity of the optimal cutoff value (≥19) were 78.0 and 77.5, respectively, but the accuracy was highest (80.6%) for a CAT score ≥21.
Fig. 5.
Receiver operating characteristic (ROC) curve for the COPD assessment test (CAT) score for predicting depression (the Patient Health Questionnaire-9 score ≥ 10). The area under the curve (AUC) was 0.849 (95% confidence interval, 0.819 to 0.880; P < 0.001).
Table 4.
Sensitivity and specificity of CAT score for predicting depression in COPD patients
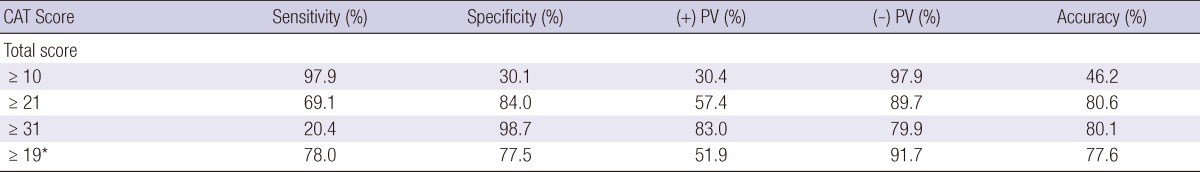
*Optimal cutoff value by the receiver operating characteristic (ROC) curve. CAT, COPD assessment test; COPD, chronic obstructive pulmonary disease; PV, predictive value.
Association of CAT items with depression
The correlation coefficients, AUC values, and odds ratios (ORs) of each CAT item for the presence of depression (PHQ-9) are shown in Table 5. Among the eight CAT items, chest tightness, activity limitation at home, confidence leaving home, sleep, and energy scores showed fair correlations (0.4≤r<0.6) and discrimination power (0.7≤AUC<0.8). Among these five items, the energy score had the best correlation and the highest AUC value, which was comparable to that of the total CAT score. In particular, the OR of the energy score for the presence of depression was significantly higher than those of the other seven CAT items.
Table 5.
Correlation analysis and AUC values between CAT and PHQ-9 scores
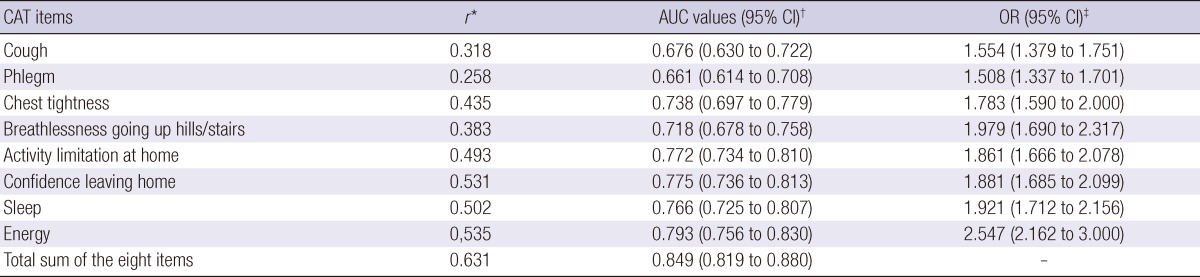
*Correlation coefficients by Pearson's correlation analysis; †Area under the receiver operating characteristic (ROC) curves for the presence of depression (PHQ-9 score of ≥10); ‡Odds ratios for the presence of depression (PHQ-9 score of ≥10). AUC, area under the curve; CAT, COPD assessment test; CI, confidence interval; OR, odds ratio; PHQ-9, Patient Health Questionnaire-9.
DISCUSSION
The present study had several important findings. First, the CAT score was significantly associated with depression, with good predictive usefulness for the presence of depression in COPD patients. Second, compared with the GOLD classification of airway limitation, the CAT score was better correlated with the depression score, and depression severity was higher in patients with higher CAT scores. Among the assessment groups based on the 2011 GOLD guidelines, the frequency of depression differed by current symptoms, but not by the severity of the airway limitation. Finally, among the eight items of the CAT, the energy score showed the best correlation with the presence of depression and had the highest discrimination power.
Depression has been extensively studied and is known to have a negative impact on COPD outcomes (4, 9, 10). However, depression often goes undiagnosed, and its exact prevalence and mechanisms in COPD are unclear. In previous studies, several composite markers have been evaluated. However, these markers are too complex for routine use in outpatient settings. In 2011, the GOLD recommended the use of the CAT for assessment of COPD patients (13, 14). It is a valid tool and simple to use. Therefore, in the present study, we investigated usefulness of the CAT for prediction of depression in COPD patients in an outpatient setting.
Among the four variables included in the multivariate analysis in our study, the CAT score was significantly associated with presence of depression. ROC curve analysis indicated good performance of the CAT score for predicting depression. The 2011 GOLD guidelines recommend a CAT score of ≥10.0 for assigning COPD patients to a treatment group (14). However, in the present study, the (+) PV of CAT scores ≥10.0 for presence of depression was only 30.4%. At an optimal cutoff value of ≥19.0, sensitivity and specificity were 78.0 and 77.5, respectively, and accuracy rate was the highest (80.6%) using a cutoff value of ≥21.0. Therefore, based on our results, a higher CAT score, possibly ≥21.0, would be more useful for depression screening in COPD patients. In addition, we also investigated association between individual items of the CAT and depression. Chest tightness, activity limitation at home, confidence leaving home, sleep, and energy scores were correlated with depression. Among these, energy score showed the highest correlation and good discrimination power. Thus, rather than traditional COPD symptoms (i.e., cough and phlegm), these five CAT items, especially energy, may be better indicators of depression in COPD patients.
The prevalence of depression in our study population was 23.8%, and depression was more common in elderly patients than in young patients. There was no difference in prevalence between genders or between severities of airway limitation. In contrast, the ECLIPSE study reported that depression was significantly associated with young age and female gender, and severe airway limitation (6). This discrepancy between the ECLIPSE study and ours may be attributable to several differences between the study populations, including differences in gender, age, and disease severity distributions, or may be a consequence of the different tools used for assessment and analysis (5). In the present study, depression was observed at all grades of GOLD classification of airway limitation. Several previous studies have also demonstrated depression even in mild-grade COPD, and we emphasized the need for early screening to reduce the risk for acute exacerbation (22-24). However, in our study, the presence of depression was dependent on current symptoms, and not on lung function. Additionally, we also demonstrated the increased severity of depression with higher CAT scores (Fig. 2 and Table 2). Thus, regardless of results of lung function tests, physicians should quickly assess the presence of depression in all COPD patients and particularly in symptomatic patients. Using the CAT, physicians may be able to assess not only patients' current symptoms but also potential depression.
Our study had several limitations. First, we did not investigate other variables such as comorbidities, exacerbation frequency, and smoking status that have associations with depression in COPD patients (5, 6). As a result, we could not include other potential variables in the multivariate model. Second, among several depression scales, the PHQ-9 was used in the present study. Although the reliability and validity of the PHQ-9 have not been extensively studied in COPD, it is the most commonly used scale in primary care. Finally, the CAT has items which are originally associated with depression, such as energy and sleep. Therefore, the superiority of the CAT over the GOLD classification in the present study may be attributable to the structure itself of the questionnaire. Despite these limitations, our nationwide, multi-center study is, to our knowledge, the first demonstration of the usefulness of the CAT for depression screening in COPD patients. According to many experts, a better understanding of the barriers to the diagnosis and treatment of depression in COPD patients will improve outcomes (5, 25). Because of its simplicity and practicality, the CAT may be a useful tool for overcoming some barriers.
In conclusion, the CAT scores are significantly associated with the presence of depression and have good performance for predicting depression in COPD patients. Therefore, the CAT may be a useful tool for depression screening in out-patient settings. Large-scale, multi-center studies are needed to further define the role of the CAT for depression screening in COPD patients.
ACKNOWLEDGMENTS
The copyright of Korean version of CAT belongs to the GlaxoSmithKline (GSK) and the authors were allowed to use CAT for this study.
We would like to thank people below for their help: Kyung Ho Kang, Department of Internal Medicine, Korea University College of Medicine, Seoul; Sang Hak Lee, Department of Internal Medicine, The Catholic University of Korea, College of Medicine, Seoul; Seong Yong Lim, Department of Internal Medicine, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Seoul; Kwang Ha Yoo, Department of Internal Medicine, Konkuk University Hospital, Seoul; In-Won Park, Department of Internal Medicine Chung-Ang University College of Medicine, Seoul; Myung Jae Park, Department of Internal Medicine, Kyung Hee University Hospital, Seoul; Jin Hwa Lee, Division of Pulmonary and Critical Care Medicine, Ewha Womans University School of Medicine, Seoul; Ji-Hyun Lee, Department of Internal Medicine, Pochon CHA University, Seongnam; Hye Sook Choi, Dongguk University Colleage of Medicine, Gyeongju Hospital, Gyeongju; Jin Woo Kim, Department of Internal Medicine, The Catholic University of Korea, College of Medicine, Uijeongbu; Jong Pil Jeong and Youngchun Ko, Department of Internal Medicine Kwangju Christian Hospital, Kwangju; Hye Yoon Park, Department of Internal Medicine, Sungkyunkwan University School of Medicine, Seoul; Hui Jung Kim, Department of Internal Medicine, Wonkwang University Sanbon Hospital, Gunpo; Kye Chul Shin, Department of Internal Medicine, Yonsei University Wonju College of Medicine, Wonju; Myung-Goo Lee, Division of Pulmonary, Allergy and Critical Care Medicine, Department of Internal Medicine, Hallym University Chuncheon Sacred Heart Hospital, Chuncheon; Hun Gyu Hwang, Eun-Jung Jung and Gune-Il Lim, Division of Pulmonology Department of Internal Medicine, Soonchunhyang University Gumi Hospital, Gumi; Jong Deog Lee, Gyeongsang National University, School of Medicine, Jinju; Yong Ho Roh, Seoul Veterans Hospital, Seoul; Yang Deok Lee, Department of Internal Medicine, Eulji University School of Medicine, Daejeon; Hyoung-Kyu Yoon, Department of Internal Medicine, The Catholic University of Korea, Seoul; Ju-Ock Kim and Jeong Eun Lee, Pulmonology section, Department of Internal Medicine, Chungnam National University Hospital, Daejeon; Ho Kee Yum, Department of Internal Medicine, Inje University Seoul Paik Hospital, Inje University College of Medicine, Seoul; Kang Hyeon Choi, Department of Internal Medicine, Chungbuk National University Hospital, Cheongju; and Se Kyu Kim, Department of Internal Medicine, Yonsei University College of Medicine, Seoul, Korea.
Footnotes
This study was supported by a grant of the Korean Healthcare Technology R&D Project, Ministry for Health and Welfare, Republic of Korea (A102065).
The authors have no conflicts of interest to disclose.
References
- 1.Abrams TE, Vaughan-Sarrazin M, Van der Weg MW. Acute exacerbations of chronic obstructive pulmonary disease and the effect of existing psychiatric comorbidity on subsequent mortality. Psychosomatics. 2011;52:441–449. doi: 10.1016/j.psym.2011.03.005. [DOI] [PubMed] [Google Scholar]
- 2.Dalal AA, Shah M, Lunacsek O, Hanania NA. Clinical and economic burden of depression/anxiety in chronic obstructive pulmonary disease patients within a managed care population. COPD. 2011;8:293–299. doi: 10.3109/15412555.2011.586659. [DOI] [PubMed] [Google Scholar]
- 3.Jennings JH, Digiovine B, Obeid D, Frank C. The association between depressive symptoms and acute exacerbations of COPD. Lung. 2009;187:128–135. doi: 10.1007/s00408-009-9135-9. [DOI] [PubMed] [Google Scholar]
- 4.Ng TP, Niti M, Tan WC, Cao Z, Ong KC, Eng P. Depressive symptoms and chronic obstructive pulmonary disease: effect on mortality, hospital read-mission, symptom burden, functional status, and quality of life. Arch Intern Med. 2007;167:60–67. doi: 10.1001/archinte.167.1.60. [DOI] [PubMed] [Google Scholar]
- 5.Maurer J, Rebbapragada V, Borson S, Goldstein R, Kunik ME, Yohannes AM, Hanania NA ACCP Workshop Panel on Anxiety and Depression in COPD. Anxiety and depression in COPD: current understanding, unanswered questions, and research needs. Chest. 2008;134:43S–56S. doi: 10.1378/chest.08-0342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hanania NA, Müllerova H, Locantore NW, Vestbo J, Watkins ML, Wouters EF, Rennard SI, Sharafkhaneh A Evaluation of COPD Longitudinally to Identify Predictive Surrogate Endpoints (ECLIPSE) Study Investigators. Determinants of depression in the ECLIPSE chronic obstructive pulmonary disease cohort. Am J Respir Crit Care Med. 2011;183:604–611. doi: 10.1164/rccm.201003-0472OC. [DOI] [PubMed] [Google Scholar]
- 7.Von Leupoldt A, Taube K, Lehmann K, Fritzsche A, Magnussen H. The impact of anxiety and depression on outcomes of pulmonary rehabilitation in patients with COPD. Chest. 2011;140:730–736. doi: 10.1378/chest.10-2917. [DOI] [PubMed] [Google Scholar]
- 8.Al-shair K, Dockry R, Mallia-Milanes B, Kolsum U, Singh D, Vestbo J. Depression and its relationship with poor exercise capacity, BODE index and muscle wasting in COPD. Respir Med. 2009;103:1572–1579. doi: 10.1016/j.rmed.2008.11.021. [DOI] [PubMed] [Google Scholar]
- 9.Balcells E, Gea J, Ferrer J, Serra I, Orozco-Levi M, de Batlle J, Rodriguez E, Benet M, Donaire-González D, Antó JM, et al. Factors affecting the relationship between psychological status and quality of life in COPD patients. Health Qual Life Outcomes. 2010;8:108. doi: 10.1186/1477-7525-8-108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ito K, Kawayama T, Shoji Y, Fukushima N, Matsunaga K, Edakuni N, Uchimura N, Hoshino T. Depression, but not sleep disorder, is an independent factor affecting exacerbations and hospitalization in patients with chronic obstructive pulmonary disease. Respirology. 2012;17:940–949. doi: 10.1111/j.1440-1843.2012.02190.x. [DOI] [PubMed] [Google Scholar]
- 11.Kil SY, Oh WO, Koo BJ, Suk MH. Relationship between depression and health-related quality of life in older Korean patients with chronic obstructive pulmonary disease. J Clin Nurs. 2010;19:1307–1314. doi: 10.1111/j.1365-2702.2009.03053.x. [DOI] [PubMed] [Google Scholar]
- 12.Jones PW, Harding G, Berry P, Wiklund I, Chen WH, Kline Leidy N. Development and first validation of the COPD Assessment Test. Eur Respir J. 2009;34:648–654. doi: 10.1183/09031936.00102509. [DOI] [PubMed] [Google Scholar]
- 13.COPD Assessment Test. [accessed on 1 January 2011]. Available at http://www.catestonline.org.
- 14.Vestbo J, Hurd SS, Agustí AG, Jones PW, Vogelmeier C, Anzueto A, Barnes PJ, Fabbri LM, Martinez FJ, Nishimura M, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med. 2013;187:347–365. doi: 10.1164/rccm.201204-0596PP. [DOI] [PubMed] [Google Scholar]
- 15.Hwang YI, Lee YS, Oh YM, Lee SD, Park SW, Kim YS, In KH, Jung BH, Lee KH, Ra SW, et al. Prevalence of depression and its influence on health-related quality of life in COPD patients. Chest. 2011;140:542A. [Google Scholar]
- 16.Han C, Jo SA, Kwak JH, Pae CU, Steffens D, Jo I, Park MH. Validation of the Patient Health Questionnaire-9 Korean version in the elderly population: the Ansan Geriatric Study. Compr Psychiatry. 2008;49:218–223. doi: 10.1016/j.comppsych.2007.08.006. [DOI] [PubMed] [Google Scholar]
- 17.Huang FY, Chung H, Kroenke K, Delucchi KL, Spitzer RL. Using the Patient Health Questionnaire-9 to measure depression among racially and ethnically diverse primary care patients. J Gen Intern Med. 2006;21:547–552. doi: 10.1111/j.1525-1497.2006.00409.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lamers F, Jonkers CC, Bosma H, Penninx BW, Knottnerus JA, van Eijk JT. Summed score of the Patient Health Questionnaire-9 was a reliable and valid method for depression screening in chronically ill elderly patients. J Clin Epidemiol. 2008;61:679–687. doi: 10.1016/j.jclinepi.2007.07.018. [DOI] [PubMed] [Google Scholar]
- 20.Ringbaek T, Martinez G, Lange P. A comparison of the assessment of quality of life with CAT, CCQ, and SGRQ in COPD patients participating in pulmonary rehabilitation. COPD. 2012;9:12–15. doi: 10.3109/15412555.2011.630248. [DOI] [PubMed] [Google Scholar]
- 21.Lee S, Lee JS, Song JW, Choi CM, Shim TS, Kim TB, Cho YS, Moon HB, Lee SD, Oh YM. Validation of the Korean version of chronic obstructive pulmonary disease assessment test (CAT) and dyspnea-12 questionnaire. Tuberc Respir Dis. 2010;69:171–176. [Google Scholar]
- 22.Chavannes NH, Huibers MJ, Schermer TR, Hendriks A, van Weel C, Wouters EF, van Schayck CP. Associations of depressive symptoms with gender, body mass index and dyspnea in primary care COPD patients. Fam Pract. 2005;22:604–607. doi: 10.1093/fampra/cmi056. [DOI] [PubMed] [Google Scholar]
- 23.De S. Prevalence of depression in stable chronic obstructive pulmonary disease. Indian J Chest Dis Allied Sci. 2011;53:35–39. [PubMed] [Google Scholar]
- 24.Di Marco F, Verga M, Reggente M, Maria Casanova F, Santus P, Blasi F, Allegra L, Centanni S. Anxiety and depression in COPD patients: the roles of gender and disease severity. Respir Med. 2006;100:1767–1774. doi: 10.1016/j.rmed.2006.01.026. [DOI] [PubMed] [Google Scholar]
- 25.Pincus HA, Hough L, Houtsinger JK, Rollman BL, Frank RG. Emerging models of depression care: multi-level ('6 P') strategies. Int J Methods Psychiatr Res. 2003;12:54–63. doi: 10.1002/mpr.142. [DOI] [PMC free article] [PubMed] [Google Scholar]