Abstract
The neural response to unpredictable auditory events is suggested to depend on frontotemporal interactions. We used magnetoencephalography in patients with behavioral variant frontotemporal dementia to study change detection and to examine the impact of disease on macroscopic network connectivity underlying this core cognitive function. In patients, the amplitudes of auditory cortical responses to predictable standard tones were normal but were reduced for unpredictable deviant tones. Network connectivity, in terms of coherence among frontal, temporal, and parietal sources, was also abnormal in patients. In the beta frequency range, left frontotemporal coherence was reduced. In the gamma frequency range, frontal interhemispheric coherence was reduced whereas parietal interhemispheric coherence was enhanced. These results suggest impaired change detection resulting from dysfunctional frontotemporal interactions. They also provide evidence of a rostrocaudal reorganization of brain networks in disease. The sensitivity of magnetoencephalography to cortical network changes in behavioral variant frontotemporal dementia enriches the understanding of neurocognitive systems as well as showing potential for studies of experimental therapies for neurodegenerative disease.
INTRODUCTION
The behavioral variant of frontotemporal dementia (bvFTD) is characterized by progressive change in personality, empathy, personal conduct, and disinhibition with loss of insight (Rascovsky et al., 2011; Neary et al., 1998). For bvFTD and other major neurodegenerative diseases, a new systems neurobiological model is emerging, which emphasizes the selective vulnerability of brain networks. This network paradigm draws extensively on brain imaging, including regional activation with mental operations (Hughes, Nestor, Hodges, & Rowe, 2011), functional networks (Zhou, Gennatas, Kramer, Miller, & Seeley, 2012; Pievani, de Haan, Wu, Seeley, & Frisoni, 2011), metabolic activity (Kipps, Hodges, Fryer, & Nestor, 2009), and structure (Rohrer, Ridgway, et al., 2010; Whitwell et al., 2009). In addition to explaining clinical phenomena, this systems level analysis may facilitate diagnostic, prognostic, or therapeutic biomarkers for novel treatments (Boxer & Boeve, 2007).
To assess the impact of neurodegenerative disease on pathophysiological and cognitive processes, formal analyses of functional neuronal networks are required (Horwitz & Rowe, 2011; Rowe, 2010). In the context of bvFTD, neuroimaging methods have shown characteristic changes in frontal, limbic, and anterior temporal structures based on PET imaging of metabolic activity (Kipps et al., 2009; Salmon et al., 2006) and structural morphometrics of MRI, including voxel-based morphometry (Gordon et al., 2010; Rohrer, Geser, et al., 2010; Pereira et al., 2009; Whitwell et al., 2009; Williams, Nestor, & Hodges, 2005). The frontal cortex is one of the regions of maximal pathology, hypometabolism, and cortical atrophy in bvFTD (Gordon et al., 2010; Rohrer, Geser, et al., 2010; Kipps et al., 2009; Pereira et al., 2009; Whitwell et al., 2009; Seeley et al., 2008; Williams et al., 2005) particularly arising within superficial layers in frontal cortex (Hampton et al., 2010; Cairns et al., 2007; Mackenzie, 2007). Frontotemporal white matter tracts are also abnormal in bvFTD (Acosta-Cabronero et al., 2011; Whitwell et al., 2010). However, these methods do not directly assess the communication within the relevant functional networks.
A formal connectivity approach can be applied to bvFTD using fMRI, for example, covariance of the spontaneous low-frequency fluctuations in resting state fMRI mirror the neurodegenerative changes in anatomical structure and connectivity (Zhou et al., 2010; Seeley, Crawford, Zhou, Miller, & Greicius, 2009). The utility of electrophysiological and biomagnetic measures in examining abnormal brain connectivity in degenerative disease has also been recognized (cf. Zamrini et al., 2011; Stam, 2010). EEG and magnetoencephalography (MEG) of degenerative disease have shown reorganization of dynamic neural networks (de Haan et al., 2009, 2012; Stam, 2010). In bvFTD, these methods have revealed specific connectivity changes (Zhou et al., 2010) and abnormal network topology (Zhou et al., 2012), with both decreases and increases in connectivity between regions. However, less is known about the impact of bvFTD on networks subserving specific cognitive operations.
The current study aimed to examine the impact of bvFTD on a fundamental cognitive operation: the detection of unpredicted events or change. Such change detection is readily assessed using an auditory MMN paradigm. Classical auditory MMN paradigms typically present a stream of predictable “standard” tones interspersed with “deviant” tones that differ from the standard by one dimension (e.g., by a change in intensity or duration). With EEG or MEG, a characteristic MMN difference in response to the two tone types is seen with a strong early component between 100 and 200 msec from tone onset.
The early MMN component is generated within bilateral auditory temporal and frontal cortices (Rosburg et al., 2005; Doeller et al., 2003; Schall, Johnston, Todd, Ward, & Michie, 2003; Liasis, Towell, Alho, & Boyd, 2001; Näätänen & Alho, 1995; Giard, Perrin, Pernier, & Bouchet, 1990). The temporal cortical MMN is affected by neuropsychiatric syndromes, suggesting a sensitive but nonspecific marker of disease (Näätänen et al., 2011, 2012; Bronnick, Nordby, Larsen, & Aarsland, 2010; Näätänen & Kahkonen, 2009; Thonnessen et al., 2008; Engeland, Mahoney, Mohr, Ilivitsky, & Knott, 2002; Pekkonen, Hirvonen, Jaaskelainen, Kaakkola, & Huttunen, 2001; Pekkonen, 2000). On the basis of the reduction of the MMN following frontal lobe injury (Alain, Woods, & Knight, 1998; Alho, Woods, Algazi, Knight, & Näätänen, 1994), we hypothesized that the integrity of the frontal lobe and frontotemporal connections are necessary for auditory change detection for many types of unpredictable sensory events.
The role of frontotemporal connections in generating an MMN can be assessed by coherence analyses or dynamic causal modeling of electrophysiological data. For example, dynamic causal models have demonstrated acute modulation of bidirectional connections between frontal and temporal cortex, underlying the MMN response to unexpected tones (Garrido et al., 2008). Furthermore, the MMN is associated with changes in local and distributed frontotemporal networks in the alpha and beta bandwidths (Hsiao, Cheng, Liao, & Lin, 2010) and gamma frequency band (Nicol et al., 2012). These methods suggest frequency-specific and hierarchically distributed frontotemporal networks for change detection and the MMN.
The importance of this network connectivity has been attributed to its role in predictive coding (Wacongne, Changeux, & Dehaene, 2012; Wacongne et al., 2011; Garrido, Kilner, Kiebel, & Friston, 2009; Garrido et al., 2008) within a generalized cognitive framework that encompasses sensory repetitions and goal-oriented behaviors (Friston, Daunizeau, Kilner, & Kiebel, 2010; Friston & Dolan, 2010). In these predictive coding schemes, the sources of backward connections are thought to arise in deep cortical layers (Mumford, 1992,) that preferentially express lower frequencies whereas forward connections in superficial cortex may exploit gamma oscillations (Arnal, Wyart, & Giraud, 2011; Buffalo, Fries, Landman, Buschman, & Desimone, 2011; van Aerde et al., 2009; Kiebel, Daunizeau, & Friston, 2008).
Given the frontal and temporal neuropathology in bvFTD, coupled with severe cognitive and behavioral impairments, the auditory MMN is an ideal paradigm to study the functional anatomy and connectivity of frontotemporal networks. We therefore used MEG to measure the MMN in an “optimum” multifeature paradigm, with five types of deviant stimulus (Näätänen, Pakarinen, Rinne, & Takegata, 2004).
We tested two key hypotheses using two models of source analysis: First, we examined the auditory cortical waveforms in response to standard and deviant tones. We predicted that despite normal responses to standard tones, the generation of an MMN would be impaired in patients with bvFTD, with reduced amplitudes to deviant tones despite relative preservation of auditory cortex. Second, we predicted bvFTD to be associated with changes in network connectivity, measured here in terms of frequency-specific coherence among frontal, temporal, and parietal sources. We proposed that changes in coherence due to altered feedback from frontal to temporal sources would be seen particularly in low-frequency alpha and beta bands. We also predicted changes in gamma coherence in bvFTD based on the gamma connectivity associated with MMN (Nicol et al., 2012) and the neuropathological burden in the superficial cortical layers (Hampton et al., 2010; Cairns et al., 2007; Mackenzie, 2007), which support gamma synchrony (Buffalo et al., 2011).
METHODS
Participants and Task
Twelve right-handed patients with progressive bvFTD (clinical diagnostic criteria, including abnormal clinical imaging; Rascovsky et al., 2011; Neary et al., 1998) were recruited from the early dementia clinic at Addenbrooke’s Hospital. Patients with nonprogressive mimics of bvFTD were not included (Kipps, Hodges, & Hornberger, 2010). One patient was excluded for being below the required screening hearing threshold. Patients underwent neuropsychological assessment including the revised Addenbrooke’s cognitive examination (ACE-R; Mioshi, Dawson, Mitchell, Arnold, & Hodges, 2006) and Mini-Mental State Examination (MMSE). Caregivers completed the Cambridge Behavioral Inventory to provide an assessment of the severity of behavioral symptoms (Wedderburn et al., 2008). Seventeen right-handed healthy older adults were recruited from the volunteer panel of the MRC Cognition and Brain Sciences Unit. No volunteers in the control group had a history of significant neurological, rheumatological, or psychiatric illness nor had any cognitive complaints. Patient and control groups did not differ significantly in terms of age or sex (bvFTD: age mean = 60 years, range = 42–68 years, seven men; Control: age mean = 61 years, range = 50–72 years, seven men). The mean duration of diagnosis was 4 years. Patients had moderately severe impairments in global cognitive function and high rates of carer endorsements on the Cambridge Behavioral Inventory: Patient details are summarized in Table 1. The study was approved by the local Research Ethics Committee, and participants gave written informed consent.
Table 1.
Details of bvFTD Patients
|
Age of
Onset |
Year
Diagnosis |
ACE-r
Total |
ACE-r Subscales
|
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Participants | Age | M/F | MMSE | Attention | Memory | Fluency | Language | VSp | CBI | |||
| 1 | 42 | f | 38 | 3 | 20 | 49 | 16 | 6 | 1 | 18 | 8 | 120 |
| 2 | 60 | f | 58 | 2 | 30 | 89 | 18 | 20 | 9 | 26 | 16 | 87 |
| 3 | 62 | f | 58 | 4 | 24 | 70 | 15 | 22 | 2 | 21 | 10 | 59 |
| 4 | 63 | f | 61 | 2 | 26 | 84 | 17 | 24 | 4 | 23 | 16 | 37 |
| 5 | 60 | f | 57 | 3 | 19 | 50 | 13 | 8 | 1 | 18 | 10 | 61 |
| 6 | 65 | m | 62 | 2 | 27 | 71 | 18 | 19 | 6 | 20 | 8 | 65 |
| 7 | 59 | m | 57 | 2 | 26 | 70 | 15 | 18 | 4 | 23 | 10 | 156 |
| 8 | 68 | m | 64 | 4 | 21 | 72 | 14 | 16 | 5 | 23 | 14 | 146 |
| 9 | 51 | m | 42 | 8 | 22 | 76 | 13 | 17 | 4 | 26 | 16 | 212 |
| 10 | 62 | m | 56 | 5 | 14 | 33 | 9 | 0 | 0 | 9 | 15 | 130 |
| 11 | 68 | m | 61 | 7 | 27 | 85 | 17 | 22 | 11 | 22 | 13 | 48 |
| 12 | 63 | m | 58 | 5 | 25 | 84 | 16 | 23 | 6 | 25 | 14 | 95 |
| Mean | 60 | 5f, 7m | 56 | 4 | 23 | 69 | 15 | 16 | 4 | 21 | 13 | 101 |
MMSE = 30-point Mini-Mental State Examination; ACE-r = 100 point Addenbrooke’s cognitive examination revised; VSp = visuospatial subscale; CBI = Cambridge Behavioral Inventory max 324 points.
The multifeature “Optimum-1” paradigm (Näätänen et al., 2004) was used to study the MMN response. The standard tone was a harmonic tone of 75-msec duration, comprising three sinusoidal partials of 500, 1000, and 1500 Hz. The five deviant tones differed from the standard by either frequency band (550, 1100, 1650 Hz), intensity (±6 dB), duration (25 vs. 75 msec), side of sound source (left or right sided rather than bilateral), and a silent gap (silent mid 25 msec). After each standard tone, one of the five deviants was presented in a pseudorandom order, such that in a sequence of 10 tones, each deviant type was presented once but the same deviant type was never immediately repeated. Tones were presented every 500 msec in three blocks of 5 min, with a total of 900 standards and 900 deviants. Tones were presented binaurally via plastic tubes and earpieces at approximately 60 dB above the hearing threshold (hearing thresholds were determined in the MEG, using an adaptive algorithm with pure tones at 1000 Hz).
Data Processing
Continuous MEG data were collected with a 306-channel Vectorview system in a magnetically shielded room (Elekta Neuromag, Helsinki, Finland), including a magnetometer and two orthogonal planar gradiometers at each of 102 positions. Data were down-sampled from 1000 to 333 Hz. Vertical and horizontal eye movements were recorded using paired EOG electrodes. Five head position indicator coils were used to monitor head position. The three-dimensional locations of the head position indicator coils and approximately 80 “head points” across the scalp and three anatomical fiducials (the nasion and left and right pre-auricular points) were recorded using a 3-D digitizer (Fastrak Polhemus, Inc., Colchester, VA). Data were pre-processed using MaxFilter software (Elekta-Neuromag) with movement compensation.
Data were high-pass filtered above 0.1 Hz (butterworth filter 6 dB/oct with no added padding). Artifact detection and eye blink correction used Brain Electrical Source Analysis (BESA Version 5.2, Germany). The artifact rejection threshold was set to 2500 ft for magnetometers and 900 ft for gradiometers. Eye blinks were corrected using BESA’s adaptive artifact correction and modeled in the source analysis with one fixed source. Epochs (−100 to 400 msec after tone onset) were time locked to the tone onset and baseline corrected (−100 to 0 msec). Two source models were used to examine the MMN. The first dipole model was used to explicitly compare between groups, the auditory cortical source waveform of the MMN. The second model examined frontal, temporal, and parietal coherence to specifically test our hypotheses that in patients the frontotemporal and frontal interhemispheric coherence would be affected by disease. Although this method allows us to test specific hypotheses about known regions associated with the oddball paradigm, it restricts analyses to a discrete number of regions (and their interactions). Thus, we do not claim that differences between patients and controls are only within these brain regions.
Data Analysis
Model 1
Data were bandpass-filtered 1–40 Hz, and epochs for the standard tones were averaged and subtracted from the average for each of the five deviant types. Using this model, we also examined the neurophysiological responses of the participants to the standard tones to further clarify that any difference between patients and controls was not due to auditory deficits. The peak latency and amplitude of the M100 (MEG equivalent of the N100, a negatively evoked potential between 80 and 120 msec after tone onset) was estimated in addition to the MMN.
Source analysis of evoked responses was performed for each participant on the MMN difference and to the standard tone using gradiometer data (bandpass-filtered 1–40 Hz). The forward model topography (leadfield) was estimated using a realistic head model in BESA 5.2, coregistered by fiducial and digitized scalp loci. The inverted leadfield matrix was applied to the gradiometer data to estimate two bilateral equivalent current dipoles (regional sources) across an interval of 100–200 msec for the mismatch waveforms (deviant vs. standard) and 50–150 msec for responses to the standard tones. Sources were optimized by varying location and orientation iteratively to minimize residual difference between scalp and model waveforms. Fitting was constrained by symmetry on the two source locations to ensure right and left auditory cortical sources were modeled efficiently, with 1% regularization constant to stabilize source fitting in the presence of noise. An analysis of variance examined potential differences in the location of sources in standardized space for each of the five deviants and between the patient and control groups. There were no differences in location between the five deviant tones, F(4, 108) = 0.12, ns, nor between the groups (controls: X = 45.34, Y = −16.23, Z = 2.19; patients: X = 46.47, Y = −18.26, Z = 1.86), F(1, 27) = 0.37, ns. The two sources accounted for a mean of 86.47% of global variance in patients and 91.26% in controls.
Statistical analyses were conducted on the waveforms from the primary orientation of each regional source. The mean amplitude and the first peak latency were estimated during an interval of 100–200 msec for the MMN waveform (to capture the likely MMN based on previous literature; Bronnick et al., 2010; Näätänen & Kahkonen, 2009; Thonnessen et al., 2008; Näätänen, Jacobsen, & Winkler, 2005; Engeland et al., 2002; Pekkonen et al., 2001; Pekkonen, 2000) and the peak negative amplitude within 50–150 msec for the standard tone waveform (to include the M100). Two repeated-measures ANOVAs were used to examine differences in Amplitude and Latency of the five deviant types (duration, frequency, side of tone, gap, and intensity) from the left and right auditory cortical sources, with Disease as a between-subject condition (bvFTD patients vs. Controls). To examine group differences in response to the standard tone, four t tests were used to test amplitude and latency differences in the M100 for the right and left cortical sources. Where appropriate, statistics were corrected using Greenhouse–Geisser estimates and considered significant at p < .05.
Model 2: Coherence Analysis
A multidipole model with six fixed regional sources was used to explore coherence among prespecified regions, including bilateral temporal sources (based on the optimal location of both groups in Model 1), frontal sources (MNI coordinates +/−35, 33, 28), and parietal sources (+/−34, −71, 13) fitted to each participant by optimal orientation. The frontal and parietal source locations were based on the BESA auditory-evoked potentials standard source montage. Inversion procedures were the same as Model 1.
We used coherence to examine network connectivity, providing a measure of the relationships between spatially segregated signals in the frequency domain (Rossini, Rossi, Babiloni, & Polich, 2007; Hoechstetter et al., 2004; Thatcher, Krause, & Hrybyk, 1986). Each participant’s six source model was used as a source montage for coherence analysis of single trial data, bandpass-filtered between 10 and 100 Hz, and notch filtered at 50 Hz. Coherence analysis was estimated on all deviant tones together (to provide a measure of global change detection, rather than investigating each deviant type separately) and all standard tones averaging the cross-spectral density between sources over trials and normalizing by the averaged auto-spectral densities (Hoechstetter et al., 2004). A lower limit of 10 Hz was used to include induced alpha oscillatory responses but reduce the contribution of evoked responses. For group comparisons, the coherence data for each subject was averaged over the principal MMN period (150 ± 25 msec) for the following frequencies: Alpha band (10–12 Hz), Beta band (14–30 Hz), and three Gamma Bands (1: 30–50 Hz, 2: 50–70 Hz, 3: 70–100 Hz).
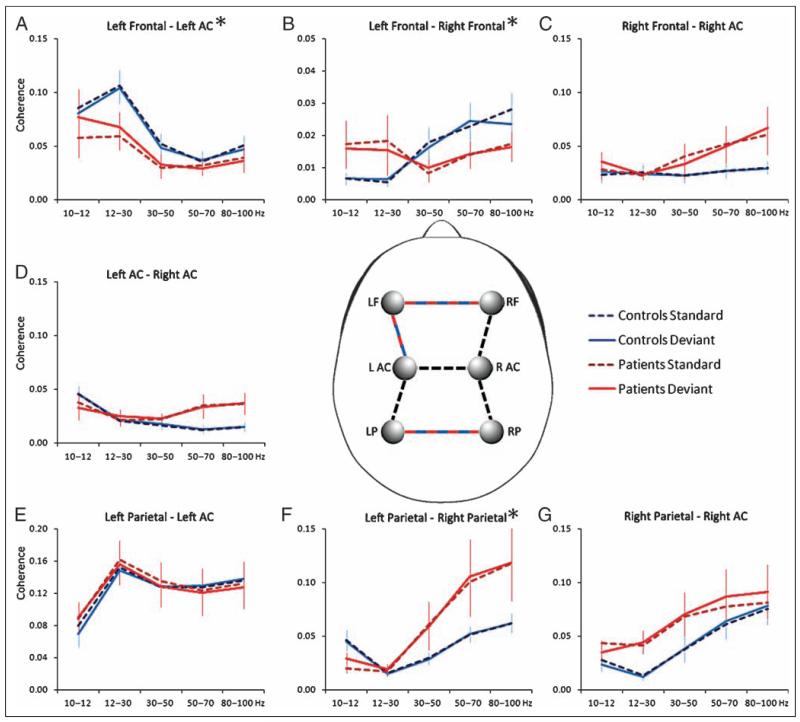
Coherence was analyzed in a multivariate repeated-measures ANOVA including a between-participant factor comparing patients and controls, with Tone Type (all standard tones vs. all deviant tones) and Frequency Band (alpha, beta, gamma1, gamma2, gamma3) as independent variables, and Source Connection included as dependent variables (seven levels, representing seven potential connections within and between hemispheres, illustrated in Figure 2, center). Pillai’s trace is reported for multivariate analyses and the F ratio for univariate tests. Degrees of freedom were corrected using Greenhouse–Geisser estimates for nonsphericity where appropriate. Effects were considered significant at p < .05.
Figure 2.
Source coherence model (Model 2) of six sources within bilateral temporal (ACL and ACR), frontal (FL and FR), and parietal (PL and PR) cortex. This model was fitted to each participants’ averaged data by optimizing orientation of dipoles. Time frequency analysis of single trial data was then used to estimate coherence among sources. The center panel illustrates the six sources of the model. The dotted lines indicate the seven source connections included in the MANOVA; the connections that significantly differ between patients and controls are highlighted in red and blue. The seven plots show mean coherence of the connections, for each group, for the standard and deviant tones. The three plots marked with an asterisk indicate significant interactions between patients and controls (see Results): Plot A shows left frontotemporal α and β coherence is reduced in patients particularly for the standard tones; plots B and F show significant interactions in interhemispheric coherence between frequency bandwidth and group, with reduced frontal (B) and increased parietal (F) gamma coherence in patients.
RESULTS
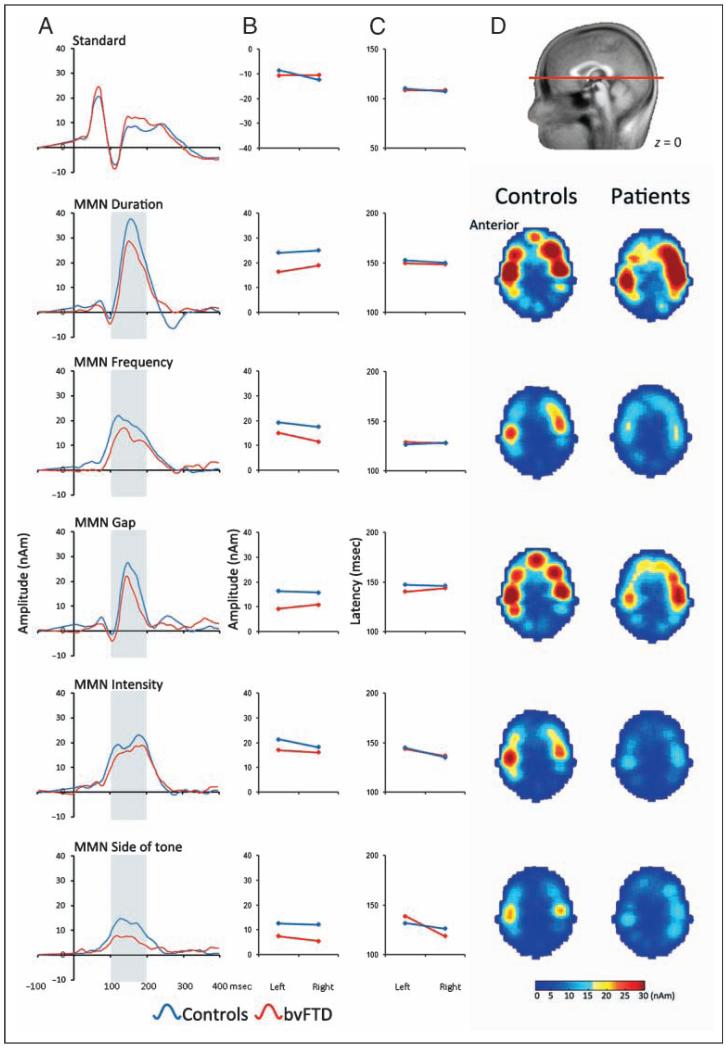
Evoked Response to the Standard Tone (Model 1)
All participants showed the normal M100 response to the standard tone (see Figure 1). There was no significant difference in the amplitude of the M100 in patients compared with controls (Left: controls mean amp = −8.5 nAm, SE = 3.7, patients mean amp = −10.6 nAm, SE = 2.9; t(27) = 0.39, ns; Right: controls mean amp = −12.3 nAm, SE = 3.2, patients mean amp = −10.5 nAm, SE = 2.1; t(27) = 0.4, ns). There was no difference in the latency of the peak amplitude lateralized within either left or right auditory cortex (Left: controls peak latency mean = 110 msec, SE = 2.6 msec, patients mean = 108 msec, SE = 2.3 msec, t(27) = 0.41, ns: Right: controls mean = 107 msec, SE = 2.8, patients mean = 108 msec, SE = 2.9, t(27) = 0.31, ns). This suggests that patients and controls had comparable auditory-evoked responses to the standard tone stimuli, and therefore, any differences in the MMN response are not attributable to hearing impairments.
Figure 1.
(A) Mean source waveforms of the standard tone and the MMN waveform for each deviant tone type (deviant tone–standard tone), averaged across left and right auditory cortex. Waveforms are estimated from bilateral dipoles fitted to sources across a 50–150 msec epoch for the standard tone and 100–200 msec epochs for each of the deviant tone types (described in Model 1; see Methods). (B, C) Mean epoch amplitude and first peak latency extracted from the waveforms. Amplitude is clearly reduced for patients for each deviant tone type, but peak latency is not different from controls. (D) The temporal and frontal sources are illustrated using standardized low-resolution brain electromagnetic tomography (sLORETA). Slices displayed are through the auditory cortex (z = 0, MNI) and show localized activity for each of the MMN epochs (averaged 100–200 msec).
Evoked MMN Waveform (Model 1)
For each participant’s MMN waveform, the average amplitude and latency of the peak amplitude were calculated during an interval of 100–200 msec for each deviant separately. There were overall significant amplitude differences between patients and controls, with patients having a diminished response compared with controls, F(1, 27) = 5.3, p = .029. However, this group effect did not interact with deviant type, F(2.9, 78.2) = 0.3, ns, or lateralization of auditory cortical response, F(1, 27) = 0.12, ns. There was a significant amplitude difference between the five deviant types, F(2.9, 78.2) = 17.4, p < .001, with the greatest MMN response to the duration deviant and the smallest response to the side of sound source deviant. Deviant type also interacted with lateralization of auditory response, F(3.5, 95) = 4.3, p = .004, with right auditory cortex having a marginally greater MMN amplitude than left (see Figure 1).
There were no effects of Disease on peak latency: Patients and controls did not differ in the latency of the peak response, F(1, 27) = 0.1, ns, and there were no interactions of disease with deviant type, F(4, 108) = 1.05, ns, nor disease with lateralization of response, F(1, 27) = 0.4, ns. There was a significant latency difference between the five deviant types, F(4, 108) = 14.4, p < .001; the frequency deviant had the earliest peak response, and duration and intensity deviants had the latest peak. There were no other significant effects.
There were no significant correlations between cognitive measures of disease severity (MMSE and ACE-r) and amplitude of the MMN. However, it should be noted that, although the ACE-r is sensitive to the presence of bvFTD and can reliably track a patients clinical progression, a given score does not represent an objective marker of the neuropathological stages of disease.
Coherence Analysis (Model 2)
Coherence was used to explore network connectivity, comparing tone type (all the deviant tones and all the standard tones), among six prespecified regions, including bilateral frontal, temporal, and parietal sources across five frequency bands (alpha, beta, and three gamma bands). A repeated-measures multivariate analysis did not identify any overall categorical coherence differences between the patient and control groups (Pillai’s trace = 0.3, F(7, 21) = 1.3, p = ns). There were significant interactions between Group and Tone Type (Pillai’s trace = 0.46, F(7, 21) = 2.5, p = .04), between Group and Frequency Band (Pillai’s trace = 0.45, F(28, 420) = 1.9, p = .004), and between Group, Tone Type, and Frequency Band (Pillai’s trace = 0.49, F(28, 420) = 2.1, p = .001). These critical higher-order interactions indicate that group differences were greater when comparing coherence for the deviant and standard tone types in a subset of frequency bands.
The significant interactions of interest were examined in the univariate analyses to indicate which source connections had the greatest differences. The significant interaction between Group and Tone Type was driven by changes within left frontotemporal connectivity, F(1, 27) = 6.9, p = .014. The significant interaction between Group, Tone Type, and Frequency Band was also driven by changes within left frontotemporal connectivity, F(1.9, 53.7) = 4.5, p = .016, respectively. These changes were evident in the alpha and beta bandwidths, for which patients have reduced coherence for the standard tone (Figure 2A). The significant interaction between Group and Frequency Band was due to changes in interhemispheric connections between the frontal sources, F(1.5, 42.9) = 4, p = .033 (Figure 2B), and between the parietal sources, F(1.2, 32.6) = 5, p = .025 (Figure 2F). These interactions were confirmed in a post hoc repeated-measures ANOVA of Connection (parietal vs. frontal) by Frequency (5 bands), by Tone Type (Deviant vs. Standard), between groups (patients vs. controls). The results show a significant interaction between Group and Site, F(1, 27) = 4.4, p = .04, suggesting that patients have relatively decreased frontal gamma coherence and increased parietal gamma coherence.
DISCUSSION
Our results show that the bvFTD impairs the automatic detection of sensory change. The global reduction of MMN to all deviant types was not attributable to an impairment of auditory cortical processing of standard tones. In addition, bvFTD changed the connectivity among frontal, temporal, and parietal cortices, specifically reducing beta band coherence in frontotemporal connections and reducing gamma coherence between frontal interhemispheric sources. However, coherence was not simply reduced in bvFTD, and coherence changes were not restricted to the deviant tone types. Rather, network connectivity was reorganized in an anatomically specific and frequency-specific manner, including an increase in gamma coherence between parietal sources to both tone types.
It is striking that bvFTD affected the response to all types of deviant stimuli, suggesting a global deficit of MMN generation. The MMN has been described as an index of many cognitive operations, including memory, language, and attention, and selective changes have been observed in neurodegenerative and psychiatric syndromes, for example, in Parkinson disease, Alzheimer disease, Huntington disease, and schizophrenia (Bronnick et al., 2010; Näätänen & Kahkonen, 2009; Thonnessen et al., 2008; Engeland et al., 2002; Pekkonen et al., 2001; Pekkonen, 2000). There are several interpretations of this phenomenon. One influential hypothesis explains the MMN as evidence of local sensory memory traces in sensory cortex, including auditory cortex (Näätänen, Paavilainen, Rinne, & Alho, 2007; Näätänen et al., 2005). This mnemonic hypothesis further suggests that the local sensory memory traces are an essential precursor for an auditory change detection mechanism, which triggers attentional switches to unattended auditory stimuli. Attentional deficits are a core symptom of bvFTD, and a dysfunction of early preattentional processes, as measured by the MMN, might contribute toward this impairment. The mechanism of the impairment was examined further in the network connectivity analyses.
We proposed that bvFTD neurodegeneration is associated with changes in distributed neural network connectivity. This was tested using time–frequency coherence analysis of MEG, which enables the identification of changes in specific frequency ranges. The frontotemporal interactions revealed a complex asymmetric pattern. This may reflect functional asymmetries in the normal auditory MMN (Nicol et al., 2012; Garrido, Kilner, Kiebel, et al., 2009) or asymmetry of neuropathology that is seen with some pathological subtypes of bvFTD (Rohrer, Ridgway, et al., 2010).
In our study, left frontotemporal coherence was reduced in bvFTD, in the lower-frequency bands and particularly to the standard tone, compared with the healthy controls. The role of these lower-frequency oscillations remains controversial (Engel & Fries, 2010). Frontotemporal phase synchronization in alpha and beta frequencies has previously been reported to contribute towards MMN responses (Hsiao et al., 2010). In motor control at least, beta oscillations signal the stability of a system, reducing before voluntary phase transitions and increasing in response to errors (Swann et al., 2009). In nonmotor paradigms, top–down attentional processes or feedback modulation have been strongly associated with induced beta oscillations (Buschman & Miller, 2009; Iversen, Repp, & Patel, 2009).
Both imaging (Boly et al., 2011; Garrido, Kilner, Kiebel, et al., 2009) and lesion studies (Alain et al., 1998; Alho et al., 1994) suggest that the MMN is dependent on feedback connections from frontal cortical regions. The role of feedback connections, specifically in the low-frequency bandwidths (Kiebel et al., 2008), has been described within the framework of predictive coding (Wang, 2011; Friston & Kiebel, 2009; Mumford, 1992), which has recently been reformulated to describe the MMN in terms of a generic neural function. Garrido, Friston, and colleagues suggest the MMN response is to a mismatch between sensation and expectation (Friston & Kiebel, 2009; Garrido, Kilner, Stephan, & Friston, 2009). Expectations or predictions are derived from the regularity of standard tones, which are violated by a deviant tone, resulting in an MMN. This is not incompatible with the influential mnemonic hypothesis (Kujala & Näätänen, 2010) but represents a generalization, which accommodates multiple cognitive processes (den Ouden, Friston, Daw, McIntosh, & Stephan, 2009; Friston & Kiebel, 2009; Summerfield, Egner, Mangels, & Hirsch, 2006; Flanagan, Vetter, Johansson, & Wolpert, 2003).
A deficit of this core cognitive process, even at an early preattentive stage of processing around 150 msec, could therefore contribute to diverse neuropsychiatric features without altering basic motor or sensory functions. A failure to respond differentially to a deviant tone after a series of standard tones might arise from abnormal network processing of the standard tone and a failure to establish a good predictive model. In Alzheimer disease, impaired MMN responses have been related to a deficit in processing the repetitive standard tone (Cheng, Wang, Hsu, & Lin, 2012). In bvFTD, we speculate that the reduced frontotemporal coherence may also reflect a failure to establish a predictive model, and in the auditory cortex, this manifests as an impaired MMN. This reduction of connectivity between regions may not be specific to bvFTD, since patients with Alzheimer’s disease have also revealed a reduction in alpha and beta band synchronization between frontotemporal nodes during resting state (Stam et al., 2006). Earlier evidence also shows that longer distance connections in the alpha band are affected in both Alzheimer’s disease and Lewy body dementia (Franciotti et al., 2006). Although in contrast to our results, de Haan et al. report no reduced synchronization in FTD (de Haan et al., 2009).
The changes in frontotemporal coherence may be compounded by abnormalities of the major frontotemporal white matter tracts with bvFTD (Acosta-Cabronero et al., 2011; Whitwell et al., 2010). An additional potential contributor to the MMN deficit is the reduction in serotonergic projections in bvFTD (Huey, Putnam, & Grafman, 2006; Kahkonen et al., 2005; Ahveninen et al., 2002; Yang & Schmitt, 2001). A role for serotoninergic medication in the bvFTD deficits seen here requires further evaluation, which is beyond the scope of this study.
The changes in transcallosal coherence were most evident in the gamma range (>30 Hz). In bvFTD, patients had reduced gamma oscillatory coupling between frontal hemispheres, compared with the healthy control participants. Gamma oscillations are a feature of many cognitive tasks including perceptual binding, learning, attention, language, and object perception (Fries, 2009). There is evidence of enhanced neuronal communication through gamma coherence (Womelsdorf et al., 2007; Fries, Reynolds, Rorie, & Desimone, 2001; Azouz & Gray, 2000) with a direct impact on the selection of behaviorally relevant stimuli (Fries et al., 2001). Of special relevance are early gamma oscillations (<150 msec) reported to increase for between local intraregional frontal connections for standard tones (Nicol et al., 2012), potentially related to the matching of top–down predictions with bottom–up inputs (Herrmann, Munk, & Engel, 2004).
The loss of frontal interhemispheric coherence in the gamma range in the bvFTD patients is potentially important because the selective pathology in the superficial layers of the prefrontal cortex may provide a plausible account for these effects. These superficial layers tend to oscillate with faster (gamma) frequencies (Arnal et al., 2011; Buffalo et al., 2011; van Aerde et al., 2009) and contain the superficial pyramidal cells that are thought to report prediction errors necessary for predictive coding (Friston & Kiebel, 2009; Mumford, 1992).
Further to the reduced transcallosal gamma coherence between frontal lobes, bvFTD patients also had increased gamma coherence between parietal lobes. Given the typical rostro-caudal gradient of pathology and atrophy in bvFTD, it is likely that the parietal cortex was relatively spared in our patients. This pattern is in contrast to patients with mild cognitive impairment who, during a memory task, are reported to have increased frontal interhemispheric gamma synchronization (Bajo et al., 2010) and loss of gamma power in parietal cortex (Aurtenetxe et al., 2012).
If gamma coherence enhances communication within networks the increased posterior gamma coherence may represent a compensatory functional reorganization in parietal association cortex. Reorganization of functional connectivity, including enhancement within the less damaged distributed cortical networks, has been noted previously in bvFTD. For example, Zhou and colleagues identified enhanced connectivity in the default mode network using fMRI (Zhou et al., 2010), whereas de Haan and colleagues observed enhanced clustering metrics in EEG (de Haan et al., 2009). It is possible that the enhanced parietal gamma coherence results from a loss of parietal suppression by frontoparietal projections. However, in other conditions such as stroke and Alzheimer disease, interhemispheric functional connectivity correlated with preserved cognitive and motor function (Carter et al., 2010; Stam et al., 2006; Strens et al., 2004) suggesting compensation rather than loss of suppression as the basis for increased connectivity.
There are several limitations to our study. First, we do not have postmortem pathological confirmation, although it is likely that both tau and TDP-43 pathologies are present. Second, we assessed our patients at one time point and on their usual medication. Further work is required to show how these changes progress over time or correlate with disease progression. Third, we used a canonical realistic head model for source analysis, coregistered to fiducial markers and scalp but not a subject-specific MRI (patients’ MRI scans had been on clinical diagnostic scanners rather than a single sequence close in time to the MEG). It could be argued that group differences in MMN are confounded by atrophy. Against this, however, is that responses to standard tones were normal in location, amplitude, and latency and that coherence effects were frequency specific not global. Despite theoretical advantages for individual MRI-based methods, the forward model for MEG (in contrast to EEG) is similar for individualized models and a canonical realistic head model (Henson, Mattout, Phillips, & Friston, 2009). The model is most dependent on the inner skull surface (Hamalainen & Sarvas, 1989), which is a priori unlikely to change with bvFTD. With severe atrophy, cortical sources could be further from the gradiometers, although when using realistic head models, errors in estimation of localization and amplitude of MEG sources increase minimally for sources 2–3 cm from the skull (Tarkiainen, Liljestrom, Seppa, & Salmelin, 2003). While important considerations, these anatomical and modeling artifacts are unlikely to be the major cause of the impairments we observe in bvFTD.
Finally, we make no claim that these observed changes in MEG source amplitudes or network coherence are specific to bvFTD. Indeed, a broad range of pathologies may affect the MMN, and we do not propose diagnostic specificity, but note that the deficits are seen here with all types of deviant tones. Nonetheless, within a given patient population, these MEG effects may provide a neurophysiological biomarker, potentially capable of assessing the impact of novel therapies for disease modification or symptomatic benefit, in terms of their restoration of functional connectivity or in terms of facilitated compensation among the brain networks supporting critical cognitive processes.
In conclusion, we have shown that damage to the frontal lobe and frontotemporal connections in the bvFTD impairs the automatic detection of change (or unexpected events) in auditory cortex. This is accompanied by reductions in frontotemporal beta coherence to the standard tone and reduced interfrontal and increased parietal gamma coherence to both standard and deviant tones. These changes have some features in common with other degenerative dementias and mild cognitive impairment but also present differences. Whether the pattern of reduced interfrontal coherence and increased interparietal coherence is specific to bvFTD or could be utilized to enhance the specificity of the disease profile remains to be tested. We interpret these results in terms of an impairment of the prediction of sensory events through frontal and temporal cortical interactions. These impairments contrast with preservation of the response to M100 in temporal cortex. The results contribute to the emerging systems level analysis of FTD including the reorganization of distributed networks, including the enhancement of connectivity among regions that are relatively less affected by the direct neuropathology.
Acknowledgments
This work has been supported by the Wellcome Trust (088324), the Medical Research Council’s Cognition and Brain Sciences Unit (MC-A060-5PQ30), and the NIHR Cambridge Comprehensive Biomedical Research Centre. We are grateful to Professor John Hodges for his comments on the manuscript in preparation.
REFERENCES
- Acosta-Cabronero J, Patterson K, Fryer TD, Hodges JR, Pengas G, Williams GB, et al. Atrophy, hypometabolism and white matter abnormalities in semantic dementia tell a coherent story. Brain. 2011;134:2025–2035. doi: 10.1093/brain/awr119. [DOI] [PubMed] [Google Scholar]
- Ahveninen J, Kahkonen S, Pennanen S, Liesivuori J, Ilmoniemi RJ, Jaaskelainen IP. Tryptophan depletion effects on EEG and MEG responses suggest serotonergic modulation of auditory involuntary attention in humans. Neuroimage. 2002;16:1052–1061. doi: 10.1006/nimg.2002.1142. [DOI] [PubMed] [Google Scholar]
- Alain C, Woods DL, Knight RT. A distributed cortical network for auditory sensory memory in humans. Brain Research. 1998;812:23–37. doi: 10.1016/s0006-8993(98)00851-8. [DOI] [PubMed] [Google Scholar]
- Alho K, Woods DL, Algazi A, Knight RT, Näätänen R. Lesions of frontal cortex diminish the auditory mismatch negativity. Electroencephalography and Clinical Neurophysiology. 1994;91:353–362. doi: 10.1016/0013-4694(94)00173-1. [DOI] [PubMed] [Google Scholar]
- Arnal LH, Wyart V, Giraud AL. Transitions in neural oscillations reflect prediction errors generated in audiovisual speech. Nature Neuroscience. 2011;14:797–801. doi: 10.1038/nn.2810. [DOI] [PubMed] [Google Scholar]
- Aurtenetxe S, Castellanos NP, Moratti S, Bajo R, Gil P, Beitia G, et al. Dysfunctional and compensatory duality in mild cognitive impairment during a continuous recognition memory task. 2012 doi: 10.1016/j.ijpsycho.2012.11.008. International Journal of Psychophysiology. doi:10.1016/j.ipsycho.2012.11.008. [DOI] [PubMed] [Google Scholar]
- Azouz R, Gray CM. Dynamic spike threshold reveals a mechanism for synaptic coincidence detection in cortical neurons in vivo. Proceedings of the National Academy of Sciences, U.S.A. 2000;97:8110–8115. doi: 10.1073/pnas.130200797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bajo R, Maestu F, Nevado A, Sancho M, Gutierrez R, Campo P, et al. Functional connectivity in mild cognitive impairment during a memory task: Implications for the disconnection hypothesis. Journal of Alzheimer’s Disease. 2010;22:183–193. doi: 10.3233/JAD-2010-100177. [DOI] [PubMed] [Google Scholar]
- Boly M, Garrido MI, Gosseries O, Bruno MA, Boveroux P, Schnakers C, et al. Preserved feedforward but impaired top-down processes in the vegetative state. Science. 2011;332:858–862. doi: 10.1126/science.1202043. [DOI] [PubMed] [Google Scholar]
- Boxer AL, Boeve BF. Frontotemporal dementia treatment: Current symptomatic therapies and implications of recent genetic, biochemical, and neuroimaging studies. Alzheimer Disease & Associated Disorders. 2007;21:S79–S87. doi: 10.1097/WAD.0b013e31815c345e. [DOI] [PubMed] [Google Scholar]
- Bronnick KS, Nordby H, Larsen JP, Aarsland D. Disturbance of automatic auditory change detection in dementia associated with Parkinson’s disease: A mismatch negativity study. Neurobiology of Aging. 2010;31:104–113. doi: 10.1016/j.neurobiolaging.2008.02.021. [DOI] [PubMed] [Google Scholar]
- Buffalo EA, Fries P, Landman R, Buschman TJ, Desimone R. Laminar differences in gamma and alpha coherence in the ventral stream. Proceedings of the National Academy of Sciences, U.S.A. 2011;108:11262–11267. doi: 10.1073/pnas.1011284108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buschman TJ, Miller EK. Serial, covert shifts of attention during visual search are reflected by the frontal eye fields and correlated with population oscillations. Neuron. 2009;63:386–396. doi: 10.1016/j.neuron.2009.06.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cairns NJ, Bigio EH, Mackenzie IR, Neumann M, Lee VM, Hatanpaa KJ, et al. Neuropathologic diagnostic and nosologic criteria for frontotemporal lobar degeneration: Consensus of the Consortium for Frontotemporal Lobar Degeneration. Acta Neuropathologica. 2007;114:5–22. doi: 10.1007/s00401-007-0237-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carter AR, Astafiev SV, Lang CE, Connor LT, Rengachary J, Strube MJ, et al. Resting interhemispheric functional magnetic resonance imaging connectivity predicts performance after stroke. Annals of Neurology. 2010;67:365–375. doi: 10.1002/ana.21905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng CH, Wang PN, Hsu WY, Lin YY. Inadequate inhibition of redundant auditory inputs in Alzheimer’s disease: An MEG study. Biological Psychology. 2012;89:365–373. doi: 10.1016/j.biopsycho.2011.11.010. [DOI] [PubMed] [Google Scholar]
- de Haan W, Pijnenburg YA, Strijers RL, van der Made Y, van der Flier WM, Scheltens P, et al. Functional neural network analysis in frontotemporal dementia and Alzheimer’s disease using EEG and graph theory. BMC Neuroscience. 2009;10:101. doi: 10.1186/1471-2202-10-101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Haan W, van der Flier WM, Wang H, Van Mieghem PF, Scheltens P, Stam CJ. Disruption of functional brain networks in Alzheimer’s disease: What can we learn from graph spectral analysis of resting-state magnetoencephalography? Brain Connect. 2012;2:45–55. doi: 10.1089/brain.2011.0043. [DOI] [PubMed] [Google Scholar]
- den Ouden HE, Friston KJ, Daw ND, McIntosh AR, Stephan KE. A dual role for prediction error in associative learning. Cerebral Cortex. 2009;19:1175–1185. doi: 10.1093/cercor/bhn161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doeller CF, Opitz B, Mecklinger A, Krick C, Reith W, Schroger E. Prefrontal cortex involvement in preattentive auditory deviance detection: Neuroimaging and electrophysiological evidence. Neuroimage. 2003;20:1270–1282. doi: 10.1016/S1053-8119(03)00389-6. [DOI] [PubMed] [Google Scholar]
- Engel AK, Fries P. Beta-band oscillations-signalling the status quo? Current Opinion in Neurobiology. 2010;20:156–165. doi: 10.1016/j.conb.2010.02.015. [DOI] [PubMed] [Google Scholar]
- Engeland C, Mahoney C, Mohr E, Ilivitsky V, Knott V. Nicotine and sensory memory in Alzheimer’s disease: An event-related potential study. Brain and Cognition. 2002;49:232–234. [PubMed] [Google Scholar]
- Flanagan JR, Vetter P, Johansson RS, Wolpert DM. Prediction precedes control in motor learning. Current Biology. 2003;13:146–150. doi: 10.1016/s0960-9822(03)00007-1. [DOI] [PubMed] [Google Scholar]
- Franciotti R, Iacono D, Della Penna S, Pizzella V, Torquati K, Onofrj M, et al. Cortical rhythms reactivity in AD, LBD and normal subjects: A quantitative MEG study. Neurobiology of Aging. 2006;27:1100–1109. doi: 10.1016/j.neurobiolaging.2005.05.027. [DOI] [PubMed] [Google Scholar]
- Fries P. Neuronal gamma-band synchronization as a fundamental process in cortical computation. Annual Review of Neuroscience. 2009;32:209–224. doi: 10.1146/annurev.neuro.051508.135603. [DOI] [PubMed] [Google Scholar]
- Fries P, Reynolds JH, Rorie AE, Desimone R. Modulation of oscillatory neuronal synchronization by selective visual attention. Science. 2001;291:1560–1563. doi: 10.1126/science.1055465. [DOI] [PubMed] [Google Scholar]
- Friston KJ, Daunizeau J, Kilner J, Kiebel SJ. Action and behavior: A free-energy formulation. Biological Cybernetics. 2010;102:227–260. doi: 10.1007/s00422-010-0364-z. [DOI] [PubMed] [Google Scholar]
- Friston KJ, Dolan RJ. Computational and dynamic models in neuroimaging. Neuroimage. 2010;52:752–765. doi: 10.1016/j.neuroimage.2009.12.068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friston KJ, Kiebel SJ. Predictive coding under the free-energy principle. Philosophical Transactions of the Royal Society of London, Series B. Biological Sciences. 2009;364:1211–1221. doi: 10.1098/rstb.2008.0300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garrido MI, Friston KJ, Kiebel SJ, Stephan KE, Baldeweg T, Kilner JM. The functional anatomy of the MMN: A DCM study of the roving paradigm. Neuroimage. 2008;42:936–944. doi: 10.1016/j.neuroimage.2008.05.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garrido MI, Kilner JM, Kiebel SJ, Friston KJ. Dynamic causal modeling of the response to frequency deviants. Journal of Neurophysiology. 2009;101:2620–2631. doi: 10.1152/jn.90291.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garrido MI, Kilner JM, Stephan KE, Friston KJ. The mismatch negativity: A review of underlying mechanisms. Clinical Neurophysiology. 2009;120:453–463. doi: 10.1016/j.clinph.2008.11.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giard MH, Perrin F, Pernier J, Bouchet P. Brain generators implicated in the processing of auditory stimulus deviance: A topographic event-related potential study. Psychophysiology. 1990;27:627–640. doi: 10.1111/j.1469-8986.1990.tb03184.x. [DOI] [PubMed] [Google Scholar]
- Gordon E, Rohrer JD, Kim LG, Omar R, Rossor MN, Fox NC, et al. Measuring disease progression in frontotemporal lobar degeneration: A clinical and MRI study. Neurology. 2010;74:666–673. doi: 10.1212/WNL.0b013e3181d1a879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamalainen MS, Sarvas J. Realistic conductivity geometry model of the human head for interpretation of neuromagnetic data. IEEE Transactions on Biomedical Engineering. 1989;36:165–171. doi: 10.1109/10.16463. [DOI] [PubMed] [Google Scholar]
- Hampton DW, Webber DJ, Bilican B, Goedert M, Spillantini MG, Chandran S. Cell-mediated neuroprotection in a mouse model of human tauopathy. Journal of Neuroscience. 2010;30:9973–9983. doi: 10.1523/JNEUROSCI.0834-10.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henson RN, Mattout J, Phillips C, Friston KJ. Selecting forward models for MEG source-reconstruction using model-evidence. Neuroimage. 2009;46:168–176. doi: 10.1016/j.neuroimage.2009.01.062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herrmann CS, Munk MH, Engel AK. Cognitive functions of gamma-band activity: Memory match and utilization. Trends in Cognitive Sciences. 2004;8:347–355. doi: 10.1016/j.tics.2004.06.006. [DOI] [PubMed] [Google Scholar]
- Hoechstetter K, Bornfleth H, Weckesser D, Ille N, Berg P, Scherg M. BESA source coherence: A new method to study cortical oscillatory coupling. Brain Topography. 2004;16:233–238. doi: 10.1023/b:brat.0000032857.55223.5d. [DOI] [PubMed] [Google Scholar]
- Horwitz B, Rowe JB. Functional biomarkers for neurodegenerative disorders based on the network paradigm. Progress in Neurobiology. 2011;95:505–509. doi: 10.1016/j.pneurobio.2011.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hsiao FJ, Cheng CH, Liao KK, Lin YY. Cortico-cortical phase synchrony in auditory mismatch processing. Biological Psychology. 2010;84:336–345. doi: 10.1016/j.biopsycho.2010.03.019. [DOI] [PubMed] [Google Scholar]
- Huey ED, Putnam KT, Grafman J. A systematic review of neurotransmitter deficits and treatments in frontotemporal dementia. Neurology. 2006;66:17–22. doi: 10.1212/01.wnl.0000191304.55196.4d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes LE, Nestor PJ, Hodges JR, Rowe JB. Magnetoencephalography of frontotemporal dementia: Spatiotemporally localized changes during semantic decisions. Brain. 2011;134:2513–2522. doi: 10.1093/brain/awr196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iversen JR, Repp BH, Patel AD. Top–down control of rhythm perception modulates early auditory responses. Annals of the New York Academy of Sciences. 2009;1169:58–73. doi: 10.1111/j.1749-6632.2009.04579.x. [DOI] [PubMed] [Google Scholar]
- Kahkonen S, Makinen V, Jaaskelainen IP, Pennanen S, Liesivuori J, Ahveninen J. Serotonergic modulation of mismatch negativity. Psychiatry Research. 2005;138:61–74. doi: 10.1016/j.pscychresns.2004.09.006. [DOI] [PubMed] [Google Scholar]
- Kiebel SJ, Daunizeau J, Friston KJ. A hierarchy of time-scales and the brain. PLoS Computational Biology. 2008;4:e1000209. doi: 10.1371/journal.pcbi.1000209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kipps CM, Hodges JR, Fryer TD, Nestor PJ. Combined magnetic resonance imaging and positron emission tomography brain imaging in behavioural variant frontotemporal degeneration: Refining the clinical phenotype. Brain. 2009;132:2566–2578. doi: 10.1093/brain/awp077. [DOI] [PubMed] [Google Scholar]
- Kipps CM, Hodges JR, Hornberger M. Nonprogressive behavioural frontotemporal dementia: Recent developments and clinical implications of the “bvFTD phenocopy syndrome”. Current Opinion in Neurology. 2010;23:628–632. doi: 10.1097/WCO.0b013e3283404309. [DOI] [PubMed] [Google Scholar]
- Kujala T, Näätänen R. The adaptive brain: A neurophysiological perspective. Progress in Neurobiology. 2010;91:55–67. doi: 10.1016/j.pneurobio.2010.01.006. [DOI] [PubMed] [Google Scholar]
- Liasis A, Towell A, Alho K, Boyd S. Intracranial identification of an electric frontal-cortex response to auditory stimulus change: A case study. Brain Research, Cognitive Brain Research. 2001;11:227–233. doi: 10.1016/s0926-6410(00)00077-x. [DOI] [PubMed] [Google Scholar]
- Mackenzie IR. The neuropathology of FTD associated with ALS. Alzheimer Disease & Associated Disorders. 2007;21:S44–S49. doi: 10.1097/WAD.0b013e31815c3486. [DOI] [PubMed] [Google Scholar]
- Mioshi E, Dawson K, Mitchell J, Arnold R, Hodges JR. The Addenbrooke’s Cognitive Examination Revised (ACE-R): A brief cognitive test battery for dementia screening. International Journal of Geriatric Psychiatry. 2006;21:1078–1085. doi: 10.1002/gps.1610. [DOI] [PubMed] [Google Scholar]
- Mumford D. On the computational architecture of the neocortex. II. The role of cortico-cortical loops. Biological Cybernetics. 1992;66:241–251. doi: 10.1007/BF00198477. [DOI] [PubMed] [Google Scholar]
- Näätänen R, Alho K. Generators of electrical and magnetic mismatch responses in humans. Brain Topography. 1995;7:315–320. doi: 10.1007/BF01195257. [DOI] [PubMed] [Google Scholar]
- Näätänen R, Jacobsen T, Winkler I. Memory-based or afferent processes in mismatch negativity (MMN): A review of the evidence. Psychophysiology. 2005;42:25–32. doi: 10.1111/j.1469-8986.2005.00256.x. [DOI] [PubMed] [Google Scholar]
- Näätänen R, Kahkonen S. Central auditory dysfunction in schizophrenia as revealed by the mismatch negativity (MMN) and its magnetic equivalent MMNm: A review. International Journal of Neuropsychopharmacology. 2009;12:125–135. doi: 10.1017/S1461145708009322. [DOI] [PubMed] [Google Scholar]
- Näätänen R, Kujala T, Escera C, Baldeweg T, Kreegipuu K, Carlson S, et al. The mismatch negativity (MMN)—A unique window to disturbed central auditory processing in ageing and different clinical conditions. Clinical Neurophysiology. 2012;123:424–458. doi: 10.1016/j.clinph.2011.09.020. [DOI] [PubMed] [Google Scholar]
- Näätänen R, Kujala T, Kreegipuu K, Carlson S, Escera C, Baldeweg T, et al. The mismatch negativity: An index of cognitive decline in neuropsychiatric and neurological diseases and in ageing. Brain. 2011;134:3435–3453. doi: 10.1093/brain/awr064. [DOI] [PubMed] [Google Scholar]
- Näätänen R, Paavilainen P, Rinne T, Alho K. The mismatch negativity (MMN) in basic research of central auditory processing: A review. Clinical Neurophysiology. 2007;118:2544–2590. doi: 10.1016/j.clinph.2007.04.026. [DOI] [PubMed] [Google Scholar]
- Näätänen R, Pakarinen S, Rinne T, Takegata R. The mismatch negativity (MMN): Towards the optimal paradigm. Clinical Neurophysiology. 2004;115:140–144. doi: 10.1016/j.clinph.2003.04.001. [DOI] [PubMed] [Google Scholar]
- Neary D, Snowden JS, Gustafson L, Passant U, Stuss D, Black S, et al. Frontotemporal lobar degeneration: A consensus on clinical diagnostic criteria. Neurology. 1998;51:1546–1554. doi: 10.1212/wnl.51.6.1546. [DOI] [PubMed] [Google Scholar]
- Nicol RM, Chapman SC, Vertes PE, Nathan PJ, Smith ML, Shtyrov Y, et al. Fast reconfiguration of high-frequency brain networks in response to surprising changes in auditory input. Journal of Neurophysiology. 2012;107:1421–1430. doi: 10.1152/jn.00817.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pekkonen E. Mismatch negativity in aging and in Alzheimer’s and Parkinson’s diseases. Audiology & Neurotology. 2000;5:216–224. doi: 10.1159/000013883. [DOI] [PubMed] [Google Scholar]
- Pekkonen E, Hirvonen J, Jaaskelainen IP, Kaakkola S, Huttunen J. Auditory sensory memory and the cholinergic system: Implications for Alzheimer’s disease. Neuroimage. 2001;14:376–382. doi: 10.1006/nimg.2001.0805. [DOI] [PubMed] [Google Scholar]
- Pereira JM, Williams GB, Acosta-Cabronero J, Pengas G, Spillantini MG, Xuereb JH, et al. Atrophy patterns in histologic vs. clinical groupings of frontotemporal lobar degeneration. Neurology. 2009;72:1653–1660. doi: 10.1212/WNL.0b013e3181a55fa2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pievani M, de Haan W, Wu T, Seeley WW, Frisoni GB. Functional network disruption in the degenerative dementias. Lancet Neurology. 2011;10:829–843. doi: 10.1016/S1474-4422(11)70158-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rascovsky K, Hodges JR, Knopman D, Mendez MF, Kramer JH, Neuhaus J, et al. Sensitivity of revised diagnostic criteria for the behavioural variant of frontotemporal dementia. Brain. 2011;134:2456–2477. doi: 10.1093/brain/awr179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rohrer JD, Geser F, Zhou J, Gennatas ED, Sidhu M, Trojanowski JQ, et al. TDP-43 subtypes are associated with distinct atrophy patterns in frontotemporal dementia. Neurology. 2010;75:2204–2211. doi: 10.1212/WNL.0b013e318202038c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rohrer JD, Ridgway GR, Modat M, Ourselin S, Mead S, Fox NC, et al. Distinct profiles of brain atrophy in frontotemporal lobar degeneration caused by progranulin and tau mutations. Neuroimage. 2010;53:1070–1076. doi: 10.1016/j.neuroimage.2009.12.088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosburg T, Trautner P, Dietl T, Korzyukov OA, Boutros NN, Schaller C, et al. Subdural recordings of the mismatch negativity (MMN) in patients with focal epilepsy. Brain. 2005;128:819–828. doi: 10.1093/brain/awh442. [DOI] [PubMed] [Google Scholar]
- Rossini PM, Rossi S, Babiloni C, Polich J. Clinical neurophysiology of aging brain: From normal aging to neurodegeneration. Progress in Neurobiology. 2007;83:375–400. doi: 10.1016/j.pneurobio.2007.07.010. [DOI] [PubMed] [Google Scholar]
- Rowe J. Connectivity analysis is essential to understand neurological disease. Frontiers in Neuroscience (Reviews) 2010;17:144. doi: 10.3389/fnsys.2010.00144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salmon E, Kerrouche N, Herholz K, Perani D, Holthoff V, Beuthien-Baumann B, et al. Decomposition of metabolic brain clusters in the frontal variant of frontotemporal dementia. Neuroimage. 2006;30:871–878. doi: 10.1016/j.neuroimage.2005.10.016. [DOI] [PubMed] [Google Scholar]
- Schall U, Johnston P, Todd J, Ward PB, Michie PT. Functional neuroanatomy of auditory mismatch processing: An event-related fMRI study of duration-deviant oddballs. Neuroimage. 2003;20:729–736. doi: 10.1016/S1053-8119(03)00398-7. [DOI] [PubMed] [Google Scholar]
- Seeley WW, Crawford R, Rascovsky K, Kramer JH, Weiner M, Miller BL, et al. Frontal paralimbic network atrophy in very mild behavioral variant frontotemporal dementia. Archives of Neurology. 2008;65:249–255. doi: 10.1001/archneurol.2007.38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seeley WW, Crawford RK, Zhou J, Miller BL, Greicius MD. Neurodegenerative diseases target large-scale human brain networks. Neuron. 2009;62:42–52. doi: 10.1016/j.neuron.2009.03.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stam CJ. Use of magnetoencephalography (MEG) to study functional brain networks in neurodegenerative disorders. Journal of the Neurological Sciences. 2010;289:128–134. doi: 10.1016/j.jns.2009.08.028. [DOI] [PubMed] [Google Scholar]
- Stam CJ, Jones BF, Manshanden I, van Cappellen van Walsum AM, Montez T, Verbunt JP, et al. Magnetoencephalographic evaluation of resting-state functional connectivity in Alzheimer’s disease. Neuroimage. 2006;32:1335–1344. doi: 10.1016/j.neuroimage.2006.05.033. [DOI] [PubMed] [Google Scholar]
- Strens LH, Asselman P, Pogosyan A, Loukas C, Thompson AJ, Brown P. Corticocortical coupling in chronic stroke: Its relevance to recovery. Neurology. 2004;63:475–484. doi: 10.1212/01.wnl.0000133010.69694.f8. [DOI] [PubMed] [Google Scholar]
- Summerfield C, Egner T, Mangels J, Hirsch J. Mistaking a house for a face: Neural correlates of misperception in healthy humans. Cerebral Cortex. 2006;16:500–508. doi: 10.1093/cercor/bhi129. [DOI] [PubMed] [Google Scholar]
- Swann N, Tandon N, Canolty R, Ellmore TM, McEvoy LK, Dreyer S, et al. Intracranial EEG reveals a time- and frequency-specific role for the right inferior frontal gyrus and primary motor cortex in stopping initiated responses. Journal of Neuroscience. 2009;29:12675–12685. doi: 10.1523/JNEUROSCI.3359-09.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tarkiainen A, Liljestrom M, Seppa M, Salmelin R. The 3D topography of MEG source localization accuracy: Effects of conductor model and noise. Clinical Neurophysiology. 2003;114:1977–1992. doi: 10.1016/s1388-2457(03)00195-0. [DOI] [PubMed] [Google Scholar]
- Thatcher RW, Krause PJ, Hrybyk M. Cortico-cortical associations and EEG coherence: A two-compartmental model. Electroencephalography and Clinical Neurophysiology. 1986;64:123–143. doi: 10.1016/0013-4694(86)90107-0. [DOI] [PubMed] [Google Scholar]
- Thonnessen H, Zvyagintsev M, Harke KC, Boers F, Dammers J, Norra C, et al. Optimized mismatch negativity paradigm reflects deficits in schizophrenia patients. A combined EEG and MEG study. Biological Psychology. 2008;77:205–216. doi: 10.1016/j.biopsycho.2007.10.009. [DOI] [PubMed] [Google Scholar]
- van Aerde KI, Mann EO, Canto CB, Heistek TS, Linkenkaer-Hansen K, Mulder AB, et al. Flexible spike timing of layer 5 neurons during dynamic beta oscillation shifts in rat prefrontal cortex. Journal of Physiology. 2009;587:5177–5196. doi: 10.1113/jphysiol.2009.178384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wacongne C, Changeux JP, Dehaene S. A neuronal model of predictive coding accounting for the mismatch negativity. Journal of Neuroscience. 2012;32:3665–3678. doi: 10.1523/JNEUROSCI.5003-11.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wacongne C, Labyt E, van Wassenhove V, Bekinschtein T, Naccache L, Dehaene S. Evidence for a hierarchy of predictions and prediction errors in human cortex. Proceedings of the National Academy of Sciences, U.S.A. 2011;108:20754–20759. doi: 10.1073/pnas.1117807108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang XJ. Neurophysiological and computational principles of cortical rhythms in cognition. Physiological Reviews. 2011;90:1195–1268. doi: 10.1152/physrev.00035.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wedderburn C, Wear H, Brown J, Mason SJ, Barker RA, Hodges J, et al. The utility of the Cambridge Behavioural Inventory in neurodegenerative disease. Journal of Neurology, Neurosurgery and Psychiatry. 2008;79:500–503. doi: 10.1136/jnnp.2007.122028. [DOI] [PubMed] [Google Scholar]
- Whitwell JL, Avula R, Senjem ML, Kantarci K, Weigand SD, Samikoglu A, et al. Gray and white matter water diffusion in the syndromic variants of frontotemporal dementia. Neurology. 2010;74:1279–1287. doi: 10.1212/WNL.0b013e3181d9edde. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitwell JL, Jack CR, Jr., Boeve BF, Senjem ML, Baker M, Rademakers R, et al. Voxel-based morphometry patterns of atrophy in FTLD with mutations in MAPT or PGRN. Neurology. 2009;72:813–820. doi: 10.1212/01.wnl.0000343851.46573.67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams GB, Nestor PJ, Hodges JR. Neural correlates of semantic and behavioural deficits in frontotemporal dementia. Neuroimage. 2005;24:1042–1051. doi: 10.1016/j.neuroimage.2004.10.023. [DOI] [PubMed] [Google Scholar]
- Womelsdorf T, Schoffelen JM, Oostenveld R, Singer W, Desimone R, Engel AK, et al. Modulation of neuronal interactions through neuronal synchronization. Science. 2007;316:1609–1612. doi: 10.1126/science.1139597. [DOI] [PubMed] [Google Scholar]
- Yang Y, Schmitt HP. Frontotemporal dementia: Evidence for impairment of ascending serotoninergic but not noradrenergic innervation. Immunocytochemical and quantitative study using a graph method. Acta Neuropathologica. 2001;101:256–270. doi: 10.1007/s004010000293. [DOI] [PubMed] [Google Scholar]
- Zamrini E, Maestu F, Pekkonen E, Funke M, Makela J, Riley M, et al. Magnetoencephalography as a putative biomarker for Alzheimer’s disease. International Journal of Alzheimer’s Disease. 2011;2011:280–289. doi: 10.4061/2011/280289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou J, Gennatas ED, Kramer JH, Miller BL, Seeley WW. Predicting regional neurodegeneration from the healthy brain functional connectome. Neuron. 2012;73:1216–1227. doi: 10.1016/j.neuron.2012.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou J, Greicius MD, Gennatas ED, Growdon ME, Jang JY, Rabinovici GD, et al. Divergent network connectivity changes in behavioural variant frontotemporal dementia and Alzheimer’s disease. Brain. 2010;133:1352–1367. doi: 10.1093/brain/awq075. [DOI] [PMC free article] [PubMed] [Google Scholar]