Abstract
The concurrent and predictive validity of 2 different methods of Millon Clinical Multiaxial Inventory–III subtyping (protocol sorting, cluster analysis) was evaluated in 125 recently detoxified opioid-dependent outpatients in a 12-week randomized clinical trial. Participants received naltrexone and relapse prevention group counseling and were assigned to 1 of 3 intervention conditions: (a) no-incentive vouchers, (b) incentive vouchers alone, or (c) incentive vouchers plus relationship counseling. Affective disturbance was the most common Axis I protocol-sorted subtype (66%), antisocial–narcissistic was the most common Axis II subtype (46%), and cluster analysis suggested that a 2-cluster solution (high vs. low psychiatric severity) was optimal. Predictive validity analyses indicated less symptom improvement for the higher problem subtypes, and patient treatment matching analyses indicated that some subtypes had better outcomes in the no-incentive voucher conditions.
Addiction subtyping research has identified constellations of personality dimensions (Barnes, Murray, Patton, Bentler, & Anderson, 2000) and psychiatric disorders (Kranzler & Rounsaville, 1998) that are associated with the onset and severity of substance abuse and may have relevance for predicting treatment response. The presence of co-occurring psychiatric disorders seems to indicate a need for specialized or more intensive addiction treatment, and depression, antisocial personality, and general psychiatric symptom severity have been the most commonly investigated problems. Depressed cocaine abusers benefit from cognitive–behavioral coping skills and pharmacotherapy (Carroll et al., 1994), and opiate abusers with greater psychiatric severity improve with more intensive psychosocial programs (McLellan et al., 1983). Antisocial alcohol abusers seem to have better outcomes with coping skills than with interactional approaches (Kadden, Cooney, Getter, & Litt, 1989; Longabaugh et al., 1994), although Kadden, Litt, Cooney, Kabela, and Getter (2001) failed to replicate this effect. Antisocial methadone patients do as well as (Brooner, Kidorf, King, & Stoller, 1998; Silverman et al., 1998), and perhaps better than (Messina, Farabee, & Rawson, 2003), non-antisocial patients when provided with potent behavioral incentives, individual psychotherapy (Woody, McLellan, Luborsky, & O’Brien, 1985), or enhanced psychosocial services (Cacciola, Alterman, & Rutherford, 1995; Cacciola, Rutherford, Alterman, McKay, & Snider, 1996). The current study evaluated psychopathology subtypes derived from the Millon Clinical Multiaxial Inventory–III (MCMI-III; Millon, 1994), the most recent edition of a widely used instrument that measures Axis I and II diagnoses of the fourth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM–IV; American Psychiatric Association, 1994) and is also rooted in a biopsychosocial personality theory that may be relevant to the treatments compared in this study.
MCMI Psychopathology Subtyping Procedures
The ability to prospectively assign or match types of substance abuse patients to specific treatments in clinical practice depends on the ease and reliability of subtyping based on psychopathology indicators. The first and second editions of the MCMI (see reviews by Craig & Weinberg, 1992a, 1992b) and the Minnesota Multiphasic Personality Inventory (see review by Graham & Strenger, 1988) have been the most widely used omnibus psychopathology inventories in substance abuse samples. Two methods are commonly used to identify psychopathology subtypes. Test protocols can be sorted on the basis of one or more clinical scale elevations, usually defined as two standard deviations above a reference sample average. Advantages of this criterion-based, protocol sorting approach are that it can be accomplished easily (i.e., without a knowledge of complex statistics) and evaluated across different treatment samples and settings. However, this scale-specific focus fails to account for important patterns of covariation between scales. The second approach, most often accomplished through cluster analysis, takes into account the relations among indicators and groups individuals according to their similarity or distance from each other on many scales. However, this multivariate classification strategy is a complex, sample-based approach, and decisions about cluster number and names can be subjective. Even when cluster solutions generalize across samples (Ball, 1996), the definition of decision rules to identify subtypes a priori (e.g., cutoff scores from a subset of predictive indicators) remains complex and sample specific.
MCMI-I and MCMI-II protocol sorting procedures have most often identified depression or anxiety as the most common Axis I scale elevations, and antisocial or narcissistic as the most common Axis II scale elevations (Calsyn, Fleming, Wells, & Saxon, 1996; Craig & Olson, 1990; Craig & Weinberg, 1992a, 1992b; Marsh, Stile, Stoughton, & Trout-Landen, 1988). These primary elevations are often combined with secondary elevations on borderline, passive–aggressive, aggressive–sadistic, histrionic, and alcohol and drug abuse scales. An antisocial–narcissistic subtype is found in 36% to 60% of drug-dependent samples; withdrawn–negativistic and dependent subtypes are also common (Calsyn et al., 1996). Cluster analyses of the MCMI-I and MCMI-II generally have yielded three to six subtypes, including antisocial–narcissistic, avoidant–passive-aggressive, dependent, histrionic, high psychiatric severity, and no elevation (Bartsch & Hoffman, 1985; Craig, 1988; Craig, Bivens, & Olson, 1997; Craig & Olson, 1990; Craig, Verinis, & Wexler, 1985; Donat, 1988; Donat, Walters, & Hume, 1991; Fals-Stewart, 1992; Haller, Miles, & Dawson, 2002; Matano, Locke, & Schwartz, 1994). McMahon, Malow, and Penedo (1998) have described the four most common MCMI-I and MCMI-II clusters as antisocial–narcissistic, neurotic (anxious–depressed), high (Axis I and II) pathology, and subclinical. Although numerous studies have identified subtypes through either protocol sorting or cluster analysis, no study has compared the validity of these alternative approaches or evaluated their treatment-matching relevance in individuals with substance abuse, and very few have used the more recently developed MCMI-III.
MCMI-Derived Subtypes and Treatment Outcome
Treatment outcome studies involving the MCMI-I and MCMI-II subtypes generally have been limited to evaluations of treatment retention in different settings (Fals-Stewart, 1992; Haller et al., 2002; McMahon, Kelley, & Kouzekanani, 1993; Stark & Campbell, 1988). With regard to protocol sorting, Calsyn et al. (1996) found that withdrawn–negative and histrionic subtypes were associated with longer 18-month retention in methadone maintenance than were the other subtypes. With regard to cluster analysis, Fals-Stewart (1992) found that avoidant–schizoid and antisocial groups had shorter retention in a long-term residential therapeutic community and relapsed faster during a 1-year follow-up (see also McMahon et al., 1993). Haller et al. (2002) found that an MCMI-II cluster with elevated narcissistic, histrionic, and compulsive scales had better retention in a day treatment program for pregnant cocaine abusers than did a high-severity cluster with multiple scale elevations.
Although no studies to date have evaluated patient–treatment matching and MCMI-derived subtypes, some have speculated on the treatment implications for the more common types (Matano et al., 1994; McMahon et al., 1998). For example, an individual with a subclinical profile or a low-severity cluster might not need additional services beyond standard addiction counseling. However, a neurotic profile or high-severity cluster might benefit from specialized psychiatric care involving psychotherapy and/or medication in addition to standard counseling (see also Woody et al., 1984; Woody, McLellan, Luborsky, & O’Brien, 1995). In contrast, an antisocial–narcissistic profile or cluster has been considered a poor candidate for psychotherapy or pharmacotherapy (Matano et al., 1994).
Matching Psychopathology Subtypes to Therapeutic Components
Although combined pharmacotherapy and psychotherapy is considered the treatment of choice for many psychiatric disorders, the identification of patient variables that predict differential benefit from different combinations of interventions has been relatively unstudied. An efficient identification of patient subtypes that may derive benefit from the addition of specific behavioral therapy interventions may be a powerful strategy for improving compliance and outcome with efficacious pharmacotherapeutic interventions for substance dependence. Although naltrexone is pharmacologically one of the most potent treatments for opiate addiction, noncompliance and early attrition remain major problems limiting its effectiveness and use in clinical practice. Carroll et al. (2001) found that two contingency management conditions receiving incentive vouchers for naltrexone compliance and abstinence were associated with better retention and reduction in substance use than was a condition without contingent incentives. The addition of a relationship counseling component did not yield significant additional improvements except in the specific domain of family functioning (Carroll et al., 2001).
In a patient–treatment matching study evaluating naltrexone and relapse prevention for alcohol-dependent outpatients, Jaffe et al. (1996) emphasized the importance of articulating a clear theoretical rationale to guide predictions for which patients may benefit more or less from specific pharmacotherapies, psychotherapies, or both. In this regard, there is reason to expect that naltrexone alone or with minimal psychosocial intervention might not be an optimal treatment for antisocial, depressed, or other co-occurring psychiatric patients. Naltrexone may deprive such patients of a primary pharmacological method of symptom or distress management as well as the pleasurable and risk-taking benefits of drugs without providing substitute alternative coping behaviors, reinforcements, or social supports. Thus, the addition of behavioral therapies may help counteract some of these natural disincentives and improve outcome for some subtypes more than others.
In addition to providing a relatively efficient assessment of DSM Axis I and II diagnoses for subtyping purposes, the different MCMI versions are rooted in a comprehensive theory of personality and psychopathology (Millon, 1999; Millon & Davis, 1996) from which testable hypotheses about current behavior and treatment response can be made. Millon’s theory emphasizes three polar domains of functioning (pleasure–pain, active–passive, self–other) that define personality patterns and pathology on the basis of a person’s primary source and nature of reinforcement. These theoretical domains are relevant to the more common MCMI-derived subtypes and to the treatment conditions with which we predicted interaction. For example, one might predict that individuals with psychopathology subtypes characterized by greater sensitivity to external contingencies and relationships who look to others for help, attention, approval, reinforcement, or support (e.g., affective, dependent, histrionic, psychiatric) might show incremental benefit from the addition of incentive vouchers and relationship counseling. In contrast, psychopathology subtypes (e.g., antisocial–narcissistic, withdrawn–negativistic) characterized by insensitivity, aversion, disdain, or resistance to external reinforcement, contingencies, or expectations might not derive benefit from the contingent reinforcement provided by incentive vouchers. Because this group also devalues, avoids, disengages from, or has other impairments in prosocial relationships, they may not derive additional benefit (or conceivably do worse) when provided with relationship counseling.
Although there is some empirical support for the hypothesis that antisocial substance abusers make less than optimal use of interpersonally focused treatments (Kadden et al., 1989; Longabaugh et al., 1994), there is little evidence that they are insensitive to externally imposed contingencies. Several studies have failed to support the widespread clinical belief that antisocial personality disorder is a risk factor for poor substance abuse treatment outcome, particularly when external contingencies are provided, such as methadone dose adjustments, take-home medication, or monetary incentives (Brooner et al., 1998; Silverman et al., 1998). In fact, a recent report by Messina et al. (2003) found that antisocial opioid-dependent patients on methadone maintenance actually had better cocaine abuse outcomes than did non-antisocial patients when provided contingency management involving an incentive voucher system. The possibility that antisocial individuals with substance abuse may be responsive to external contingencies involving immediate, personal gain (monetary incentives), but not requiring cooperative work with others (as in relationship counseling or an interactional group), is at least partly consistent with Millon’s (1999) description of antisocial and narcissistic personality patterns. By comparison, depressed, anxious, or otherwise psychiatrically distressed subtypes might be expected to require significant social support or engagement with others for sustained symptom reduction. Monetary incentives also may be helpful for these types of distressed patients to the extent that they increase the anticipation of pleasure rather than pain from the environment, improve behavioral mobility, or counteract hopeless or helpless beliefs about symptom improvement. Thus, reinforcement contingencies, coping skills, and relational support may provide differential benefit to subtypes based on Millon’s biopsychosocial personality theory.
Study Predictions
Despite a substantial MCMI-I and MCMI-II literature on psychopathology subtypes of substance abuse, no studies have compared the validity of the two most common alternative subtyping strategies, evaluated their treatment matching relevance, and few have used the current, third edition version (MCMI-III). This study compared the concurrent and predictive validity of protocol sorting and cluster analysis methods in outpatients treated in a randomized clinical trial that evaluated the addition of different behavioral therapies (no-incentive vouchers; incentive vouchers alone; incentive vouchers plus relationship counseling) to improve a standard treatment (naltrexone and coping skills group) for opioid dependence.
With regard to subtyping procedures, we predicted that the protocol sorting method would yield prevalence rates approximating those found by Calsyn et al. (1996) in their methadone sample. We also predicted that we would identify approximately four clusters (e.g., antisocial–narcissistic; negative affect; withdrawn-negativistic; low severity) that have been found most commonly in prior MCMI-I and MCMI-II cluster analysis studies. Because these empirically derived clusters appear to overlap with several of the a priori protocol sorting subtypes, we did not predict that one method would necessarily have substantially greater evidence of concurrent or predictive validity. In terms of subtyping main effects, we predicted that the more severe subtypes (higher psychopathology) would have worse retention and compliance and less reduction in substance abuse and psychosocial impairment than their lower psychopathology counterparts.
We anticipated that protocol sorting and/or cluster analysis would identify sufficient numbers of antisocial, neurotic (affective disturbance), and global psychiatric subtypes to permit analysis of Patient Attribute × Treatment Condition hypotheses derived from the empirical literature and Millon’s theory (Millon & Davis, 1996). We predicted that an antisocial subtype would derive benefit from the addition of monetary incentives to standard treatment (thrice weekly naltrexone and urine tests with weekly group therapy) and would show just as much improvement as non-antisocial individuals in retention, compliance, substance use, and psychosocial indicators over 12 weeks. However, we did not predict that antisocial individuals would benefit as much as non-antisocial individuals from the addition of relationship counseling to incentive vouchers. Somewhat different hypotheses were made for the neurotic (affective disturbance) and psychiatric subtypes. Here, we predicted that the more severe subtypes would have a better outcome in the two incentive voucher conditions than in the no-incentive voucher condition and would have a better outcome with incentive vouchers plus relationship counseling than in the incentive voucher alone condition because of the added social support or services.
Method
Participants
Participants were 125 opioid-dependent individuals seeking outpatient detoxification and pharmacotherapy (naltrexone) through the Central Medical Unit of the APT Foundation in New Haven, Connecticut. All participants were clinically diagnosed as opioid dependent by an admitting physician, and this was confirmed using the Structured Clinical Interview for the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (SCID; First, Spitzer, Gibbon, & Williams, 1995) conducted by a master’s-level project director. Individuals were excluded from participating if they had significant medical conditions (especially liver dysfunction that would contraindicate naltrexone treatment), had lifetime schizophrenia or bipolar disorder, had received addiction treatment in the previous 3 months, or could not identify a significant other willing to participate in treatment. Details of the total sample screened for eligibility are provided in Carroll et al. (2001). A total of 130 participants completed the MCMI-III, five of which were judged to be invalid (see below), and so subtyping and concurrent validity analyses are reported on 125. Ten of these participants dropped out of the study prior to or after randomization; thus, predictive validity analyses were reported on 115.
Participants were predominantly single (54%; 22% married or cohabitating; 22% separated or divorced), male (74%; 26% female), Caucasian (80%; 13% African American; 6% Hispanic American), high school educated (83%) adults (mean 32.6, SD = 8.1 years). Fifty percent were unemployed, but only 16% reported receiving public assistance. Participants had substantial legal histories with a mean of 5.0 (SD = 9.1) previous arrests, although only 14% were currently on probation or parole. Half (54%) of the participants had been treated for substance abuse previously (mean episodes 2.3, SD = 3.1), had an average of 5.2 (SD = 6.0) years of opiate use, 38% were intravenous drug users, 20% reported previous methadone maintenance, and had used heroin an average of 20.7 (SD = 6.8) days out of the 28 prior to detoxification (mean ‘bags’ per day 2.8, SD = 1.6). The treatment groups differed significantly with respect to baseline intensity of opioid use (number of ‘bags’ per day).
Assessments
MCMI-III
The MCMI-III (Millon, 1994) is a 175-item, true–false, self-report inventory that measures clinical syndromes and personality disorders grouped by level of severity corresponding closely to most of the Axis I and II categories of the diagnostic system of the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM–IV; American Psychiatric Association, 1994). Table 1 lists the scale names for the clinical scales (along with base rates and elevations for descriptive purposes). A base rate of 85 or greater suggests a disorder of clinical significance (i.e., primary diagnosis) while a score of 75–84 indicates characteristics of the disorder. The MCMI-III contains four scales (validity, disclosure, desirability, and debasement) that are used to detect the presence of response sets and invalid profiles. Following test manual recommendations, four profiles were excluded that had a raw Disclosure (X) scale score exceeding 179. One profile was excluded with a Validity (V) scale score exceeding 2 and two profiles were excluded because most of the personality disorder scales were below a base rate of 59. No profiles were excluded for missing items (>12). Although the MCMI has been criticized as a diagnostic instrument (convergent validity), the reliability and validity of the first (MCMI-I) and second (MCMI-II) versions has been extensively evaluated, particularly in substance abusers (Craig & Weinberg, 1992a, 1992b). However, it should be noted that, to date, few studies have used the MCMI-III in substance abusers, and there have been significant changes in item content, scoring, and scales.
Table 1.
MCMI-III Base-Rate Scale Means and Elevations
| Scale base rate |
||||
|---|---|---|---|---|
| Scale | M | SD | >75% | >85% |
| Axis I | ||||
| Alcohol Abuse | 64.4 | 22.5 | 40.8 | 10.4 |
| Drug Abuse | 85.1 | 14.6 | 76.0 | 52.0 |
| Anxiety | 68.3 | 32.3 | 67.2 | 33.6 |
| PTSD | 48.0 | 26.8 | 8.0 | 1.6 |
| Dysthymia | 61.5 | 28.2 | 50.4 | 14.4 |
| Major Depression | 58.3 | 25.5 | 24.0 | 9.6 |
| Bipolar Manic | 57.3 | 18.6 | 9.6 | 3.2 |
| Somatoform | 59.6 | 23.3 | 16.0 | 6.4 |
| Delusional | 45.2 | 25.5 | 2.4 | 0.8 |
| Thought Disorder | 50.2 | 25.6 | 4.0 | 1.6 |
| Axis II | ||||
| Paranoid | 48.6 | 26.3 | 10.4 | 0.0 |
| Schizoid | 60.1 | 23.2 | 25.6 | 8.0 |
| Schizotypal | 45.1 | 25.4 | 1.6 | 0.0 |
| Antisocial | 73.4 | 18.9 | 56.8 | 29.6 |
| Borderline | 54.7 | 26.2 | 23.2 | 7.2 |
| Histrionic | 49.1 | 18.0 | 7.2 | 2.4 |
| Narcissistic | 61.9 | 18.3 | 22.4 | 10.4 |
| Avoidant | 50.1 | 26.0 | 20.0 | 1.6 |
| Dependent | 54.2 | 25.7 | 21.6 | 4.8 |
| Compulsive | 42.0 | 18.1 | 4.8 | 0.8 |
| Depressive | 55.1 | 29.7 | 28.8 | 10.4 |
| Negativistic | 54.6 | 27.5 | 29.6 | 10.6 |
| Self-Defeating | 51.6 | 28.1 | 14.4 | 2.4 |
| Aggressive–Sadistic | 60.2 | 16.7 | 14.4 | 5.6 |
Note. MCMI-III = Millon Clinical Multiaxial Inventory–III; PTSD = Posttraumatic Stress Disorder.
Substance Use Calendar
The substance use calendar, based on the Form 90 developed by Miller and DelBoca (1994), was used as a structured tool to facilitate the collection of information on treatment participation, medication compliance, and substance use on a day-to-day basis. It allows for a flexible, continuous evaluation of outcome and minimizes missing data. In addition to these self-report measures of substance use, the Roche Ontrack system was used to evaluate each thrice-weekly urine specimen for the presence of metabolites of opiates, cocaine, and benzodiazepines. Of the over 2000 urine specimens collected from all participants during the treatment phase of the study, 96% were consistent with the participants’ self-report of opioid use (Carroll et al., 2001).
Addiction Severity Index
The Addiction Severity Index (ASI; McLellan et al., 1992) is a structured interview assessing addiction-related impairment in seven areas of functioning: medical, employment, alcohol, drug, family–social, legal, and psychological. Various items from each subscale were used to compute composite scores that have been found to be reliable and valid indicators of changes in psychosocial impairment over time (Bovasso, Alterman, Cacciola, & Cook, 2001).
Beck Depression Inventory
The Beck Depression Inventory (Beck, 1978) is a 13-item self-report measure. The inventory provides a reliable and valid assessment (Beck, Steer, & Garbin, 1988) of past 30-day depression symptoms and has been used extensively in substance abuse studies.
Treatment Procedures and Conditions
All eligible individuals were offered an outpatient detoxification (5-day), involving clonidine or clonidine–naltrexone protocols described in previous reports (O’Connor et al., 1995, 1997) or were referred for an inpatient detoxification (2-day) in New Haven. Following informed consent and completion of detoxification, baseline assessments were completed and participants were randomly assigned, with an urn randomization program, to one of three conditions delivered over 12 weeks. Each of the three conditions received thrice weekly naltrexone and a weekly coping skills group but differed on the basis of the type of contingency management enhancement received: (a) no-incentive voucher; (b) incentive vouchers delivered contingent on naltrexone compliance and drug-free urine specimens; (c) contingent-incentive vouchers plus relationship counseling, which involved the participation of a significant other (family or partner) for up to six sessions over 12 weeks.
The weekly group sessions were based on a cognitive–behavioral coping skills manual developed by Carroll (1998). These open groups provided a rotating series of early recovery coping topics and were co-led by a master’s-level counselor and a nurse practitioner who received weekly, videotape-based supervision from the first author. Participants in the two contingency management conditions received incentive vouchers redeemable for goods and services following an effective system developed by Higgins (Budney & Higgins, 1998; Higgins et al., 1991) and adapted for this study to directly address naltrexone’s weaknesses by targeting two behaviors (observed naltrexone ingestion and drug-negative urine specimens). Incentives were provided on an escalating schedule with resetting of the amount following a missed medication or positive urine (see Carroll et al., 2001, for a detailed description). Participants could earn a maximum of $561 worth of items during the 12-week treatment. The significant other sessions in the incentive voucher plus relationship counseling condition were adapted from guidelines described by Budney and Higgins (1998) and delivered by a master’s-level social worker supervised by the principal investigator (fifth author). Participants also were encouraged within these sessions to redeem vouchers for goods and services that might strengthen their relationships and recovery.
In addition to the baseline assessments completed prior to randomization, participants were evaluated weekly during treatment and at the end of the 12-week course of treatment (mean number of treatment weeks completed was 7.1, SD = 4.7). Urine specimens were collected thrice weekly coinciding with medication visits. After 12 weeks, the coping skills group, incentive vouchers, and relationship counseling components were terminated. Following completion of this study treatment phase, participants were offered transfer for ongoing naltrexone and counseling at the affiliated Substance Abuse Treatment Unit.
Statistical Analyses
Subtype Derivation: Protocol Sorting (Criterion-Based)
Calsyn et al. (1996) developed a series of sorting rules from an extensive literature on MCMI-I and MCMI-II profiles in substance-abusing populations and from scoring and interpretation rules developed by Millon and others to define the most relevant and clinically meaningful subtypes in this population. We followed Calsyn et al.’s procedure by sorting the profiles twice, once to determine Axis I subtypes and once to determine Axis II subtypes. For all scales, an elevation was defined as being above a base rate of 74. Axis I subtypes were defined as: (a) no elevation, (b) drug-alcohol abuse only (only high on Drug Abuse or Alcohol Abuse), (c) psychotic symptoms (high on Thought Disorder or Delusional), (d) affective disturbance (high on Anxiety, Dysthymia, or Major Depression but not on Thought Disorder or Delusional), and (e) other (none of the above). Axis II subtypes were defined by the additional requirement that one of the elevated scales be the highest of any Axis II scale: (a) no elevation, (b) severe personality disorder (high on Schizotypal, Borderline, or Paranoid), (c) antisocial–narcissistic (high on Narcissistic or Antisocial), (d) withdrawn–negativistic (high on Schizoid or Avoidant), (e) dependent (high on Dependent), (f) histrionic (high on Histrionic), and (g) other (none of the above). Although these sorting rules were developed by Calsyn et al. on the basis of research with the earlier versions of the MCMI, no adjustments seemed necessary for our use of the MCMI-III because none of the newer scales (Posttraumatic Stress Disorder, Self-Defeating, Aggressive–Sadistic, Depressive) were used in the sorting rules.
Protocol Sorting: Cluster Analysis (Sample-Based)
Following Fals-Stewart’s (1992) and McMahon et al.’s (1998) methods, we used both hierarchical agglomerative cluster analysis (average linkage with squared Euclidean distance minimizes the average distance between all cases in the clusters) and non-hierarchical k-means (nearest centroid method maximizes between-cluster separation relative to within-cluster variation). Following Aldenderfer and Blashfield’s (1984) and Craig et al.’s (1997) guidelines, we first identified several possible cluster solutions by graphing the number of clusters against the fusion or amalgamation coefficients (i.e., the values at which various cases merge into clusters). The examination of increases in coefficient magnitude facilitated the location of points where two very dissimilar clusters merged, and then the number of clusters prior to this large increase was considered a possible solution. We then used kappa to identify the level of agreement between hierarchical and non-hierarchical clustering methods and evaluated performance on the external validity measures to guide final decisions about the optimal cluster solution. The comparison of cluster solutions on the concurrent validity variables helped determine whether increasing numbers of clusters were accompanied by increasing validity. We also considered the number of cases assigned to each cluster and regarded with a suspicion of unreliability (i.e., unlikely to generalize to other samples) any solution with subtypes consisting of fewer than 10% of the entire sample.
Some studies have cluster analyzed the Axis I and II scales separately (Donat et al., 1991; Mayer & Scott, 1988), whereas others have combined them (Bartsch & Hoffman, 1985; Craig et al., 1985, 1997; Donat, 1988). We first analyzed the axes separately to determine whether the empirically derived clusters resembled the a priori Axis I and II protocol-sorted subtypes. This was also a more appropriate first analytic step given our sample size and the number of scales involved. On the basis of an analysis of cluster redundancy, we then chose to cluster all scales together and report on this solution and its validity. Because previous cluster analyses with the earlier versions of the MCMI had not included some of the newer scales (Posttraumatic Stress Disorder, Self-Defeating, Aggressive–Sadistic, Depressive), we conducted clustering procedures with and without these scales and found highly similar patterns of results. Thus, we report on clusters including all MCMI-III scales.
Validity Analysis
Concurrent validity analyses involved t tests and chi-square tests to assess the relation between the MCMI-III–derived subtypes and various substance abuse and psychosocial indicators. Predictive validity analyses focused on retention in treatment, compliance with naltrexone (number of doses ingested over 12 weeks), opioid use frequency (self-reported days of use and percentage of opioid-free urine specimens), and improvement in addiction-related biopsychosocial impairment. The principal analytic strategies for predictive validity (treatment outcome and matching) were analysis of covariance (for aggregate data such as number of sessions completed) or random regression models (for data collected repeatedly over the 12-week study) involving two orthogonal contrasts. First, we conducted a contingency management contrast to evaluate the effect of reward contingencies: The two groups that received incentive vouchers (i.e., alone or with relationship counseling) were compared with the one group that did not receive incentive vouchers. Next, we conducted a significant-other contrast to evaluate the effect of additional relational support to contingency management: The incentive voucher plus relationship counseling condition was compared with the group that received incentive vouchers alone. Analyses were conducted on the intent-to-treat (i.e., randomized) sample, and significance tests were two-tailed with alpha level set at p < .05.
Results
Subtype Derivation
Table 1 lists the base rate means and standard deviations for the MCMI-III clinical and personality scales as well as the percentage of participants who experienced significant features (base rate > 75) and a probable diagnosis (base rate > 85). Among the Axis I scales, Drug Abuse, Anxiety, Dysthymia, and Alcohol Abuse were significantly elevated in this sample, and the remaining scales were in the average range of those found in general psychiatric samples. Among the Axis II scales, Antisocial, Narcissistic, and Schizoid were among the more elevated scales (see Table 1).
Protocol Sorting
Profiles sorted following Calsyn et al.’s (1996) method indicated the following Axis I subtype prevalence rates: affective disturbance (66%), drug and alcohol only (14%), no elevations (11%), psychotic symptoms (6%), and other (2%). Axis II subtype prevalence rates were as follows: antisocial–narcissistic (46%), other (25%), dependent (10%), no elevation (10%), histrionic (4%), severe personality disorder (4%), and withdrawn–negativistic (2%). Among the Axis I scales, affective disturbance was found to be twice as high as that found in the Calsyn et al. (1996) study, and the Other Axis II category was three times as high.
On the basis of the small number of individuals within many of the Axis I and II sorted categories (making analysis of treatment-matching interactions impossible), we chose to evaluate the concurrent and predictive validity of only the two most common Axis I and Axis II subtypes: affective disturbance and antisocial–narcissistic. These two subtypes were not significantly associated with each other, suggesting that separate concurrent and predictive validity analyses would provide nonredundant information.
Cluster Analysis
A series of hierarchical (average linkage) and non-hierarchical (k-means) cluster analyses conducted separately for the Axis I and II scales did not yield subtypes resembling those identified for protocol sorting, even when considering the 3–10 cluster solutions. Instead, a 2-cluster solution appeared optimal for both Axis I and II scales and could be labeled high- and low-severity clusters. The separate Axis I and Axis II cluster categories were closely associated, χ2(1, N = 125) = 75.5, p < .01 (κ = .78), suggesting that they did not provide independent methods of classifying individuals. For the sake of parsimony, we report only on cluster analyses of the combined Axis I and II scales using average linkage and k-means.
On the basis of the various indices discussed above (agglomeration coefficients, cell sizes, mean differences, kappa, and validity), it appeared that a 2-cluster solution was optimal. Both k-means (87/38) and average linkage analysis (109/16) yielded a high- and low-psychiatric severity subtype: kappa for the two methods = .50; χ2(1, N = 125) = 42.1, p < .01. The high-psychiatric subtype scored higher on all Axis I scales and all Axis II scales except Histrionic, Narcissistic, and Compulsive, on which the low-psychiatric subtype scored higher (see Table 2). At each stage of the analyses, a disproportionately larger number of participants remained classified as a high-severity type, and the lower severity types were divided into increasingly smaller groups that were less clearly differentiated (on derivation and validation indices) and in ways that did not lend themselves to easy labeling. In general, the higher level (3–10) cluster solutions would be unlikely to replicate in the future sample sizes typically used in randomized clinical trials and did not yield incremental validity to what was found for the 2-cluster solution. The concurrent and predictive validity analyses discussed below focus only on the k-means solution because the cell sizes were better (than average linkage) for analyses of interactions.
Table 2.
MCMI-III K-Means Two-Cluster Solution (Sample-Based)
| Subtype 1 (n = 87) |
Subtype 2 (n = 38) |
|||
|---|---|---|---|---|
| Scale | M | SD | M | SD |
| Axis I | ||||
| Drug Abuse | 88.6 | 12.7 | 77.1 | 15.7 |
| Alcohol Abuse | 72.0 | 15.2 | 47.0 | 26.7 |
| Anxiety | 84.3 | 15.4 | 31.8 | 31.2 |
| PTSD | 61.8 | 15.3 | 16.3 | 19.4 |
| Dysthymia | 75.2 | 14.9 | 30.0 | 26.1 |
| Major Depression | 68.5 | 17.0 | 35.1 | 26.7 |
| Bipolar Manic | 63.6 | 13.2 | 42.8 | 20.9 |
| Somatoform | 67.9 | 13.8 | 40.5 | 28.9 |
| Delusional | 52.7 | 21.6 | 27.9 | 25.6 |
| Thought Disorder | 65.0 | 8.8 | 16.2 | 17.7 |
| Axis II | ||||
| Paranoid | 57.7 | 21.0 | 27.7 | 25.5 |
| Schizoid | 67.7 | 16.0 | 42.9 | 27.8 |
| Schizotypal | 56.6 | 16.2 | 18.8 | 23.1 |
| Antisocial | 79.9 | 12.6 | 58.6 | 22.5 |
| Borderline | 69.0 | 12.3 | 22.1 | 19.2 |
| Histrionic | 44.4 | 17.3 | 59.9 | 14.8 |
| Narcissistic | 58.2 | 17.9 | 70.4 | 16.2 |
| Avoidant | 61.5 | 19.3 | 23.9 | 19.9 |
| Dependent | 64.9 | 19.0 | 29.7 | 21.8 |
| Compulsive | 35.9 | 16.2 | 55.8 | 14.5 |
| Depressive | 69.9 | 17.5 | 21.1 | 23.3 |
| Negativistic | 67.6 | 19.5 | 25.0 | 19.0 |
| Self-Defeating | 65.5 | 16.6 | 20.0 | 22.9 |
| Aggressive–Sadistic | 66.5 | 11.3 | 46.0 | 18.4 |
Note. All t tests are significant at p < .01 with Cluster 1 scoring higher than Cluster 2 on all scales except Histrionic, Narcissistic, and Compulsive on which Cluster 2 scored higher. MCMI-III = Millon Clinical Multiaxial Inventory–III; PTSD = posttraumatic stress disorder.
Concurrent Validity
Protocol Sorting: Affective (vs. Non-Affective) Disturbance Subtype (83/42)
There were no differences on demographic measures (gender, marital, employment, education, criminal justice referral) or baseline substance abuse measures (prior detoxification, drug treatment, route of use, lifetime diagnosis of alcohol, cocaine, or marijuana abuse). There was a significant race effect for this subtype in which proportionately more Caucasian (71%) than non-Caucasian (African and Hispanic American) (48%) participants were categorized as having affective disturbance, χ2(1, N = 125) = 4.74, p < .03.
Individuals with the affective disturbance subtype scored higher than non-affective subtype individuals on the Beck Depression Inventory, t(120) = 3.23, p < .01, ASI Medical, t(111) = 2.25, p < .03, and Psychological, t(120) = 2.18, p < .03, composite severity scales. Those in the affective disturbance category reported more years of opiate use, t(123) = 2.03, p < .04 and were more bothered by their substance-related problems, t(112) = 2.38, p < .02, than were non-affective disturbance individuals. Consistent with the 2-cluster scale derivation described above, the affective disturbance subtype scored higher on all MCMI-III Axis II scales except Histrionic, Narcissistic, and Compulsive, on which they scored lower than non-affective participants.
Protocol Sorting: Antisocial–Narcissistic (vs. Non–Antisocial–Narcissistic) Subtype (57/68)
The only baseline demographic difference was for rates of current employment, which was proportionately lower in individuals of antisocial-narcissistic subtypes in comparison with non-antisocial-narcissistic subtypes who were more often working, χ2(1, N = 125) = 4.23, p < .04. The only MCMI-III Axis I scale on which individuals of the antisocial–narcissistic subtype scored higher than non–antisocial–narcissistic individuals was the Drug Abuse scale, t(123) = 3.60, p < .01. Antisocial–narcissistic subtype individuals used heroin more frequently in the month prior to treatment initiation, t(110) = 2.82, p < .01, than did non–antisocial–narcissistic individuals. They had a higher ASI Heroin composite severity score, t(112) = 2.89, p < .01. In addition, there were trends for more long-standing use of cocaine and heroin in comparison with non–antisocial–narcissistic individuals. In contrast to the other two high-psychopathology subtypes (affective disturbance, psychiatric), the antisocial–narcissistic subtype reported feeling less troubled by their psychological problems, t(112) = −2.42, p < .02, and had a correspondingly lower ASI Psychological composite severity score, t(109) = −2.25, p < .03.
Cluster Analysis: High (vs. Low) Psychiatric Severity Cluster (87/38)
There were no differences on baseline demographic or substance abuse measures. Individuals in the high-psychiatric severity cluster scored higher than did those in the low-psychiatric severity cluster on the Beck Depression Inventory, t(120) = 5.54, p < .01, and the ASI Psychological composite, t(109) = 6.75, p < .01, and were more troubled by their psychological problems, t(112) = 5.08, p < .01. They were also more troubled by their substance problems, t(112) = 2.35, p < .02, and family and social problems, t(112) = 3.30, p < .01, and scored higher on the ASI Family composite, t(112) = 3.10, p < .03.
Predictive Validity
Overall, ASI Medical, Employment, Heroin Use, Drug Use, Legal, Family, and Psychological composite scores decreased over time. Alcohol scores did not change significantly from baseline to treatment endpoint. We found no subtype main effects or Type × Treatment interactions on retention (number of weeks in treatment post-detoxification), medication compliance (number of naltrexone doses taken), or end-of-treatment abstinence rates (number of negative urine results, total number of days abstinent), although several time effects were significant for opiate use.
Affective (vs. Non-Affective) Disturbance Subtype
Subtype × Time interactions
Individuals of the non-affective subtype exhibited decreased probability of opiate use over 12 weeks (substance use calendar confirmed by urine testing) in comparison with affective disturbance subtype individuals, who showed no significant reduction in opiate use (z = −3.05, p < .01). The affective disturbance subtype had a greater reduction in the ASI Medical composite, z = 2.52, p < .01, but less reduction in the ASI Legal composite (z = −1.92, p < .05) than did non-affective individuals over 12 weeks.
Subtype × Treatment × Time interactions
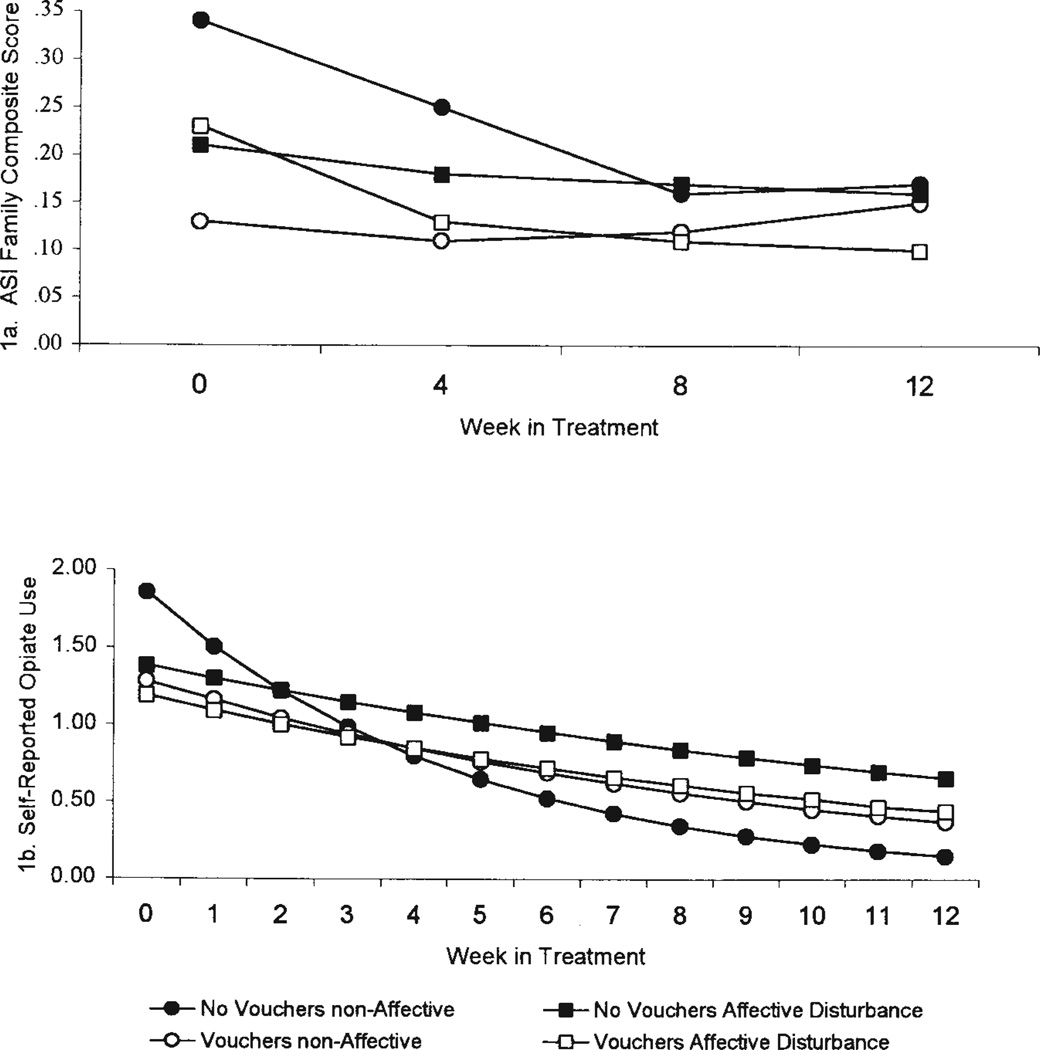
There was evidence for patient-treatment matching for weekly probability of opiate use and monthly ASI Family Composite severity ratings. The affective disturbance subtype had a greater reduction in the ASI Family composite severity than did non-affective individuals in the two (combined) incentive voucher conditions over 12 weeks and greater reduction in these incentive conditions than when no-incentive vouchers were received for medication compliance and drug abstinence. Individuals of the non-affective subtype had a greater reduction in ASI Family composite severity in the no-incentive voucher than in the incentive conditions, z = 2.00, p < .05 (see Figure 1a). Individuals of the non-affective subtype also had a greater reduction in the probability of opiate use in the no-incentive voucher than in the incentive-voucher condition and greater reduction than individuals of the affective subtype in the no-incentive voucher condition, z = −2.41, p < .02 (see Figure 1b).
Figure 1.
(a) Affective Disturbance Subtype × Treatment × Time interaction for monthly Addiction Severity Index (ASI) Family Composite severity. (b) Affective Disturbance Subtype × Treatment × Time interaction for weekly probability of opiate use.
Antisocial–Narcissistic (vs. Non–Antisocial–Narcissistic) Subtype
Subtype × Time interactions
Non–antisocial–narcissistic subtype individuals had a greater reduction in opiate use in comparison with antisocial-narcissistic participants who did not show a decreased probability of opiate use over 12 weeks, z = −2.05,p < .04. However, the antisocial-narcissistic subtype had a greater reduction in ASI Legal composite than did non–antisocial–narcissistic individuals over a 12-week period, z = 1.97,p < .05.
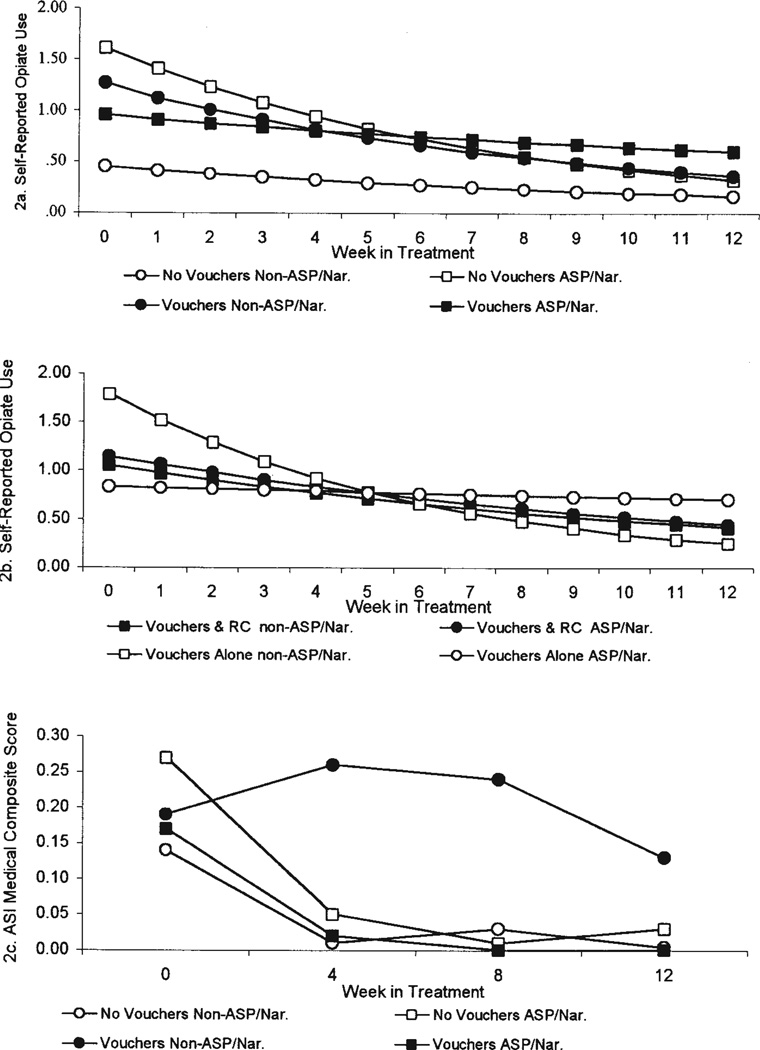
Subtype × Treatment × Time interactions
Individuals of the antisocial-narcissistic subtype had greater reduction in probability of opiate use in the no-incentive voucher than in the two (combined) incentive voucher conditions, z = 3.69, p < .01 (see Figure 2a). In addition, antisocial-narcissistic subtype individuals had greater opiate use reduction when provided with incentive vouchers plus relationship counseling than when given incentive vouchers alone. In contrast, non–antisocial–narcissistic subtype individuals had greater reduction in probability of opiate use in the incentives alone condition than in the incentives plus relationship counseling conditions z = −3.68,p < .01 (see Figure 2b).
Figure 2.
(a) Antisocial/Narcissistic Subtype × Treatment × Time interaction for weekly probability of opiate use (vouchers vs. no-vouchers). (b) Antisocial/Narcissistic Subtype × Treatment × Time interaction for weekly probability of opiate use (vouchers alone vs. vouchers and relationship counseling). (c) Antisocial/Narcissistic Subtype × Treatment × Time interaction for monthly Addiction Severity Index (ASI) Medical Composite severity. ASP = antisocial personality; Nar. = narcissistic personality; RC = relationship counseling.
With regard to treatment matching effects for the ASI composites, non–antisocial–narcissistic subtype individuals showed less improvement in ASI Medical composite reduction when receiving incentive vouchers than in the no-incentive voucher condition and less improvement than the antisocial–narcissistic subtype in the no-incentive voucher condition, z = 4.27, p < .01 (see Figure 2c).
High (vs. Low) Psychiatric Severity Cluster
Subtype × Time interactions
The low-psychiatric cluster demonstrated greater reduction in the probability of opiate use than did the high-psychiatric cluster, which showed no decrease in probability of opiate use over 12 weeks, z = −2.25, p < .03. The low-psychiatric cluster also had greater reduction in ASI Family composite severity (z = −2.12, p < .03) and Psychological composite severity, z = −3.58, p < .01, than did the high-psychiatric cluster over 12 weeks.
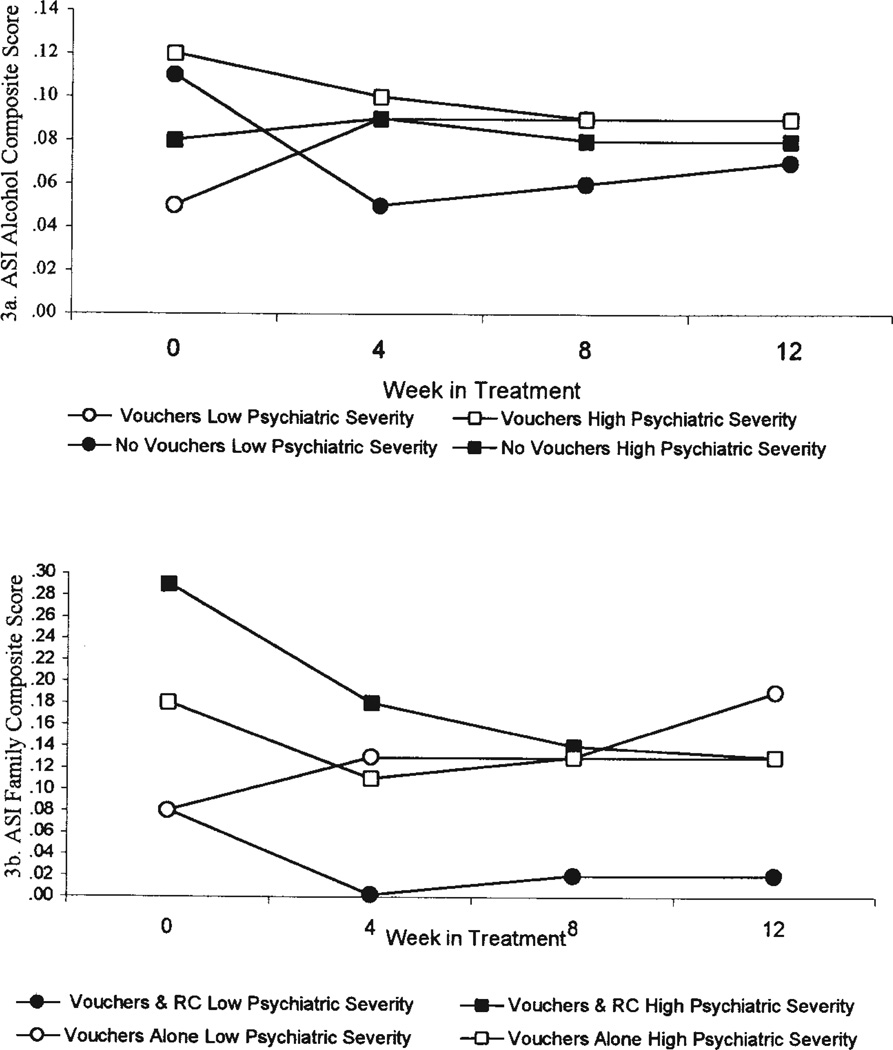
Subtype × Treatment × Time interactions
The low-psychiatric cluster had a greater reduction in ASI Alcohol composite severity in the no-incentive voucher condition than in the two incentive voucher conditions, z = −2.46, p < .01 (see Figure 3a). The low-psychiatric cluster had greater reduction in ASI Family composite severity in the incentive voucher plus relationship counseling condition than in the incentives alone condition, z = −1.96, p < .05 (see Figure 3b).
Figure 3.
(a) Psychiatric Severity Cluster × Treatment × Time interaction for monthly Addiction Severity Index (ASI) Alcohol Composite severity. (b) Psychiatric Severity Cluster × Treatment × Time interaction for monthly ASI Family Composite severity. RC = relationship counseling.
Discussion
This was the first study to compare the validity of the two most common methods of subtyping substance-dependent patients and to evaluate treatment matching for one of the most widely studied omnibus psychopathology inventories in substance abuse samples. We assessed the concurrent and predictive validity of MCMI-III protocol-sorted (criterion-based) and cluster analyzed (sample-based) groups of opioid-dependent outpatients treated in a randomized clinical trial comparing different behavioral therapy interventions added to naltrexone pharmacotherapy.
Protocol Sorting and Cluster Analysis Subtypes
Consistent with Calsyn et al.’s (1996) protocol-sorting findings, affective disturbance (66%) and antisocial–narcissistic (46%) were the most common subtypes. Our sample had higher rates of affective disturbance and other Axis II subtypes, but prevalence rates were otherwise similar to those obtained by Calsyn et al. despite different sample characteristics and different versions of the MCMI. Calsyn et al.’s sample had a somewhat higher percentage of African Americans and a more chronic history of opioid dependence and were receiving methadone rather than naltrexone treatment.
Cluster analysis statistics supported the consideration of several solutions, but none of these resembled the protocol-sorting subtypes or those found in previous studies and did not improve the validity analysis over the more parsimonious two-cluster solution. Our high-psychiatric severity cluster (70% of sample) resembled that found by Craig et al. (1997) using the MCMI-II in that all scales were elevated except for lower scores on Histrionic, Narcissistic, and Compulsive scales. Craig et al. described these patients as a highly distressed, but emotionally detached, group with poor organizational and planning skills. Although these individuals are not sociopathic in the primary sense, they are likely to exhibit antisocial behavior when frustrated or stressed, to have higher rates of suicide attempts, and to have had prior treatment for substance abuse and psychiatric problems. Craig et al.’s hypothesis that these individuals might have trouble adhering to or following the routine of a structured treatment program has received some support from a recent MCMI-II cluster analysis outcome study by Haller et al. (2002), which found that a similar cluster had the worst retention in a day treatment program.
In comparing the two methodologically very different processes, but partially overlapping subtype models (high psychiatric cluster overlapped with affective disturbance profile), our results suggested that protocol sorting was at least as valid as cluster analysis despite a derivation approach that was potentially biased in favor of a cluster-derived solution (i.e., the two-cluster model was chosen over the three-, four-, five-, and six-cluster solutions according to reliability and validity comparisons). In addition, protocol sorting has the advantage of being much simpler to implement and apply consistently across samples and has the real-world, clinical applicability advantage of permitting patients to be sorted on a case-by-case basis for treatment-planning purposes, rather than being derived after an entire sample is collected. This aspect, combined with the added advantages of computerized administration, scoring, and interpretation of self-report inventories, results in a potentially more cost-efficient assessment for prospective matching or treatment-assignment purposes. We conclude that the MCMI profiles of individuals with substance abuse have been sufficiently cluster analyzed and that this has served the useful purpose of describing subtypes that can now be identified through protocol sorting. Future research should focus on the more efficiently derived protocol-sorting subtypes.
Some might rightly argue with a recommendation to pursue further research with the MCMI-III and might criticize our choice of this instrument given its reputation for under-identification of substance use disorders (Bryer, Martines, & Dignan, 1990; Marsh et al., 1988) and over-identification of other Axis I and II disorders in substance-dependent individuals (Calsyn & Saxon, 1990; Calsyn et al., 1996; Craig, 1988; Marsh et al., 1988). Research on the diagnostic validity and efficiency of the MCMI-I and MCMI-II personality disorder scales is mixed: Some studies have found adequate discriminant and convergent validity (Craig, 1988; Dubro, Wetzler, & Kahn, 1988; Torgersen & Alnaes, 1990), whereas others have found poor validity with the DSM constructs (Piersma, 1987; Repko & Cooper, 1985; Wetzler & Dubro, 1990; Widiger & Sanderson, 1987). Although not a focus of our current study, we too found limited correspondence between the MCMI-III Alcohol Abuse, Drug Abuse, Antisocial, and Major Depression scales with those from the SCID. The reliability and validity of all versions of the MCMI and other self-report inventories of personality disorders have been criticized, especially when they are administered to an acutely symptomatic patient at a time when differentiating substance-related state effects from personality traits can be very complicated (Ball, Rounsaville, Tennen, & Kranzler, 2001). This would certainly be the case in the group of opioid-dependent individuals presenting for detoxification in this study. Given these limitations, the different versions of the MCMI probably should not be used for diagnostic purposes in those with active substance abuse, although they may be useful for subtyping or screening for psychopathology.
Our cluster analysis did not reveal several subtypes that have been found in previous MCMI-I and MCMI-II studies (e.g., avoidant–withdrawn, negativistic, psychotic, histrionic, dependent) even when 3–10 clusters were considered. The reasons for this may be related to methodological differences in participant sampling and assessment. With regard to assessment, there have been major changes across the three editions of the MCMI. Of equal if not greater importance to the four changes in clinical or personality scales, more than half of the items were changed from MCMI-II to MCMI-III, item weights for prototypic scoring were altered, and validity scales and score adjustments or corrections were modified. As a result, there is less item redundancy and intercorrelation. The average scale correlation between the MCMI-II and MCMI-III is about .70, ranging from a low of .59 (dependent) to a high of .88 (dysthymia; Millon, 1994). Although these correlations are highly significant, the different MCMI versions are not interchangeable, and the changes made could have an impact on cluster-analytic findings. With regard to participant sampling, studies with more cases and perhaps greater heterogeneity (e.g., including severe dual diagnosis cases) may be able to derive a greater number of more differentiated clusters. Although a larger or broader group of participants might have resulted in our identifying these subtypes, it is unknown whether these finer distinctions (e.g., clusters differing from each other on 1–2 scales) will have reliability and validity across studies from a symptom presentation, treatment outcome, or matching perspective.
Treatment Outcome and Matching
With regard to subtype main effects, as predicted, the affective disturbance, antisocial–narcissistic, and psychiatric severity subtypes had more severe substance use at baseline and less reduction after 12 weeks of outpatient treatment. The affective disturbance and psychiatric severity subtypes reported greater psychosocial impairment (and less reduction over time), but antisocial-narcissistic individuals reported less psychological distress and more improved legal functioning after 12 weeks of treatment. Unlike a few previous studies (Calsyn et al., 1996; Fals-Stewart, 1992; Haller et al., 2002; Stark & Campbell, 1988), our subtypes were unrelated to treatment retention. Although it is possible that the three different versions of the MCMI used across these five studies accounts for the inconsistent results, a more likely reason lies in the interaction of patient differences (race, gender, criminal justice referrals) with treatment modality differences (methadone, naltrexone, therapeutic community, day treatment, outpatient) across studies.
The current study builds on findings by Carroll et al. (2001), demonstrating a number of potentially interesting Patient Attribute (subtype) × Treatment Condition interactions, although very few of these supported our hypotheses that the more severe psychopathology subtypes would derive greater benefit from incentive vouchers. In fact, a number of unpredicted effects occurred that favored no-incentive vouchers over the two-incentive voucher conditions for some subtypes. Although individuals of the affective disturbance subtype did demonstrate better improvement in ASI Family severity in the incentive condition, non-affective subtype individuals actually did better on this measure and also had decreased probability of opiate use in the no-incentives condition. These results paralleled findings for low psychiatric severity (which was significantly associated with affective disturbance) in which this cluster demonstrated better ASI Alcohol severity outcome in the no-incentive condition than in the incentive conditions. The low-psychiatric severity cluster also demonstrated better ASI Family outcomes when given incentives and relationship counseling than when receiving incentives alone.
We also did not find support for predictions that the higher psychiatric cluster might benefit more from enhanced behavioral interventions, and this was conceptually inconsistent with the McLellan et al. (1983), Woody et al. (1984), and Woody, McLellan, Luborsky, & O’Brien (1995) findings in which enhanced psychosocial services improved outcome for more severe methadone patients. Incentive vouchers alone, by narrowly targeting only substance abstinence and antagonist compliance, may not be an adequate psychosocial enhancement (in the same way that psychiatric or psychotherapeutic services might be) to address the psychiatric distress of these patients. Of somewhat greater interest was the finding that the non-affective subtype and low-psychiatric cluster had better outcomes on some substance-related measures when they received no incentives. Future research should explore whether addicted patients experiencing very few psychological problems or external pressures to receive treatment exhibit a countertherapeutic reaction to external contingencies being placed on behavior they already may be intending to change.
Two matching findings for the antisocial–narcissistic subtype were also unexpected, as this group exhibited greater reduction in opiate use probability in the no-incentives condition than in the two incentive conditions. In addition, the antisocial–narcissistic subtype benefited from the addition of relationship counseling to the incentive condition more than when receiving incentive vouchers alone. In contrast, it was the non–antisocial–narcissistic subtype individuals who showed no benefit from the added relationship counseling and had better opiate use outcomes when receiving incentive vouchers alone. Of interest, our finding that the antisocial–narcissistic subtype did not respond well to the addition of incentive vouchers appears to be consistent with Millon’s theory that these individuals are insensitive to or even disdainful of external contingencies. However, this finding is inconsistent with several findings that antisocial methadone maintenance patients either do as well as or better than non-antisocial individuals when behavioral or monetary incentives for abstinence are added to standard addiction treatment (Brooner et al., 1998; Messina et al., 2003; Silverman et al., 1996, 1998).
Our finding that antisocial–narcissistic individuals derive additional benefit from relationship counseling was inconsistent with conclusions from alcoholism researchers (Kadden et al., 1989; Longabaugh et al., 1994) that sociopathic individuals may not respond well to relational or interactional interventions. In addition, this finding was also inconsistent with our predictions, derived from Millon’s theory, which views this group as deficient in reciprocal relationship functioning. It is possible that the discrepancy between our findings and previous research on antisocial personality responsivity to behavioral incentives and relational interventions is due to differences in the measurement of this construct. Specifically, this previous research has either analyzed DSM–III–R antisocial personality disorder on the basis of a structured diagnostic interview (SCID) or sociopathy on the basis of a self-report socialization scale. Although all versions of the MCMI were developed to parallel changes in the DSM, most research has found poor concordance between the Axis II constructs of the two systems, as described earlier. Nonetheless, it has become clear from an emerging body of evidence that antisocial individuals with substance abuse are heterogeneous in their response to different treatment interventions across studies and do not have uniformly poor outcome. One also might argue that this study’s eligibility criteria of being able to identify a significant other willing to participate resulted in an absence of primarily sociopathic individuals for whom relationship counseling might provide no obvious benefit. In addition, several of our personality disorder scale elevations were lower than those found in some previous studies and suggested that we may not have included many deeply sociopathic characters in our sample.
An important caution should be mentioned regarding the Patient (attribute) × Treatment interactions themselves. These types of complex interactions can be very difficult to replicate even with only minor variations in study samples and methods. Among the limitations of this investigation summarized by Carroll et al. (2001) was sample representativeness. Although not unusual in treatment settings, about half of the entire group of opioid-dependent individuals approached about the study dropped out prior to, during, or immediately after initiating treatment. In addition, our sample was seeking detoxification and antagonist treatment and was somewhat higher functioning, better educated, and more likely to be employed, and also had lower rates of intravenous heroin use than what is seen in most methadone programs. Our relatively few matching effects may not generalize to higher or lower potency incentive conditions or even to the exact same contingency management comparisons delivered to a somewhat different opioid-dependent sample receiving a different pharmacotherapy. For example, Messina et al. (2003) found that methadone maintained patients with a SCID antisocial personality disorder diagnosis had significantly better cocaine outcomes than did non-antisocial individuals when they received a contingency management protocol similar to ours. It will be important for future research to replicate and extend our findings in other samples.
Nonetheless, this study raises some important questions about the use of voucher-based incentives for all types of individuals with substance abuse. This approach was initially developed for cocaine-dependent outpatients and generated considerable excitement as one of the only replicated effective treatments (psychosocial or pharmacological) for cocaine abuse (Higgins et al., 1991; Higgins, Alessi, & Dantona, 2002). Since then, incentive vouchers have demonstrated efficacy in methadone (Silverman et al., 1996), naltrexone (Preston et al., 1999), opiate detoxification (Bickel, Amass, Higgins, Badger, & Esch, 1997), alcohol (Petry, Martin, Cooney, & Kranzler, 2000), marijuana (Budney, Higgins, Radonovich, & Novy, 2000), and dual diagnosis patients (Shaner et al., 1997; Sigmon, Steingard, Badger, Anthony, & Higgins, 2000). Although the treatment retention and substance reduction rates have not been quite as dramatic as some of the original cocaine studies, participants as a whole who receive incentive vouchers typically do at least twice as well as those who do not receive incentives. Nonetheless, there are still a substantial number of participants who do not derive significant benefit from incentives, often as many as half of those in the condition. Presumably, there are also individuals who actually do better when receiving no-incentive vouchers, as in our study in which several subtypes did better on certain outcomes. Very little has been written on reverse or nonresponders to incentive vouchers. Future research should focus on improving our understanding of this group as a critical next step in what has been an impressive, systematic series of studies on incentives (Higgins et al., 2002).
In conclusion, behavioral therapies can be targeted to the compliance-related limitations of pharmacotherapy and thus may play an important role in broadening the utility of available medications for addiction (Carroll et al., 2001). In addition, the identification of patient subtypes to guide decisions about specific types of behavioral therapies may be another necessary component to the process of improving pharmacotherapeutic response. This may be especially relevant for the use of naltrexone, which despite tremendous potential as a highly specific and effective antagonist with minimal side effects, is widely regarded as having limited effectiveness in standard clinical practice and is possibly effective only with select populations (e.g., professionals or other individuals mandated to treatment; Cornish et al., 1997; Greenstein, Fudala, & O’Brien, 1997). Thus, the identification of individuals who may benefit from specific behavioral therapy enhancements to promising medications deserves further study.
Acknowledgments
Support for this study was provided by National Institute on Drug Abuse Grants P50-DA0924, K05-DA00457 (to Kathleen M. Carroll), and K05-DA00089 (to Bruce J. Rounsaville).
We acknowledge the contribution of staff from the APT Foundation Central Medical Unit (Maureen Lewis, Carol Eggers, Julia Shi, Patrick O’Connor, Janet Constantino, and Susan Henry) and the Yale University/ APT Clinical Research Unit (Tami Frankforter, Monica Canning-Ball, Art Woodard, Roseann Bisighini, Elise Triffleman, Theresa Babuscio, Lynn Gordon, and Joanne Corvino).
References
- Aldenderfer MS, Blashfield RK. Cluster analysis. In: Lewis-Beck MS, editor. Quantitative applications in the social sciences. Beverly Hills, CA: Sage University; 1984. (Sage University Paper Series 07–044) [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed. Washington, DC: Author; 1994. [Google Scholar]
- Ball SA. Type A and B alcoholism: Applicability across sub-populations and treatment settings. Alcohol Health and Research World. 1996;20:30–35. [PMC free article] [PubMed] [Google Scholar]
- Ball SA, Rounsaville BJ, Tennen H, Kranzler HR. Reliability of personality disorder symptoms and personality traits in substance dependent inpatients. Journal of Abnormal Psychology. 2001;110:341–352. doi: 10.1037//0021-843x.110.2.341. [DOI] [PubMed] [Google Scholar]
- Barnes GE, Murray RP, Patton D, Bentler PM, Anderson RE. The addiction-prone personality. New York: Plenum; 2000. [Google Scholar]
- Bartsch TW, Hoffman JJ. A cluster analysis of Millon Clinical Multiaxial Inventory profiles: More about taxonomy of alcohol subtypes. Journal of Clinical Psychology. 1985;41:707–713. doi: 10.1002/1097-4679(198509)41:5<707::aid-jclp2270410521>3.0.co;2-w. [DOI] [PubMed] [Google Scholar]
- Beck AT. Beck Depression Inventory. New York: Psychological Corporation; 1978. [Google Scholar]
- Beck AT, Steer RA, Garbin MG. Psychometric properties of the Beck Depression Inventory: Twenty-five years of evaluation. Clinical Psychology Review. 1988;8:77–100. [Google Scholar]
- Bickel WK, Amass L, Higgins ST, Badger GJ, Esch RA. Effects of adding behavioral treatment to opioid detoxification with buprenorphine. Journal of Consulting and Clinical Psychology. 1997;65:803–810. doi: 10.1037//0022-006x.65.5.803. [DOI] [PubMed] [Google Scholar]
- Bovasso GB, Alterman AI, Cacciolo JS, Cook TG. Predictive validity of the Addiction Severity Index’s composite scores in the assessment of 2-year outcomes in a methadone maintenance population. Psychology of Addictive Behaviors. 2001;15:171–176. [PubMed] [Google Scholar]
- Brooner RK, Kidorf M, King VL, Stoller K. Preliminary evidence of good treatment response in antisocial drug abusers. Drug and Alcohol Dependence. 1998;49:249–260. doi: 10.1016/s0376-8716(98)00018-0. [DOI] [PubMed] [Google Scholar]
- Bryer JB, Martines KA, Dignan MA. Millon Clinical Multiaxial Inventory Alcohol Abuse and Drug Abuse scales and the identification of substance-abuse patients. Psychological Assessment. 1990;4:438–441. [Google Scholar]
- Budney AJ, Higgins ST. A community reinforcement plus vouchers approach. Treating cocaine addiction: Therapy manuals for drug addiction. Rockville, MD: National Institute on Drug Abuse, U.S. Department of Health and Human Services; 1998. [Google Scholar]
- Budney AJ, Higgins ST, Radonovich KJ, Novy PL. Adding voucher-based incentives to coping skills and motivation enhancement improves outcomes during treatment for marijuana dependence. Journal of Consulting and Clinical Psychology. 2000;68:1051–1061. doi: 10.1037//0022-006x.68.6.1051. [DOI] [PubMed] [Google Scholar]
- Cacciola JS, Alterman AI, Rutherford MJ. Treatment response and problem severity of antisocial substance abusers. Journal of Nervous and Mental Disease. 1995;183:166–171. doi: 10.1097/00005053-199503000-00007. [DOI] [PubMed] [Google Scholar]
- Cacciola JS, Rutherford MJ, Alterman AI, McKay JR, Snider EC. Personality disorders and treatment outcome in methadone maintenance patients. Journal of Nervous and Mental Disease. 1996;184:234–239. doi: 10.1097/00005053-199604000-00006. [DOI] [PubMed] [Google Scholar]
- Calsyn DA, Fleming C, Wells EA, Saxon AJ. Personality disorder subtypes among opiate addicts in methadone maintenance. Psychology of Addictive Behaviors. 1996;10:3–8. [Google Scholar]
- Calsyn DA, Saxon AJ. Personality disorder subtypes among cocaine and opioid addicts using the Millon Clinical Multiaxial Inventory. The International Journal of the Addictions. 1990;25:1037–1049. doi: 10.3109/10826089009058871. [DOI] [PubMed] [Google Scholar]
- Carroll KM. A cognitive–behavioral approach. Treating cocaine addiction: Therapy manuals for drug addiction. Rockville, MD: National Institute on Drug Abuse, U.S. Department of Health and Human Services; 1998. [Google Scholar]
- Carroll KM, Ball SA, Nich C, O’Connor PG, Eagan D, Frank-forter TL, Triffleman EG, Shi J, Rounsaville BJ. Targeting behavioral therapies to enhance naltrexone treatment of opioid dependence: Efficacy of contingency management and significant other involvement. Archives of General Psychiatry. 2001;58:755–761. doi: 10.1001/archpsyc.58.8.755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carroll KM, Rounsaville BJ, Gordon LT, Nich C, Jatlow PM, Bisighini RM, Gawin FH. Psychotherapy and pharmacotherapy for ambulatory cocaine abusers. Archives of General Psychiatry. 1994;51:177–187. doi: 10.1001/archpsyc.1994.03950030013002. [DOI] [PubMed] [Google Scholar]
- Cornish JW, Metzger D, Woody GE, Wilson D, McLellan AT, Vandergrift B, O’Brien CP. Naltrexone pharmacotherapy for opioid dependent federal probationers. Journal of Substance Abuse Treatment. 1997;14:529–534. doi: 10.1016/s0740-5472(97)00020-2. [DOI] [PubMed] [Google Scholar]
- Craig RJ. A psychometric study of the prevalence of DSM-III personality disorders among treated opiate addicts. International Journal of the Addictions. 1988;23:115–124. doi: 10.3109/10826088809085111. [DOI] [PubMed] [Google Scholar]
- Craig RJ, Bivens A, Olson R. MCMI-III derived typological analysis of cocaine and heroin addicts. Journal of Personality Assessment. 1997;69:583–595. doi: 10.1207/s15327752jpa6903_11. [DOI] [PubMed] [Google Scholar]
- Craig RJ, Olson RE. MCMI comparisons of cocaine and heroin addicts. Journal of Clinical Psychology. 1990;46:231–237. doi: 10.1002/1097-4679(199003)46:2<230::aid-jclp2270460217>3.0.co;2-7. [DOI] [PubMed] [Google Scholar]
- Craig RJ, Verinis JS, Wexler W. Personality characteristics of drug addicts and alcoholics on the Millon Clinical Multiaxial Inventory. Journal of Personality Assessment. 1985;49:156–160. doi: 10.1207/s15327752jpa4902_10. [DOI] [PubMed] [Google Scholar]
- Craig RJ, Weinberg D. Assessing alcoholics with the Millon Clinical Multiaxial Inventory: A review. Psychology of Addictive Behaviors. 1992a;6:200–208. [Google Scholar]
- Craig RJ, Weinberg D. Assessing drug abusers with the Millon Clinical Multiaxial Inventory: A review. Journal of Substance Abuse Treatment. 1992b;9:249–255. doi: 10.1016/0740-5472(92)90068-y. [DOI] [PubMed] [Google Scholar]
- Donat DC. Millon Clinical Multiaxial Inventory (MCMI) clusters for alcohol abusers: Further evidence of validity and implications for medical psychotherapy. Medical Psychotherapy. 1988;1:41–50. [Google Scholar]
- Donat DC, Walters J, Hume A. Personality characteristics of alcohol dependent inpatients: Relationship of MCMI subtypes to self-reported drinking behavior. Journal of Personality Assessment. 1991;57:335–344. doi: 10.1207/s15327752jpa5702_11. [DOI] [PubMed] [Google Scholar]
- Dubro AF, Wetzler S, Kahn MW. A comparison of three self-report inventories for the diagnosis of DSM-III personality disorders. Journal of Personality Disorders. 1988;2:256–266. [Google Scholar]
- Fals-Stewart W. Personality characteristics of substance abusers: An MCMI cluster typology of recreational drug users treated in a therapeutic community and its relationship to length of stay and outcome. Journal of Personality Assessment. 1992;59:515–527. doi: 10.1207/s15327752jpa5903_7. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured clinical interview for DSM–IV. Washington, DC: American Psychiatric Association; 1995. patient edition. [Google Scholar]
- Graham JR, Strenger VE. MMPI characteristics of alcoholics: A review. Journal of Consulting and Clinical Psychology. 1988;56:197–205. doi: 10.1037//0022-006x.56.2.197. [DOI] [PubMed] [Google Scholar]
- Greenstein RA, Fudala PJ, O’Brien CP. Alternative pharmacotherapies for opiate addiction. In: Lowinsohn JH, Ruiz P, Millman RB, Langrod JG, editors. Comprehensive textbook of substance abuse. 3rd ed. New York: Williams & Wilkins; 1997. pp. 415–425. [Google Scholar]
- Haller DL, Miles DR, Dawson KS. Psychopathology influences treatment retention among drug-dependent women. Journal of Substance Abuse Treatment. 2002;23:431–436. doi: 10.1016/s0740-5472(02)00283-0. [DOI] [PubMed] [Google Scholar]
- Higgins ST, Alessi SM, Dantona RL. Voucher-based incentives: A substance abuse treatment innovation. Addictive Behaviors. 2002;27:887–910. doi: 10.1016/s0306-4603(02)00297-6. [DOI] [PubMed] [Google Scholar]
- Higgins ST, Delaney DD, Budney AJ, Bickel WK, Hughes JR, Foerg F, Fenwick JW. A behavioral approach to achieving initial cocaine abstinence. American Journal of Psychiatry. 1991;148:1218–1224. doi: 10.1176/ajp.148.9.1218. [DOI] [PubMed] [Google Scholar]
- Jaffe AJ, Rounsaville B, Chang G, Schottenfeld RS, Meyer RE, O’Malley SS. Naltrexone, relapse prevention, and supportive therapy with alcoholics: An analysis of patient treatment matching. Journal of Consulting and Clinical Psychology. 1996;64:1044–1053. doi: 10.1037//0022-006x.64.5.1044. [DOI] [PubMed] [Google Scholar]
- Kadden RM, Cooney NL, Getter H, Litt MD. Matching alcoholics to coping skills or interactional treatments: Posttreatment results. Journal of Consulting and Clinical Psychology. 1989;57:698–704. doi: 10.1037//0022-006x.57.6.698. [DOI] [PubMed] [Google Scholar]
- Kadden RM, Litt MD, Cooney NL, Kabela E, Getter H. Prospective matching of alcoholic clients to cognitive-behavioral or interactional group therapy. Journal of Studies on Alcohol. 2001;62:359–369. doi: 10.15288/jsa.2001.62.359. [DOI] [PubMed] [Google Scholar]
- Kranzler HR, Rounsaville BJ, editors. Dual diagnosis and treatment: Substance abuse and comorbid medical and psychiatric disorders. New York: Marcel Dekker; 1998. [Google Scholar]
- Longabaugh R, Rubin A, Malloy P, Beattie M, Clifford PR, Noel N. Drinking outcome of alcohol abusers diagnosed as antisocial personality disorder. Alcoholism: Clinical and Experimental Research. 1994;18:410–416. doi: 10.1111/j.1530-0277.1994.tb00040.x. [DOI] [PubMed] [Google Scholar]
- Marsh DT, Stile SA, Stoughton NL, Trout-Landen BL. Psychopathology of addiction: Comparative data from the MMPI and MCMI. American Journal of Drug and Alcohol Abuse. 1988;14:17–27. doi: 10.3109/00952998809001532. [DOI] [PubMed] [Google Scholar]
- Matano RA, Locke KD, Schwartz K. MCMI personality subtypes for male and female alcoholics. Journal of Personality Assessment. 1994;63:250–264. doi: 10.1207/s15327752jpa6302_5. [DOI] [PubMed] [Google Scholar]
- Mayer GS, Scott KJ. An exploration of heterogeneity in an inpatient male alcoholic population. Journal of Personality Disorders. 1988;2:243–255. [Google Scholar]
- McLellan AT, Kucher H, Metzger D, Peters R, Smith I, Grisson G, Pettinati H, Argerious M. The fifth edition of the Addiction Severity Index. Journal of Substance Abuse Treatment. 1992;9:199–213. doi: 10.1016/0740-5472(92)90062-s. [DOI] [PubMed] [Google Scholar]
- McLellan AT, Luborsky L, Woody GE, O’Brien CP, Druley KA. Predicting response to alcohol and drug abuse treatments: Role of psychiatric severity. Archives of General Psychiatry. 1983;40:620–625. doi: 10.1001/archpsyc.1983.04390010030004. [DOI] [PubMed] [Google Scholar]
- McMahon RC, Kelley A, Kouzekanani K. Personality and coping style in the prediction of dropout from treatment for cocaine abuse. Journal of Personality Assessment. 1993;61:147–155. doi: 10.1207/s15327752jpa6101_11. [DOI] [PubMed] [Google Scholar]
- McMahon RC, Malow RM, Penedo FJ. Substance abuse problems, psychiatric severity, and HIV risk in Millon Clinical Multiaxial Inventory-II personality subgroups. Psychology of Addictive Behaviors. 1998;12:3–13. [Google Scholar]
- Messina N, Farabee D, Rawson R. Treatment responsivity of cocaine-dependent patients with antisocial personality disorder to cognitive-behavioral and contingency management interventions. Journal of Consulting and Clinical Psychology. 2003;71:320–329. doi: 10.1037/0022-006x.71.2.320. [DOI] [PubMed] [Google Scholar]
- Miller WR, DelBoca FK. Measurement of drinking behavior using the Form 90 family of instruments. Journal of Studies on Alcohol. 1994;12(Suppl.):112–118. doi: 10.15288/jsas.1994.s12.112. [DOI] [PubMed] [Google Scholar]
- Millon T. The Millon Clinical Multiaxial Inventory. 3rd ed. Minneapolis, MN: National Computer Systems; 1994. [Google Scholar]
- Millon T. Personality-guided therapy. New York: Wiley; 1999. [Google Scholar]
- Millon T, Davis RD. Disorders of personality: DSM–IV and beyond. New York: Wiley; 1996. [Google Scholar]
- O’Connor PG, Carroll KM, Shi JM, Schottenfeld RS, Kosten TR, Rounsaville BJ. Primary care based ambulatory opioid detoxification: Results of a clinical trial. Journal of General Internal Medicine. 1995;10:255–260. doi: 10.1007/BF02599882. [DOI] [PubMed] [Google Scholar]
- O’Connor PG, Waugh ME, Carroll KM, Diakogiannis IA, Schottenfeld RS, Rounsaville BJ. A randomized trial of three methods of primary-care based outpatient opioid detoxification. Annals of Internal Medicine. 1997;127:526–530. doi: 10.7326/0003-4819-127-7-199710010-00004. [DOI] [PubMed] [Google Scholar]
- Petry NM, Martin B, Cooney JL, Kranzler HR. Give them prizes, and they will come: Contingency management for treatment of alcohol dependence. Journal of Consulting and Clinical Psychology. 2000;68:250–257. doi: 10.1037//0022-006x.68.2.250. [DOI] [PubMed] [Google Scholar]
- Piersma HL. The MCMI as a measure of DSM-III axis II diagnoses: An empirical comparison. Journal of Clinical Psychology. 1987;43:478–483. doi: 10.1002/1097-4679(198709)43:5<478::aid-jclp2270430508>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- Preston KL, Silverman K, Umbricht A, DeJesus A, Montoya ID, Schuster CR. Improvement in naltrexone treatment compliance with contingency management. Drug and Alcohol Dependence. 1999;54:127–135. doi: 10.1016/s0376-8716(98)00152-5. [DOI] [PubMed] [Google Scholar]
- Repko GR, Cooper R. The diagnosis of personality disorder: A comparison of MMPI profile, Millon inventory, and clinical judgment in a workers’ compensation population. Journal of Clinical Psychology. 1985;41:867–881. doi: 10.1002/1097-4679(198511)41:6<867::aid-jclp2270410624>3.0.co;2-d. [DOI] [PubMed] [Google Scholar]
- Shaner A, Roberts LJ, Eckman TA, Tucker DE, Tsuang JW, Wilkins JN, Mintz J. Monetary reinforcement of abstinence from cocaine among mentally ill patients with cocaine dependence. Psychiatric Services. 1997;48:807–810. doi: 10.1176/ps.48.6.807. [DOI] [PubMed] [Google Scholar]
- Sigmon SC, Steingard S, Badger GJ, Anthony SL, Higgins ST. Contingent reinforcement of marijuana abstinence among individuals with serious mental illness: A feasibility study. Experimental and Clinical Psychopharmacology. 2000;8:509–517. doi: 10.1037//1064-1297.8.4.509. [DOI] [PubMed] [Google Scholar]
- Silverman K, Higgins ST, Brooner RK, Montoya ID, Cone EJ, Schuster C, Preston KL. Sustained cocaine abstinence in methadone maintenance patients through voucher-based reinforcement therapy. Archives of General Psychiatry. 1996;53:409–415. doi: 10.1001/archpsyc.1996.01830050045007. [DOI] [PubMed] [Google Scholar]
- Silverman K, Wong C, Umbricht-Schneiter A, Montoya I, Schuster C, Preston K. Broad beneficial effects of cocaine abstinence reinforcement among methadone patients. Journal of Consulting and Clinical Psychology. 1998;66:811–824. doi: 10.1037//0022-006x.66.5.811. [DOI] [PubMed] [Google Scholar]
- Stark MJ, Campbell BK. Personality, drug use and early attrition from substance abuse treatment. American Journal of Drug and Alcohol Abuse. 1988;14:475–485. doi: 10.3109/00952998809001565. [DOI] [PubMed] [Google Scholar]
- Torgersen S, Alnaes R. The relationship between the MCMI personality scales and DSM III Axis II. Journal of Personality Assessment. 1990;55:698–707. doi: 10.1080/00223891.1990.9674105. [DOI] [PubMed] [Google Scholar]
- Wetzler S, Dubro A. Diagnosis of personality disorders by the Millon Clinical Multiaxial Inventory. The Journal of Nervous and Mental Disease. 1990;178:261–263. doi: 10.1097/00005053-199004000-00008. [DOI] [PubMed] [Google Scholar]
- Widiger T, Sanderson C. The convergent and discriminant validity of the MCMI as a measure of DSM III personality disorders. Journal of Personality Assessment. 1987;51:228–242. doi: 10.1207/s15327752jpa5102_7. [DOI] [PubMed] [Google Scholar]
- Woody G, McLellan AT, Luborsky L, O’Brien CP. Sociopathy and psychotherapy outcome. Archives of General Psychiatry. 1985;42:1081–1086. doi: 10.1001/archpsyc.1985.01790340059009. [DOI] [PubMed] [Google Scholar]
- Woody GE, McLellan AT, Luborsky L, O’Brien CP. Psychotherapy in community methadone programs: A validation study. American Journal of Psychiatry. 1995;152:1302–1308. doi: 10.1176/ajp.152.9.1302. [DOI] [PubMed] [Google Scholar]
- Woody GE, McLellan AT, Luborsky L, O’Brien CP, Blaine J, Fox S, et al. Severity of psychiatric symptoms as a predictor of benefits from psychotherapy: The Veterans Administration-Penn Study. American Journal of Psychiatry. 1984;141:1172–1177. doi: 10.1176/ajp.141.10.1172. [DOI] [PubMed] [Google Scholar]