Abstract
Background
Primary care physicians (PCPs) treat many women of reproductive age who need contraceptive and preconception counseling.
Study Design
To evaluate perceptions of rates of unintended pregnancy, we distributed an online survey in 2009 to 550 PCPs trained in General Internal Medicine or Family Medicine practicing in Western Pennsylvania, Central Pennsylvania, Rhode Island or Oregon.
Results
Surveys were completed by 172 PCPs (31%). The majority (54%) of respondents underestimated the prevalence of unintended pregnancy in the United States [on average, by 23±8 (mean±SD) percentage points], and 81% underestimated the risk of pregnancy among women using no contraception [on average, by 35±20 (mean±SD) percentage points]. PCPs also frequently underestimated contraceptive failure rates with typical use: 85% underestimated the failure rate for oral contraceptive pills, 62% for condoms and 16% for contraceptive injections. PCPs more often overestimated the failure rate of intrauterine devices (17%) than other prescription methods. In adjusted models, male PCPs were significantly more likely to underestimate the rate of unintended pregnancy in the United States than female PCPs [adjusted odds ratio (95% confidence interval): 2.17 (1.01–4.66)].
Conclusions
Many PCPs have inaccurate perceptions of rates of unintended pregnancy, both with and without use of contraception, which may influence the frequency and the content of the contraceptive counseling they provide.
Keywords: Contraceptive counseling, Contraception, Primary care, Women’s health, Unplanned pregnancy, Contraception failure rate
1. Introduction
Unintended pregnancy remains a pressing public health issue for the United States. Nearly 50% of US pregnancies are unplanned [1], with far-reaching consequences for both mothers and babies [2–4]. Primary care providers (PCPs) treat many women of reproductive age [5,6], including women whose disease and use of potentially teratogenic medications may increase risk of birth defects and other adverse pregnancy outcomes [7–10]. As recently highlighted by the Institute of Medicine (IOM), preconception counseling and contraceptive counseling are key components of comprehensive preventive care [11] which can help women, particularly those with chronic conditions, improve their health status prior to pregnancy and reduce the risk of adverse birth outcomes. As PCPs have regular contact with patients and are aware of their existing health conditions and prescriptions, they are well positioned to provide this counseling [12,13], which has been associated with greater contraceptive use among primary care patients [14–17].
However, prior work has shown that PCPs rarely provide preconception and contraceptive counseling [18,19]. PCPs’ perceptions of their patients’ risk of unintended pregnancy and perceptions of the relative effectiveness of contraceptive options likely influence both the frequency with which they feel it is necessary to provide such counseling as well as the content of the counseling they provide. Effective contraceptive counseling can only occur when PCPs recognize their patients’ needs for counseling and are able to deliver accurate messages regarding risk of pregnancy and the effectiveness of available contraceptives. Family medicine trainees [19] and family medicine physicians [20] have been found to have lower levels of contraceptive knowledge than obstetrics and gynecology trainees and physicians. This is of concern because contraceptive effectiveness is a major factor in women’s contraceptive decision-making [21,22]. Provision of inaccurate information by PCPs may translate into suboptimal contraceptive choices by patients and may be one reason why use of highly effective contraceptives, such as intrauterine devices (IUDs), is much lower in the United States than in other developed countries [23].
This analysis sought to assess perceptions among general internists and family physicians of the prevalence of unintended pregnancy in the United States, perceptions of rates of pregnancy when using no method of contraception and perceptions of the typical-use failure rates of available contraceptives. Additionally, we sought to identify physician characteristics associated with inaccurate perceptions of these rates in order to identify possible targets for educational efforts.
2. Materials and methods
We distributed an online survey to a convenience sample of 550 PCPs trained in General Internal Medicine or Family Medicine practicing in Western Pennsylvania (n=70), Central Pennsylvania (n=100), Rhode Island (n=180) and Oregon (n=200) in 2009. Physicians invited to complete the survey shared an institutional or professional affiliation with one of the study investigators, allowing for easy distribution of the survey through existing e-mail list servers. Physicians were offered US$ 20 for completing the survey. This survey was part of a larger project designed to assess PCPs’ experiences using clinical decision support systems. Physicians provided information on the number of patients they care for per week, the characteristics of their patient population, their clinical responsibilities, whether they had religious objections to contraceptive use and personal demographic information. Relevant to this analysis, the survey contained six open-ended questions that asked physicians to provide the rate of unintended pregnancy in the United States and risk of pregnancy among users of various contraceptive methods. Specifically, physicians were asked, “What percentage of U.S. pregnancies are unintended?” and “If 100 fertile women are sexually active, how many would you expect to become pregnant within one year if they use [each of the following methods: no method, condoms, oral contraceptive pills, contraceptive injections and IUDs]?”
Responses were grouped into three categories: “correct estimate,” “underestimate” or “overestimate.” Responses were considered to be a “correct estimate” if they were within 2 percentage points above or below the “typical-use failure rates” provided by the 19th edition of Contraceptive Technology [24]: no method (85%), condoms (15%), oral contraceptive pills (8%), contraceptive injections (3%) and IUDs (<1%). Typical-use failure rates describe the effectiveness of contraceptives for a real-world woman who may forget to take a daily pill or have other difficulties with using a method consistently. Forty-nine percent was used as the correct answer for rate of unintended pregnancy in the United States because it is both the most recently published rate [1] and a statistic that has remained unchanged for over a decade [25].
We described the characteristics of the survey respondents both overall and by gender using χ2 and Fisher’s Exact Tests to test for significant differences. We calculated the number of questions each physician answered correctly. To explore the range of physician responses, histograms were created for each survey question. We also examined the breakdown of responses that were correct, underestimates and overestimates, and calculated the average degree of under- or overestimation for each contraceptive. Finally, we used multivariable logistic regression to identify physician characteristics potentially associated with underestimating rates of unintended pregnancy. We ran six separate models, one for each question of interest. All models were adjusted for geographic location to control for variation in the number of responses by location. Each model included the same group of potential predictors: gender, age category, experience supervising clinical trainees [yes/no (Y/N)], being a parent (Y/N), religious objections to use of contraception (Y/N), number of patients seen per week and percent of patients who are women of reproductive age. All variables were added to the model simultaneously. Because it was impossible to underestimate the typical-use failure rate of an IUD, we instead sought to identify factors related to overestimation of the IUD failure rate. We recognize that defining a “correct estimate” for contraceptive failure rates to be within 2 percentage points is a relatively narrow window, so we ran additional models defining a “correct estimate” to be ±5 percentage points of the published typical-use failure rates as a sensitivity analysis.
In order to explore whether inaccurate perceptions were associated with less frequent provision of family planning services to female patients, we conducted a subanalysis using data from Western Pennsylvanian PCPs. We linked these physicians’ survey responses to prescribing data abstracted from the electronic medical record (EMR). We abstracted data from all visits with female patients between 18 and 50 years of age who did not have documentation of surgical sterilization, menopause or infertility. For each PCP, we calculated the percentage of all of their visits that had evidence of provision of family planning services (new or active contraception prescriptions, contraceptive counseling, referrals to family planning specialists and pregnancy testing), as well as the percentage of their visits which involved a prescription for a potentially teratogenic medication that also had evidence of family planning services. We calculated the Pearson correlation coefficient for the relationship between percent of visits with family planning services and the percent of survey questions answered correctly. We also compared the mean percent of visits with family planning services in the group that provided an incorrect estimate to the mean percent of visits with family planning services in the group that answered correctly.
The University of Pittsburgh Institutional Review Board approved the study, and participants provided informed consent. All statistical analyses were performed using Stata 11.0 (StataCorp. College Station, TX, USA).
3. Results
One hundred and seventy-two PCPs completed the survey questions of interest (a response rate of 31%). Surveys were most frequently returned from Western Pennsylvania (contributing 33% of surveys); 21% of surveys were contributed by Oregon, 11% were from Central Pennsylvania, and 5% were from Rhode Island. An additional 30% of respondents did not provide information on their location because they declined compensation for completing the survey and, thus, were not asked to provide their address. Thus, we cannot determine specific response rates for each of the geographic locations. The characteristics of the physician respondents are provided in Table 1. Compared to the female respondents, male respondents were significantly older, were more likely to be parents, had been practicing for a greater number of years, saw a greater number of patients per week and reported that a lower percentage of their patients were females of reproductive age (Table 1).
Table 1.
Description of participating primary care physicians
| Characteristic | Overall | Male | Female | p value |
|---|---|---|---|---|
| n=172 | n=73 | n=99 | ||
| Age category, n (%) | .01 | |||
| <30 years | 40 (23.3) | 12 (16.4) | 28 (28.3) | |
| 30–39 years | 60 (34.9) | 23 (31.5) | 37 (37.4) | |
| 40–49 years | 33 (19.2) | 13 (17.8) | 20 (20.2) | |
| ≥50 years | 39 (22.7) | 25 (34.3) | 14 (14.1) | |
| Have children, n (%) | 92 (53.5) | 46 (63.0) | 46 (46.5) | .03 |
| Supervise trainees, n (%) | 66 (38.4) | 31 (42.5) | 35 (35.4) | .34 |
| Have a religious objection to contraception, n (%) | 15 (8.7) | 8 (11.0) | 7 (7.1) | .37 |
| Number of patients per week, median (IQR) | 23.5 (54) | 40 (67) | 20 (36) | .006 |
| % of patients who are women of reproductive age, median (IQR) | 25 (27.5) | 20 (18) | 30 (30) | <.001 |
IQR, interquartile range
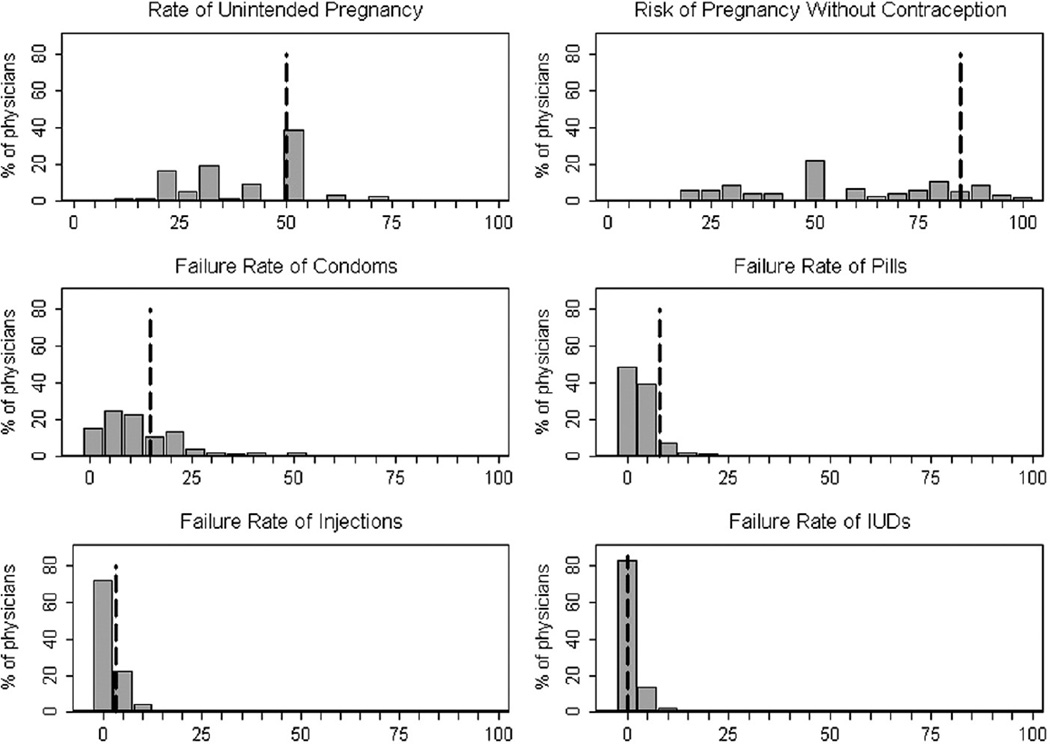
On average, physicians answered 38%±16% (mean±SD) of the six questions correctly. Three PCPs scored over 80%, and 36 scored under 20%. The distributions of PCP responses to each question are presented in Fig. 1, and the proportions of responses falling into each category of accuracy are reported in Table 2. The majority (54%) of responding PCPs underestimated the unintended pregnancy rate in the United States, and their responses ranged widely. On average, those who underestimated the unintended pregnancy rate did so by 23±8 (mean±SD) percentage points. Similarly, 81% of respondents underestimated the risk of pregnancy when using no contraception, and the response range was wide: those who underestimated the risk of pregnancy when using no contraception did so by 35±20 (mean±SD) percentage points. The majority of PCPs also underestimated the typical-use failure rate of birth control pills [85% underestimated, by an average of 5±2 (mean±SD) percentage points] and condoms [62% underestimated, by an average of 9±3 (mean±SD) percentage points]. Respondents less frequently underestimated the failure rate of contraceptive injections (16% underestimated). It was impossible to underestimate the failure rate of IUDs since the failure rate is so low. However, PCPs more often overestimated the failure rate of IUDs (17% overestimated) than of other prescription methods (Table 2); on average, PCPs overestimated the failure rate of IUDs by 7±11 (mean±SD) percentage points.
Fig. 1.
Distribution of PCPs’ perceptions of US unintended pregnancy rates, risk of pregnancy if using no contraception and typical-use failure rates of available methods per 100 woman–years, with dotted line indicating the correct response, n=172.
Table 2.
Proportion of PCPs underestimating, correctly estimating and overestimating US unintended pregnancy rate, risk of pregnancy with no contraception and typical-use failure rates (n=172)
| Question | Published rate per 100 woman–yearsa |
Underestimate n (%) |
Correctb n (%) |
Overestimate n (%) |
|---|---|---|---|---|
| Unintended pregnancy rate in the United States | 49% | 93 (54.1) | 67 (38.9) | 12 (7.0) |
| Risk of pregnancy without contraception | 85% | 140 (81.4) | 9 (5.2) | 23 (13.4) |
| Typical-use failure rate of condoms | 15% | 107 (62.2) | 19 (11.1) | 46 (26.7) |
| Typical-use failure rate of oral contraceptive pills | 8% | 147 (85.5) | 18 (10.5) | 7 (4.1) |
| Typical-use failure rate of contraceptive injections | 3% | 27 (15.7) | 134 (77.9) | 11 (6.4) |
| Typical-use failure rate of IUDs | <1% | 0 (0.0) | 142 (82.6) | 30 (17.4) |
Source: the 19th edition of Contraceptive Technology
Responses were considered to be “correct” if they were within ±2 percentage points of published “typical-use failure rates.”
In multivariable models, male PCPs were over two times as likely to underestimate the US unintended pregnancy rate than female PCPs [adjusted odds ratio (OR) (95% confidence interval {CI}): 2.17 (1.01–4.66)] (Table 3). Additionally, as the percentage of a PCP’s patients who were women of reproductive age increased, the likelihood of underestimating the unintended pregnancy rate decreased (Table 3). Males were not significantly more likely to underestimate the risk of pregnancy among nonusers of contraception compared to females (Table 3), but they were almost three times as likely as female PCPs to underestimate the rate of condom failure [adjusted OR (95% CI): 2.95 (1.28–6.78)] and over three times as likely as female PCPs to overestimate the failure rate of IUDs [adjusted OR (95% CI): 3.45 (1.25–9.48)] (Table 4). PCPs who supervise trainees were not more likely to have accurate perceptions of rates of unintended pregnancy, risk of pregnancy without contraception (Table 3) or contraceptive failure rates (Table 4) than PCPs who do not supervise trainees. Considering responses to be correct if they were within a wider range of ±5 percentage points mitigated, but did not eliminate, the effect of male gender on underestimation of rates of unintended pregnancy [adjusted OR (95% CI): 2.17 (1.00–4.66)] and of condom failure rate [adjusted OR (95% CI): 2.03 (0.95–4.36)] when compared to female gender.
Table 3.
Association of physician characteristics with underestimation of US unintended pregnancy rate and risk of pregnancy when using no method of contraception (n=172)
| Physician characteristics | Underestimate US unintended pregnancy rate OR (95% CI) |
Underestimate risk of pregnancy with no contraception OR (95% CI) |
|---|---|---|
| Gender | ||
| Female | Referent | Referent |
| Male | 2.17 (1.01–4.66) | 0.90 (0.33–2.42) |
| Age category | ||
| <30 years | Referent | Referent |
| 30–39 years | 0.56 (0.20–1.55) | 0.29 (0.08–1.06) |
| 40–49 years | 1.29 (0.34–4.98) | 0.89 (0.16–5.00) |
| ≥50 years | 0.79 (0.20–3.03) | 0.79 (0.15–4.11) |
| Have children | ||
| No | Referent | Referent |
| Yes | 1.57 (0.59–4.14) | 1.29 (0.43–3.92) |
| Supervise trainees | ||
| No | Referent | Referent |
| Yes | 0.88 (0.39–1.98) | 1.66 (0.62–4.41) |
| Religious objection to contraception | ||
| No | Referent | Referent |
| Yes | 2.23 (0.59–8.41) | 0.96 (0.22–4.17) |
| Number of patients per weeka | 1.00 (0.99–1.01) | 0.99 (0.99–1.00) |
| % of patients who are women of reproductive agea | 0.97 (0.96–0.99) | 1.00 (0.97–1.02) |
Logistic regression models adjusted for all variables in the table, as well as geographic location
Entered as a continuous variable
Table 4.
Association of physician characteristics with incorrect perceptions of typical-use contraceptive failure rates (n=172)
| Underestimate condom failure rate OR (95% CI) |
Underestimate pill failure rate OR (95% CI) |
Underestimate injection failure rate OR (95% CI) |
Overestimate IUDa failure rate OR (95% CI) |
|
|---|---|---|---|---|
| Gender | ||||
| Female | Referent | Referent | Referent | Referent |
| Male | 2.95 (1.28–6.78) | 2.64 (0.85–8.23) | 0.56 (0.18–1.70) | 3.45 (1.25–9.48) |
| Age category | ||||
| <30 years | Referent | Referent | Referent | Referent |
| 30–39 years | 0.59 (0.21–1.70) | 1.00 (0.29–3.43) | 0.64 (0.15–2.62) | 0.98 (0.26–3.64) |
| 40–49 years | 0.38 (0.10–1.49) | 1.18 (0.18–7.73) | 1.90 (0.33–10.92) | 4.30 (0.79–23.21) |
| ≥50 years | 0.24 (0.06–0.97) | 0.43 (0.07–2.66) | 2.50 (0.39–15.93) | 1.11 (0.20–6.19) |
| Have children | ||||
| No | Referent | Referent | Referent | Referent |
| Yes | 1.27 (0.48–3.34) | 2.37 (0.66–8.55) | 0.52 (0.15–1.80) | 0.57 (0.16–2.00) |
| Supervise trainees | ||||
| No | Referent | Referent | Referent | Referent |
| Yes | 1.18 (0.53–2.63) | 0.66 (0.19–2.24) | 1.75 (0.59–5.21) | 0.36 (0.12–1.04) |
| Religious objection to contraception | ||||
| No | Referent | b | Referent | Referent |
| Yes | 1.74 (0.51–5.94) | b | 1.29 (0.29–5.70) | 1.62 (0.41–6.36) |
| Number of patients per weekc | 0.99 (0.99–1.00) | 1.00 (0.99–1.01) | 1.00 (0.99–1.01) | 1.00 (0.99–1.01) |
| % of patients who are women of reproductive agec | 0.99 (0.97–1.00) | 1.00 (0.97–1.02) | 1.03 (1.00–1.05) | 1.00 (0.97–1.02) |
Logistic regression models adjusted for all variables in the table, as well as geographic location.
This model predicts overestimation of failure rates of intrauterine devices (IUDs) because the failure rate is <1% and impossible to underestimate.
All PCPs with a religious objection to contraception underestimated pill failure rates.
Entered as a continuous variable.
When we linked survey data from 56 PCPs from Western Pennsylvania to their EMR prescribing records, we found that the percent of survey questions answered correctly by the PCP was significantly associated with the percent of a PCP’s visits with evidence of family planning services (r=+0.31, p=.02), as well as the percent of their visits involving a teratogenic prescription with evidence of family planning services (r= +0.27, p=.04). Provision of family planning services was documented on 30%±11% (mean±SD) of visits made by a woman of reproductive age to PCPs with accurate perceptions of US rates of unintended pregnancy, but family planning services were documented on only 23%±10% (mean±SD) of visits made by such women to PCPs with inaccurate perceptions of rates of unintended pregnancy, p=.03. This disparity remained even when we limited the analysis to visits in which a PCP prescribed potentially teratogenic medications [22.2%±13.8% (mean±SD) correct responders vs. 18.0%±16.1% (mean±SD) incorrect responders, p=.3].
4. Discussion
The majority of PCPs in this study underestimated US rates of unintended pregnancy and rates of pregnancy when no contraception is used. Further, PCPs frequently underestimated the typical-use failure rates of condoms and oral contraceptive pills, the two most popular reversible contraceptive options in the United States. Compared to other prescription contraceptives, PCPs were more likely to overestimate the failure rate of IUDs. Male PCPs were significantly more likely than female PCPs to underestimate the rate of unintended pregnancy and the failure rate of condoms and to overestimate the failure rate of IUDs. Of concern, PCPs involved in training future PCPs were not more likely to have accurate perceptions of rates of unintended pregnancy and contraceptive effectiveness. In addition, inaccurate perceptions of rates of unintended pregnancy were associated with less frequent provision of family planning services to female patients, even when potentially teratogenic medications were prescribed. Inaccurate perceptions of pregnancy risk could lead to less frequent provision of family planning services. Additionally, although the IOM has made clear that these are core preventive health services [11], some PCPs may never even consider pregnancy risk in the context of providing care, as they may not feel responsible for addressing a woman’s family planning needs, expecting this aspect of care to be managed by the woman’s gynecologist. However, this fragmentation of care is particularly dangerous when PCPs prescribe potentially teratogenic medications. This study cannot distinguish between the effects of inaccurate perceptions vs. the effects of an essential lack of consideration of a woman’s pregnancy risk and her family planning needs.
To our knowledge, this is the first study to examine PCPs’ perceptions of rates of unintended pregnancy and the effects these perceptions may have on PCPs’ provision of contraceptive services. We are aware of only one other study that specifically asked PCPs about contraceptive failure rates [26]; however, in that analysis, responses were considered to be correct if they were consistent with either typical-use or perfect-use failure rates. Our findings are consistent with other recent studies which have concluded that many PCPs hold inaccurate and outdated views about available contraceptive methods and that male PCPs have less accurate contraceptive knowledge than female PCPs [19,20]. Our findings also support several recent studies which have found that PCPs are greatly misinformed about the side effects of and range of women who could benefit from the use of an IUD [27–29].
While some may consider our window of ±2 percentage points above or below the published value to be overly strict, these failure rates have been widely reported since 2004 when they were published in the 18th edition of Contraceptive Technology and are lower than more recently published rates [30], so physicians reporting these new rates would not be categorized as underestimating failure rates in our analysis. Additionally, the typical-use failure rates of these methods are fairly close together, and underestimating the rate of one method, even by a few percentage points, could lead the patient to choose a less effective method.
There are, however, several limitations to this study. We surveyed a convenience sample of PCPs from only four geographic areas, we have no information on how responding PCPs differed from nonresponders, and the response rate was low (31%). Physicians are notoriously difficult to survey [31], and our response rate is similar to that typically seen with other online surveys [32,33], but these factors do make our results less generalizable. Additionally, our limited sample size did not provide enough power to detect the potentially important contribution of certain predictors or the presence of interactions. Although we attempted to control for the fact that the male PCPs in our sample were substantially older than the females, saw more patients per week and saw less female patients of reproductive age, it is impossible to make conclusions regarding younger male PCPs or male PCPs who see a high percentage of female patients because there were so few of them in this sample. In addition, we did not collect information on PCPs’ personal experiences with unintended pregnancy, the average age (and thus fecundity) of their female patients or past receipt of specialized training in family planning and/or women’s health, all of which could significantly influence PCP perceptions. The EMR data used in the subanalysis do not completely capture instances of contraceptive and preconception counseling because PCPs cannot bill for these services and some women depend on nonprescription contraception or a partner’s vasectomy. However, under-documentation of provision of contraceptive counseling or services should not differ by the PCPs’ perceptions of rates of unintended pregnancy. As respondents could have accessed clinical references while completing this survey, their responses may overestimate their true level of knowledge. Finally, as most of the physicians surveyed are affiliated with academic medical centers, the responses to this survey likely overestimate awareness of contraceptive effectiveness among community-based PCPs.
In conclusion, preconception counseling and contraceptive counseling are key components of comprehensive primary care [11] that are particularly important to women with chronic medical conditions who require use of potentially teratogenic medications. The findings from this study raise important issues regarding primary care training and continuing education to ensure safe prescribing practices and optimal pregnancy outcomes. Given the fact that PCPs prescribe the majority of potentially teratogenic medications [7], efforts are needed to educate PCPs on the importance of their role in providing preconception and contraceptive counseling to their female patients. To improve PCPs’ abilities to provide such counseling in an accurate and effective manner, PCPs’ need to be aware of the true rate of unintended pregnancy in the United States and the typicaluse failure rates of available contraceptive options. Our findings suggest that male PCPs, particularly those who are older, may have particular needs for continuing education. Future studies are needed to assess how to effectively design education programs and systems to inform PCPs of current rates of unintended pregnancy and remind them of this risk when prescribing potentially teratogenic medications. Whether more accurate knowledge about rates of unintended pregnancy and contraceptive effectiveness will increase PCPs’ provision of preconception and contraceptive counseling deserves further study.
Acknowledgments
The data used in this analysis were collected with funding from the Agency for Healthcare Research and Quality (R18HS017093). Dr. Schwarz was funded by the National Institute of Child Health and Human Development (K23 HD051585).
Footnotes
An oral abstract describing this work was presented at the Society for General Internal Medicine’s Annual Meeting in Phoenix, AZ, on May 5, 2011.
References
- 1.Finer LB, Henshaw SK. Disparities in rates of unintended pregnancy in the United States, 1994 and 2001. Perspect Sex and Reprod Health. 2006;38:90–96. doi: 10.1363/psrh.38.090.06. [DOI] [PubMed] [Google Scholar]
- 2.Cheng D, Schwarz EB, Douglas E, Horon I. Unintended pregnancy and associated maternal preconception, prenatal and postpartum behaviors. Contraception. 2009;79:194–198. doi: 10.1016/j.contraception.2008.09.009. [DOI] [PubMed] [Google Scholar]
- 3.Tsui AO, McDonald-Mosley R, Burke AE. Family planning and the burden of unintended pregnancies. Epidemiol Rev. 2010;32:152–174. doi: 10.1093/epirev/mxq012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gipson JD, Koenig MA, Hindin MJ. The effects of unintended pregnancy on infant, child, and parental health: a review of the literature. Stud Family Plann. 2008;39:18–38. doi: 10.1111/j.1728-4465.2008.00148.x. [DOI] [PubMed] [Google Scholar]
- 5.Schoelle SH, Chang JC, Harman J, McNeil M. Trends in women’s health services by type of physician seen: data from the 1985 and 1997–98 NAMCS. Women Health Iss. 2002;12:165–177. doi: 10.1016/s1049-3867(02)00139-1. [DOI] [PubMed] [Google Scholar]
- 6.Henderson JT, Weisman CS, Grason H. Are two doctors better than one? Women’s physician use and appropriate care. Women Health Iss. 2002;12:138–149. doi: 10.1016/s1049-3867(02)00134-2. [DOI] [PubMed] [Google Scholar]
- 7.Schwarz EB, Maselli J, Norton M, Gonzales R. Prescriptions of teratogenic medications in United States ambulatory practices. Am J Med. 2005;118:1240–1249. doi: 10.1016/j.amjmed.2005.02.029. [DOI] [PubMed] [Google Scholar]
- 8.Chu SY, Kim SY, Lau J, Schmid CH, Dietz PM, Callaghan WM. Maternal obesity and risk of stillbirth: a metaanalysis. Am J Obstet Gynecol. 2007;197:223–228. doi: 10.1016/j.ajog.2007.03.027. [DOI] [PubMed] [Google Scholar]
- 9.Centers for Disease Control. Birth defects. [cited 7/20/2011];2011 Available from http://www.cdc.gov/ncbddd/bd/default.htm.
- 10.Chakravarty EF, Nelson L, Krishnan E. Obstetric hospitalizations in the United States for women with systemic lupus erythematosus and rheumatoid arthritis. Arthritis Rheum. 2006;54:899–907. doi: 10.1002/art.21663. [DOI] [PubMed] [Google Scholar]
- 11.Committee on Preventive Services for Women, Institute of Medicine. Clinical preventive services for women: closing the gaps. Washington, DC: National Academies Press; 2011. [Google Scholar]
- 12.Files J, David P, Frey K. The patient-centered medical home and preconception care: an opportunity for internists. J Gen Intern Med. 2008;23:1518–1520. doi: 10.1007/s11606-008-0657-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Berghella V, Buchanan E, Pereira L, Baxter JK. Preconception care. Obstet Gynecol Surv. 2010;65:119–131. doi: 10.1097/OGX.0b013e3181d0c358. [DOI] [PubMed] [Google Scholar]
- 14.Lee JK, Parisi SM, Akers AY, Borrerro S, Schwarz EB. The impact of contraceptive counseling in primary care on contraceptive use. J Gen Intern Med. 2011:1–6. doi: 10.1007/s11606-011-1647-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Upson K, Reed SD, Prager SW, Schiff MA. Factors associated with contraceptive nonuse among US women ages 35–44 years at risk of unwanted pregnancy. Contraception. 2010;81:427–434. doi: 10.1016/j.contraception.2009.12.013. [DOI] [PubMed] [Google Scholar]
- 16.Huber LR, Ersek JL. Contraceptive use among sexually active university students. J Womens Health. 2009;18:1063–1070. doi: 10.1089/jwh.2008.1131. [DOI] [PubMed] [Google Scholar]
- 17.Harper CC, Brown BA, Foster-Rosales A, Raine TR. Hormonal contraceptive method choice among young, low-income women: how important is the provider? Patient Educ Couns. 2010;81:349–354. doi: 10.1016/j.pec.2010.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Frost JJ. Trends in U.S. women’s use of sexual and reproductive health care services, 1995–2002. Am J Public Health. 2008;98:1814–1817. doi: 10.2105/AJPH.2007.124719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Schreiber CA, Harwood BJ, Switzer GE, Creinin MD, Reeves MF, Ness RB. Training and attitudes about contraceptive management across primary care specialties: a survey of graduating residents. Contraception. 2006;73:618–622. doi: 10.1016/j.contraception.2006.01.014. [DOI] [PubMed] [Google Scholar]
- 20.Dehlendorf C, Levy K, Ruskin R, Steinauer J. Health care providers’ knowledge about contraceptive evidence: a barrier to quality family planning care? Contraception. 2010;81:292–298. doi: 10.1016/j.contraception.2009.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Garcia SG, Snow R, Aitken I. Preferences for contraceptive attributes: voices of women in Cuidad Juárez, Mexico. Int Fam Plan Perspec. 1997;23:52–58. [Google Scholar]
- 22.Grady WR, Klepinger DH, Nelson-Wally A. Contraceptive characteristics: the perceptions and priorities of men and women. Fam Plann Perspect. 1999;31:168–175. [PubMed] [Google Scholar]
- 23.United Nations, Department of Economic and Social Affairs, Population Division. [cited 5/3/2011];World contraceptive use. 2009 Available from http://www.un.org/esa/population/publications/WCU2009/Main.html. [Google Scholar]
- 24.Trussell J. Contraceptive efficacy. In: Hatcher RA, Trussell J, Nelson AL, Cates W, Stewart FH, Kowal D, editors. Contraceptive technology: nineteenth revised edition. New York, NY: Ardent Media; 2007. [cited 1/5/2011]. Available from http://www.contraceptivetechnology.org/table.html. [Google Scholar]
- 25.Henshaw S. Unintended pregnancy in the United States. Fam Plann Perspect. 1998;30:24–29. 46. [PubMed] [Google Scholar]
- 26.Eisenberg D, Stika C, Desai A, Baker D, Yost K. Providing contraception for women taking potentially teratogenic medications: a survey of internal medicine physicians’ knowledge, attitudes and barriers. J Gen Intern Med. 2010;25:291–297. doi: 10.1007/s11606-009-1215-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Harper CC, Blum M, de Bocanegra HT, et al. Challenges in translating evidence to practice: the provision of intrauterine contraception. Obstet Gynecol. 2008;111:1359–1369. doi: 10.1097/AOG.0b013e318173fd83. [DOI] [PubMed] [Google Scholar]
- 28.Madden T, Allsworth JE, Hladky KJ, Secura GM, Peipert JF. Intrauterine contraception in Saint Louis: a survey of obstetrician and gynecologists’ knowledge and attitudes. Contraception. 2010;81:112–116. doi: 10.1016/j.contraception.2009.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rubin SE, Fletcher J, Stein T, Segall-Gutierrez P, Gold M. Determinants of intrauterine contraception provision among US family physicians: a national survey of knowledge, attitudes and practice. Contraception. 2011;83:472–478. doi: 10.1016/j.contraception.2010.10.003. [DOI] [PubMed] [Google Scholar]
- 30.Kost K, Singh S, Vaughan B, Trussell J, Bankole A. Estimates of contraceptive failure from the 2002 National Survey of Family Growth. Contraception. 2008;77:10–21. doi: 10.1016/j.contraception.2007.09.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Asch S, Connor SE, Hamilton EG, Fox SA. Problems in recruiting community-based physicians for health services research. J Gen Intern Med. 2000;15:591–599. doi: 10.1046/j.1525-1497.2000.02329.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Fricker RD, Schonlau M. Advantages and disadvantages of Internet research surveys: evidence from the literature. Field Method. 2002;14:347–367. [Google Scholar]
- 33.Hamilton MB. Online survey response rates and times: background and guidance for industry. [cited 2011 5/3/2011];2003 Available from http://www.supersurvey.com/whitepapers.htm.