One of today's overwhelming health concerns is obesity and related illnesses, such as diabetes mellitus, high blood pressure, and cardiovascular disease. The number of affected individuals has steadily increased over the last several decades, to the point that more than a third of the United States population is now obese. Furthermore, obesity in adolescents is worrisome, because the current incidence in children is 20%, increased from 5% in 1980.1 Although a multitude of risk factors, such as genetic predisposition, lead to obesity, the recent and significant rise is definitively linked to increased caloric intake, coupled with an overall decrease in physical activity. The surplus of calories is stored as fat, either in peripheral adipose tissue, or within the abdomen, muscle, and liver. A potential consequence is the development of metabolic syndrome, which includes diabetes mellitus, hypertension, hyperlipidemia, and fatty liver. Together, obesity and these related diseases significantly increase the risk of cardiovascular disease and reduce life expectancy.
Substantial weight loss is the definitive treatment for metabolic syndrome. However, the means by which this is achieved can be difficult. Diet programs can be effective, but they are usually temporary and their effects indurable. Furthermore, it is extremely difficult to lose large amounts of weight (>100 lb) by these conservative measures.2 Medications have proved to be ineffective for substantial weight loss and can pose health threats. The best chance for success, then, involves a lifestyle change: small portions, healthful food choices, and an active lifestyle. But what is the best way to accomplish this?
Bariatric surgery offers the most effective and durable outcome. The most commonly performed bariatric procedures are Roux-en-Y gastric bypass, sleeve gastrectomy, and adjustable gastric banding (Fig. 1). The Roux-en-Y gastric bypass involves the creation of a small gastric pouch and intestinal rerouting. The sleeve gastrectomy is performed by removing 75% of the stomach. The adjustable gastric band is a silicone ring placed around the stomach that acts by limiting the amount of food that can be consumed.
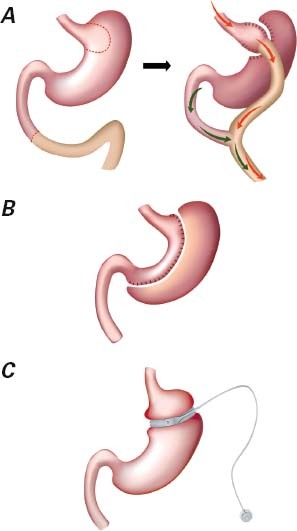
Fig. 1 Commonly performed bariatric surgery operations: A) Roux-en-Y gastric bypass, B) sleeve gastrectomy, and C) adjustable gastric banding.
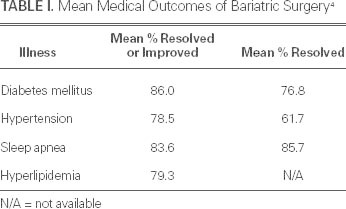
A multitude of scientific studies have confirmed that bariatric surgery is the most effective tool available to lose weight and to maintain the loss, thereby improving health and life expectancy. In one study, bariatric surgery was shown to reduce the relative risk of death in morbidly obese individuals by 89%.3 Bariatric surgery patients in that study not only lived longer, but had significantly fewer admissions to the hospital and better overall health, when compared with their cohorts who had not undergone bariatric surgery. Furthermore, bariatric surgery has been shown to be extremely effective at improving and possibly resolving obesity-related illnesses, such as diabetes, hypertension, sleep apnea, and hyperlipidemia (Table I).4
TABLE I. Mean Medical Outcomes of Bariatric Surgery4
Yet all bariatric surgeries are not created equal. The gold standard is the Roux-en-Y gastric bypass, which yields an average loss of 70% of excess weight. The sleeve gastrectomy yields an average loss of about 60% of excess weight. The gastric band is least effective and carries a high long-term failure rate. Current research indicates that the effectiveness of the type of bariatric surgery is linked not only to volume restriction, but, even more so, to the metabolic effect. The Roux-en-Y gastric bypass and sleeve gastrectomy have been shown to have significantly greater metabolic effects than the adjustable gastric band. For instance, the blood sugar level might return to normal in diabetic patients who have undergone a Roux-en-Y gastric bypass, before a substantial weight loss has taken place. The impact on diabetes improvement was shown in the STAMPEDE trial, in which 37% of sleeve gastrectomy and 42% of Roux-en-Y gastric bypass patients achieved normal HbA1c test results within one year of their surgeries.5
Bariatric surgery has become recognized as the most effective weapon in the fight against obesity and metabolic syndrome. When used to effect a lifelong lifestyle change, patients can expect a substantial, durable weight loss and a longer, healthier life.
Footnotes
Address for reprints: Vadim Sherman, MD, FACS, 6550 Fannin St., SM1661, Houston, TX 77030
E-mail: vsherman@tmhs.org
References
- 1.Ogden CL, Carroll MD, Curtin LR, Lamb MM, Flegal KM. Prevalence of high body mass index in US children and adolescents, 2007–2008. JAMA 2010;303(3):242–9. [DOI] [PubMed]
- 2.Treatment of obesity in adults. Council on Scientific Affairs. JAMA 1988;260(17):2547–51. [PubMed]
- 3.Christou NV, Sampalis JS, Liberman M, Look D, Auger S, McLean AP, MacLean LD. Surgery decreases long-term mortality, morbidity, and health care use in morbidly obese patients. Ann Surg 2004;240(3):416–24. [DOI] [PMC free article] [PubMed]
- 4.Buchwald H, Avidor Y, Braunwald E, Jensen MD, Pories W, Fahrbach K, Schoelles K. Bariatric surgery: a systematic review and meta-analysis [published erratum appears in JAMA 2005;293(14):1728]. JAMA 2004;292(14):1724–37. [DOI] [PubMed]
- 5.Schauer PR, Kashyap SR, Wolski K, Brethauer SA, Kirwan JP, Pothier CE, et al. Bariatric surgery versus intensive medical therapy in obese patients with diabetes. N Engl J Med 2012; 366(17):1567–76. [DOI] [PMC free article] [PubMed]


