Abstract
Biventricular takotsubo cardiomyopathy is associated with more hemodynamic instability than is isolated left ventricular takotsubo cardiomyopathy; medical management is more invasive and the course of hospitalization is longer.
In March 2011, a 62-year-old woman presented at our emergency department with abdominal pain, nausea, and vomiting. On hospital day 2, she experienced chest pain. An electrocardiogram and cardiac enzyme levels suggested an acute myocardial infarction. She underwent cardiac angiography and was found to have severe left ventricular systolic dysfunction involving the mid and apical segments, which resulted in a left ventricular ejection fraction of 0.10 to 0.15 in the absence of obstructive coronary artery disease. Her hospital course was complicated by cardiogenic shock that required hemodynamic support with an intra-aortic balloon pump and dobutamine. A transthoracic echocardiogram revealed akinesis of the mid-to-distal segments of the left ventricle and mid-to-apical dyskinesis of the right ventricular free wall characteristic of biventricular takotsubo cardiomyopathy. After several days of medical management, the patient was discharged from the hospital in stable condition.
To the best of our knowledge, this is the first review of the literature on biventricular takotsubo cardiomyopathy that compares its hemodynamic instability and medical management requirements with those of isolated left ventricular takotsubo cardiomyopathy. Herein, we discuss the case of our patient, review the pertinent medical literature, and convey the prevalence and importance of right ventricular involvement in patients with takotsubo cardiomyopathy.
Key words: Cardiomyopathies/radiography; hemodynamic instability/takotsubo; magnetic resonance angiography; takotsubo cardiomyopathy, biventricular/diagnosis; transient apical ballooning syndrome; ventricular dysfunction, left; ventricular dysfunction, right
WEBSITE FEATURE
Transient left ventricular apical ballooning syndrome (TLVABS) is an acute cardiac syndrome that typically is characterized by transient left ventricular (LV) wall-motion abnormalities, electrocardiographic (ECG) findings of ST-T segment changes, and minimal release of cardiac enzymes in the absence of significant stenosis of the coronary arteries (<50% luminal stenosis).1–8 This syndrome was first described in Japan in 1991 and named takotsubo-like LV dysfunction in reference to the asynergy, which consists of hypokinesis or akinesis of the mid-to-apical LV and hyperkinesis of the basal LV extending over more than one coronary artery region.8–11 Since then, this asynergy has been called takotsubo cardiomyopathy (TC), stress cardiomyopathy, ampulla syndrome, broken-heart syndrome, and neurogenic stunned myocardium.12–14 Takotsubo cardiomyopathy presents clinically with chest pain and dyspnea associated with ECG changes, thereby mimicking ST-segment elevation myocardial infarction that is often preceded by emotional or physical stress.1-7,9,10 Indeed ST-segment elevation is the most common ECG abnormality, reported in approximately 82% of patients with TC, followed by T-wave inversion in 64%.8,15 This peculiar cardiac syndrome results in severe impairment of systolic function.
There are several variants of TC. Isolated LV involvement is the most common variant, but right ventricular (RV) involvement is gaining increased recognition. Although there is only one documented case of isolated RV stress cardiomyopathy,16 the recognition of biventricular TC is increasing. It has been reported that RV involvement affects approximately 25% to 42% of patients diagnosed with TC.12,13,17,18 In addition to isolated LV, isolated RV, and biventricular involvement, a variety of ballooning patterns has been observed. The typical apical-ballooning shape, with akinesis of the apical and mid-ventricular LV segments, is the most common; however, a mid-ventricular variant with apical sparing and a variant with isolated basal ballooning have been recognized.18
Left ventricular systolic dysfunction and heart failure—with simultaneous RV dysfunction—identifies a patient population with an extremely poor prognosis.19 Therefore, it is not surprising that TC with RV involvement appears to be associated with more severe LV dysfunction that results in significantly longer hospitalization and hemodynamic instability that is associated with a worse prognosis.1-4,13,18 Clinicians need to be aware of the prevalence and complications of RV involvement and dysfunction, because it can affect patient management, morbidity, and, ultimately, mortality rates in substantial ways.
The data concerning RV involvement in TC are sparse, because they are derived from several case reports and case series studies. This review of the literature documents the prevalence, pathophysiology, diagnostic imaging characteristics, clinical findings, management, and prognosis of patients with biventricular TC. Throughout this article, TC with RV involvement will be referred to as biventricular TC, whereas classic left ventricular TC (with apical ballooning) will be referred to as TLVABS. All of the documented cases of biventricular TC have been evaluated and analyzed in regard to how the patient presented, how the TC was diagnosed and managed, and how we can improve in managing the even more hemodynamically unstable biventricular TC, in comparison with TLVABS.
Case Report
In March 2011, a 62-year-old woman presented at our emergency department with one week's duration of abdominal pain, nausea, vomiting, and diarrhea. Three weeks before, she had undergone a kidney biopsy, which showed thin basement membrane disease. The patient's vital signs were stable upon presentation.
During hospital day 2, she experienced chest pain, T-wave inversion in leads V2 through V6, and elevated levels of troponin I (3.84 ng/mL) and creatine kinase–MB (11.3 ng/mL). The patient underwent cardiac catheterization for a suspected acute myocardial infarction. During angiography, the coronary arteries were seen to be absent of significant luminal stenosis. A left ventriculogram showed akinesis of the mid-to-apical LV segments, hyperkinesis of the basal segments, and an LV ejection fraction (LVEF) of 0.10 to 0.15 (Fig. 1). The patient went into cardiogenic shock that necessitated hemodynamic support with dobutamine and an intra-aortic balloon pump (IABP).

Fig. 1 Left ventriculogram shows akinesis of the mid-to-apical left ventricular segments with hyperkinesis of the basal segments at end-systole.
Real-time motion image is available at www.texasheart.org/journal.
A transthoracic echocardiogram showed severe LV systolic dysfunction (LVEF, 0.15), with akinesis of the mid-to-distal segments of the LV, along with mid-to-apical dyskinesis of the RV free wall suggestive of biventricular TC (Fig. 2). Grade 3 mitral valve insufficiency was also noted.

Fig. 2 Two-dimensional echocardiogram (subcostal view) shows mid-to-apical ballooning of the right and left ventricles at end-systole.
Real-time motion image is available at www.texasheart.org/journal.
The patient was medically managed (standard therapy) for heart failure with severe LV systolic dysfunction. After 9 days, she was discharged from the hospital in stable condition. Her cardiac medications at discharge included simvastatin, aspirin, furosemide, lisinopril, and metoprolol.
A follow-up transthoracic echocardiogram at 5 weeks showed complete resolution of the LV systolic dysfunction and the RV wall-motion abnormalities. The LVEF was 0.50 to 0.55 upon follow-up (Fig. 3). Once LV systolic dysfunction resolved, heart-failure medications were discontinued. Aspirin and simvastatin were continued to treat nonobstructive coronary artery disease.

Fig. 3 Two-dimensional echocardiogram (4-chamber apical view) at 5-week follow-up shows complete resolution of the left and right ventricular systolic dysfunction at end-systole.
Real-time motion image is available at www.texasheart.org/journal.
Literature Review
Methods
We performed a careful electronic search of the English-language literature, cross-referencing published studies and identifying 10 that pertained to biventricular TC. Two of the articles, by Haghi and colleagues12 and Elesber and associates,13 compared multiple patients with TLVABS to those with biventricular TC who had presented to their institutions over a period of time. There has been one documented case of isolated right ventricular stress cardiomyopathy.16
All case studies were retrospective. Each study reported results on 1 to 9 patients. This review of biventricular TC encompasses 25 documented cases of patients with biventricular TC, our report of 1 additional case of biventricular TC, and 1 report of an isolated RV case.
Results
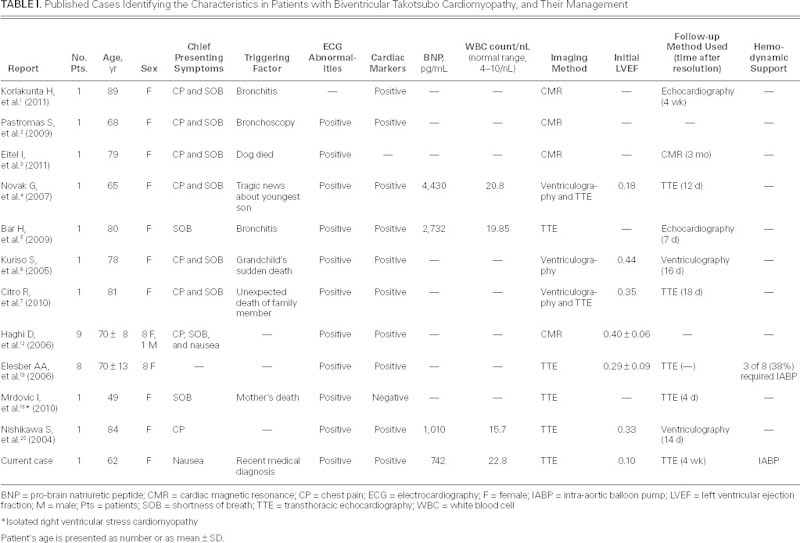
The main characteristics of the 26 cases of biventricular TC and the 1 case of isolated RV stress cardiomyopathy included in this review are summarized in Table I.1–7,12,13,16,20
TABLE I. Published Cases Identifying the Characteristics in Patients with Biventricular Takotsubo Cardiomyopathy, and Their Management
Several studies8,17,18,21 have reported that TC accounts for approximately 2% of all ST-segment-elevation acute coronary syndromes. Furthermore, several reports12,13,17,18 have concluded that the RV is involved in roughly 25% to 42% of all TC presentations.
In evaluating transient RV involvement and associated dysfunction by means of conventional echocardiography, Elesber and associates13 showed that 8 of 25 patients (32%) had biventricular involvement. These clinicians evaluated the hemodynamic impact of RV involvement by comparing patients with biventricular TC to those with TLVABS. There was no statistical difference between the 2 groups regarding age, coronary artery risk factors, discharge cardiac medications, presentation, ECG findings, cardiac catheterization findings, and maximal troponin release. However, patients with biventricular TC had significant reduction in LVEF (0.29 vs 0.42), were hospitalized 4 days longer (11 vs 7 d) on average, presented with notably increased tricuspid regurgitation velocity, and had an increased complication rate in comparison with TLVABS patients (but not at follow-up). Seven patients (88%) with RV involvement had severe congestive heart disease or required IABP placement, intubation, or cardiopulmonary resuscitation (CPR), compared with 2 patients (12%) with no RV involvement. Furthermore, the study showed that only when the RV is involved is there an association with IABP use, intubation, and CPR, all of which suggests greater hemodynamic instability. Similarly, there were 2 deaths (25%) associated with RV involvement, compared with only 1 death (5.8%) associated with TLVABS.
Using cardiac magnetic resonance (CMR) to detect RV involvement, Haghi and colleagues12 showed that 9 of 34 cases of TC (26%) had biventricular apical ballooning. They also found that 6 patients (67%) with RV involvement had pleural effusions, compared with 2 patients (8%) without RV involvement. However, bilateral (44%) or noteworthy (22%) pleural effusions did not occur unless both ventricles showed abnormal wall movements. It is postulated that as LV function declines, pulmonary venous pressure increases, which can result in leakage of fluid from the visceral pleural surface. In addition, patients with RV dysfunction also experience an increase in systemic venous pressure, which increases the filtration of fluid from parietal capillaries and simultaneously decreases lymphatic flow from the pleural cavity, resulting in an even more pronounced accumulation of fluid in the pleural cavity.22
Eitel and co-authors17 also stated that significant bilateral pleural effusion was evident only when the RV was involved, which suggests that pleural effusion in TC is a reliable indicator of RV involvement, as we have mentioned.
Polak and coworkers23 conducted a series of studies to determine how RV dysfunction affects LV systolic function. They found that depressed RV function was linked to more severely compromised LV function, as confirmed by a greater reduction in LVEF and by an increase of LV dyskinesia. Moreover, these patients had a greater prevalence of chronic obstructive pulmonary disease, increased pulmonary capillary wedge pressure, and significant increases in both indices of RV overload (pulmonary artery pressure and pulmonary vascular resistance). In conclusion, depressed RV ejection fraction is an indicator of increased morbidity and mortality rates among patients who have chronic congestive heart failure secondary to atherosclerotic heart disease.
Hemodynamics
Takotsubo cardiomyopathy with RV involvement is associated with more severe systolic dysfunction, congestive heart failure, the need for IABP and CPR, more in-hospital complications, and pleural effusions.1,2,4,12,13,17 Therefore, it is of great importance to note the treatment requirements and regimens that have been documented in patients with biventricular TC; unfortunately, very few case studies provide such documentation. Elesber and associates13 stated that 6 of 8 patients (75%) with RV involvement had severe congestive heart failure, 5 required intubation (63%), 3 required IABP (38%), and 1 required CPR (13%).
Mrdovic and colleagues16 documented the first and only reported case of isolated right ventricular TC, but no hemodynamic requirements or treatment regimens were discussed within the case report.
Gianni and colleagues8 described the different presenting clinical findings, complications, treatments, and outcomes of 14 different case-review articles (covering 286 cases) on TC. They noted that only 8 of these articles specified the treatment in the acute phase and that very few reported the ongoing medical regimen. However, they did document that in the 14 articles, cardiogenic shock was a serious clinical presentation in 4.2% of cases, and that 23 of the 212 patients (10.8%) were treated with intra-aortic balloon counterpulsation. Unfortunately, within the 14 case-review articles analyzed, we do not know which cases, if any, involved the RV. However, on the basis of our knowledge of the current literature, we believe it probable that those requiring IABP and other more serious interventions had RV involvement complicating medical management.
Similarly, when members of the Angina Pectoris-Myocardial Infarction (AP-MI) investigations11 in Japan retrospectively registered and analyzed patients with TLVABS, they concluded that out of 88 patients with characteristics of TLVABS, 13 (15%) experienced cardiogenic shock, 7 (8%) required IABP, and 17 (19%) required dopamine or dobutamine; there was 1 sudden death. However, because we do not know which, if any, cases involved the RV, we cannot compare TLVABS with biventricular TC in regard to hemodynamic differences.
Although they are excellent sources of information regarding TC, Gianni and colleagues8 and the AP-MI investigations11 in Japan further illustrate the under-recognition of RV involvement in patients diagnosed with TC and the need to document that involvement more thoroughly. It is of interest that these 2 studies, in common with most previous studies of TC, depended upon either echocardiography or left ventriculography to identify patients with TC, thereby under-recognizing RV involvement. As CMR is used more widely throughout the world, RV involvement in patients with TC is gaining recognition.
Eitel and co-authors18 performed a prospective study at 7 tertiary care centers in Europe and North America, using CMR to define the exact prevalence and clinical spectrum of TC in a large population. Their findings are consistent with previously mentioned studies insofar as RV involvement occurs in 34% of patients with TC. They concluded that biventricular TC resulted in a significantly lower LVEF (0.43) than that in patients without RV involvement (0.48); and patients with biventricular TC tended to be older (73.4 vs 66.5 yr), to have significantly more stressful events preceding presentation (86% vs 65%), and to experience longer hospitalizations (7 vs 5 d). In addition, pleural effusions were more common in patients with biventricular TC (62% vs 19%).
Cardiac Magnetic Resonance
Cardiac magnetic resonance has emerged as a noninvasive imaging method to accurately quantify LV and RV function, visualize regional wall-motion abnormalities, and help differentiate TC from similar causes of acute cardiac disease by evaluating markers for reversible (inflammation, ischemic edema) and irreversible (necrosis/fibrosis) injury.18,24 Previous studies that used CMR to evaluate TC considered the absence of late gadolinium enhancement (LGE) as an important finding, because it differentiates TC from acute myocardial infarction and myocarditis.13,17,18,24 The lack of delayed gadolinium enhancement suggests that the area of ballooning does not undergo irreversible damage, which might explain the complete recovery of LV and RV function in patients with TC.
Nakamori and associates24 monitored 23 patients who met certain criteria for the diagnosis of TC. Patients underwent CMR to evaluate LGE signal characteristics among patients who presented acutely with TC. Upon presentation, all patients manifested wall-motion abnormalities from the mid-ventricular to apical regions of the LV. Myocardial edema on T2-weighted magnetic resonance imaging was observed in 22 of 23 patients (96%). Late gadolinium enhancement was observed in 5 of 23 patients (22%). All instances of LGE were observed in an area that exhibited both wall-motion abnormalities and edema in a transmural distribution. In patients with TC, the contrast-to-noise ratio of these segments was significantly lower than the contrast-to-noise ratio of infarcted segments in patients with acute myocardial infarction.
At the 3-month follow-up, CMR revealed no edema on the T2-weighted magnetic resonance imaging in any of the patients of Nakamori and associates.24 All patients who had no segments showing LGE had complete recovery of wall motion. Among the 5 patients who manifested LGE in the acute phase, 2 patients showed no evidence of LGE at the 3-month follow-up. However, residual wall-motion abnormalities were observed in the remaining 3 patients; at 12-month follow-up CMR, both LGE and wall-motion abnormalities in these patients were completely resolved.24
Cardiac magnetic resonance performed by Eitel and co-authors18 found that 117 of 139 patients (84%) who presented with TC had myocardial edema with a transmural distribution. Focal or patchy LGE was seen in 21 of 139 patients (15%).
Cardiac magnetic resonance findings in TC are summarized in Table II.18,23
TABLE II. Cardiac Magnetic Resonance Characteristics at Acute Presentation and Follow-Up
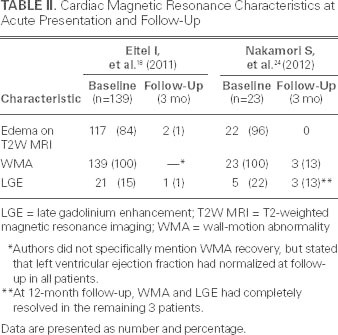
Nakamori24 and Eitel18 and their respective colleagues have been pivotal in determining the imaging diagnostic criteria and the pathophysiology for TC. Cardiac magnetic resonance that exhibits a gray myocardial signal on LGE has been found in approximately 20% of patients who present with TC. Furthermore, the presence of LGE in the acute phase of TC seems to predict prolonged recovery of wall-motion abnormalities. Although segmental LGE is seen among patients with TC, it is important to note that the signal intensity is much lower and the extent of LGE substantially smaller, when compared with acute myocardial infarction.
Conclusion
Several pathologic mechanisms have been proposed to explain the peculiar asynergy and features of TC, such as multivessel coronary vasospasm, abnormalities in coronary microvascular function, focal myocarditis, and catecholamine-mediated cardiotoxicity. Even though the exact cause and pathophysiology of TC remains unknown, there are many who believe the cause is multifactorial. Merli and associates14 suggest that other factors must also account for the asynergy of the ventricles. They suggest that an induced severe transient mid-ventricular cavity dynamic gradient—combined with a catecholamine-induced reduction in subendocardial flow—could account for the marked discrepancy between the distribution of the transient wall-motion abnormalities and the distribution of epicardial coronary artery flow.4,6,8,9,12,14,20,25
In all the cases regarding RV involvement in TC to which we refer in our review of the literature, we noted that 1) most patients with biventricular TC are elderly women; 2) presenting symptoms are similar to those of acute myocardial infarction; 3) acute ECG findings usually reveal ST-segment elevation, T-wave inversion, or both; 4) asynergy extending over more than one coronary artery region is transient and resolves within several days to weeks; and 5) RV involvement increases hemodynamic instability, increasing the risk of complications and requiring more intensive and aggressive management.
We can conclude from this review of the literature that biventricular involvement has a substantial impact on hospitalization length and hemodynamic instability, thereby affecting the patient's prognosis, morbidity, and outcome. Recognition of RV involvement in patients diagnosed with TC will better prepare physicians to treat the increased hemodynamic instability that is associated with RV involvement, potentially leading to decreased morbidity and mortality rates.
In the absence of studies that specifically document medical regimens for the treatment of biventricular TC, that treatment continues to be entirely case dependent and should be individualized in accordance with the patient's characteristics and hemodynamic requirements at the time of presentation and throughout hospitalization. The fact is that standard heart-failure therapy (aspirin, β-blockers, angiotensin-converting enzyme inhibitors/angiotensin II receptor blockers, vasodilators, and diuretics) has proved beneficial in the management of patients with stress cardiomyopathy.8,11,18,24
Limitations. Our case study and literature review has certain limitations. First, all our data are derived from retrospective research; therefore, not all information (such as laboratory values) was documented, and not all cardiac procedures were performed in a manner that would support or weaken our conclusions. Second, the lack of data on biventricular TC is probably attributable to the diagnosis of most TC cases by means of left ventriculography during cardiac catheterization; right ventriculography is seldom performed, because it increases risk and yields no particular benefit. However, CMR is becoming more common in diagnosing TC, and it has the added benefit of noninvasively visualizing the RV and providing LGE markers to determine the extent of edema and inflammation, which might help to predict recovery time. Third, we probably have not accounted for all cases of documented biventricular TC, despite our careful electronic searches and cross-referencing of published articles for RV involvement; consequently, our review draws from a small number of cases and reports. However, this present analysis is the most complete review of the available data on biventricular TC to date.
Acknowledgment
We express sincere appreciation to Darlene Frankhouser, RDCS, Technical Director of the Echocardiography Laboratory at Memorial Hospital, for her assistance in organizing and preparing the cardiac images.
Supplementary Material
Footnotes
Address for reprints: Joseph Daoko, MD, FACC, York Heart and Vascular Specialists, 1600 Sixth Ave., Suite 105, York, PA 17403
E-mail: jdaoko@mhyork.org
References
- 1.Korlakunta H, Butkevich A, Muthupillai R, Cheong BY. Biventricular takotsubo cardiomyopathy: cardiac magnetic resonance imaging as useful diagnostic tool. Tex Heart Inst J 2011;38(1):88–9. [PMC free article] [PubMed]
- 2.Pastromas S, Koulouris S, Gavaliatsis IP, Temperikidis P, Manolis AS. Tako tsubo cardiomyopathy with right ventricular involvement. Hospital Chronicles 2009;4(4):181–3.
- 3.Eitel I, Schuler G, Gutberlet M, Thiele H. Biventricular stress-induced (takotsubo) cardiomyopathy with left midventricular and right apical ballooning. Int J Cardiol 2011;151(2):e63–4. [DOI] [PubMed]
- 4.Novak G, Kross K, Follmer K, Brofferio A, Shirani J. Transient biventricular apical ballooning: a unique presentation of the “broken heart”. Clin Cardiol 2007;30(7):355–8. [DOI] [PMC free article] [PubMed]
- 5.Bar H, Katus HA, Mereles D. Biventricular involvement in transient apical ballooning syndrome. Int J Cardiol 2009;133 (2):e79–80. [DOI] [PubMed]
- 6.Kurisu S, Inoue I, Kawagoe T, Ishihara M, Shimatani Y, Mitsuba N, et al. Takotsubo-like transient biventricular dysfunction with pressure gradients. Intern Med 2005;44(7):727–32. [DOI] [PubMed]
- 7.Citro R, Caso I, Provenza G, Santoro M, Gregorio G, Bossone E. Right ventricular involvement and pulmonary hypertension in an elderly woman with tako-tsubo cardiomyopathy. Chest 2010;137(4):973–5. [DOI] [PubMed]
- 8.Gianni M, Dentali F, Grandi AM, Sumner G, Hiralal R, Lonn E. Apical ballooning syndrome or takotsubo cardiomyopathy: a systematic review. Eur Heart J 2006;27(13):1523–9. [DOI] [PubMed]
- 9.Kurisu S, Sato H, Kawagoe T, Ishihara M, Shimatani Y, Nishioka K, et al. Tako-tsubo-like left ventricular dysfunction with ST-segment elevation: a novel cardiac syndrome mimicking acute myocardial infarction. Am Heart J 2002;143(3):448–55. [DOI] [PubMed]
- 10.Dote K, Sato H, Tateishi H, Uchida T, Ishihara M. Myocardial stunning due to simultaneous multivessel coronary spasms: a review of 5 cases [in Japanese]. J Cardiol 1991;21(2):203–14. [PubMed]
- 11.Tsuchihashi K, Ueshima K, Uchida T, Oh-mura N, Kimura K, Owa M, et al. Transient left ventricular apical ballooning without coronary artery stenosis: a novel heart syndrome mimicking acute myocardial infarction. Angina Pectoris-Myocardial Infarction Investigations in Japan. J Am Coll Cardiol 2001;38(1):11–8. [DOI] [PubMed]
- 12.Haghi D, Athanasiadis A, Papavassiliu T, Suselbeck T, Fluechter S, Mahrholdt H, et al. Right ventricular involvement in takotsubo cardiomyopathy. Eur Heart J 2006;27(20):2433–9. [DOI] [PubMed]
- 13.Elesber AA, Prasad A, Bybee KA, Valeti U, Motiei A, Lerman A, et al. Transient cardiac apical ballooning syndrome: prevalence and clinical implications of right ventricular involvement. J Am Coll Cardiol 2006;47(5):1082–3. [DOI] [PubMed]
- 14.Merli E, Sutcliffe S, Gori M, Sutherland GG. Tako-tsubo cardiomyopathy: new insights into the possible underlying pathophysiology. Eur J Echocardiogr 2006;7(1):53–61. [DOI] [PubMed]
- 15.Qaqa A, Daoko J, Jallad N, Aburomeh O, Goldfarb I, Shamoon F. Takotsubo syndrome in African American vs. non-African American women. West J Emerg Med 2011;12(2): 218–23. [PMC free article] [PubMed]
- 16.Mrdovic I, Kostic J, Perunicic J, Asanin M, Vasiljevic Z, Ostojic M. Right ventricular takotsubo cardiomyopathy. J Am Coll Cardiol 2010;55(16):1751. [DOI] [PubMed]
- 17.Eitel I, Behrendt F, Schindler K, Kivelitz D, Gutberlet M, Schuler G, Thiele H. Differential diagnosis of suspected apical ballooning syndrome using contrast-enhanced magnetic resonance imaging. Eur Heart J 2008;29(21):2651–9. [DOI] [PubMed]
- 18.Eitel I, von Knobelsdorff-Brenkenhoff F, Bernhardt P, Carbone I, Muellerleile K, Aldrovandi A, et al. Clinical characteristics and cardiovascular magnetic resonance findings in stress (takotsubo) cardiomyopathy. JAMA 2011;306(3):277–86. [DOI] [PubMed]
- 19.Toldo S, Bogaard HJ, Van Tassell BW, Mezzaroma E, Seropian IM, Robati R, et al. Right ventricular dysfunction following acute myocardial infarction in the absence of pulmonary hypertension in the mouse. PLoS One 2011;6(3):e18102. [DOI] [PMC free article] [PubMed]
- 20.Nishikawa S, Ito K, Adachi Y, Katoh S, Azuma A, Matsubara H. Ampulla (‘takotsubo’) cardiomyopathy of both ventricles: evaluation of microcirculation disturbance using 99mTc-tetrofosmin myocardial single photon emission computed tomography and Doppler guide wire. Circ J 2004;68(11):1076–80. [DOI] [PubMed]
- 21.Bybee KA, Prasad A, Barsness GW, Lerman A, Jaffe AS, Murphy JG, et al. Clinical characteristics and thrombolysis in myocardial infarction frame counts in women with transient left ventricular apical ballooning syndrome. Am J Cardiol 2004;94(3):343–6. [DOI] [PubMed]
- 22.Kinasewitz GT. Transudative effusions. Eur Respir J 1997;10 (3):714–8. [PubMed]
- 23.Polak JF, Holman BL, Wynne J, Colucci WS. Right ventricular ejection fraction: an indicator of increased mortality in patients with congestive heart failure associated with coronary artery disease. J Am Coll Cardiol 1983;2(2):217–24. [DOI] [PubMed]
- 24.Nakamori S, Matsuoka K, Onishi K, Kurita T, Ichikawa Y, Nakajima H, et al. Prevalence and signal characteristics of late gadolinium enhancement on contrast-enhanced magnetic resonance imaging in patients with takotsubo cardiomyopathy. Circ J 2012;76(4):914–21. [DOI] [PubMed]
- 25.Wittstein IS, Thiemann DR, Lima JA, Baughman KL, Schulman SP, Gerstenblith G, et al. Neurohumoral features of myocardial stunning due to sudden emotional stress. N Engl J Med 2005;352(6):539–48. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


