Abstract
Given the epidemic of obesity, approaches to weight loss that can be applied on a community, state, or national level are needed. We report results from Shape Up Rhode Island 2007 (SURI), a state-wide Internet based program involving team-based competition to increase physical activity and achieve weight loss. A total of 4,717 adults (84% female; mean BMI = 29.6 kg/m2) enrolled in the 16 week weight loss competition of SURI and 3311 completed at least 12 weeks. Completers reported losing 3.2 ± 3.4 kg, and 30% achieved a clinically significant weight loss of 5% or more. Although modest, these weight losses shifted the BMI distribution from a mean BMI of 29.4 to 28.2 kg/m2 and reduced the population that was obese from 39% to 31%. More conservative intent-to-treat analyses and analysis of 132 participants with objective weights still showed a significant reduction in BMI of −0.8 units. These findings suggest that state-wide weight loss campaigns can produce modest weight losses in large numbers of participants. These data provide a bench-mark that can be used for comparisons with other state-wide campaigns. Research on ways to improve such campaigns is needed.
Introduction
Obesity has reached epidemic levels. It is estimated that 66.3% of Americans are overweight and 32.2% are obese. 1 These individuals are at increased risk for a number of medical problems, including hypertension, diabetes, cancer, and cardiovascular disease, disability, and mortality. 2–4 The annual medical cost associated with obesity in America exceeds $75 billion. 5
The treatment for obesity is based on a medical model, where affected individuals receive group or individual counseling regarding diet, exercise and behavioral strategies. These programs, which often involve weekly meetings for six months and then bi-weekly meetings, have been shown to produce weight losses of 7% to 10% of body weight, and to have positive health benefits. 6–8 While effective, such intensive, costly programs cannot service the large and growing population of overweight and obese adults. Commercial and Internet weight loss programs have greater population outreach, but more limited results. 9, 10
Recently a large number of state- and nation-wide programs have been developed that use team-based competitions to increase physical activity and weight loss. These programs, which are often implemented entirely via the Internet, contrast with earlier community- and company sponsored weight loss competitions that included lesson materials and individual weigh-ins. Given the large number of individuals who are participating in these state-wide interventions (e.g. 30,000 in Iowa and 12,000 in Arkansas), it is important to provide some information on their efficacy. The fact that these programs are typically short-term and rely entirely on self-reported data makes them difficult to evaluate.
We report results from 4,717 participants in the weight loss competition of Shape Up Rhode Island, 2007 (www.shapupri.org). In addition, a small validation study is included with objective weights and a subgroup provides 6 month follow-up data. While not a randomized comparison, this analysis provides a bench-mark that can be used for comparisons between this program and other state-wide programs.
Methods
Participants
Shape-Up RI was created in 2005 as a 501 (c) (3) nonprofit organization. The program involves competition among teams for weight loss, pedometer steps, and exercise minutes. Enrollment for the 2007 Shape Up Rhode Island (SURI) campaign began on December 15, 2006 and ended on January 28, 2007. The state’s largest employers were targeted and television advertisements, press releases, and information distributed by employers to their employees were used to recruit participants. A total of 6,815 participants were enrolled in the 2007 SURI program. All participants were required to be either Rhode Island residents or employed in Rhode Island; enrollees were drawn from 38 of the 39 municipalities in Rhode Island.
All participants were required to pay a $15 registration fee to join the program; for 62% of participants this registration fee was paid by their employer. Participants with medical conditions that might affect their ability to safely participate in the program or their ability to exercise were encouraged to obtain written permission from a physician before entering the program.
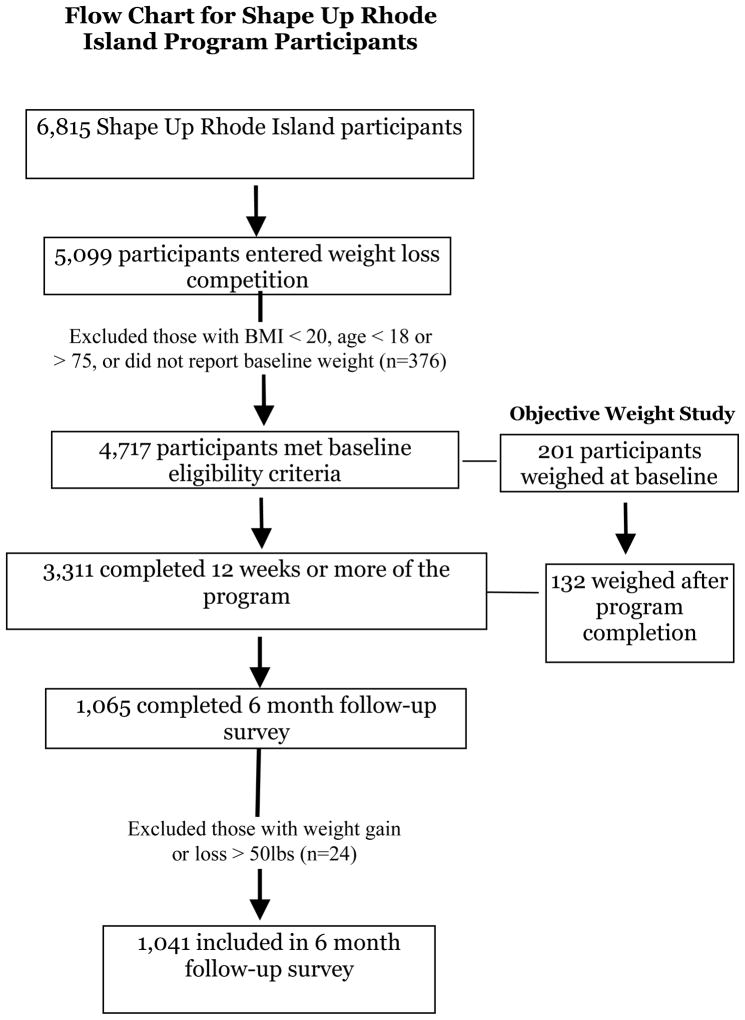
A total of 5,090 participants (74.7% of all SURI participants) entered the weight loss division (98% of whom also participated in the pedometer step or activity minutes division). From these 5,090, we excluded 373 participants who did not meet the study eligibility criteria of having a BMI > 20 kg/m2 (N = 108), age ≥ 18 or ≤ 75 (N = 26), and providing a baseline weight (N = 242). The final sample in this study included 4,717 SURI participants (Figure 1).
Figure 1.
Flow Chart for Shape Up Rhode Island Program Participants
The 4,717 participants included 83.6% females. The average age was 42.6 ± 11.0 years, with 28% of participants between 18 and 35, 46% between 36 and 50, and 26% over 50 years of age. Mean baseline weight was 81.6 kg ± 19.4 kg with a BMI of 29.6 ± 6.2 kg/m2; 24% of the participants had a BMI of 18.5 – 24.9; 35% had a BMI of 25 – 29.9; and 40% had a BMI of > 30.
A sub-group of 201 SURI participants were recruited at the program’s opening event and enrolled in the objective weight substudy. These participants averaged 45.9 ± 10.5 years of age, with a BMI of 31.5 ± 5.7, and 90% were females.
Procedures for SURI 2007
SURI 2007 was a 16-week program supported by contributions from a local hospital and a local insurance company. Participants were required to enroll in SURI as part of a team, with team size of 5 to 11 members. Each team was formed by a captain who registered for the SURI program online through www.shapeupri.org and had the responsibility of recruiting team members, monitoring the progress of their team, and motivating their team members. Teams could choose to compete to lose the most weight, take the most pedometer steps, and/or exercise the largest number of hours. The captains were encouraged to set online team goals for these competitions. Winners of competitions received verbal praise and commendation, but no prizes were provided.
Participants received a digital step pedometer, a blue silicone wristband to showcase their involvement in SURI, and a paper log-book to record their daily information. A robust online software tracking system prompted participants to record their weight, total hours exercised, and/or total pedometer steps every two weeks. This system allowed participant data to be collected and organized in an efficient manner and enabled participants to view their own performance and the performance of their teams versus other teams at the end of every two-week reporting period. Weekly electronic newsletters with updates on the competition and basic information on diet and exercise (e.g., recipe suggestions, local walking events) were also provided.
In addition to this team-based competition, other motivational and educational activities occurred during the 16 week program. The SURI campaign was featured in over thirty newspaper articles and television and radio segments. Participants were invited to attend an opening kick-off event, and over 65 free fitness events and educational workshops took place throughout the state, including sessions on healthy cooking, proper reading of nutrition labels, diabetes management for African American women, pilates classes, ice skating, dancing, and healthy grocery shopping. At the closing awards ceremony, winning teams were congratulated and honored by former Arkansas Governor Mike Huckabee and by Rhode Island Governor Donald Carcieri. Participating companies also provided additional support for their employees; many of these employers paid the registration fee for their employees, hosted ancillary events to publicize the SURI campaign, and/or provided small gifts to their members.
Participants self-reported their weight and physical activity data every two weeks on the SURI tracking system. In addition, they were emailed a six-month follow-up questionnaire to assess their ability to maintain their weight loss over time.
Participants in the objective-weight sub-study were weighed at the opening event by a member of the research team. They were then weighed at the completion of the program either at the closing event or at the participant’s office or home. The baseline objective weigh-in occurred within one week of the baseline self-reported weight in SURI; the follow-up objective weight occurred within four weeks after the SURI final self-reported weight. Participants were paid $5 for completing the final weigh-in.
This study was approved by The Miriam Hospital IRB.
Statistical Analysis
At baseline, participants were instructed to enter their height, weight, and basic demographic data on the SURI tracking system. Height and weight were used to compute body mass index (BMI; wt/ht2); BMI of 18.5–24.9, 25–29.9 and >30 were used to define normal weight, overweight, and obese respectively. Participants also entered their weight every two weeks throughout the 16 week program (eight rounds). For the current analyses, “completers” are defined as those who entered their weight at the end of round 6, 7, or 8 (using the data from the latest round completed). Those who did not complete at least round six are considered non-completers. As a conservative approach to estimating the weight loss of dropouts, these participants were assumed to have remained at their baseline weight. If the team was participating in the physical activity competitions as well, the number of steps and/or the minutes of activity were also entered every two weeks. The physical activity measures were averaged over the eight rounds with missing data omitted from the averages. Analyses for the sub-study on objective weights were based on the participants’ pre and post objective weight measures and comparisons of these results with the information they reported during the campaign.
Results
SURI Completion
A total of 3,311 of the 4717 participants (70.2%) completed SURI, defined as providing data at round 6, 7, or 8 (of the 3311 completers, 2738 had data at round eight, 280 at round seven and 293 at round six). Completers and non-completers did not differ by gender, but completers were older (43.3 ± 10.9 vs. 41.1 ± 11.2 years, p < .001) and less overweight (BMI 29.4 ± 6.1 vs. 30.2 ± 6.4, p < .001) than dropouts (Table 1). Whereas 72% of normal weight and overweight participants completed the program, only 67.7% of the obese completed round 6, 7, or 8 (p < .01).
Table 1.
Baseline Characteristics (Mean ± SD) of Shape Up Rhode Island Participants
| Completers (N = 3,311) | Non-completers (N = 1,406) | Objective Weight Completers (N = 132) | |
|---|---|---|---|
| Age | 43.3 ± 10.9 | 41.1 ± 11.2* | 46.9 ± 10.4* |
| Weight (kg) | 81.1 ± 19.2 | 82.8 ± 19.9* | 85.0 ± 17.1+ |
| BMI | 29.4 ± 6.1 | 30.2 ± 6.4* | 31.3 ± 5.7* |
| Female Gender | 83.4% | 84.1% | 92%* |
Significant difference from completers;
p < .01;
p < .05
Objective weights were assessed on 201 individuals at baseline 132 (66%) of these individuals were also weighed at the end of SURI. The sample with follow-up objective weights was older, heavier, and included a greater proportion of women than the completers of SURI (all p’s < .05). The discrepancy between objective and self-reported weight was examined in 107 of these participants.
Weight Losses
Weight losses are presented (Table 2) for the 3,311 participants who completed round 6, 7, or 8, and for the full cohort of participants (assuming dropouts were at their baseline weight). As shown, the average weight loss for completers was 3.2 ± 3.4 kg; the average weight loss for the full cohort was 2.3 ± 3.2 kg. Of particular note is the fact that 30.2% of the completers reported a clinically significant weight loss of ≥ 5% of their body weight, with 6.3% reporting a 10% weight loss. Only 6% of completers gained weight, and almost equal proportions reported losing 0 – 5 lbs (36%), 5 – 9.9 lb (30%) or > 10 lb (28%). When analyses were restricted to participants who were overweight or obese at baseline, findings were very similar.
Table 2.
Results of Shape Up Rhode Island 2007 Campaign
| Completers (n = 3,311) | Full Cohort (n = 4,717) | Objective Weight Completers (n = 132) | |
|---|---|---|---|
| Weight Loss (kg) | −3.2 ± 3.4 | −2.3 ± 3.2 | −2.3 ± 4.7 |
| Weight Loss (% of initial weight) | −3.8 ± 3.7 | −2.7 ± 3.6 | −2.4 ± 4.7 |
| BMI Change | −1.2 ± 1.2 | −0.8 ± 1.1 | −0.8 ± 1.7 |
| Overweight and Obese (Baseline BMI > 25) | |||
| (n = 2476) | (n = 3565) | (n = 121) | |
| Weight loss (kg) | −3.7 ± 3.6 | −2.6 ± 3.5 | −2.4 ± 4.8 |
| Weight Loss (% of initial weight) | −4.2 ± 3.8 | −2.9 ± 3.7 | −2.5 ± 4.7 |
| BMI Change | −1.3 ± 1.3 | −0.9 ± 1.2 | −0.9 ± 1.7 |
Assuming dropouts were at baseline weight
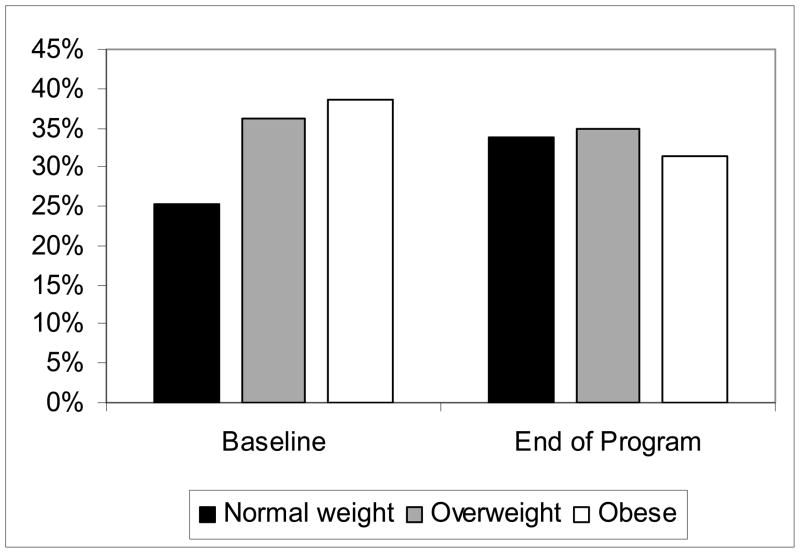
Figure 2 shows that the BMI distribution was shifted significantly over the 16 weeks of SURI (p < .001). At baseline, BMI averaged 29.4 ± 6.1 among completers, but this was significantly reduced to 28.2 ± 5.8 (p < .001) at program completion. Moreover, among completers, 39% of the population was obese at baseline, but only 31% were obese at follow-up. The proportion that was normal weight increased from 25% to 34%. Similar results are seen with all study participants (assuming no weight loss in drop outs). With this approach, BMI decreased from 29.6 ± 6.2 at baseline to 28.8 ± 6.0, (p < .001) and the proportion of the population that was obese decreased from 40% at baseline to 35% at round 8; in contrast, only 24% of the population was normal weight at baseline compared to 30% at round 8.
Figure 2.
Percent of Shape Up Rhode Island completers who were normal weight (BMI of 18 – 25), overweight (BMI of 25 – 30) or obese (BMI > 30) at baseline and at wend (week 16) of the program
In the sub-group of participants with objective weight data (N = 132) weight losses averaged 2.3 ± 4.7 kg., with a 2.4% reduction in their body weight and a −0.8 BMI unit weight reduction. Twenty five percent lost 5% or more of their initial body weight. Although the difference between the self-reported and the objective weights was statistically significant (3.9 ± 4.4 vs. 2.3 ± 4.7 kg, p < .001), the objective weight data confirmed the overall benefit of the SURI program.
Variables Associated with Weight Loss
Further analyses of SURI completers showed that weight losses were greater in those participants who were heavier at baseline (p < .001). Participants who entered SURI with a BMI <25 lost 1.7 ± 1.9 kg (2.7 ± 3.0% weight reduction), whereas those who were overweight lost 3.0 ± 2.9 kg (3.9 ± 3.7% weight reduction) and those who were obese lost 4.5 ± 4.1 kg (4.5 ± 3.9% weight reduction). Age was not significantly related to weight loss in SURI and there were no differences between younger (18–35 years of age), middle (36–50 years) or older adults (>50 years). Men lost more weight than women (4.0 vs. 3.1 kg, p <.001), but the changes in BMI were similar for men and women (1.3 ± 1.3 vs. 1.1 ± 1.2, p = .06). Team captains were more likely to complete the program than team members (75.8% vs. 69.5%; p<.001) and those who self-paid were more likely to complete than those whose company paid (72% vs. 69.1%, p=.03). However, among completers, there were no differences in weight loss for captains compared to team members or for self-paid compared to company paid.
Of particular interest was the strong dose-response association between weight loss and both minutes of activity and average steps per day (Table 3). Those who lost >10% of their body weight reported over 10,000 steps per day (mean=11261) and about 48 minutes of physical activity per day.
Table 3.
Physical activity levels (mean ± SD) in Shape Up Rhode Island Completers
| Weight Loss (% of initial weight)
| ||||||
|---|---|---|---|---|---|---|
| Lost ≥ 10% | Lost 5–9.9% | Lost 0 – 5% | Gained | P | ||
| Minutes of Physical Activity/week* | N | 208 | 791 | 2108 | 204 | <.001 |
| Mean | 339 | 281 | 230 | 210 | ||
| SD | 244 | 221 | 192 | 176 | ||
|
| ||||||
| Pedometer Steps/day* | N | 187 | 723 | 1950 | 185 | <.001 |
| Mean | 11261 | 9833 | 8869 | 8271 | ||
| SD | 4661 | 4347 | 3803 | 4054 | ||
Significant differences between all groups except Lost<5% and Gained.
Six month Follow-Up
A single e-mail was sent to all SURI participants at six month follow-up. A total of 1065 participants responded to this e-mail and reported their weight; those who reported weight gains or losses of >50 pounds over the six months (n=24) were considered to have made data entry errors and were dropped from the analysis leaving 1041 respondents. At follow-up, participants reported that they were still 2.4 ± 4.8 kg below the weight they had been at the start of the SURI program (Table 4); those who had completed the program (N=921), reported that they had lost 3.3 ± 3.4 kg during SURI and had regained only 0.8 kg on average over the six months, i.e. they had maintained 76% of their initial weight loss.
Table 4.
Overall Weight Loss (Baseline to 6-month follow-up) in Shape Up Rhode Island Participants
| All (n = 1,041) | Overweight and Obese (Baseline BMI > 25) (n = 767) | |
|---|---|---|
| Weight Loss (kg) | −2.4 ± 4.8 | −2.9 ± 5.3 |
| Weight Loss (% of initial weight loss) | −2.8 ± 5.6 | −3.3 ± 5.9 |
| BMI Change | −0.9 ± 1.7 | −1.1 ± 1.9 |
Discussion
State-wide weight loss programs are increasing in popularity. For example, Shape-Up Rhode Island grew from 1738 participants in 2006, to 6815 participants in 2007. Of note is the fact that this entire program was developed and implemented by two medical students (Kumar and Weinberg) and will be financially self-sustaining by the year 2009. Other states are offering similar programs, but to date, there have been no data published on the outcomes of these interventions.
We found that 75% of Shape Up Rhode Island’s 6815 participants chose to enter the weight loss component of this program, and 70% of these individuals completed at least 12 of the 16 weeks. Those who completed the program lost an average of 3.2 kg and maintained a weight loss of 2.4 kg at six months (i.e. 76% of their initial weight loss). Among individuals who entered the program with a BMI >25 (i.e. overweight or obese), and thus were really in need of weight loss (rather than weight maintenance), self-reported weight loss averaged 3.7 kg, with 34.5% achieving a clinically significant weight loss of >5% of their initial body weight and overall weight losses (baseline to six months) averaging 2.9 kg. The objective weights suggested somewhat smaller weight loss, averaging 2.3 kg, with 25% achieving a weight loss of ≥ 5%.
Data from this study suggest that weight losses in programs such as this are modest compared to clinical programs, but given their large enrollment, may have an important public health impact. SURI was effective in producing an average decrease of −1.2 BMI units by self-report or −0.8 BMI units by objective weighing. The program was able to decrease the proportion of the population that was obese from 39% at baseline to 31% at study end. The weight losses achieved in this study would be expected to have public health benefits. Modest weight losses of 5 to 10% have been shown to reduce the incidence of diabetes by over 50%, 7, 11 with each kilogram of weight loss reducing incident diabetes by 16%, 12 and lowering systolic blood pressure by 1.0 to 2.4 mmHg. 13 Since every one unit change in body mass index reduces medical costs by 2.3%, 14 these results would yield significant savings in health care costs.
The study should be put in the context of other studies on weight loss competitions published in the 1980s. 15–18 Most of these studies were small, but they demonstrated that team competition was more effective than individual competitions both in reducing attrition and improving weight loss outcomes. In the largest of the worksite studies, Stunkard, Cohen and Felix 18 reported on 1177 employees from ten different companies who were more than 10% overweight and took part in a 12 week competition. Weight losses of these participants averaged 6.3 kg for men and 4.4 kg for women. The larger initial weight losses achieved in these early programs compared to Shape-Up RI may result from the written educational material that was provided and/or to increased accountability resulting from the weekly objective weigh-ins. At six month follow-up in three of the companies, participants were 3.2 kg below their baseline weight. Thus, they had maintained 54% of their initial weight loss compared to 76% in the current program. Shape Up Rhode Island thus suggests that such competitions can be effectively implemented via the internet on a much larger scale with similar overall results.
The dose-response relationship between pedometer steps or exercise hours and weight loss highlights the importance of the inclusion of exercise in such interventions. Exercise has been shown to be highly related to weight loss and weight loss maintenance, 19 perhaps reflecting a clustering of behavior changes, with participants who successfully change one aspect of their behavior also changing other behaviors. 20, 21
The strengths of this study include the objective assessment of weight in a subgroup of participants, the fact that 70.2% of participants completed at least 12 weeks of the program, and that six-month weight maintenance was assessed. Limitations include a study population that mainly consisted of overweight females, reflecting traditional participants in weight loss programs and the possible self-selection bias of participants in the objective weighing subgroup and the six month follow-up data. This study also is limited by the lack of a control group that did not receive the Shape-Up intervention and the inability to identify which components of this program contributed to its results. Future studies should evaluate campaigns such as Shape-Up RI using the RE-AIM framework,22–24 which assesses the Reach, Effectiveness, Adoption, Implementation and Maintenance of the program. Using this framework, greater attention would be paid to variables such as the numbers who join the program relative to those offered it and additional measures of effectiveness such as reductions in health care costs.
In conclusion, this study suggests that team-based weight loss competitions are effective at promoting modest weight loss in large numbers of participants. Hopefully this study will serve as a catalyst for other programs to report their results and begin to generate hypotheses about the components needed to increase outreach and efficacy of these interventions. Further studies should examine ways to improve such programs, possibly by including education about diet and physical activity, teaching strategies for behavior change, or providing access to health coaches.
Acknowledgments
Funding/Support: This study was supported by internal funds available to Dr. Wing
Footnotes
Author Contributions: Dr. Wing had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study Concept and Design: Wing, Pinto, Gorin
Collection of Data: Crane, Pinto
Development and Delivery of Program: Kumar created the Shape-Up Rhode Island program, Weinberg developed the software tracking system
Drafting of the Manuscript: Wing
Critical Revision of the Manuscript: Pinto, Kumar, Weinberg, Gorin
Statistical Analysis: Pinto, Crane
Human Participant Protection: Procedures used in this study were reviewed and approved by The Miriam Hospital Institutional Review Board.
Financial Disclosures: Rajiv Kumar is founder and Chairman of Shape Up Rhode Island; Rajiv Kumar and Brad Weinberg are managing partners of Shape Up the Nation.
References
- 1.Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM. Prevalence of overweight and obesity in the United States, 1999–2004. JAMA. 2006;295(13):1549–55. doi: 10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- 2.National Heart, Lung, and Blood Institute. Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults--The Evidence Report. National Institutes of Health. Obes Res. 1998;6 (Suppl 2):51S–209S. [PubMed] [Google Scholar]
- 3.Alley DE, Chang VW. The changing relationship of obesity and disability, 1988–2004. JAMA. 2007;298(17):2020–7. doi: 10.1001/jama.298.17.2020. [DOI] [PubMed] [Google Scholar]
- 4.Flegal KM, Graubard BI, Williamson DF, Gail MH. Excess deaths associated with underweight, overweight, and obesity. JAMA. 2005;293(15):1861–7. doi: 10.1001/jama.293.15.1861. [DOI] [PubMed] [Google Scholar]
- 5.Finkelstein EA, Fiebelkorn IC, Wang G. State-level estimates of annual medical expenditures attributable to obesity. Obes Res. 2004;12(1):18–24. doi: 10.1038/oby.2004.4. [DOI] [PubMed] [Google Scholar]
- 6.Wing RR. Behavioral approaches to the treatment of obesity. In: Bray G, Bouchard C, editors. Handbook of Obesity: Clinical Applications. 2. New York: Marcel Dekker, Inc; 2004. [Google Scholar]
- 7.Diabetes Prevention Program Research Group. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346(6):393–403. doi: 10.1056/NEJMoa012512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Look AHEAD Research Group. Reduction in weight and cardiovascular disease risk factors in individuals with type 2 diabetes: one-year results of the Look AHEAD trial. Diabetes Care. 2007;30(6):1374–83. doi: 10.2337/dc07-0048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Heshka S, Anderson JW, Atkinson RL, et al. Weight loss with self-help compared with a structured commercial program: A randomized trial. JAMA. 2003;289(14):1792–8. doi: 10.1001/jama.289.14.1792. [DOI] [PubMed] [Google Scholar]
- 10.Womble LG, Wadden T, McGuckin BG, Sargent SL, Rothman RA, Krauthamer-Ewing ES. A randomized controlled trial of commercial Internet weight loss programs. Obes Res. 2004;12:1011–1018. doi: 10.1038/oby.2004.124. [DOI] [PubMed] [Google Scholar]
- 11.Tuomilehto J, Lindstrom J, Eriksson J, et al. Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N Engl J Med. 2001;344:1343–1350. doi: 10.1056/NEJM200105033441801. [DOI] [PubMed] [Google Scholar]
- 12.Hamman RF, Wing RR, Edelstein SL, et al. Effect of weight loss with lifestyle intervention on risk of diabetes. Diabetes care. 2006;29(9):2102–7. doi: 10.2337/dc06-0560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Neter JE, Stam BE, Kok FJ, Grobbee DE, Geleijnse JM. Influence of weight reduction on blood pressure: a meta-analysis of randomized controlled trials. Hypertension. 2003;42(5):878–84. doi: 10.1161/01.HYP.0000094221.86888.AE. [DOI] [PubMed] [Google Scholar]
- 14.Wang F, McDonald T, Bender J, Reffitt B, Miller A, Edington DW. Association of healthcare costs with per unit body mass index increase. J Occup Environ Med. 2006;48(7):668–74. doi: 10.1097/01.jom.0000225045.77734.f4. [DOI] [PubMed] [Google Scholar]
- 15.Wing RR, Epstein LH. A community approach to weight control: The American Cancer Society Weight-A-Thon. Prev Med. 1982;11:245–250. doi: 10.1016/0091-7435(82)90023-8. [DOI] [PubMed] [Google Scholar]
- 16.Cohen RY, Stunkard AJ, Felix MRJ. Comparison of three worksite weight-loss competitions. J Behav Med. 1987;10(5):467–479. doi: 10.1007/BF00846145. [DOI] [PubMed] [Google Scholar]
- 17.Brownell KD, Cohen RY, Stunkard AJ, Felix MRJ, Cooley NB. Weight loss competitions at the work site: Impact on weight, morale and cost-effectiveness. Am J Publ Health. 1984;74:1283–1285. doi: 10.2105/ajph.74.11.1283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Stunkard AJ, Cohen RY, Felix MR. Weight loss competitions at the worksite: how they work and how well. Prev Med. 1989;18:460–474. doi: 10.1016/0091-7435(89)90006-6. [DOI] [PubMed] [Google Scholar]
- 19.Pronk NP, Wing RR. Physical activity and long-term maintenance of weight loss. Obes Res. 1994;2(6):587–599. doi: 10.1002/j.1550-8528.1994.tb00110.x. [DOI] [PubMed] [Google Scholar]
- 20.Wing RR, Hamman RF, Bray GA, et al. Achieving weight and activity goals among diabetes prevention program lifestyle participants. Obes Res. 2004;12(9):1426–34. doi: 10.1038/oby.2004.179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jakicic J, Wing RR, Winters-Hart C. Relationship of physical activity to eating behaviors and weight loss in women. Med Sci Sports Exerc. 2002;34(10):1653–1659. doi: 10.1097/00005768-200210000-00018. [DOI] [PubMed] [Google Scholar]
- 22.Glasgow RE, Klesges LM, Dzewaltowski DA, Bull SS, Estabrooks P. The future of health behavior change research: What is needed to improve translation of research into health promotion practice? Ann Behav Med. 2004;27:3–12. doi: 10.1207/s15324796abm2701_2. [DOI] [PubMed] [Google Scholar]
- 23.Glasgow RE. Translating Research to Practice: Lessons Learned, Areas for Improvement, and Future Directions. Diabetes Care. 2003;26:2451–2456. doi: 10.2337/diacare.26.8.2451. [DOI] [PubMed] [Google Scholar]
- 24.Farris RP, Will JC, Khavjou O, Finkelstein EA. Beyond effectiveness: Evaluating the public health impact of the WISEWOMAN Program. Am J Publ Health. 2007;97:641–647. doi: 10.2105/AJPH.2005.072264. [DOI] [PMC free article] [PubMed] [Google Scholar]