Abstract
Aims
Obesity is associated with the presence of coronary artery disease (CAD) risk factors and cardiovascular events. We examined the relationship between body mass index (BMI) and the presence, extent, severity, and risk of CAD in patients referred for coronary computed tomographic angiography (CCTA).
Methods and results
We evaluated 13 874 patients from a prospective, international, multicentre registry of individuals without known CAD undergoing CCTA. We compared risk factors, CAD findings, and risk of all-cause mortality and non-fatal myocardial infarction (MI) amongst individuals with underweight (18.5–20.0 kg/m2), normal (20.1–24.9 kg/m2), overweight (25–29.9 kg/m2), and obese (≥30 kg/m2) BMI. The mean follow-up was 2.4 ± 1.2 years with 143 deaths and 193 MIs. Among underweight, normal weight, overweight, and obese individuals, there was increasing prevalence of diabetes (7 vs.10% vs. 12 vs. 19%), hypertension (37 vs. 40% vs. 46 vs. 59%), and hyperlipidaemia (48 vs. 52% vs. 56 vs. 56%; P < 0.001 for trend). After multivariable adjustment, BMI was positively associated with the prevalence of any CAD [odds ratio (OR) 1.25 per +5 kg/m2, 95% confidence interval (CI): 1.20–1.30, P < 0.001] and obstructive (≥50% stenosis) CAD (OR: 1.13 per +5 kg/m2, 95% CI: 1.08–1.19, P < 0.001); a higher BMI was also associated with an increased number of segments with plaque (+0.26 segments per +5 kg/m2, 95% CI: 0.22–0.30, P < 0.001). Larger BMI categories were associated with an increase in all-cause mortality (P = 0.004), but no difference in non-fatal MI. After multivariable adjustment, a higher BMI was independently associated with increased risk of MI (hazards ratio: 1.28 per +5 kg/m2, 95% CI: 1.12–1.45, P < 0.001).
Conclusions
Amongst patients with suspected CAD referred for CCTA, individuals with increased BMI have greater prevalence, extent, and severity of CAD that is not fully explained by the presence of traditional risk factors. A higher BMI is independently associated with increased risk of intermediate-term risk of myocardial infarction.
Keywords: Obesity, Coronary artery disease, Myocardial infarction, Body mass index
Introduction
Obesity is an important public health issue, and the prevalence of obesity is rapidly rising, with 32 and 34% of adults in the USA currently defined as overweight and obese, respectively. In prior studies, obesity has been positively associated with coronary artery disease (CAD) risk factors,1 as well as increased rates of incident adverse coronary heart disease events.2–8 While asymptomatic obese individuals are observed to have an increased prevalence of CAD as defined by the coronary artery calcium score,9 the prevalence of obstructive CAD identified by non-invasive CCTA as related to body mass index (BMI) has not been established. To determine the relationship between BMI and the angiographic prevalence, extent, severity, and risk of CAD, we examined individuals within a prospective multicentre international registry of patients undergoing coronary computed tomographic angiography (CCTA) in a cohort of individuals undergoing non-invasive coronary angiography.
Methods
Design overview
The CONFIRM (COronary CT Angiography EvaluatioN For Clinical Outcomes: An InteRnational Multicentre) registry is a dynamic open-label, international, multicentre observational registry designed to prospectively evaluate the associations between patient characteristics, CCTA findings, and adverse events. The rationale and design of this study has been previously reported.10 All sites had the approval of respective institutional review boards, and were compliant with the Health Insurance Portability and Accountability Act where applicable. As per each individual institution's policy, patient consent or a waiver of informed consent was obtained at each site in keeping with site-specific regulations. The study was consistent with the principles of the Declaration of Helsinki.
Setting and participants
We examined a total of 16 291 patients who underwent CCTA at seven centres in six countries (Canada, South Korea, USA, Germany, Switzerland, and Italy) who were enrolled into the registry between February 2003 and December 2009. Inclusion criteria for enrollment in the registry included an age ≥18 years; a CCTA study performed on a scanner with at least 64-detector rows; an interpretable CCTA examination; a normal, overweight, or obese BMI; prospective data collection for CAD risk factors; and enrollment sites with reported BMI and available all-cause mortality and non-fatal myocardial infarction (MI) outcomes. Patients were referred for a variety of indications, including evaluation of symptoms; potential signs of cardiac disease such as abnormal resting or stress electrocardiographic tests; or asymptomatic patients requiring preoperative evaluation, or with peripheral arterial disease, congenital heart disease, cerebrovascular disease, or multiple CAD risk factors.
The present study examined patients stratified by underweight BMI (≤20.0 kg/m2), normal BMI (20.1–24.9 kg/m2), overweight BMI (25–29.9 kg/m2), and obese BMI (≥30 kg/m2). Individuals with prior coronary revascularization or MI, or with missing BMI or CCTA findings were excluded. A total of 13 968 patients met these criteria; 94 individuals were lost to follow-up, resulting in 13 874 patients who were evaluated in this study.
All CCTA performance, data acquisition, image post-processing, and interpretation in the study cohort were consistent with the Society of Cardiovascular Computed Tomography guidelines.11,12 All CCTA studies were performed using a scanner with at least 64 detector rows. Coronary artery calcium score (CACS) was assessed using the Agatston score method as previously described.13 All scans were interpreted by a Level III-equivalent cardiologist or radiologist with the experience of interpreting several thousand CCTA examinations, using uniform data elements with standardized definitions.
In each coronary artery, coronary atherosclerosis was defined as any tissue structures ≥1 mm2 in size within or adjacent to the coronary artery lumen that could be discriminated from surrounding pericardial tissue, epicardial fat, or the vessel lumen itself. The luminal stenosis of coronary atherosclerotic lesions was determined by visual estimation in accordance with guidelines.12 CAD was defined as the presence of any plaque, and was stratified as no CAD (no plaque), mild CAD (maximal stenosis 1–49%), moderate CAD (maximal stenosis 50–69%), and severe CAD (≥70% stenosis). Obstructive CAD was defined as ≥50% luminal diameter stenosis. CAD was also assessed by the segment involvement score and a segment stenosis score, using a 16-segment model as previously described.14 The segment involvement score is a measure of overall plaque distribution, and represents the number of segments with any plaque (range 0–16). The segment stenosis score is a measure of overall coronary artery plaque burden and severity, and grades each segment on scale of 0–3 as having no, mild (1–49% stenosis), moderate (50–69% stenosis), or severe (≥70% stenosis); each segment is added together for a total score of 0–48.14,15
Outcomes and follow-up
The primary endpoints were mortality by any cause and non-fatal MI, which were ascertained by a dedicated physician and/or research nurse. All-cause mortality in the USA was obtained by query of the national death index. All-cause mortality in other countries and non-fatal MI in all countries were obtained by direct patient interview; telephone contact with the patient, the patient's immediate family, or the patient's physician; or by the review of medical records as described.10
Statistical analysis
A post hoc power analysis was performed to determine the robustness of the study sample size to discriminate the differences between groups in the rate of obstructive CAD. Based on the study results, the achieved one-tailed power at an alpha of 0.05 was 99.9% between the normal and overweight BMI cohorts, and 99.9% between the normal and obese BMI cohorts. Additional post hoc power analyses were performed to delineate the adequacy of the sample size to the achieved one-tailed power at an alpha of 0.05 to identify the differences between death and non-fatal MI between BMI groups. The achieved power for all-cause mortality was 0.78 between individuals with a normal and overweight BMI, and 0.95 between individuals with a normal and obese BMI. The achieved power for non-fatal MI was 0.93 for those with normal vs. overweight BMI, and 0.99 for those with normal vs. obese BMI.
Comparisons were performed for a trend in increasing BMI categories defined as underweight BMI, normal BMI, overweight and obese individuals. Categorical variables were compared using χ2 tests for trends across increasing BMI groups. Comparisons between continuous variables with a normal distribution were performed by t-tests and ANOVA with the Tukey post hoc test, while comparisons between continuous variables with non-normal distributions were performed by the Mann–Whitney U test.
To determine the independent relationship between CAD and BMI, backwards stepwise logistic regression models considered variables associated with the presence of any CAD and obstructive CAD; stepwise linear regression models considered variables associated with CAD assessed by the segment involvement score and segment stenosis score. We additionally evaluated this model using standardized coefficients to assess the relative strength of the predictors.
Comparisons of adverse events were performed using log-rank tests and Cox regression analyses to determine the relationship between BMI and adverse events. For all multivariable analyses, considered variables included typical cardiovascular risk factors: age; gender; medical history of hypertension, hyperlipidaemia, and diabetes; current tobacco smoking; and BMI. Only variables with a univariate P < 0.10 were entered into the final model to prevent over-fitting of the models. We additionally examined whether there were significant interaction terms between BMI and other risk factors for prediction of non-fatal MI and prediction of all-cause mortality; no significant interaction terms were observed.
In exploratory analyses, we examined the risk of MI and prevalence of CAD in specific subgroups defined by region (North America, Asia, and Europe) and by ethnicity (Caucasian, Asian). All analyses were performed using SPSS 19.0 (IBM, Somers, NY). Power analyses were performed using PASS 11.0 (NCSS, Kaysville, UT, USA). A P < 0.05 was considered statistically significant. There was no funding support for this study.
Results
The overall mean (SD) age was 56.9 (11.8) years, 55.7% were male, and the mean (SD) follow-up was 2.4 (1.2) years. The 13 874 patients in the study were stratified into those with underweight BMI, normal BMI, overweight BMI, and obese BMI. There was a significant trend in the increase in BMI and increased prevalence of cardiovascular risk factors except smoking (Table 1). Amongst the 12 826 individuals with known symptom status, chest pain was present in 69.2, 65.4, 63.6, and 62.9% of individuals with underweight BMI, normal BMI, overweight BMI, and obese BMI, respectively (P-value for trend = 0.0045).
Table 1.
Patient demographics and medical history by body mass index
| Underweight BMI (n = 341) | Normal BMI (n = 4593) | Overweight BMI (n = 5776) | Obese BMI (n = 3164) | P-value for trend | Tukey comparisons | |
|---|---|---|---|---|---|---|
| Age (years) | 55.6 (13.4) | 57.7 (12.0) | 57.2 (11.4) | 55.3 (11.8)* | <0.0001 | Underweight vs. normal, P = 0.0065; normal vs. obese, P < 0.0001; overweight vs. obese, P < 0.0001 |
| Male gender (%) | 24.6 | 50.1 | 63.0 | 53.7 | <0.0001 | |
| Diabetes (%) | 6.6 | 9.8 | 12.0 | 18.7* | <0.0001 | |
| Hypertension (%) | 37.1 | 39.8 | 46.2 | 58.8* | <0.0001 | |
| Hyperlipidaemia (%) | 48.2 | 52.3 | 55.6 | 55.7* | 0.0002 | |
| Smoking (%) | 22.0 | 16.5 | 16.3 | 16.8 | 0.4500 | |
| BMI (kg/m2) | 19.5 (0.4) | 23.1 (1.3) | 27.1 (1.4) | 34.2 (4.5)* | <0.0001 | All groups significantly different, P < 0.0001 for all |
Values are provided as the mean (standard deviation) or percentage. BMI, body mass index.
*P < 0.01 between the three groups.
BMI and the presence of CAD
There were significant differences in patterns of CAD between groups (Table 2). There was a significant increase in the prevalence of any plaque as well as moderate and severe obstructive CAD for increased BMI categorization. There was no difference in the prevalence of left main obstructive CAD between the BMI groups. There was a significant increase in the prevalence of obstructive CAD in each of the other epicardial coronary arteries; a higher number of obstructive vessels; and increased extent and severity as manifest by the segment involvement and segment stenosis scores.
Table 2.
Coronary artery findings by body mass index
| Underweight BMI (n = 341) | Normal BMI (n = 4593) | Overweight BMI (n = 5776) | Obese BMI (n = 3164) | Test for trend P-value | Tukey comparisons | |
|---|---|---|---|---|---|---|
| Calcium score (n = 12467) | 162.2 (571.8) | 115.1 (345.8) | 137.3 (384.0) | 176.3 (469.0) | <0.0001 | Normal vs. overweight, P = 0.0481; Normal vs. obese, P < 0.0001; Overweight vs. obese, P = 0.0003 |
| CAD stenosis severity (%) | ||||||
| Any plaque | 34.9 | 49.2 | 57.0 | 57.7 | <0.0001 | |
| ≥Moderate (≥50%) | 11.4 | 15.9 | 20.6 | 20.7 | <0.0001 | |
| ≥Severe (≥70%) | 2.9 | 7.7 | 10.2 | 11.2 | <0.0001 | |
| Obstructive CAD by artery (%) | ||||||
| Left main | 0.9 | 1.0 | 1.1 | 1.1 | 0.6029 | |
| Left anterior descending | 5.6 | 12.1 | 15.4 | 15.5 | <0.0001 | |
| Left circumflex | 2.7 | 5.2 | 7.2 | 6.8 | <0.0001 | |
| Right coronary | 5.0 | 6.6 | 8.9 | 9.6 | <0.0001 | |
| Vessels with obstructive CAD (%) | <0.0001 | |||||
| One | 8.9 | 9.9 | 12.4 | 12.4 | ||
| Two | 1.8 | 3.8 | 5.4 | 5.5 | ||
| Three | 0.3 | 2.0 | 2.7 | 2.8 | ||
| CAD severity and extent grades | ||||||
| Segment involvement score | 0 (0–1) | 0 (0–2) | 1 (0–3) | 1 (0–4) | <0.0001 | All groups significantly different, P < 0.03 for all |
| Segment stenosis Score | 0 (0–1) | 0 (0–3) | 1 (0–4) | 1 (0–5) | <0.0001 | All groups significantly different, P < 0.04 for all |
Values are provided as the mean (standard deviation) for calcium score, median (interquartile range) for CAD severity and extent grades or percentage. Obstructive CAD defined as a diameter stenosis ≥50%. BMI, body mass index; CAD, coronary artery disease.
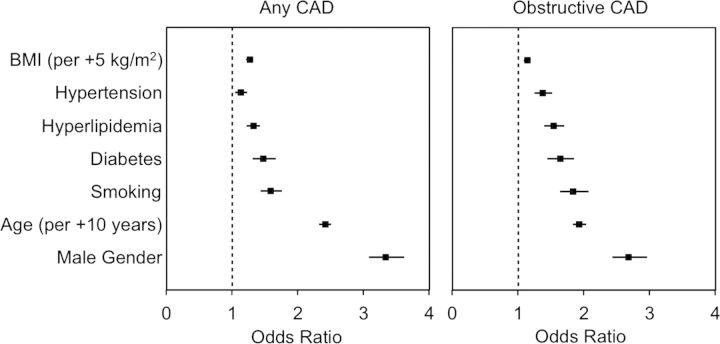
After adjustment for CAD risk factors, an increased BMI was independently associated with an increased probability of any CAD [odds ratio (OR): 1.25 per +5 kg/m2, 95% confidence interval (CI): 1.20–1.30, P < 0.001) and obstructive CAD (OR: 1.13 per +5 kg/m2, 95% CI: 1.08–1.19, P < 0.001) (Figure 1). Further, multivariate analyses also determined that an increased BMI was independently associated with greater segment involvement scores (+0.26 score per +5 kg/m2, 95% CI: 0.22–0.30, P < 0.001) and higher segment stenosis scores (+0.30 score per +5 kg/m2, 95% CI: 0.24–0.37, P < 0.001).
Figure 1.
Variables independently associated with the presence of any CAD and obstructive CAD. These represent the adjusted odds ratios (boxes) and 95% confidence intervals (horizontal lines) for each of the risk factors in the models. An increased BMI (per +5 kg/m2) was independently associated with a greater presence of any CAD (P < 0.001) and obstructive CAD (P < 0.001). Obstructive CAD is defined as the presence of any stenosis ≥50% in diameter. BMI, body mass index; CAD, coronary artery disease.
We additionally examined a model using standardized coefficients to assess the relative strength of each of the predictors. In this model, the adjusted variables most strongly associated with the presence of CAD (from strongest to weakest) were increased age (OR: 2.82, 95% CI: 2.69–2.96, P < 0.001), male gender (OR: 1.81, 95% CI: 1.75–1.90, P < 0.001), increased BMI (OR: 1.24, 95% CI: 1.19–1.29, P < 0.001), current smoking (OR: 1.18, 95% CI: 1.14–1.23, P < 0.001), hyperlipidaemia (OR: 1.15, 95% CI: 1.11–1.20, P < 0.001), diabetes (OR: 1.14, 95% CI: 1.09–1.18, P < 0.001), and hypertension (OR: 1.06, 95% CI: 1.02–1.10, P = 0.004).
BMI and adverse events
There were a total of 143 deaths and 193 non-fatal MIs during an intermediate-term follow-up. Death and non-fatal MI occurred in 10 and 2 patients with underweight BMI, 50 and 44 patients with a normal BMI, 53 and 83 overweight individuals, and 30 and 64 obese patients, respectively. While no significant differences were observed between groups in non-fatal MIs (Figure 2A), normal, overweight, and obese individuals had increased risks of all-cause mortality (Figure 2B). For individuals with a BMI <20.0, 20.0–24.9, 25.0–29.9, 30.0–34.9, and ≥35 kg/m2, the annualized event rate for death was 1.2, 0.4, 0.4, 0.5, 0.4, and 0.4%, respectively; while the annualized event rate for non-fatal MI was 0.3, 0.3, 0.5, 0.7, and 1.2%, respectively.
Figure 2.
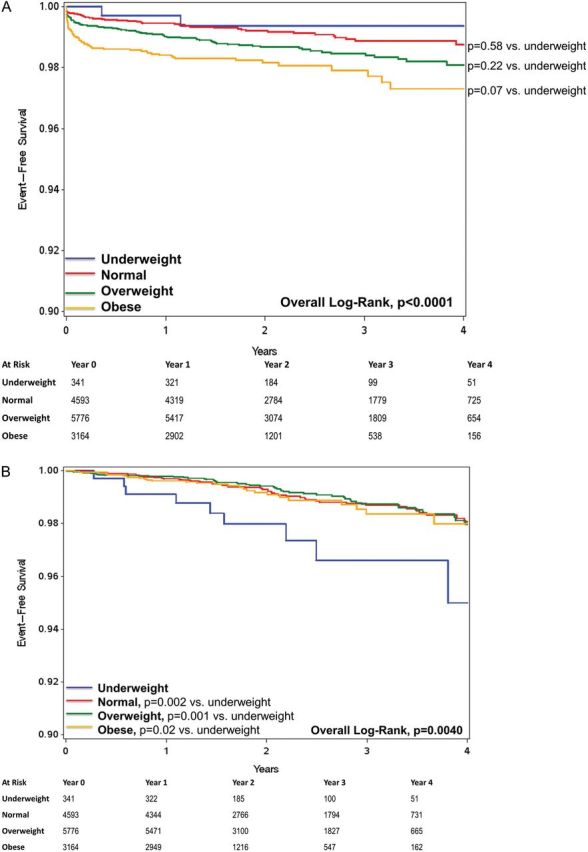
(A) Kaplan–Meier survival plot for non-fatal myocardial infarction and (B) all-cause mortality.
After adjustment for CAD risk factors and BMI, variables independently associated with the risk of non-fatal MI included smoking [hazards ratio (HR): 1.64, 95% CI: 1.15–2.33, P = 0.006), hypertension (HR: 1.42, 95% CI: 1.04–1.94, P = 0.03), age (HR: 1.47 per +10 years, 95% CI: 1.28–1.69, P < 0.001), diabetes (HR: 1.51, 95% CI: 1.06–2.15, P = 0.02), and BMI (HR: 1.28 per +5 kg/m2, 95% CI: 1.12–1.45, P < 0.001); male gender (P = 0.29) and hyperlipidaemia (P = 0.65) were not independently associated with the risk of non-fatal MI.
Using a model with standardized coefficients to assess the relative strength of each of the predictors, the adjusted variables most strongly associated with the risk of MI (from strongest to weakest), were increased age (HR: 1.70, 95% CI: 1.41–2.04, P < 0.001), higher BMI (HR: 1.32, 95% CI: 1.15–1.52, P < 0.001), hypertension (HR: 1.23, 95% CI: 1.03–1.46, P = 0.02), and current smoking (HR: 1.18, 95% CI: 1.02–1.37, P = 0.03).
After adjustment for CAD risk factors, a normal vs. elevated BMI (<25 vs. ≥25 kg/m2, P = 0.69) and an obese vs. non-obese BMI (<30 vs. ≥30 kg/m2, P = 0.27) were not associated with the risk of all-cause mortality.
Relationship of BMI with CAD as stratified by geographical location and ethnicity
We performed subgroup analyses to determine whether there were potential differences in results between regions, and compared patients from North America (n = 6087), Europe (n = 3922), and Asia (n = 3865). After adjustment for risk factors and BMI, an increased BMI was independently associated with the presence of any CAD amongst individuals in North America (OR: 1.11 per +5 kg/m2, 95% CI: 1.05–1.17, P < 0.001), with no significant relationship observed amongst individuals in Europe (OR: 1.08 per +5 kg/m2, 95% CI: 0.98–1.17, P = 0.15) or Asia (OR: 1.13 per +5 kg/m2, 95% CI: 0.99–1.28, P = 0.07). For these subgroups, there were no significant differences observed between BMI and adjusted risk of non-fatal MI (P = 0.79, 0.91, and 0.50 for North America, Europe, and Korea, respectively).
We performed additional subgroup analyses to determine whether there were differences in findings between ethnic groups. Ethnicity information was available in 10 205 individuals; amongst these individuals, 5699 were Caucasian, 3880 were Asian, and the remaining 626 patients represented other ethnicities. An increased BMI was independently associated with a greater prevalence of any CAD in Caucasian (OR: 1.15 per +5 kg/m2, 95% CI: 1.08–1.22, P < 0.001) and Asian patients (OR: 1.22 per +5 kg/m2, 95% CI: 1.08–1.39, P = 0.002), with no significant difference observed in the remaining ethnicity groups combined (OR: 1.13 per +5 kg/m2, 95% CI: 0.96–1.33, P = 0.15). For the larger subgroups, there were no significant differences observed between BMI and adjusted risk of non-fatal MI (P = 0.16 and 0.60 for Caucasian and Asian individuals, respectively).’
Discussion
The results of this prospective multicentre international study demonstrate a strong and consistent relationship between an increased BMI and the prevalence, extent and severity of CAD. Further, we determined that a greater BMI was significantly related to incident risk of non-fatal MIs, although no significant relationship was observed between BMI and all-cause mortality during the intermediate-term follow-up of the study. Finally, we observed that the increased rates of CAD and risk of non-fatal MI were independently associated with a higher BMI in a manner that was not fully explained by the co-existence of traditional CAD risk factors alone.
The present findings may serve to clarify the relationship between BMI and non-invasive measures of CAD as previously examined in prior studies. As an example, a substudy of 6814 individuals from the low-risk Multi-Ethnic Study of Atherosclerosis (MESA) population aged 45–84 years observed that obese individuals had an increased risk of CAD as measured by coronary artery calcification score.16 In a cohort referred for invasive coronary angiography, Rubinshtein et al.17 evaluated 928 patients, and reported that obese individuals were less likely to have three-vessel or left main disease, although there was a significant decrease in age with increasing BMI, which ranged from a mean age of 71–59 years for those with a BMI <21 and ≥35 kg/m2, respectively. Another study examined 770 patients referred for invasive coronary angiography and observed negative correlations between BMI and CAD burden as well as BMI and age, suggesting a potential referral bias in which that individuals with a higher BMI were referred for invasive angiography at a younger age, which may have explained the lower extent and severity of CAD.18 The present data extend those from prior studies by examining a distinct population of patients referred for non-invasive diagnostic imaging by CCTA who would be expected to be at higher risk of CAD than population-based cohorts tested by calcium scoring, and at lower risk of CAD than individuals referred for invasive procedures. This is reflected in the intermediate observed prevalence of obstructive CAD (20%) by CCTA in the present study, and the present findings are most consistent with those reported in the MESA population, as the present study identifies significant increases in CAD by both CCTA and CACS measures in patients with an increased BMI. When we examined subgroups by region or by ethnicity, we did not observe significant differences in all of the ethnic groups and regions. This may be due to inadequate power for these subgroup analyses, or may be a result of inherent differences between groups; future larger studies may be warranted to better evaluate these findings across regions and ethnic groups.
Prior population-based studies including the Framingham Heart Study, Nurses Health Study, Physicians' Health Study, Women's Health Study, and Interheart Study have observed increased mortality and/or adverse cardiac events in overweight and/or obese individuals,2–7 findings were consistent with a recent meta-analysis.8 Further, a recent study of over 1 million Asian individuals observed increased mortality in East Asians with an elevated BMI, although no differences were observed in South Asian individuals.19 The findings contrast with observations in patients with known obstructive CAD; a recent meta-analysis of 40 studies including over 250 000 patients with known CAD reported that overweight patients had the lowest rates of all-cause mortality, with no difference in mortality seen in obese patients.20 Further, a study of 16 816 patients referred for myocardial perfusion single-photon emission computed tomography observed that the BMI of patients with suspected but not known CAD was not independently associated with the risk of cardiac death, while individuals with known obstructive CAD were observed to have an inverse relationship between BMI and the risk of cardiac death.21
We examined patients with suspected CAD referred for non-invasive diagnostic imaging by CCTA, while excluding individuals with established obstructive CAD. Our results suggest that an increased BMI is associated with a significantly increased risk of non-fatal MIs in a population without known CAD referred for non-invasive diagnostic testing, even during the relatively short follow-up time of the study. These findings are consistent with the observed increase in the prevalence, extent, and severity of CAD by CCTA in larger individuals, which may be expected to be associated with an increased risk of adverse events.22 While no significant relationship was observed between BMI and non-fatal MI in subgroups by region and ethnicity, it is expected that this may be due to inadequate power in these smaller cohorts, as the overall study population only had 80% power to determine a relationship between BMI and risk of this event.
We did not observe a significant relationship between BMI and all-cause mortality. While the study was underpowered for comparisons between normal and overweight individuals, it did have adequate power between normal and obese individuals on post hoc analysis. The lack of a significant difference may be related to the relatively short period of follow-up. While a large collaborative analysis of nearly 900 000 adults from 57 prospective studies demonstrated an increase in long-term all-cause mortality between individuals with normal and increasing BMI, the study excluded the initial 5 years of follow-up, and reported events only during a subsequent mean follow-up of 8 years.8 In contrast, the current study examined only events during a intermediate-term follow-up after the CCTA study (mean of 2.4 years), and cannot determine the risk of longer-term mortality.
Of note, the relationship between BMI, other cardiovascular risk factors, and the prevalence and risk of CAD are complex. Obesity and/or an increased BMI are independently associated with greater risk of insulin resistance, metabolic syndrome, diabetes, hypertension, and dyslipidaemia, and data suggest that the presence of these comorbidities may be more important markers of CAD risk than obesity alone.23–26 Further, there is increasing evidence of a relationship between obesity and systemic inflammation, including an increased production of inflammatory factors such as leptin, tumor necrosis factor-α, interleukin-6, and resistin, as well as decreased production of adiponectin.27,28
One limitation of the present study is that it assessed risk factors as present or absent based on patient-reported history and prescribed medications, and did not confirm these diagnoses from physician records or laboratory testing at the point of service. The present study could not assess the severity of risk factors such as hypertension and diabetes, did not examine all potential covariates (such as metabolic syndrome or insulin resistance), did not evaluate the duration and treatment of risk factors, and did not obtain specific variables such as blood pressure, and inflammatory markers. Future prospective trials assessing these variables may be warranted to improve our understanding of the relationship between BMI and the prevalence, patterns, and risk of CAD.
This study has additional limitations. BMI may be an imperfect method to identify abdominal and visceral fat, as it does not distinguish lean and adipose tissue, and visceral fat (including epicardial fat) has been associated with increased CAD burden and risk of adverse events.29,30 Nevertheless, while waist-to-height ratio is observed to have the best model fit to identify risk of cardiovascular events, the difference between this measure and BMI has been reported to be of minor clinical significance.5 We employed BMI, as this is the most commonly employed metric for assessing obesity and may be easily determined, permitting these results to be maximally generalizable. Further, while CCTA has been demonstrated to have high diagnostic performance to identify obstructive CAD, it can be associated with false-positive results31–33 and may overestimate the prevalence of obstructive CAD. In addition, due to the anatomic detail provided by CT images, readers were not blinded to the patient's body habitus. Finally, the study evaluated only intermediate-term events during a mean follow-up of 2.4 years, and the risk of events over a longer period cannot be determined. While we demonstrated adequate power for risk of non-fatal MI, we did not have adequate power for risk of all-cause mortality, and as such, the latter should be considered exploratory.
In this prospective multicentre study of patients referred for non-invasive coronary imaging, overweight and obese individuals possess a greater prevalence, extent, and severity of CAD that does not appear to be entirely explained by the presence or absence of traditional risk factors alone. Further, a higher BMI is independently associated with an increased risk of intermediate-term non-fatal MI.
Conflicts of interest: There was no financial support for this manuscript. B.C. has research support from GE Healthcare, Pfizer, and AstraZeneca; and has educational support from TeraRecon. E.M. has grant support from GE Healthcare. F.C. has grant support from GE Healthcare, is on the speakers' bureau for Bracco, and is a consultant for Servier. G.R. has grant support from Siemens, Blue Cross Blue Shield Blue Care of Michigan and Bayer. J.M. is on the speakers' bureau for GE Healthcare, is on the medical advisory board for GE Healthcare, and has research support from GE Healthcare. J.H. has a research support from Siemens. K.C. has research support from Bayer and Blue Cross Blue Shield Blue Care of Michigan. M.Al.-M. has research support from the American Heart Association, the Blue Cross Blue Shield of Michigan, and Astellas. P.K. has research support from GE Healthcare and the Swiss National Science Foundation. S.A. has research support from Siemens and Bayer Schering and is a consultant for Servier.
Funding
There was no financial support for this study.
References
- 1.Klein S, Burke LE, Bray GA, Blair S, Allison DB, Pi-Sunyer X, et al. Clinical implications of obesity with specific focus on cardiovascular disease: a statement for professionals from the American Heart Association Council on nutrition, physical activity, and metabolism: endorsed by the American College of Cardiology Foundation. Circulation. 2004;110:2952–67. doi: 10.1161/01.CIR.0000145546.97738.1E. [DOI] [PubMed] [Google Scholar]
- 2.Hubert HB, Feinleib M, McNamara PM, Castelli WP. Obesity as an independent risk factor for cardiovascular disease: a 26-year follow-up of participants in the Framingham Heart Study. Circulation. 1983;67:968–77. doi: 10.1161/01.cir.67.5.968. [DOI] [PubMed] [Google Scholar]
- 3.Manson JE, Colditz GA, Stampfer MJ, Willett WC, Rosner B, Monson RR, et al. A prospective study of obesity and risk of coronary heart disease in women. N Engl J Med. 1990;322:882–9. doi: 10.1056/NEJM199003293221303. [DOI] [PubMed] [Google Scholar]
- 4.Hu FB, Willett WC, Li T, Stampfer MJ, Colditz GA, Manson JE. Adiposity as compared with physical activity in predicting mortality among women. N Engl J Med. 2004;351:2694–703. doi: 10.1056/NEJMoa042135. [DOI] [PubMed] [Google Scholar]
- 5.Gelber RP, Gaziano JM, Orav EJ, Manson JE, Buring JE, Kurth T. Measures of obesity and cardiovascular risk among men and women. J Am Coll Cardiol. 2008;52:605–15. doi: 10.1016/j.jacc.2008.03.066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yusuf S, Hawken S, Ounpuu S, Dans T, Avezum A, Lanas F, et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the interheart study): case-control study. Lancet. 2004;364:937–52. doi: 10.1016/S0140-6736(04)17018-9. [DOI] [PubMed] [Google Scholar]
- 7.Arnlov J, Ingelsson E, Sundstrom J, Lind L. Impact of body mass index and the metabolic syndrome on the risk of cardiovascular disease and death in middle-aged men. Circulation. 2010;121:230–6. doi: 10.1161/CIRCULATIONAHA.109.887521. [DOI] [PubMed] [Google Scholar]
- 8.Whitlock G, Lewington S, Sherliker P, Clarke R, Emberson J, Halsey J, et al. Body-mass index and cause-specific mortality in 900 000 adults: collaborative analyses of 57 prospective studies. Lancet. 2009;373:1083–96. doi: 10.1016/S0140-6736(09)60318-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Folsom AR, Kronmal RA, Detrano RC, O'Leary DH, Bild DE, Bluemke DA, et al. Coronary artery calcification compared with carotid intima-media thickness in the prediction of cardiovascular disease incidence: the multi-ethnic study of atherosclerosis (mesa) Arch Intern Med. 2008;168:1333–9. doi: 10.1001/archinte.168.12.1333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Min JK, Dunning A, Lin FY, Achenbach S, Al-Mallah MH, Berman DS, et al. Rationale and design of the CONFIRM (coronary CT angiography evaluation for clinical outcomes: an international multicenter) registry. J Cardiovasc Comput Tomogr. 2011;5:84–92. doi: 10.1016/j.jcct.2011.01.007. [DOI] [PubMed] [Google Scholar]
- 11.Abbara S, Arbab-Zadeh A, Callister TQ, Desai MY, Mamuya W, Thomson L, et al. Scct guidelines for performance of coronary computed tomographic angiography: a report of the society of cardiovascular computed tomography guidelines committee. J Cardiovasc Comput Tomogr. 2009;3:190–204. doi: 10.1016/j.jcct.2009.03.004. [DOI] [PubMed] [Google Scholar]
- 12.Raff GL, Abidov A, Achenbach S, Berman DS, Boxt LM, Budoff MJ, et al. Scct guidelines for the interpretation and reporting of coronary computed tomographic angiography. J Cardiovasc Comput Tomogr. 2009;3:122–36. doi: 10.1016/j.jcct.2009.01.001. [DOI] [PubMed] [Google Scholar]
- 13.Carr JJ, Nelson JC, Wong ND, McNitt-Gray M, Arad Y, Jacobs DR, Jr, et al. Calcified coronary artery plaque measurement with cardiac CT in population-based studies: standardized protocol of multi-ethnic study of atherosclerosis (mesa) and coronary artery risk development in young adults (cardia) study. Radiology. 2005;234:35–43. doi: 10.1148/radiol.2341040439. [DOI] [PubMed] [Google Scholar]
- 14.Min JK, Shaw LJ, Devereux RB, Okin PM, Weinsaft JW, Russo DJ, et al. Prognostic value of multidetector coronary computed tomographic angiography for prediction of all-cause mortality. J Am Coll Cardiol. 2007;50:1161–70. doi: 10.1016/j.jacc.2007.03.067. [DOI] [PubMed] [Google Scholar]
- 15.Lin F, Shaw LJ, Berman DS, Callister TQ, Weinsaft JW, Wong FJ, et al. Multidetector computed tomography coronary artery plaque predictors of stress-induced myocardial ischemia by SPECT. Atherosclerosis. 2008;197:700–9. doi: 10.1016/j.atherosclerosis.2007.07.002. [DOI] [PubMed] [Google Scholar]
- 16.Burke GL, Bertoni AG, Shea S, Tracy R, Watson KE, Blumenthal RS, et al. The impact of obesity on cardiovascular disease risk factors and subclinical vascular disease: the multi-ethnic study of atherosclerosis. Arch Intern Med. 2008;168:928–35. doi: 10.1001/archinte.168.9.928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rubinshtein R, Halon DA, Jaffe R, Shahla J, Lewis BS. Relation between obesity and severity of coronary artery disease in patients undergoing coronary angiography. Am J Cardiol. 2006;97:1277–80. doi: 10.1016/j.amjcard.2005.11.061. [DOI] [PubMed] [Google Scholar]
- 18.Niraj A, Pradhan J, Fakhry H, Veeranna V, Afonso L. Severity of coronary artery disease in obese patients undergoing coronary angiography: ‘obesity paradox’ revisited. Clin Cardiol. 2007;30:391–6. doi: 10.1002/clc.20113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zheng W, McLerran DF, Rolland B, Zhang X, Inoue M, Matsuo K, et al. Association between body-mass index and risk of death in more than 1 million Asians. N Engl J Med. 2010;364:719–29. doi: 10.1056/NEJMoa1010679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Romero-Corral A, Montori VM, Somers VK, Korinek J, Thomas RJ, Allison TG, et al. Association of bodyweight with total mortality and with cardiovascular events in coronary artery disease: a systematic review of cohort studies. Lancet. 2006;368:666–78. doi: 10.1016/S0140-6736(06)69251-9. [DOI] [PubMed] [Google Scholar]
- 21.Kang X, Shaw LJ, Hayes SW, Hachamovitch R, Abidov A, Cohen I, et al. Impact of body mass index on cardiac mortality in patients with known or suspected coronary artery disease undergoing myocardial perfusion single-photon emission computed tomography. J Am Coll Cardiol. 2006;47:1418–26. doi: 10.1016/j.jacc.2005.11.062. [DOI] [PubMed] [Google Scholar]
- 22.Nelson RC, Feuerlein S, Boll DT. New iterative reconstruction techniques for cardiovascular computed tomography: how do they work, and what are the advantages and disadvantages? J Cardiovasc Comput Tomogr. 2011;5:286–92. doi: 10.1016/j.jcct.2011.07.001. [DOI] [PubMed] [Google Scholar]
- 23.Klein S, Allison DB, Heymsfield SB, Kelley DE, Leibel RL, Nonas C, et al. Waist circumference and cardiometabolic risk: a consensus statement from Shaping America's Health: Association for Weight Management and Obesity Prevention; NAASO, the Obesity Society; the American Society for Nutrition; and the American Diabetes Association. Obesity (Silver Spring) 2007;15:1061–7. doi: 10.1038/oby.2007.632. [DOI] [PubMed] [Google Scholar]
- 24.Katzmarzyk PT, Janssen I, Ross R, Church TS, Blair SN. The importance of waist circumference in the definition of metabolic syndrome: prospective analyses of mortality in men. Diabetes Care. 2006;29:404–9. doi: 10.2337/diacare.29.02.06.dc05-1636. [DOI] [PubMed] [Google Scholar]
- 25.Song Y, Manson JE, Meigs JB, Ridker PM, Buring JE, Liu S. Comparison of usefulness of body mass index versus metabolic risk factors in predicting 10-year risk of cardiovascular events in women. Am J Cardiol. 2007;100:1654–8. doi: 10.1016/j.amjcard.2007.06.073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wildman RP, McGinn AP, Lin J, Wang D, Muntner P, Cohen HW, et al. Cardiovascular disease risk of abdominal obesity vs. metabolic abnormalities. Obesity (Silver Spring) 2011;19:853–60. doi: 10.1038/oby.2010.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bastard JP, Maachi M, Lagathu C, Kim MJ, Caron M, Vidal H, et al. Recent advances in the relationship between obesity, inflammation, and insulin resistance. Eur Cytokine Netw. 2006;17:4–12. [PubMed] [Google Scholar]
- 28.Galic S, Oakhill JS, Steinberg GR. Adipose tissue as an endocrine organ. Mol Cell Endocrinol. 2010;316:129–39. doi: 10.1016/j.mce.2009.08.018. [DOI] [PubMed] [Google Scholar]
- 29.Cheng VY, Dey D, Tamarappoo B, Nakazato R, Gransar H, Miranda-Peats R, et al. Pericardial fat burden on ECG-gated noncontrast CT in asymptomatic patients who subsequently experience adverse cardiovascular events. JACC Cardiovasc Imaging. 2010;3:352–60. doi: 10.1016/j.jcmg.2009.12.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rosito GA, Massaro JM, Hoffmann U, Ruberg FL, Mahabadi AA, Vasan RS, et al. Pericardial fat, visceral abdominal fat, cardiovascular disease risk factors, and vascular calcification in a community-based sample: the Framingham Heart Study. Circulation. 2008;117:605–13. doi: 10.1161/CIRCULATIONAHA.107.743062. [DOI] [PubMed] [Google Scholar]
- 31.Budoff MJ, Dowe D, Jollis JG, Gitter M, Sutherland J, Halamert E, et al. Diagnostic performance of 64-multidetector row coronary computed tomographic angiography for evaluation of coronary artery stenosis in individuals without known coronary artery disease: results from the prospective multicenter accuracy (assessment by coronary computed tomographic angiography of individuals undergoing invasive coronary angiography) trial. J Am Coll Cardiol. 2008;52:1724–32. doi: 10.1016/j.jacc.2008.07.031. [DOI] [PubMed] [Google Scholar]
- 32.Miller JM, Rochitte CE, Dewey M, Arbab-Zadeh A, Niinuma H, Gottlieb I, et al. Diagnostic performance of coronary angiography by 64-row CT. N Engl J Med. 2008;359:2324–36. doi: 10.1056/NEJMoa0806576. [DOI] [PubMed] [Google Scholar]
- 33.Meijboom WB, Meijs MF, Schuijf JD, Cramer MJ, Mollet NR, van Mieghem CA, et al. Diagnostic accuracy of 64-slice computed tomography coronary angiography: a prospective, multicenter, multivendor study. J Am Coll Cardiol. 2008;52:2135–44. doi: 10.1016/j.jacc.2008.08.058. [DOI] [PubMed] [Google Scholar]