Abstract
Objectives To provide an integrative review of the existing literature on the interrelationships among sleep, culture, and medical conditions in children. Methods A comprehensive literature search was conducted using PubMed, Medline, and PsychINFO computerized databases and bibliographies of relevant articles. Results Children with chronic illnesses experience more sleep problems than healthy children. Cultural beliefs and practices are likely to impact the sleep of children with chronic illnesses. Few studies have examined cultural factors affecting the relationship between sleep and illness, but existing evidence suggests the relationship between sleep and illness is exacerbated for diverse groups. Conclusions Sleep is of critical importance to children with chronic illnesses. Cultural factors can predispose children both to sleep problems and to certain medical conditions. Additional research is needed to address the limitations of the existing literature, and to develop culturally sensitive interventions to treat sleep problems in children with chronic illnesses.
Keywords: children, chronic illness, culture, ethnicity, sleep
Sleep-related behaviors are shaped not only by biological and developmental factors, but also by sociocultural context, including cultural values, cultural norms, and parenting practices (Jenni & O’Connor, 2005). Despite cultural differences in how, where, and when children sleep, sleep problems are common in children, and are present in 25–40% of the general population (Owens, 2005). A large body of research has linked sleep problems with a host of negative consequences, including difficulties with academic performance, cognitive skills, memory, and learning (Sadeh, Gruber, & Raviv, 2002). Moreover, sleep problems in children have been associated with both internalizing (Johnson, Chilcoat, & Breslau, 2000) and externalizing problems (Aronen, Paavonen, Fjallberg, Soininen, & Torronen, 2000).
Emerging evidence also suggests that sleep has unique importance for health. For example, sleep deprivation alters immune function in healthy adults (Ozturk et al., 1999) and delays wound healing in animal models (Gumustekin et al., 2004). Behavioral changes associated with sleep deprivation can amplify the pain response and affect adherence to medical regimens. Conversely, adequate sleep may facilitate recovery from illness or injury through secretion of melatonin, which increases the immune response, and growth hormone, which promotes healing (Yarrington & Mehta, 1998).
Sleep is particularly important for pediatric populations, because both chronic and acute medical conditions increase the risk of sleep disruption. Illness may affect children’s sleep through various pathways. Brain structures responsible for sleep are located in the hypothalamus, brainstem, and basal forebrain, all of which can be affected by insults to the brain, such as brain tumors, epilepsy, stroke, or by treatments such as chemotherapy or radiation therapy (Rosen, Shor, & Geller, 2008). Some illnesses (e.g., asthma and epilepsy) may have worsening symptoms at night, and others (e.g., diabetes) may require nighttime medication. Furthermore, pain, hospitalization, and side-effects of medications may all interfere with sleep (Valrie, Gil, Redding-Lallinger, & Daeschner, 2007). Unique features of the hospital environment, such as noise, light, and nocturnal disruptions related to nursing care, can disrupt sleep routines.
Not surprisingly, children with chronic illnesses have elevated rates of sleep problems, and in particular, achieve less parent-reported daytime and nighttime sleep than healthy children (Mindell, Spirito, & Carskadon, 1990). In a recent population-based study, children with chronic illnesses reported more difficulty initiating and maintaining sleep than their healthy peers; however, this finding was reduced to nonsignificance after controlling for emotional and behavioral problems (Hysing, Sivertsen, Stormark, Elgen, & Lundervold, 2009).
Pediatric studies have sought to identify factors that may influence variations in sleep, including racial and ethnic differences (Villaneuva, Buchanan, Yee, & Grunstein, 2005), sociocontextual factors such as socioeconomic status (Spilsbury et al., 2006), individual factors such as psychological functioning (Ivanenko, Crabtree, Obrien, & Gozal, 2006), and medical factors such as pain (Valrie et al., 2007). The influence of cultural factors on sleep in pediatric populations has been understudied. Specific groups may face experiences (e.g., acculturative stress, discrimination, lack of knowledge of specific illness regimens and the importance of sleep, and/or difficulty navigating health care systems) that may affect both the quality of children’s health and sleep outcomes. Cultural beliefs about health and sleep may affect how illness is managed, and in turn may affect sleep behaviors. Understanding how culture can affect sleep patterns and behaviors is a topic of clinical importance, as it provides not only a context to understand additional influences on children’s sleep behaviors, but it also offers providers an opportunity to make meaningful connections with families around how to best intervene to enhance the quality of sleep in children with specific health needs.
The terms “culture” or “cultural factors”, “race,” and “ethnicity” are often used interchangeably in pediatric studies, when each of these terms has distinct meanings. Betancourt and Lopez (1993) have argued that “researchers who study cultural differences frequently fail to identify the specific aspects of culture that are thought to influence behavior. Consequently, we learn that cultural group, race, or ethnicity may be related to a given psychological phenomenon, but we learn little about the specific elements of these group variables that contribute to the proposed relationship” (p. 629). To clarify the distinction between these terms, Betancourt and Lopez (p. 630) refer to Rohner’s (1984) definition of cultures as “highly variable systems of meanings”, which are “learned” and “shared by a people or an identifiable segment of a population,” and represent “designs and ways of life transmitted from one generation to another.” Race, on the other hand, typically refers to groupings of individuals by physical characteristics, such as skin color (Betancourt & López, 1993, p. 631). Ethnicity is used in reference to groupings of individuals by a common nationality, culture, or language. These researchers recommend that as a general approach, it is important to measure directly the variable of interest that may influence behavior, as opposed to simply examining group differences by ethnicity or race. The former approach provides further depth about which cultural element (e.g., social norms, roles, beliefs, and values) may be important to a specific group, and may drive certain behaviors. Increased specification with regard to cultural variables of interest could improve understanding of the cultural variables responsible for the differences observed between specific races or ethnic groups (Sue, 1988; Sue & Zane, 1987; Zuckerman, 1990).
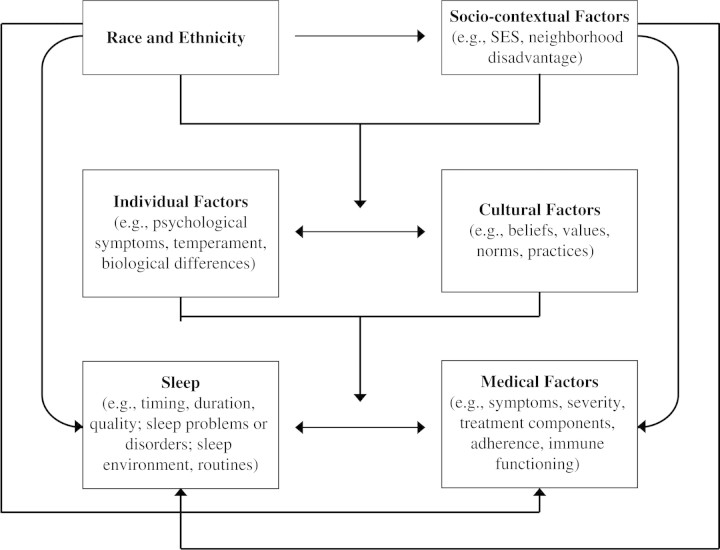
To further understand culture’s impact on sleep in pediatric populations, we propose a multi-level conceptual model whereby race and ethnicity, sociocontextual factors, individual factors, and cultural factors are interrelated, and exert influence on both sleep and medical conditions (Fig. 1). The specific pathways by which these processes may influence sleep and medical conditions will be discussed in more detail below in the context of the current literature. To summarize, it is proposed that race/ethnicity may affect sociocontextual, individual, and cultural factors, and these factors in combination, or on their own, can impact sleep and medical-related factors. Furthermore, we propose that specific cultural factors (such as cultural beliefs, values, practices) should be distinguished from group descriptors commonly used to measure culture, such as race and ethnicity.
Figure 1.
Conceptual model of the relationships among cultural and culture-related factors, sleep, and medical factors
Purpose of this Review
The purpose of this review is to critically examine the role of culture and cultural factors in the sleep of children with medical conditions. We sought to identify and understand how cultural processes, such as cultural beliefs, experiences, and other cultural elements mentioned above, may be meaningful to children with chronic disease and may affect sleep-related behaviors. We also sought to examine potential factors relevant to diverse groups (e.g., ethnic minority status, racial background, and socioeconomic status) that are more commonly studied, in the hope of providing suggestions on how to incorporate specific cultural considerations in future research. Though it is beyond the scope of this article to provide a detailed review of sleep and culture in healthy children (Jenni & O'Connor, 2005), or to provide a detailed review of sleep in children with chronic illnesses (Bandla & Splaingard, 2004), we borrow from the literature on healthy children, sleep, and culture, in order to discuss clinical implications and propose directions for future inquiry.
Methods
Literature searches were performed using PubMed, Medline, and PsychINFO computerized databases and bibliographies of relevant articles. The following keywords were used: (a) sleep; (b) child or pediatric; (c) culture, ethnicity, race, or minority; and (d) illness, disease, or one of the following illness-specific terms: asthma, atopic dermatitis, cancer, cystic fibrosis, diabetes, eczema, epilepsy, headache, inflammatory bowel disease, juvenile rheumatoid arthritis, migraine, obesity, pain, recurrent abdominal pain, sickle cell disease (SCD), and sudden infant death syndrome (SIDS). In addition, reference sections of relevant articles were reviewed to find additional studies that did not appear in the search engine. The articles included in this review met the following criteria: (a) study was published in English; (b) study was published in a peer-reviewed publication; (c) study was published from 1989 through February 2009; (d) study included a diverse sample or addressed cultural issues. Exclusion criteria included: (a) single subject case reports; and (b) study included no measure or report of sleep.
Results
A total of 238 abstracts were identified and screened. Of these abstracts, most were immediately eliminated due to exclusion criteria, and 83 were selected for further review. After full review, eight studies were identified that examined interrelationships among sleep, culture, and children’s health: three focused on sleep-related differences in pediatric conditions, one focused on napping in pediatric populations, two focused on co-sleeping in pediatric populations, and two focused on the link between sleep disordered breathing and pediatric obesity. More detailed descriptions of these studies will be integrated into the sections below. Because of the dearth of studies specifically examining these interrelationships, we also identified representative articles that focus on relationships between sleep and culture (16 studies), and sleep and children’s health (15 studies), in order to support relevant themes or inform clinical implications and research directions. Due to the small number of studies, as well as the fact that many of the studies reviewed did not include any type of control group, statistical approaches to integrating the data (e.g., meta-analysis) were not undertaken. The following sections address: (a) ethnic and racial differences in sleep in pediatric conditions; (b) sociocontextual (e.g., neighborhood disadvantage, and socioeconomic status) and individual factors (e.g., psychological functioning) affecting sleep in pediatric populations; and (c) cultural practices affecting sleep in pediatric populations.
Racial and Ethnic Differences in Sleep in Pediatric Populations
Sleep Timing and Duration
The timing and duration of children’s sleep varies across racial/ethnic groups (Jenni & O'Connor, 2005), though only one study has examined these differences in pediatric populations. Kieckhefer and colleagues (Kieckhefer, Ward, Tsai, & Lentz, 2008) found napping to be more common among children with asthma than healthy controls. Further, ethnic minority children had later bedtimes and obtained less nighttime sleep than Caucasian children. Future studies are needed to determine whether napping is more common than expected in ethnic minority children with asthma, potentially to compensate for inadequate nighttime sleep, as well as potential nocturnal sleep disruptions due to asthma symptoms.
A study of napping among healthy children found that non-Hispanic white children nap significantly less frequently than African-American children, and have longer bouts of nighttime sleep, though total sleep duration was nearly equivalent (Crosby, LeBourgeois, & Harsh, 2005). Racial variability in napping could be explained by genetic differences in homeostatic sleep mechanisms, cultural differences in the acceptability of napping, demographic variables such as school/day care status, or differences in awareness of children's afternoon sleep propensity.
Sleep duration is likely to be of particular importance for pediatric populations, given its potential influence on healing and immune function (Yarrington & Mehta, 1998). Moreover, short sleep duration has been found to contribute to weight gain in children in cross-sectional and prospective studies (Agras, Hammer, McNicholas, & Kraemer, 2004). Although the mechanism for this link is not entirely clear, one hypothesis is that partial chronic sleep deprivation may cause alterations in the levels of leptin and ghrelin hormones, which govern hunger and satiety (Spiegel, Tasali, Penev, & Van Cauter, 2004). Similarly, recent prospective epidemiological studies in both children and adults suggest a potential causative role of short sleep in the increased risk of diabetes (Knutson & Van Cauter, 2008). A review of laboratory and epidemiological studies (Van Cauter et al., 2007) found that experimental sleep restriction is not only associated with dysregulation of the neuroendocrine control of appetite, but also with alterations in glucose tolerance that are characteristic of type 2 diabetes. While the obesity epidemic has impacted all age groups and ethnicities, ethnic minority children and children with low socioeconomic status (SES) are disproportionately affected (Lutfiyya, Garcia, Dankwa, Young, & Lipsky, 2008). Given the prevalence of both overweight and type 2 diabetes in minority children, more work is needed to identify potential cultural factors (e.g., beliefs about food, diet, and sleep) and sleep practices that may affect racial and/or ethnic variations in how sleep duration and timing may affect sleep outcomes and disease burden in this group.
Several studies have found racial differences in adolescents' sleep duration, with African-American adolescents achieving less sleep than other racial groups (Adam, Snell, & Pendry, 2007; Spilsbury et al., 2004). These differences persist after controlling for SES, napping, and family functioning variables. This has important implications for daytime functioning, given research demonstrating that after controlling for SES, the cognitive functioning of African-American children may be more vulnerable to the effects of sleep disruptions (Buckhalt, El-Sheikh, & Keller, 2007).
Sleep Disruption
One study including non-Hispanic White and African-American children with asthma from middle to upper class backgrounds showed associations among the number of asthma-related awakenings (1–7 times per week), school absences, and poor school performance (Diette, Markson, Skinner, Nguen, & Algatt-Bergstrom, 2000). African-American children with asthma were reported to miss school more frequently than non-Hispanic White children with asthma. While it seems plausible that these absences could be accounted for by night time awakenings due to asthma symptoms, differences in asthma-related awakenings were not reported by racial group. More importantly, factors that may underlie both nighttime awakenings and school absences for specific groups have not been studied.
Sleep Disorders
Racial and ethnic differences have been observed in rates of childhood sleep disorders. For example, periodic limb movements in sleep are more common in non-Hispanic White than African-American children, potentially due to genetic differences in iron metabolism and dopaminergic gene variance (O'Brien, Holbrook, Faye Jones, & Gozal, 2007).
Sleep disordered breathing, including Obstructive Sleep Apnea (OSA), is four times more prevalent among African-American children than non-Hispanic White children (Redline et al., 1999). The increased risk for OSA among African-American children may be partly due to anatomical differences in oropharyngeal structure (Redline et al., 1999). While overweight is strongly linked to OSA in adults, the association between weight and OSA is generally weaker in children (Kohler & van den Heuvel, 2008). However, race may mediate the relationship between weight and OSA. In a study of Caucasian children, obesity was a weak predictor of OSA severity, explaining <5% of the variance (Kohler et al., 2008). In contrast, other studies have found a stronger relationship between body mass index and OSA in African-American (Rudnick, Walsh, Hampton, & Mitchell, 2007) and Asian (Wing et al., 2003) children. Thus, African-American children or Asian children may be more susceptible to the effects of overweight than children from other racial/ethnic backgrounds (Villaneuva et al., 2005).
Several studies (Kaleyias et al., 2008) have indicated higher prevalence rates of sleep disordered breathing in children with SCD, which disproportionately affects ethnic minority children. Sleep-disordered breathing has been linked with increased pain in SCD, potentially via nocturnal hypoxemia increasing the likelihood of vaso-occlusive crises (Kirkham & Datta, 2006). Among children with SCD, daytime pain is related to poor sleep quality, which is, in turn, related to pain the following day (Valrie et al., 2007). Therefore, sleep problems may increase disease burden in this population.
Despite higher rates of OSA, African-American children are less likely to be diagnosed and treated for this disorder. Untreated OSA is associated with a number of potential adverse consequences, including higher rates of neurocognitive problems and emotional or behavioral problems, particularly hyperactivity and inattention (Mitchell & Kelly, 2005). Moreover, sleep disordered breathing has also been associated with alterations in glucose and lipid metabolism in children, independent of body mass index (Kohler & van den Heuvel, 2008). It has been hypothesized that OSA may increase risk of metabolic syndrome in children with obesity, through common inflammatory pathways. As ethnic minority children are already at heightened risk for metabolic syndrome (de Ferranti et al., 2004), identification and treatment of sleep disordered breathing has important implications for addressing health disparities.
In summary, there is support for ethnic and racial differences in the timing and duration of children's sleep, as well as the incidence of particular sleep problems. For example, childhood obesity is linked to inadequate sleep duration and to OSA, and ethnic minority children are at heightened risk for all three conditions. The interaction between obesity and inadequate sleep duration may place ethnic minority children at greater risk for additional adverse health outcomes. While some studies have suggested that the increased risk in certain racial or ethnic groups may be accounted for by biological differences, issues related to cultural and social context also need to be explored as potential underlying mechanisms.
Sociocontextual and Individual Factors Affecting Sleep in Pediatric Populations
There are, of course, unique experiences that diverse populations of children with chronic illnesses face. Given that ethnic minority families are disproportionately present in inner city environments, daily stressors related to lack of financial resources (e.g., parents' work schedules, overall access to good nutrition), parents’ level of stress and psychological functioning, lack of social support, and neighborhood disadvantage and safety, may affect the overall family environment and climate of the household, and subsequent sleep behaviors of the child (e.g., inconsistent sleep routines). Studies have consistently shown independent associations between race (e.g., African-American race), low SES, and sleep problems in healthy ethnic minority children (Buckhalt et al., 2007; McLaughlin Crabtree et al., 2005). Although sociocontextual factors are not traditionally thought of as “cultural factors,” we believe a review of the literature focusing on sleep and social factors is important to highlight, given such stressors may affect diverse families’ sleep behaviors and routines more frequently.
Neighborhood Disadvantage
Neighborhood stressors (e.g., high crime rates, noise, substandard and/or crowded housing conditions, reduced access to community resources, and increased exposure to violence) place children at risk for poor health and development (Koinis Mitchell et al., 2007). Spilsbury and colleagues (2006) found that living in a neighborhood of severe socioeconomic disadvantage was significantly associated with OSA in a group of 8- to 11-year-old children from a community-based cohort (even after controlling for previously established risk factors, including obesity, African-American race, and premature birth). The specific pathways by which aspects of the neighborhood context affect chronic illness management and sleep need to be further studied.
Socioeconomic status
Lower levels of SES consistently have been associated with poorer sleep outcomes among children from various disease groups. For example, in a sample of urban children, sleep-disordered breathing was associated with low SES, African-American race, and poor school performance (Chervin et al., 2003). However, the relationship between sleep-disordered breathing and school performance was diminished after controlling for low SES. The authors hypothesized that low SES may be related to sleep-disordered breathing through a third variable, such as overweight. In support of this hypothesis, another study found that median neighborhood income and short sleep duration were independently associated with increased odds of obesity status in a diverse sample of children 8–11 years of age (Ievers-Landis, Storfer-Isser, Rosen, Johnson, & Redline, 2008). Family income has also emerged as a significant correlate of sleep problems in a sample of children with juvenile idiopathic arthritis, headache, and SCD, suggesting that family resources and related factors are important to consider in future research (Long, Krishnamurthy, & Palermo, 2008).
Although specific mechanisms underlying this association have not been determined, the immediate home and neighborhood environment is affected by family resources and stresses, and also has the potential to interfere with sleep. For example, inner-city children with asthma may face conditions (e.g., low-quality housing, exposure to allergens) that challenge families’ abilities to control symptoms, resulting in an increased risk for nocturnal symptoms, poor disease management, and disrupted sleep. Although such conditions have been found to be associated with higher levels of psychological distress and more frequent symptoms, which can complicate effective management behaviors (Wright et al., 2004), the role of sleep in this context has been understudied. Sociocontextual factors may also influence cultural beliefs that underlie sleep practices (Fig. 1). For example, due to a crowded living area or concerns about neighborhood safety, parents may make a decision to have their children sleep together in one room or with them, which may influence sleep routines and sleep behaviors. Thus, it may be important to disentangle sociocontextual versus cultural factors that influence these sleep routines.
Psychological Functioning
Stressors related to social context, as well as children’s chronic illness, can affect psychological functioning, and in turn, children’s sleep quality. Ethnic minority, poor, and urban children are at greater risk for increased depressive and anxiety symptoms (Alegria, Canino, Stinson, & Grant, 2006). This may be due to a variety of factors related to acculturation, potential discrimination, or increased stress as a result of financial circumstances (Vera et al., 1991). Emotional and behavioral problems are associated with sleep problems in children in both clinical (Ivanenko et al., 2006) and population-based studies (Paavonen et al., 2002). The presence of a chronic illness has also been found to increase risk for emotional and behavioral problems in children (Hysing et al., 2009). Although the direction of this association is unclear, sleep problems may adversely affect daytime behavior; conversely, behavior and emotional problems may affect sleep patterns, such as rumination in children with anxiety or bedtime resistance in children with defiant behavior. Chronic illness may also be an independent risk factor for sleep problems, and result in increased risk for internalizing or externalizing problems. For example, children with asthma are more prone to anxiety and depressive symptoms (McQuaid, Kopel, & Nassau, 2001). While this relationship is complex, the presence of nocturnal asthma symptoms may increase anxiety and affect sleep. Psychiatric symptoms can complicate chronic illness management and subsequent sleep-related behaviors, and these symptoms may be particularly prevalent in specific ethnic minority groups. Therefore, it is important for research assessing sleep and chronic illness in diverse populations to consider how the presence of psychiatric symptoms may be influencing sleep behaviors.
Cultural Practices and Sleep in Pediatric Populations
Co-Sleeping
Cultural differences may affect where, when, and how children sleep. In the United States, pediatricians most commonly recommend that children should fall asleep alone at bedtime, and remain asleep alone throughout the night (Morgan & Johnson, 2001), reflective of a western industrialized societal emphasis on individual autonomy. However, a number of cultural, socioeconomic, and family values may support co-sleeping, and parents may choose to sleep with their children for a variety of reasons, ranging from promotion of bonding to crowded living conditions. For example, co-sleeping is more prevalent among families with lower SES and among mothers who are breastfeeding (McCoy et al., 2004). In cultural groups that place greater value on interdependence, rates of bed sharing are higher. A large national study of infant bed sharing found that African-American and Asian infants were significantly more likely to share a bed with a parent, even after adjusting for sociodemographic and infant characteristics (Willinger, Ko, Hoffman, Kessler, & Corwin, 2003). Another study of preschool children found that after controlling for sociodemographic and environmental characteristics, Hispanic children were more likely to sleep in their parents' room, and African-American children were more likely to sleep in a room with siblings, likely reflecting cultural differences in parental goals for family relationships (Milan, Snow, & Belay, 2007).
In infants, bed sharing may be associated with both a higher risk of SIDS and the risk of accidental suffocation; therefore, the American Academy of Pediatrics (AAP) has recommended a separate, yet proximal, sleep environment for babies (American Academy of Pediatrics, 2005). African-American infants have a higher incidence of SIDS (Pollack & Frohna, 2001) and are more likely to sleep in their parents' bed than infants from other ethnic groups (Shields, Hunsaker, Muldoon, Corey, & Spivack, 2005). Pediatrician recommendations and parental practices regarding co-sleeping may be discordant, particularly among parents with low SES or African-American ethnicity (Morgan & Johnson, 2001). Further, parental decisions about bed sharing are likely influenced by value systems (e.g., emphasis on interdependence vs. autonomy) and sociodemographic variables (e.g., economic circumstances, parental work schedules, etc.).
Although there is scant information about co-sleeping among children with health conditions, evidence suggests that co-sleeping often develops in response to a medical crisis. For example, parents may institute co-sleeping to keep closer watch on a child who has developed seizures, but this pattern may persist after the acute phase of the illness has resolved. Williams and colleagues (Williams et al., 2000) examined the sleeping arrangements of children with epilepsy (n = 179) and diabetes (n = 155). Parents were more likely to initiate co-sleeping after a diagnosis of epilepsy (22%) than diabetes (8%), possibly due to parental anxiety about seizure occurrence. Although it was not a focus of the study, it is noteworthy that among children with epilepsy, 38% of the African-American children in the sample began co-sleeping after diagnosis, while half as many (19%) of the Caucasian children in the sample began co-sleeping after diagnosis.
Co-sleeping may also emerge to help manage symptoms of chronic illness. In a sample of 270 children with atopic dermatitis (Chamlin et al., 2005), 30% of parents reported co-sleeping to help the child manage illness symptoms, and 66% of these parents were bothered by the co-sleeping. Co-sleeping was significantly more prevalent among Asian-American families of a child with atopic dermatitis, although again, the study was not designed specifically to examine ethnic differences. In summary, parents of children with chronic illnesses may engage in co-sleeping to increase monitoring of their child's health, or implement aspects of their child's treatment regimen. To date, little research has examined the manner in which specific cultural factors intersect with parental concerns and sleep behaviors in children with chronic illnesses; however, findings thus far indicate that cultural values and parenting practices may amplify the relationship between co-sleeping and chronic illness (Fig. 1).
Sleep Positioning
Cultural beliefs may also affect attitudes toward sleep positioning. The AAP recommends that infants be placed in the supine position for sleep, based on epidemiological studies documenting a connection between SIDS and sleep in the prone position (Kochanek, Murphy, Anderson, & Scott, 2004). African-American infants are more likely to be placed in the prone position for sleep (Hauck et al., 2002), a factor which likely contributes to the greater incidence of SIDS. A qualitative study of inner-city, primarily African-American caregivers identified a number of barriers to adopting the supine sleep position for infants, including limited or erroneous knowledge of AAP recommendations; concerns that infants may choke if placed on their back; mistrust of healthcare providers (and conversely, reliance on older female family members for child-rearing advice); and concern about the infant's comfort (Colson et al., 2005). Another study of largely low-income, African-American women found that mothers with persistent depressive symptoms were half as likely to use the back sleep position compared to women without depression (Chung, McCollum, Elo, Lee, & Culhane, 2004). In summary, cultural beliefs and values, sociodemographic variables, and individual factors such as depression all influence sleep positioning, which in turn, affects infant and child health.
Conclusion
Sleep problems have a number of negative consequences for all children. However, sleep has unique importance for children with health conditions, given its potential impact on disease course (e.g., healing, immune function) and severity (e.g., pain). Children with chronic illnesses are at increased risk for sleep problems. There are a number of commonalities in the way that sleep can affect children with chronic illnesses, including nocturnal symptoms affecting quality of sleep, as well as nocturnal disruptions due to disease management.
With regard to the conceptual model (Fig. 1), this review revealed more support for some pathways denoted in the model (e.g., race/ethnicity and sleep, SES and sleep, individual factors and sleep) than others (e.g., cultural factors and sleep) in pediatric populations. Existing studies tend to focus on racial and ethnic differences in the prevalence of sleep problems (particularly OSA) in children with health conditions such as obesity. Overall, the literature focusing on specific cultural factors (such as cultural beliefs or values) affecting sleep in children with medical conditions is sparse. Studies have examined racial and ethnic differences in the culturally constructed practice of co-sleeping among children with atopic dermatitis, epilepsy, and diabetes, and in co-sleeping and sleep positioning as risk factors for SIDS. One study used focus groups to identify common cultural beliefs (e.g., concern about choking) and practices (e.g., older female family members as trusted sources of health advice) related to prone sleep placement (Colson et al., 2005). However, most of the studies reviewed were not specifically designed to assess relationships among cultural factors, sleep, and medical conditions.
Children from ethnic minority backgrounds with chronic illnesses may be at greater risk for adverse sleep outcomes due to independent contributions or a potential interaction of factors related to genetic predisposition, disease severity, psychological factors, or social context. Our review of the literature on sleep in healthy children suggests that ethnic and/or racial background, social context, and cultural beliefs and values affect the decisions families make regarding sleep routines and behaviors. In turn, these sleep routines and behaviors may affect management of chronic illness. More research is needed to identify specific cultural factors related to belief systems, values, and experiences that may contribute to sleep and variations in specific health outcomes. In addition, the interaction between specific pathways (e.g., race/ethnicity, SES, cultural factors, and medical-related factors) and their subsequent effect on sleep in children needs to studied in further depth. The ways in which sociocontextual, individual, cultural, and illness-related factors may moderate or mediate the association between race/ethnicity and sleep also warrants further attention.
Implications for Future Research with Pediatric Populations
There is a need to include more diverse samples of children when studying the relationship between sleep and chronic illness. Despite the widespread recognition that certain pediatric conditions disproportionately affect ethnic minority groups, studies examining sleep in children with chronic illnesses tend to include small samples from nonminority backgrounds. Inclusion of more representative samples will enable the field to learn how race and ethnicity may mediate or moderate associations between sleep and illness outcomes.
Moreover, there is a need to move beyond the measurement of ethnicity, race, and SES, and to examine cultural processes related to families’ ethnic and cultural background that may have relevance to both sleep and to chronic illness management (Koinis-Mitchell et al., 2007). Future studies should identify specific elements of culture that may account for variations in sleep outcomes. For example, recent research has indicated that Hispanic caregivers may be more inclined to use alternative approaches to asthma treatment such as home remedies (Koinis-Mitchell et al., 2008). Some of these alternative remedies, and their use in place of traditional asthma medications, may have an impact on sleep quality. There are a number of other culturally constructed sleep practices, such as co-sleeping, that would be relevant to illness management, and merit further investigation. As adherence to specific aspects of medical regimens is often problematic in disadvantaged populations, the relationship between sleep and adherence among children with medical conditions, and disentangling differences due to racial/ethnic background, SES, or cultural factors, could be another productive area of inquiry.
Finally, future studies should include a clear conceptual definition and methodological approach to the assessment of both culture and sleep. While there are similarities among cultural processes that are commonly ascribed to by families within various groups (e.g., a focus on allocentrism in families of Hispanic background) that may affect how families view sleep behaviors and routine, much heterogeneity exists within specific ethnic and racial subgroups. Therefore, measurement strategies that assess specific cultural factors on a continuum may be useful. With regard to assessment of sleep in chronically ill populations, sleep problems were assessed using a single parent-report item in many studies reviewed. The field should move toward validated measures of sleep [e.g., Pediatric Sleep Questionnaire (PSQ), Children’s Sleep Habits Questionnaire (CSHQ)], and when possible, utilize objective measurements such as actigraphy or polysomnography. This may be particularly important with diverse populations, given ethnic differences in the perception and meaning of sleep symptoms.
Implications for Clinical Work
Clinicians treating children with medical conditions should routinely screen for sleep problems and offer sleep hygiene recommendations, given the potential impact of sleep on disease course, symptomatology, and quality of life. It would be prudent to focus increased attention to sleep screening among ethnic minority patients, who may have a greater incidence of sleep problems. Similarly, comorbidities such as depression and anxiety are more prevalent in ethnic minorities (Alegria et al., 2006) and have the potential to affect not only sleep, but also illness management, adherence, and pain.
In many cases, parents do not consult with a doctor about their children's sleeping problems, and may not be aware that health care professionals can help in this area (Rona, Li, Gulliford, & Chinn, 1998). There is some suggestion from research with adults that perception of sleep problems and threshold for reporting sleep concerns may be affected by sociocultural factors, including attitudes toward medicine (Villaneuva et al., 2005) and health literacy (Hackney, Weaver, & Pack, 2008). A recent study found that non-Hispanic white mothers were more likely than African-American and Latina mothers to report their preschooler had sleep difficulties, possibly reflective of cultural expectations for child development (Milan et al., 2007). There may even be ethnic differences in the words parents choose to describe sleep problems (Gottlieb et al., 2003).
Efficacious treatments are available for children’s sleep problems (Ramchandani, Wiggs, Webb, & Stores, 2000). However, only one study to date has examined any treatment for sleep problems among children with chronic health conditions. A behavioral intervention for sleep onset difficulties and nighttime awakenings among 22 children with illnesses (primarily asthma and chronic ear infections) and 39 children with disabilities (primarily developmental disabilities or autism) resulted in significant improvements in these sleep parameters at 3–6 month follow-up (Bartlet & Beaumont, 1998). Of note, the authors found that treatment of sleep problems in this population typically was more complex than treatment of sleep problems in healthy children, as maternal depression, family issues, and medical issues often required attention before behavioral interventions could be initiated. Clearly, more research is needed to develop and test behavioral interventions for sleep problems in youth with chronic health conditions, particularly given the unique importance of sleep for this group. Consideration should be given to tailoring the format, content, and treatment goals of such interventions to address cultural issues, attitudes, and practices regarding sleep. For example, techniques such as extinction that involve ignoring a child at bedtime may be seen as overly harsh by cultural groups who value interdependence. Graduated extinction with parental presence may be more congruent with cultural values, and this could enhance acceptability and implementation of the treatment plan.
In summary, children with chronic illnesses should be routinely screened for sleep problems, particularly in those at high risk by virtue of cultural factors. Healthcare providers need to be cognizant of cultural factors and health literacy levels when eliciting information about sleep problems in children at increased risk.
Conflicts of interest: None declared.
References
- Adam EK, Snell EK, Pendry P. Sleep timing and quantity in ecological and family context: A nationally representative time-diary study. Journal of Family Psychology. 2007;21(1):4–19. doi: 10.1037/0893-3200.21.1.4. [DOI] [PubMed] [Google Scholar]
- Agras WS, Hammer LD, McNicholas F, Kraemer HC. Risk factors for childhood overweight: A prospective study from birth to 9.5 years. Journal of Pediatrics. 2004;145(1):20–25. doi: 10.1016/j.jpeds.2004.03.023. [DOI] [PubMed] [Google Scholar]
- Alegria M, Canino G, Stinson FS, Grant BF. Nativity and DSM-IV psychiatric disorders among Puerto Ricans, Cuban Americans, and non-Latino Whites in the United States: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Journal of Clinical Psychiatry. 2006;67(1):56–65. doi: 10.4088/jcp.v67n0109. [DOI] [PubMed] [Google Scholar]
- American Academy of Pediatrics. The changing concept of sudden infant death syndrome: Diagnostic coding shifts, controversies regarding the sleeping environment, and new variables to consider in reducing risk. Pediatrics. 2005;116(5):1245–1255. doi: 10.1542/peds.2005-1499. [DOI] [PubMed] [Google Scholar]
- Aronen ET, Paavonen EJ, Fjallberg M, Soininen M, Torronen J. Sleep and psychiatric symptoms in school-age children. Journal of the American Academy of Child and Adolescent Psychiatry. 2000;39(4):502–508. doi: 10.1097/00004583-200004000-00020. [DOI] [PubMed] [Google Scholar]
- Bandla H, Splaingard M. Sleep problems in children with common medical disorders. Pediatric Clinics of North America. 2004;51(1):203–227. doi: 10.1016/s0031-3955(03)00185-8. viii. [DOI] [PubMed] [Google Scholar]
- Bartlet L, Beaumont J. Treating the sleep disorders of children with disabilities and illness: A one-year project. Clinical Child Psychology and Psychiatry. 1998;3(4):591–612. [Google Scholar]
- Betancourt H, López SR. The study of culture, ethnicity, and race in American psychology. American Psychologist. 1993;48(6):629–637. [Google Scholar]
- Buckhalt JA, El-Sheikh M, Keller P. Children's sleep and cognitive functioning: Race and socioeconomic status as moderators of effects. Child Development. 2007;78(1):213–231. doi: 10.1111/j.1467-8624.2007.00993.x. [DOI] [PubMed] [Google Scholar]
- Chamlin SL, Mattson CL, Frieden IJ, Williams ML, Mancini AJ, Cella D, Chren MM. The price of pruritus: Sleep disturbance and cosleeping in atopic dermatitis. Archives of Pediatrics and Adolescent Medicine. 2005;159(8):745–750. doi: 10.1001/archpedi.159.8.745. [DOI] [PubMed] [Google Scholar]
- Chervin RD, Clarke DF, Huffman JL, Szymanski E, Ruzicka DL, Miller V, Giordani BJ. School performance, race, and other correlates of sleep-disordered breathing in children. Sleep Medicine. 2003;4(1):21–27. doi: 10.1016/s1389-9457(02)00243-5. [DOI] [PubMed] [Google Scholar]
- Chung EK, McCollum KF, Elo IT, Lee HJ, Culhane JF. Maternal depressive symptoms and infant health practices among low-income women. Pediatrics. 2004;113(6):e523–e529. doi: 10.1542/peds.113.6.e523. [DOI] [PubMed] [Google Scholar]
- Colson ER, McCabe LK, Fox K, Levenson S, Colton T, Lister G, Corwin MJ. Barriers to following the back-to-sleep recommendations: Insights from focus groups with inner-city caregivers. Ambulatory Pediatrics. 2005;5(6):349–354. doi: 10.1367/A04-220R1.1. [DOI] [PubMed] [Google Scholar]
- Crosby B, LeBourgeois MK, Harsh J. Racial differences in reported napping and nocturnal sleep in 2- to 8-year-old children. Pediatrics. 2005;115(1 Suppl):225–232. doi: 10.1542/peds.2004-0815D. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Ferranti SD, Gauvreau K, Ludwig DS, Neufeld EJ, Newburger JW, Rifai N. Prevalence of the metabolic syndrome in American adolescents: Findings from the Third National Health and Nutrition Examination Survey. Circulation. 2004;110(16):2494–2497. doi: 10.1161/01.CIR.0000145117.40114.C7. [DOI] [PubMed] [Google Scholar]
- Diette GB, Markson L, Skinner EA, Nguen TT, Algatt-Bergstrom P. Nocturnal asthma in children affects school attendance, school performance and parents' work attendance. Archives of Pediatric Adolescent Medicine. 2000;154:923–928. doi: 10.1001/archpedi.154.9.923. [DOI] [PubMed] [Google Scholar]
- Gottlieb DJ, Vezina RM, Chase C, Lesko SM, Heeren TC, Weese-Mayer DE, Corwin MJ. Symptoms of sleep-disordered breathing in 5-year-old children are associated with sleepiness and problem behaviors. Pediatrics. 2003;112(4):870–877. doi: 10.1542/peds.112.4.870. [DOI] [PubMed] [Google Scholar]
- Gumustekin K, Seven B, Karabulut N, Aktas O, Gursan N, Aslan S, Dane S. Effects of sleep deprivation, nicotine, and selenium on wound healing in rats. International Journal of Neuroscience. 2004;114(11):1433–1442. doi: 10.1080/00207450490509168. [DOI] [PubMed] [Google Scholar]
- Hackney JE, Weaver TE, Pack AI. Health literacy and sleep disorders: A review. Sleep Medicine Reviews. 2008;12(2):143–151. doi: 10.1016/j.smrv.2007.07.002. [DOI] [PubMed] [Google Scholar]
- Hauck FR, Moore CM, Herman SM, Donovan M, Kalelkar M, Christoffel KK, Rowley D. The contribution of prone sleeping position to the racial disparity in sudden infant death syndrome: The Chicago Infant Mortality Study. Pediatrics. 2002;110(4):772–780. doi: 10.1542/peds.110.4.772. [DOI] [PubMed] [Google Scholar]
- Hysing M, Sivertsen B, Stormark KM, Elgen I, Lundervold AJ. Sleep in children with chronic illness, and the relation to emotional and behavioral problems—a population-based study. Journal of Pediatric Psychology. 2009;34(6):665–670. doi: 10.1093/jpepsy/jsn095. [DOI] [PubMed] [Google Scholar]
- Ievers-Landis CE, Storfer-Isser A, Rosen C, Johnson NL, Redline S. Relationship of sleep parameters, child psychological functioning, and parenting stress to obesity status among preadolescent children. Journal of Developmental and Behavioral Pediatrics. 2008;29(4):243–252. doi: 10.1097/DBP.0b013e31816d923d. [DOI] [PubMed] [Google Scholar]
- Ivanenko A, Crabtree VM, Obrien LM, Gozal D. Sleep complaints and psychiatric symptoms in children evaluated at a pediatric mental health clinic. Journal of Clinical Sleep Medicine. 2006;2(1):42–48. [PubMed] [Google Scholar]
- Jenni OG, O'Connor BB. Children's sleep: An interplay between culture and biology. Pediatrics. 2005;115(1 Suppl):204–216. doi: 10.1542/peds.2004-0815B. [DOI] [PubMed] [Google Scholar]
- Johnson EO, Chilcoat HD, Breslau N. Trouble sleeping and anxiety/depression in childhood. Psychiatry Research. 2000;94(2):93–102. doi: 10.1016/s0165-1781(00)00145-1. [DOI] [PubMed] [Google Scholar]
- Kaleyias J, Mostofi N, Grant M, Coleman C, Luck L, Dampier C, Kothare SV. Severity of obstructive sleep apnea in children with sickle cell disease. Journal of Pediatric Hematology and Oncology. 2008;30(9):659–665. doi: 10.1097/MPH.0b013e31817eb7ef. [DOI] [PubMed] [Google Scholar]
- Kieckhefer GM, Ward TM, Tsai SY, Lentz MJ. Nighttime sleep and daytime nap patterns in school age children with and without asthma. Journal of Developmental and Behavioral Pediatrics. 2008;29(5):338–344. doi: 10.1097/DBP.0b013e318182a99e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirkham FJ, Datta AK. Hypoxic adaptation during development: Relation to pattern of neurological presentation and cognitive disability. Developmental Science. 2006;9(4):411–427. doi: 10.1111/j.1467-7687.2006.00507.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knutson KL, Van Cauter E. Associations between sleep loss and increased risk of obesity and diabetes. Annals of the New York Academy of Sciences. 2008;1129:287–304. doi: 10.1196/annals.1417.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kochanek KD, Murphy SL, Anderson RN, Scott C. Deaths: Final data for 2002. National Vital Statistics System. 2004;53(5):1–115. [PubMed] [Google Scholar]
- Kohler MJ, Lushington K, Couper R, Martin J, van den Heuvel C, Pamula Y, Kennedy D. Obesity and risk of sleep related upper airway obstruction in Caucasian children. Journal of Clinical Sleep Medicine. 2008;4(2):129–136. [PMC free article] [PubMed] [Google Scholar]
- Kohler MJ, van den Heuvel CJ. Is there a clear link between overweight/obesity and sleep disordered breathing in children? Sleep Medicine Reviews. 2008;12(5):347–361. doi: 10.1016/j.smrv.2008.04.008. discussion 363–344. [DOI] [PubMed] [Google Scholar]
- Koinis-Mitchell D, McQuaid EL, Seifer R, Kopel SJ, Esteban C, Canino G, Fritz GK. Multiple urban and asthma-related risks and their association with asthma morbidity in children. Journal of Pediatric Psychology. 2007;32(5):582–595. doi: 10.1093/jpepsy/jsl050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koinis-Mitchell D, McQuaid EL, Friedman D, Colon A, Soto J, Rivera DV, Canino G. Latino caregivers' beliefs about asthma: Causes, symptoms, and practices. Journal of Asthma. 2008;45(3):205–210. doi: 10.1080/02770900801890422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Long AC, Krishnamurthy V, Palermo TM. Sleep disturbances in school-age children with chronic pain. Journal of Pediatric Psychology. 2008;33(3):258–268. doi: 10.1093/jpepsy/jsm129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lutfiyya MN, Garcia R, Dankwa CM, Young T, Lipsky MS. Overweight and obese prevalence rates in African American and Hispanic children: An analysis of data from the 2003–2004 National Survey of Children's Health. Journal of the American Board of Family Medicine. 2008;21(3):191–199. doi: 10.3122/jabfm.2008.03.070207. [DOI] [PubMed] [Google Scholar]
- McCoy RC, Hunt CE, Lesko SM, Vezina R, Corwin MJ, Willinger M, Mitchell AA. Frequency of bed sharing and its relationship to breastfeeding. Journal of Developmental and Behavioral Pediatrics. 2004;25(3):141–149. doi: 10.1097/00004703-200406000-00001. [DOI] [PubMed] [Google Scholar]
- McLaughlin Crabtree V, Beal Korhonen J, Montgomery-Downs HE, Faye Jones V, O'Brien LM, Gozal D. Cultural influences on the bedtime behaviors of young children. Sleep Medicine. 2005;6(4):319–324. doi: 10.1016/j.sleep.2005.02.001. [DOI] [PubMed] [Google Scholar]
- McQuaid EL, Kopel SJ, Nassau JH. Behavioral adjustment in children with asthma: A meta-analysis. Journal of Developmental and Behavioral Pediatrics. 2001;22(6):430–439. doi: 10.1097/00004703-200112000-00011. [DOI] [PubMed] [Google Scholar]
- Milan S, Snow S, Belay S. The context of preschool children's sleep: Racial/ethnic differences in sleep locations, routines, and concerns. Journal of Family Psychology. 2007;21(1):20–28. doi: 10.1037/0893-3200.21.1.20. [DOI] [PubMed] [Google Scholar]
- Mindell JA, Spirito A, Carskadon MA. Prevalence of sleep problems in chronically ill children. Sleep Research. 1990;19:337. [Google Scholar]
- Mitchell RB, Kelly J. Child behavior after adenotonsillectomy for obstructive sleep apnea syndrome. Laryngoscope. 2005;115(11):2051–2055. doi: 10.1097/01.MLG.0000181516.65577.94. [DOI] [PubMed] [Google Scholar]
- Morgan SK, Johnson CM. Infant sleep: Resident recommendations and socioeconomic status differences in patient practices. Family Medicine. 2001;33(8):614–620. [PubMed] [Google Scholar]
- O'Brien LM, Holbrook CR, Faye Jones V, Gozal D. Ethnic difference in periodic limb movements in children. Sleep Medicine. 2007;8(3):240–246. doi: 10.1016/j.sleep.2006.08.009. [DOI] [PubMed] [Google Scholar]
- Owens JA. Epidemiology of sleep disorders during childhood. In: Sheldon SH, Ferber R, Kryger MH, editors. Principles and practices of pediatric sleep medicine. Philadelphia: Elsevier Saunders; 2005. pp. 27–33. [Google Scholar]
- Ozturk L, Pelin Z, Karadeniz D, Kaynak H, Cakar L, Gozukirmizi E. Effects of 48 hours sleep deprivation on human immune profile. Sleep Research Online. 1999;2(4):107–111. [PubMed] [Google Scholar]
- Paavonen EJ, Almqvist F, Tamminen T, Moilanen I, Piha J, Rasanen E, Aronen ET. Poor sleep and psychiatric symptoms at school: An epidemiological study. European Journal of Child and Adolescent Psychiatry. 2002;11(1):10–17. doi: 10.1007/s007870200002. [DOI] [PubMed] [Google Scholar]
- Pollack HA, Frohna JG. A competing risk model of sudden infant death syndrome incidence in two US birth cohorts. Journal of Pediatrics. 2001;138(5):661–667. doi: 10.1067/mpd.2001.112248. [DOI] [PubMed] [Google Scholar]
- Ramchandani P, Wiggs L, Webb V, Stores G. A systematic review of treatments for settling problems and night waking in young children. British Medical Journal. 2000;320(7229):209–213. doi: 10.1136/bmj.320.7229.209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Redline S, Tishler PV, Schluchter M, Aylor J, Clark K, Graham G. Risk factors for sleep-disordered breathing in children. Associations with obesity, race, and respiratory problems. American Journal of Respiratory and Critical Care Medicine. 1999;159(5 Pt 1):1527–1532. doi: 10.1164/ajrccm.159.5.9809079. [DOI] [PubMed] [Google Scholar]
- Rohner RP. Toward a conception of culture for cross-cultural psychology. Journal of Cross-Cultural Psychology. 1984;15(2):111–138. [Google Scholar]
- Rona RJ, Li L, Gulliford MC, Chinn S. Disturbed sleep: Effects of sociocultural factors and illness. Archives of Disease in Childhood. 1998;78(1):20–25. doi: 10.1136/adc.78.1.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosen GM, Shor AC, Geller TJ. Sleep in children with cancer. Current Opinion in Pediatrics. 2008;20(6):676–681. doi: 10.1097/mop.0b013e328312c7ad. [DOI] [PubMed] [Google Scholar]
- Rudnick EF, Walsh JS, Hampton MC, Mitchell RB. Prevalence and ethnicity of sleep-disordered breathing and obesity in children. Otolaryngology - Head and Neck Surgery. 2007;137(6):878–882. doi: 10.1016/j.otohns.2007.08.002. [DOI] [PubMed] [Google Scholar]
- Sadeh A, Gruber R, Raviv A. Sleep, neurobehavioral functioning, and behavior problems in school-age children. Child Development. 2002;73(2):405–417. doi: 10.1111/1467-8624.00414. [DOI] [PubMed] [Google Scholar]
- Shields LB, Hunsaker DM, Muldoon S, Corey TS, Spivack BS. Risk factors associated with sudden unexplained infant death: A prospective study of infant care practices in Kentucky. Pediatrics. 2005;116(1):e13–e20. doi: 10.1542/peds.2004-2333. [DOI] [PubMed] [Google Scholar]
- Spiegel K, Tasali E, Penev P, Van Cauter E. Brief communication: Sleep curtailment in healthy young men is associated with decreased leptin levels, elevated ghrelin levels, and increased hunger and appetite. Annals of Internal Medicine. 2004;141(11):846–850. doi: 10.7326/0003-4819-141-11-200412070-00008. [DOI] [PubMed] [Google Scholar]
- Spilsbury JC, Storfer-Isser A, Drotar D, Rosen CL, Kirchner LH, Benham H, Redline S. Sleep behavior in an urban US sample of school-aged children. Archives of Pediatrics and Adolescent Medicine. 2004;158(10):988–994. doi: 10.1001/archpedi.158.10.988. [DOI] [PubMed] [Google Scholar]
- Spilsbury JC, Storfer-Isser A, Kirchner HL, Nelson L, Rosen CL, Drotar D, Redline S. Neighborhood disadvantage as a risk factor for pediatric obstructive sleep apnea. Journal of Pediatrics. 2006;149(3):342–347. doi: 10.1016/j.jpeds.2006.04.061. [DOI] [PubMed] [Google Scholar]
- Sue S. Psychotherapeutic services for ethnic minorities. Two decades of research findings. American Psychologist. 1988;43(4):301–308. doi: 10.1037//0003-066x.43.4.301. [DOI] [PubMed] [Google Scholar]
- Sue S, Zane N. The role of culture and cultural techniques in psychotherapy. A critique and reformulation. American Psychologist. 1987;42(1):37–45. doi: 10.1037//0003-066x.42.1.37. [DOI] [PubMed] [Google Scholar]
- Valrie CR, Gil KM, Redding-Lallinger R, Daeschner C. Brief report: sleep in children with sickle cell disease: An analysis of daily diaries utilizing multilevel models. Journal of Pediatric Psychology. 2007;32(7):857–861. doi: 10.1093/jpepsy/jsm016. [DOI] [PubMed] [Google Scholar]
- Van Cauter E, Holmback U, Knutson K, Leproult R, Miller A, Nedeltcheva A, Spiegel K. Impact of sleep and sleep loss on neuroendocrine and metabolic function. Hormone Research. 2007;67(Suppl 1):2–9. doi: 10.1159/000097543. [DOI] [PubMed] [Google Scholar]
- Vera M, Alegria M, Freeman D, Robles RR, Rios R, Rios CF. Depressive symptoms among Puerto Ricans: Island poor compared with residents of the New York City area. American Journal of Epidemiology. 1991;134(5):502–510. doi: 10.1093/oxfordjournals.aje.a116122. [DOI] [PubMed] [Google Scholar]
- Villaneuva AT, Buchanan PR, Yee BJ, Grunstein RR. Ethnicity and obstructive sleep apnoea. Sleep Medicine Reviews. 2005;9(6):419–436. doi: 10.1016/j.smrv.2005.04.005. [DOI] [PubMed] [Google Scholar]
- Williams J, Lange B, Sharp G, Griebel M, Edgar T, Haley T, Dykman R. Altered sleeping arrangements in pediatric patients with epilepsy. Clinical Pediatrics. 2000;39(11):635–642. doi: 10.1177/000992280003901102. [DOI] [PubMed] [Google Scholar]
- Willinger M, Ko CW, Hoffman HJ, Kessler RC, Corwin MJ. Trends in infant bed sharing in the United States, 1993-2000: The National Infant Sleep Position study. Archives of Pediatrics and Adolescent Medicine. 2003;157(1):43–49. doi: 10.1001/archpedi.157.1.43. [DOI] [PubMed] [Google Scholar]
- Wing YK, Hui SH, Pak WM, Ho CK, Cheung A, Li AM, Fok TF. A controlled study of sleep related disordered breathing in obese children. Archives of Disease in Childhood. 2003;88(12):1043–1047. doi: 10.1136/adc.88.12.1043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright RJ, Mitchell H, Visness CM, Cohen S, Stout J, Evans R, Gold DR. Community violence and asthma morbidity: The Inner-City Asthma Study. American Journal of Public Health. 2004;94(4):625–632. doi: 10.2105/ajph.94.4.625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yarrington A, Mehta P. Does sleep promote recovery after bone marrow transplantation?—A hypothesis. Pediatric Transplantation. 1998;2(1):51–55. [PubMed] [Google Scholar]
- Zuckerman M. Some dubious premises in research and theory on racial differences: Scientific, social, and ethical issues. American Psychologist. 1990;45(12):1297–1303. doi: 10.1037//0003-066x.45.12.1297. [DOI] [PubMed] [Google Scholar]