Cardiovascular disease (CVD) remains the leading cause of death among women in the United States. In 2008, more than 400,000 women died of CVD.1 The increased risk of CVD from established modifiable risk factors—tobacco use, hypertension, diabetes mellitus, and hypercholesterolemia—is well documented.2 More recently, nonestablished behavioral and lifestyle risk factors—like obesity, physical inactivity, and sedentary behavior—have been studied. Understanding the crucial role that weight and daily activity play in CVD risk can greatly influence the counseling advice and recommendations that clinicians give their patients.
Obesity, Physical Activity, and Cardiovascular Disease Risk
In 2011, obesity affected 27% of all women in the United States.3 Of note, marked disparities in the prevalence of obesity exist across racial and ethnic groups: 33% of white women, 46% of Hispanic-American women, and 54% of black women.4 Obesity increases the risk for diabetes, hypertension, and hyperlipidemia. However, obesity should not simply be considered the “risk factor's risk factor.” During the last few years, evidence suggests that obesity independently increases the risk of CVD in women even in the absence of other metabolic abnormalities.5 Figure 1 shows that increasing weight alone can increase the risk of coronary heart disease.
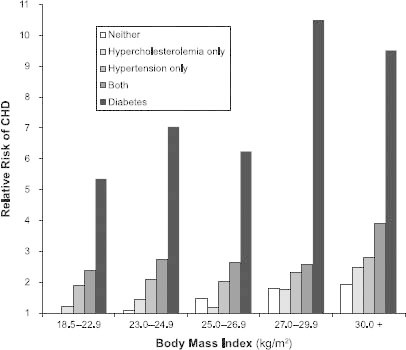
Fig. 1 Relative risk of congestive heart disease (CHD) among women by body mass index, hypercholesterolemia, hypertension, both, or diabetes. From the Nurses' Health Study. Reproduced with permission from Nature Publishing Group.5
Adjusted for age, family history of myocardial infarction, smoking, height, marital status, profession, intake of alcohol, saturated fat, polyunsaturated fat, trans fat, folate, vitamin E, and total energy.
Similarly, the effects of physical activity are now also known to independently influence CVD risk in women. Thirty minutes of moderate physical activity are recommended on most days of the week; however, as few as 75 minutes of activity each week—which equates to about 11 minutes a day for 7 days—can reduce cardiovascular risk by 14%.6 Notably, there is evidence that this protective effect might be more pronounced in women than in men.
Sedentary Behavior and Cardiovascular Disease Risk
New in the conversation regarding lifestyle factors that influence CVD risk is sedentary behavior. Contrary to popular perception, being sedentary is not simply the low end of the physical-activity spectrum. Evidence is now mounting that the negative effects of sitting for long periods of time are not greatly mitigated by meeting weekly exercise recommendations. The top graphs in Figure 2 show that the hazard ratio for death is lower for someone who rarely sits during the day and does not “exercise” in the established sense than it is for someone who meets exercise requirements but sits for long periods of time.7
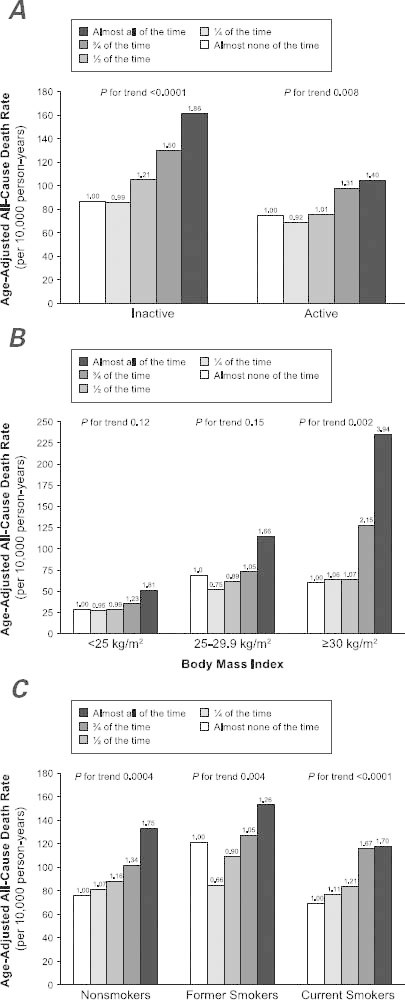
Fig. 2 Age-adjusted all-cause death rates across categories of daily sitting time in subgroups defined by A) leisure-time physical activity (active defined as ≥7.5 METċhrċwk−1), B) body mass index (BMI), and C) smoking status in 17,013 men and women from the Canada Fitness Survey, 1981–1993. The height of the bars indicates the mortality rates, and the numbers atop the bars are the hazard ratios from the proportional hazards regression. The sample size for body mass index was 10,477.
Reproduced with permission from Wolters Kluwer Health (Katzmarzyk Medicine & Science in Sports & Exercise, 2009).7
Television viewing appears to be a particularly unhealthful sedentary behavior. Women who sit and watch television for longer than 40 hours a week have a 94% increased risk of developing obesity and a 70% increased risk of developing diabetes.8 Both these conditions are well established as risk factors for CVD in women. In addition, evidence shows that all-cause mortality rates, and CVD mortality rates in particular, are negatively influenced by time spent sitting. Survival rates among individuals “sitting none of the time” are better than those for individuals “sitting all of the time.”7 In addition, sex differences appear to exist regarding the negative impact of sedentary time: women undergo greater associated risk of CVD death than do men for any given amount of time sitting.
The physiologic consequences of sedentary behavior that might explain increased mortality rates are only just recently being explored. A few early studies link sedentary behavior with increased adipocyte inflammation,9 increased triglyceride levels, insulin insensitivity, and glucose intolerance.10 These biometric changes begin to shed light on how uninterrupted sitting has detrimental effects on the health of women. On the positive side, small studies suggest that brief interruptions of sitting time may overcome some of the negative metabolic effects of sitting.11
Clinical Implications
In addition to their management of established, modifiable CVD risk factors, strong evidence supports patients in achieving a 7% weight loss and engaging in physical activity for up to 150 min/week.12 Free online resources (http://www.bsc.gwu.edu/dpp/lifestyle/dpp_part.html) and community-led programs (http://www.ymca.net/diabetes-prevention) can aid patients in achieving these goals, in conjunction with a provider's support and encouragement. In contrast, there are no evidence-based guidelines on how to counsel patients about the negative effects of sitting and how to change their behavior in that regard. Nonetheless, now that we have evidence of the detrimental effects of prolonged sitting, it is important that providers discuss this risk factor with patients. Simple suggestions such as asking patients to stand up from their desk or couch every 30 to 60 minutes to stretch or walk around might be enough to offset the risks associated with the present-day sedentary lifestyle.
The new CVD risk-reduction toolbox is getting bigger as research continues. Clinicians now have a variety of ways to empower patients to lower their risk of CVD. Providers should continue to encourage their patients to stop smoking, control blood pressure, control blood sugar, and control cholesterol. In addition, they should promote the maintenance of a healthful weight or a 7% weight loss, participation in regular physical activity (10–30 min at least 5 d/wk), and avoidance of prolonged sitting-time.
Footnotes
Address for reprints: Ann Smith Barnes, MD, MPH, Department of Medicine, Baylor College of Medicine, One Baylor Plaza, MS 285, Houston, TX 77030
E-mail: smith@bcm.edu
References
- 1.American Heart Association and American Stroke Association. Women and cardiovascular disease. Statistical fact sheet 2012 update.
- 2.Romero CX, Romero TE, Shlay JC, Ogden LG, Dabelea D. Changing trends in the prevalence and disparities of obesity and other cardiovascular disease risk factors in three racial/ethnic groups of USA adults. Adv Prev Med 2012;2012:172423. [DOI] [PMC free article] [PubMed]
- 3.Centers for Disease Control: Office of Surveillance, Epidemiology, and Laboratory Services. Behavioral risk factor surveillance system 2011. Prevalence and trends data. Overweight and obesity (BMI).
- 4.U.S. Department of Health and Human Services, National Center for Health Statistics. Health, United States, 2011: with special feature on socioeconomic status and health. DHHS Publication No. 2012–1232. [PubMed]
- 5.Flint AJ, Hu FB, Glynn RJ, Caspard H, Manson JE, Willett WC, Rimm EB. Excess weight and the risk of incident coronary heart disease among men and women. Obesity (Silver Spring) 2010;18(2):377–83. [DOI] [PMC free article] [PubMed]
- 6.Sattelmair J, Pertman J, Ding EL, Kohl HW 3rd, Haskell W, Lee IM. Dose response between physical activity and risk of coronary heart disease: a meta-analysis. Circulation 2011;124 (7):789–95. [DOI] [PMC free article] [PubMed]
- 7.Katzmarzyk PT, Church TS, Craig CL, Bouchard C. Sitting time and mortality from all causes, cardiovascular disease, and cancer. Med Sci Sports Exerc 2009;41(5):998–1005. [DOI] [PubMed]
- 8.Hu FB, Li TY, Colditz GA, Willett WC, Manson JE. Television watching and other sedentary behaviors in relation to risk of obesity and type 2 diabetes mellitus in women. JAMA 2003;289(14):1785–91. [DOI] [PubMed]
- 9.Allison MA, Jensky NE, Marshall SJ, Bertoni AG, Cushman M. Sedentary behavior and adiposity-associated inflammation: the Multi-Ethnic Study of Atherosclerosis. Am J Prev Med 2012;42(1):8–13. [DOI] [PMC free article] [PubMed]
- 10.Saunders TJ, Larouche R, Colley RC, Tremblay MS. Acute sedentary behaviour and markers of cardiometabolic risk: a systematic review of intervention studies. J Nutr Metab 2012; 2012:712435. [DOI] [PMC free article] [PubMed]
- 11.Dunstan DW, Kingwell BA, Larsen R, Healy GN, Cerin E, Hamilton MT, et al. Breaking up prolonged sitting reduces postprandial glucose and insulin responses. Diabetes Care 2012;35(5):976–83. [DOI] [PMC free article] [PubMed]
- 12.Knowler WC, Barrett-Connor E, Fowler SE, Hamman RF, Lachin JM, Walker EA, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med 2002;346(6):393–403. [DOI] [PMC free article] [PubMed]


