Abstract
Objective
Compare patient-reported outcomes for health plan members who did or did not return after an initial psychotherapy visit.
Methods
Routinely administered member surveys (n=2666) were used to assess satisfaction with care, patient-rated therapeutic alliance, and patient-rated clinical improvement following an initial psychotherapy visit.
Results
34% of those making an initial therapy visit did not return within 45 days. The distribution of satisfaction, therapeutic alliance, and self-rated improvement scores differed significantly between those who did and did not return (p<.001 for all comparisons). Patients not returning were both more likely to report favorable outcomes (high satisfaction, strong therapeutic alliance, maximum improvement) and more likely to report unfavorable outcomes (low satisfaction, weak alliance, no improvement).
Conclusion
Failure to return after an initial psychotherapy visit can represent either successful and satisfying treatment or unsuccessful and unsatisfying treatment. Systematic outreach and outcome assessment will be necessary to distinguish these two groups of patients.
Up to one third of adults beginning psychotherapy do not return for a second visit (1–3). Early dropout from therapy has been associated with younger age, lower income or educational attainment, less social support, and substance use disorders (4–8).
Surprisingly few data are available regarding outcomes of those who attend only a single psychotherapy visit. We have reported that adults who drop out after a first visit had milder symptoms at time of telephone triage (2), but no data were available regarding treatment outcomes. Among patients continuing treatment, many do experience sustained improvement after a single visit (9–12). However, findings from patients continuing treatment may not apply to those who do not return. We are not aware of any published data regarding outcomes of patients in community practice who discontinue psychotherapy after one visit.
Here we used routinely collected satisfaction survey data from a mixed-model prepaid health system to examine self-reported outcomes in a sample of health plan members who did or did not return after an initial psychotherapy visit.
METHODS
Group Health Cooperative is a not-for-profit, mixed-model prepaid health system serving approximately 650,000 members in Washington and Idaho. Members are demographically similar to the area population and are enrolled through a mixture of employer-sponsored coverage, individual insurance, and publicly-funded programs. Group Health provides specialty mental health care at seven group model mental health clinics (serving members in or near the cities of Bellevue, Bremerton, Olympia, Seattle, Spokane, and Tacoma) and through a network of approximately 300 external fee-for-service providers.
Group Health members may directly request specialty mental health care without referral or authorization. Members requesting mental health services call a centralized screening program and complete a brief structured assessment of primary problem, recent mental health treatment, perceived urgency, screening for substance use disorders, and risk of harm to self or others. In 2008, the most common presenting problems were depression (34%), adjustment/interpersonal problems (19%), anxiety (14%), and attention deficit disorder (7%). Members living in areas served by Group Health clinics are offered appointments with internal therapists and those living in other areas are offered referrals to external providers.
Group Health's Behavioral Health Service routinely mails satisfaction surveys to a random sample of members visiting mental health providers (13). Health plan billing records are used to select a random sample of up to 10 visits each month for each mental health provider (including both internal and external providers). For each visit sampled, the member is mailed a two-page survey concerning satisfaction with care from the individual provider, the facility, and the mental health department. Although only approximately 40% of surveys are completed, our previous research found no significant evidence of response bias (13). In March, 2008, the satisfaction survey was expanded to assess patient-rated therapeutic alliance and patient-rated improvement since starting treatment. Overall satisfaction with treatment was rated on a 0-to-10 scale ranging from “Worst possible mental health care” to “Best possible mental health care”(14). A single item regarding self-rated improvement since starting treatment was rated on a five-point scale ranging from “much worse” to “much improved” (15). Three items were selected from the patient-rated version of Horvath's Working Alliance Inventory (16), a standard measure of therapeutic alliance: one from the Bond subscale (“I feel my therapist appreciates me.”), one from the Goal subscale (“We collaborate on setting goals.”), and one from the Task subscale (“The way we are working with my problem is correct.”). Each was rated on a five-point scale ranging from “Seldom” to “Always”.
We selected all surveys regarding initial psychotherapy visits occurring between March 10, 2008 and September 30, 2010. Survey results were linked to computerized records data regarding prior treatment, diagnosis at the index visit, and return visits to the same provider. Analyses compared survey responses for patients who returned or did not return for a second visits, using chi-square statistics for unadjusted comparisons and logistic regression to adjust for potential confounders.
The Group Health Human Subjects Review Committee approved a waiver of consent for this use of de-identified records data.
RESULTS
The procedures described above identified 2666 member surveys satisfying our inclusion criteria (2030 regarding visits to internal staff therapists and 636 regarding visits to contracted network therapists). These members had a mean age of 48 years (± 15 yrs) and 71% were female. The primary diagnosis at the initial psychotherapy visit was depressive disorder in 56%, anxiety disorder in 26%, substance use disorder in 4%, bipolar disorder in 4%, schizophrenia or other psychotic disorder in 2%, and some other condition in 8%. In 906 (34%) of these episodes, there was no return visit to the same therapist within 45 days of the initial visit.
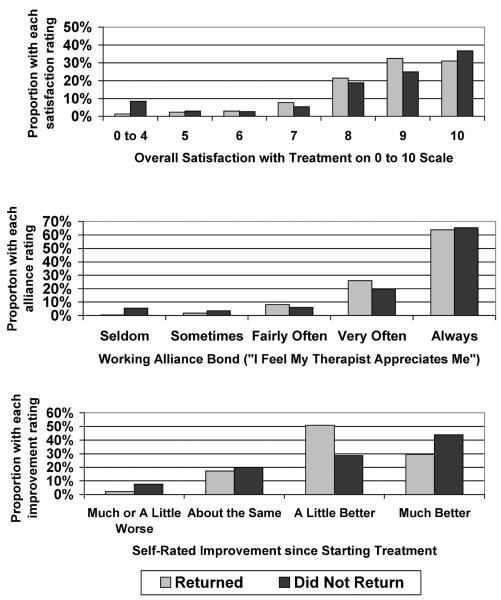
Those returning and not returning had roughly similar mean scores for overall satisfaction (8.67 ± 1.41 vs. 8.28 ± 2.45), Working Alliance Inventory Bond ratings (4.62 ± .70 vs. 4.50 ± .96) and self-rated global improvement (4.07 ± .74 vs. 4.17 ± .91). The distributions of these ratings, however, differed significantly between the two groups. As shown in Figure 1, those not returning were both more likely to report the lowest possible satisfaction ratings (8% vs. <1%) with ratings of 0 through 4) and more likely to report the highest possible ratings (37% vs. 31% with rating of 10) compared to those returning. This difference in distribution far exceeded that expected by chance (X2=98.6, df=6, p<.001). Similarly, those returning and not returning differed significantly in distribution of self-rated improvement (X2=89.5, df=3, p<.001) and Working Alliance Inventory Bond ratings (X2=44.6, df=4, p<.001). As shown in Figure 1, those not returning were more likely to report both the lowest level (8% vs. 2%) and highest level (44% vs. 30%) of self-rated improvement and more likely to report the lowest level of therapeutic alliance (5% vs. <1%). Results for Working Alliance Inventory Goal and Task items showed the identical pattern (see online appendix).
Figure 1.
Comparison of overall satisfaction, patient-rated therapeutic alliance, and patient-rated global improvement for adult health plan members returning and not returning after an initial psychotherapy visit.
Because the associations between various predictors (satisfaction, therapeutic alliance, self-rated improvement) and returning for a second visit might be confounded by other patient characteristics, logistic regression models were used to examine the association between each of these predictors and likelihood of return. Given the non-linear relationships seen in Figure 1, each predictor was represented by a series of indicator variables (e.g. three indicator variables to represent four levels of self-rated improvement). In each of these models, adjustment for potential confounding variables (patient age and sex, primary diagnosis at the index visit, internal vs. external therapist, and duration of enrollment in the health plan) had no meaningful effect on the patterns of association shown in Figure 1 (see online appendix).
DISCUSSION
We find that approximately one third of adult health plan members attending an initial psychotherapy visit did not return for a second visit. Compared to those returning for a second visit, those failing to return were more likely to report care experiences at the positive extreme (high satisfaction, strong therapeutic alliance, large clinical improvement) and at the negative extreme (low satisfaction, poor therapeutic alliance, and clinical worsening). Comparison of mean scores obscured these significant differences in distributions of scores. These differences were not explained by patients' pre-treatment characteristics.
The primary limitations of these findings include the low response rate for mailed satisfaction surveys and the brief assessments of self-rated improvement and therapeutic alliance. Our previous research (13) found that response to satisfaction surveys was associated with female sex, older age, and longer health plan enrollment; but none of these predictors of response led to bias in assessment of provider-level satisfaction ratings. We cannot determine, however, if the associations we examine in this report differed between those who did and did not return satisfaction surveys. The routinely administered survey included only a one-item assessment of self-rated clinical outcome and only three items adapted from the 48-item Working Alliance Inventory. Self-rated improvement may not necessarily agree with clinical assessment, but it is probably more relevant to patients' decisions about continuing treatment.
These findings indicate that dropout after a first therapy visit can sometimes reflect satisfying treatment and a good clinical outcome. As shown in Figure 1, approximately one third of patients not returning for a second visit gave the highest possible satisfaction rating, over 60% gave the highest rating for therapeutic alliance, and over 40% reported that symptoms or problems were much better since starting treatment. Fifteen percent of those not returning gave the highest possible ratings on all three of these measures. While these outcomes may represent spontaneous recovery rather than true treatment effects, outreach to promote engagement in additional therapy would seem unnecessary for this group.
These findings, however, also support the need for routine outcomes monitoring in psychotherapy. Failure to return after a first psychotherapy visit was also associated with the most unfavorable experience of care, and over 25% of those not returning reported that the symptoms or problems that prompted seeking treatment were unimproved or worse. For this group, outreach to promote re-engagement in treatment might help to prevent unfavorable outcomes.
The pattern we observe here is similar to that seen in previous studies of early dropout from antidepressant pharmacotherapy (17). Patients who fail to refill an initial antidepressant prescription included a sizable group with good outcomes and a sizable group with unfavorable outcomes. Successful interventions to improve antidepressant pharmacotherapy were built around systematic outreach to assess outcomes and intensify services according to need (18). Our findings point toward a similar approach to address early dropout from psychotherapy.
Acknowledgments
Supported by NIMH grants P20MH068572 and R01MH081112
Footnotes
The authors have no relevant financial interests to disclose
REFERENCES
- 1.Mohr D, Vella L, Hart S, et al. The effect of telephone-administered psychotherapy on symptoms of depression and attrition: a meta-analysis. Clinical Psychology: Science and Practice. 2008;15:243–253. doi: 10.1111/j.1468-2850.2008.00134.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Simon GE, Ludman EJ. Predictors of early dropout from psychotherapy for depression in community practice. Psychiatric Services. 2010;61:684–689. doi: 10.1176/ps.2010.61.7.684. [DOI] [PubMed] [Google Scholar]
- 3.Hamilton S, Moore AM, Crane R, Payne SH. Psychotherapy Dropouts: Differences by Modality, License, and DSM-IV Diagnosis. Journal of Marital and Family Therapy. 2011;37:333–343. doi: 10.1111/j.1752-0606.2010.00204.x. [DOI] [PubMed] [Google Scholar]
- 4.Centorrino F, Hernan M, Drago-Ferrante G, et al. Factors associated with noncompliance with psychiatric outpatient visits. Psychiatric Services. 2001;52:378–380. doi: 10.1176/appi.ps.52.3.378. [DOI] [PubMed] [Google Scholar]
- 5.Renk K, Dinger T, Bjugstad K. Predicting therapy duration from therapist experience and client psychopathology. Journal of Clinical Psychology. 2000;56:1609–1614. doi: 10.1002/1097-4679(200012)56:12<1609::AID-11>3.0.CO;2-U. [DOI] [PubMed] [Google Scholar]
- 6.Foulks E, Persons J, Merkel R. The effect of patients' beliefs about their illness on compliance in psychotherapy. American Journal of Psychiatry. 1986;143:340–344. doi: 10.1176/ajp.143.3.340. [DOI] [PubMed] [Google Scholar]
- 7.Pekarik G. Relationship of clients' reasons for dropping out of treatment to outcomes and satisfaction. Journal of Clinical Psychology. 1992;48:91–98. doi: 10.1002/1097-4679(199201)48:1<91::aid-jclp2270480113>3.0.co;2-w. [DOI] [PubMed] [Google Scholar]
- 8.Sparr L, Moffitt M, Ward M. Missed psychiatric appointments: who returns and who stays away. American Journal of Psychiatry. 1993;150:801–805. doi: 10.1176/ajp.150.5.801. [DOI] [PubMed] [Google Scholar]
- 9.Baldwin SA, Berkeljon A, Atkins DC. Rates of change in naturalistic psychotherapy: contrasting dose-effect and good-enough level models of change. Jorunal of Consulting and Clinical Psychology. Apr;77:203–211. doi: 10.1037/a0015235. [DOI] [PubMed] [Google Scholar]
- 10.Beckham EE. Improvement after evaluation in psychotherapy of depression: evidence of a placebo effect? Journal of Clinical Psychology. 1989 Nov;45:945–950. doi: 10.1002/1097-4679(198911)45:6<945::aid-jclp2270450620>3.0.co;2-2. [DOI] [PubMed] [Google Scholar]
- 11.Stiles WB, Leach C, Barkham M, et al. Early sudden gains in psychotherapy under routine clinic conditions: practice-based evidence. Journal of Consulting and Clinical Psychology. 2003;71:14–21. [PubMed] [Google Scholar]
- 12.Lutz W, Stulz N, Kock K. Patterns of early change and their relationship to outcome and follow-up among patients with major depressive disorders. Journal of Affective Disorders. 2009;118:60–68. doi: 10.1016/j.jad.2009.01.019. [DOI] [PubMed] [Google Scholar]
- 13.Simon G, Rutter C, Crosier M, et al. Are comparisons of consumer satisfaction with providers biased by nonresponse or case-mix differences? Psychiatric Services. 2009;60:67–73. doi: 10.1176/appi.ps.60.1.67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Agency for Health Care Research and Quality . ECHO Experience of Care and Health Outcomes Survey. US Department of Health and Human Services; Rockville, MD: 2008. [September 14, 2011]; Available from: https://www.cahps.ahrq.gov/content/products/ECHO/PROD_ECHO_Intro.asp. [Google Scholar]
- 15.Guy W. ECDEU Assessment Manual for Psychopharmacology. National Institute of Mental Health; Rockville, MD: 1976. [Google Scholar]
- 16.Horvath AO, Luborsky L. The role of the therapeutic alliance in psychotherapy. Journal of Consulting and Clinical Psychology. 1993;61:561–573. doi: 10.1037//0022-006x.61.4.561. [DOI] [PubMed] [Google Scholar]
- 17.Simon G, Lin E, Katon W, et al. Outcomes of “inadequate” antidepressant treatment in primary care. Journal of General Internal Medicine. 1995;10:663–670. doi: 10.1007/BF02602759. [DOI] [PubMed] [Google Scholar]
- 18.Bower P, Gilbody S, Richards D, et al. Collaborative care for depression in primary care. Making sense of a complex intervention: systematic review and meta-regression. British Journal of Psychiatry. 2006;189:484–493. doi: 10.1192/bjp.bp.106.023655. [DOI] [PubMed] [Google Scholar]