Abstract
Background/Aim:
Our aim was to evaluate the diagnostic accuracy of multi-detector row computerized tomography (MDCT) in staging of rectal cancer by comparing it to rectal endoscopic ultrasound (EUS).
Materials and Methods:
We prospectively included all patients with rectal cancer referred to our gastroenterology unit for staging of rectal cancer from December 2007 until February 2011, 53 patients whose biopsy had proven rectal cancer underwent both MDCT scan of the pelvis and rectal EUS. Both imaging modalities were compared and the agreement between T- and N-staging of the disease was assessed.
Results:
We staged 62 patients with rectal cancer during the study period. Of these, 53 patients met the inclusion criteria and were evaluated (25 women and 28 men). The mean age was 57.79 ± 14.99 years (range 21-87). MDCT had poor accuracy compared with EUS in T-staging with a low degree of agreement (kappa = 0.26), while for N-staging MDCT had a better accuracy and a moderate degree of agreement with EUS (kappa = 0.45).
Conclusions:
MDCT has a poor accuracy for predicting tumor invasion compared to EUS for T-staging while it has moderate accuracy for N-staging.
Keywords: Cancer staging, cancer, endoscopic ultrasound, multi-detector row computerized tomography, rectal
Colorectal cancer (CRC) is the most common gastrointestinal malignancy and the second cause of cancer-related deaths in North America.[1] CRC is the second most common cancer in Saudi males (accounting for 8.8% of all male cancers, with an average annual age standardized rate (ASR) of 7.2/100,000 population) and the third most common cancer in Saudi females (accounting for 7.6% of all cancers, with an average annual ASR of 6.1/100,000 population).[2]
Accurate staging of rectal cancer is necessary to provide the optimal treatment strategy. The prognosis of rectal cancer is related to several factors, such as the depth of tumoral invasion, number of metastatic lymph nodes, and the percentage of the circumference of the rectum involved by the tumor.[3,4] Pre-operative staging is of great importance for adequate management. 6-10% of patients with primary rectal cancer still experience intra-pelvic local recurrence with or without pre-operative neoadjuvant therapy,[5,6] however, therapy improves survival and diminishes recurrence rates in patients with locally advanced cancer (T3-4, N0 or N1-2).[7,8,9]
Assessment of the depth of cancer invasion (T-stage) in rectal cancer and the presence of lymph node involvement (N-stage) remains an important part in management of patients with rectal cancer.
Rectal endoscopic ultrasound (EUS) is a safe diagnostic method that allows both tumor invasion and lymph node involvement to be staged and significantly contributes to the selection of the optimum management strategy in patients with rectal cancer.[10] Reported EUS accuracy in rectal cancer varies between 69% and 97% for T-staging[11] and is 70-75% accurate for N-staging.[12] However, the accuracy of EUS is related to many factors, such as the operator's experience, tumor stenosis, peritumoral inflammation, hemorrhage, and the shape of the tumor itself whether it is villous or pedunculated. Even with these limitations EUS remains one of the most accurate techniques available for rectal tumor staging, it is found to be superior to computerized tomography (CT) scan and equivalent to magnetic resonance imaging (MRI).[13]
The current role of CT in patients with known colon cancer is controversial. Accuracy rates for pre-operative staging of colon cancer with CT have been disappointing. For the T-staging it ranges between 48% and 77%,[14,15,16,17,18] while for N-staging accuracy has ranged from 54% to 70%.[19] The use of contrast enhanced multi-detector row computerized tomography (MDCT) colonography has improved the staging accuracy.[20] At present, only a few MDCT studies have been published on the subject of rectal cancer staging although there are studies comparing CT and EUS, but the impact of MDCT was not evaluated on such a comparison.
The application of chemoradiation has become the initial treatment modality for locally advanced rectal cancer. This has created a methodological problem for the evaluation of the staging accuracy of new imaging techniques, due to tumor down staging by neoadjuvant therapy,[21,22,23,24] therefore, the traditional gold standard of histology is no longer valid.
Thus, the aim of this study was to evaluate the accuracy of MDCT for the prediction of T and N in rectal cancer staging with EUS as reference standard.
MATERIALS AND METHODS
The study was conducted at the King Khalid University Hospital, Riyadh, Saudi Arabia, which is considered one of the major teaching hospitals in the country and a major tertiary care center in Riyadh. Prospective EUS examinations performed for rectal cancers are stored in an electronic database. All patients with biopsy proven rectal carcinoma were included. The study period was from December 2007 until February 2011. Two endoscopists performed the EUS examinations in our endoscopy unit. Informed consent was obtained from all of the patients prior to the examination.
Patients were included if the distal margin of the tumor was within 15 cm from the anal verge[25,26] and was proven to be adenocarcinoma on biopsy. The staging by EUS and CT occurred prior to chemoradiation therapy, both were done within the same week with no preferential sequence. Patients with obstructive lesions were excluded from the study.
Rectal EUS
All the exams were performed using an ALOKA ProSound α 10 machine (7.5-10 MHz) and a 360° electronic radial scanning echoendoscope (Olympus, GF-UE160-AL5e), filling the transducer balloon with degassed water to enable coupling with the tumor. A second endoscopist was present during the procedure and the final staging of the tumor was made after the agreement of both. Both endoscopists were blinded to the MDCT results.
Patients were prepared with two 250-cc cleansing enemas administered 2 hours before the procedure. No sedation was given. EUS was carried out with the patients in the left lateral position. The bowel wall is represented in five sonographic layers as a result of differences in acoustic impedance.
Beginning with the lumen, the five layers are: (1) Hyperechoic layer from the interface between mucosa and ultrasound probe; (2) hypoechoic layer produced from the mucosa and muscularis mucosae; (3) hyperechoic layer corresponding to the submucosa; (4) hypoechoic layer corresponding to the muscularis propria; and (5) hyperechoic layer being the interface between the muscularis propria and perirectal fat/serosa.
The EUS staging corresponds to the TNM classification: (1) T1 is when the tumor is confined to mucosa and submucosa; (2) T2, when the tumor infiltrates the muscularis propria; (3) T3 is when the tumor invades the perirectal fat; and (4) T4 is when the tumor infiltrates surrounding organs.[27]
The echoendoscope was advanced to 20-25 cm from the anus for the detection of iliac lymph nodes. All detected lymph nodes, more than 5 mm in size, hypoechoic, rounded were considered to be suspicious for malignancy.[28]
MDCT scan of the pelvis
All patients were examined by CT using 16-MDCT (LightSpeed 16, GE Medical Systems, and Milwaukee, USA). A detailed consent was discussed with and signed by the patients. The protocol study included the acquisition of unenhanced images of the entire liver followed by acquisition of triple-phase contrast-material-enhanced images during the hepatic arterial phase, portal venous phase and delayed phase.[29] All CT acquisitions were started at the top of the liver and preceded in a craniocaudal direction during a single breath-hold on deep inspiration. Patients were instructed to hold their breath with tidal inspiration during acquisition. With slice thickness = 0.625 mm, interval 0.625 mm, pitch 1.35, 1 mm section overlapping every 0.7 mm. Contrast-enhanced images were obtained with a dose of 1.8 ml/kg body weight of non-ionic iodinated contrast material. Oral contrast was given after fasting for 6 hours as 3% diluted water-soluble contrast as 1 L given over 2 hours, one cup was given on table at the time of examination while rectal contrast was given diluted water-soluble contrast (15 cc of gastrografin diluted in 500 cc of water).
Statistical analysis
Pre-operative EUS and MDCT findings were compared to assess the concordance between the two methods. Kappa-statistics were used to check how well EUS and MDCT classified subjects in the T- and N-stage groups. The degree of agreement was quantified by weighted kappa, which assumes the categories (Tl, T2, etc.) are ordered and accounts for how far apart EUS and MDCT are in classifying them.
RESULTS
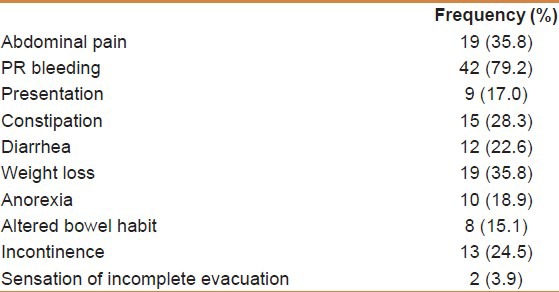
A total of 53 patients with rectal cancer were staged in our unit (25 females and 28 males). The mean age was 57.79 ± 14.99 (range 21-87). The main presenting symptoms were bleeding per rectum in 42 patients (79.2%) and abdominal pain in 19 patients (35.8%). There was a positive family history for colon cancer in 7 (13.2%) and 6 patients (11, 3%) had a past history of adenomas [Table 1].
Table 1.
Demographic data of 53 patients with rectal cancer
For T-staging, MDCT was found to under stage 14 patients (26%), while 6 patients (11%) were over staged. 30 patients (63%) were correctly staged compared with EUS. The agreement on T-staging between MDCT and EUS was found to be fair (kappa = 0.26).
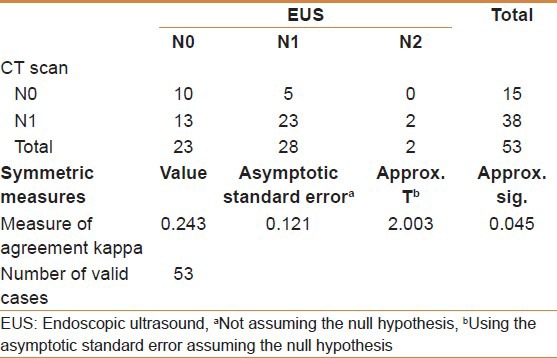
Regarding N-staging, MDCT under staged 7 patients (12%), over staged 13 patients (24%), while 33 patients (64%) were correctly staged compared with EUS. The degree of agreement between EUS and MDCT was found to be moderate (kappa = 0.45).
Tables 2 and 3 show the comparison of both MDCT and EUS for both T- and N-staging.
Table 2.
Comparing multi-detector row computerized tomography to endoscopic ultrasound for T-staging
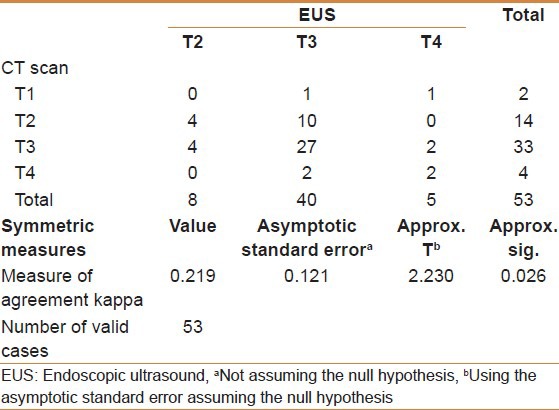
Table 3.
Comparing multi-detector row computerized tomography to endoscopic ultrasound for N-staging
DISCUSSION
The present study evaluated the accuracy of preoperative MDCT for determining the T- and N-stages for rectal cancer compared to EUS as a reference standard. We found a fair agreement between MDCT and EUS in T-staging of rectal cancer (kappa = 0.26), while there was moderate correlation for N-staging with kappa = 0.45.
Treatment options for rectal cancer depend on the stage at presentation.[30] Accurate preoperative staging is mandatory and mostly based on imaging.[31] CT, EUS, and MRI are the imaging modalities predominantly utilized for preoperative staging of rectal cancer.
EUS is one of the most accurate techniques for rectal cancer staging and has been in use since the early 1980s. EUSs overall accuracy was 81.8%.[32] Although, most of earlier studies had accuracies of 85-95% but in two large studies that included more than 400 patients the accuracy for nodal staging was 63.3% and 69%,[33,34] while for tumor staging it ranged from 70% to 75%.[35,36] EUS can distinguish the different anatomic layers of the bowel and thus, it appears to have advantages over both CT or MRI in assessing mural penetration and is invaluable in assessing patients considered for local resection. A meta-analysis by Bipat et al.,[37] also found that rectal EUS was the best technique for assessing local invasion. We do think that the role of these imaging modalities is complementary rather than competitive as there are studies that had found that EUS and MRI have similar accuracies in the staging of T2 and T3 tumors while MRI could not visualize T1 lesions, EUS under staged T4 lesions.[38]
New technological advances such as contrast-aided EUS and three-dimensional (3D) EUS may offer high accuracy for T- and N-staging in rectal cancer. 3D EUS consists of the traditional transverse scan as well as coronal and sagittal scans that allow for a multiplanar display, it also improves visualization of subtle protrusions of tumors infiltrating into adjacent tissues and organs, allowing for improved T- and N-staging. This procedure has been found to be superior to CT and two-dimensional EUS in accurately determining tumor margins.[39]
CT is unable to differentiate the different layers of the rectal wall and has lower overall predictive accuracy than EUS and MRI. Initial data showed CT T-staging accuracy of 79% to 94% in patients with primarily advanced T-stage disease,[40,41,42] while its accuracy fell to a range of 52-74% when a broader spectrum of tumor sizes were analyzed.[43,44,45] While nodal staging accuracy has ranged from 54% to 70%.[46,47]
The decrease in accuracy may have been due in part to the lack of detailed spatial and contrast resolution offered by standard CT imaging techniques, leading to diminished accuracy for early-stage lesions confined to the rectal wall. Although improvement in CT imaging (e.g., MDCT) has occurred, however, data are limited on whether such advances will result in improved locoregional staging accuracy.[20] In a study of 21 patients comparing MDCT with MRI an agreement of 95% was found between MDCT and histology,[48] while Kulinna, et al.,[49] reported an accuracy of 86% in a 92 patient study, A study by Taylor, et al., addressed the clinical important prediction of the tumor relationship to the MRI and reported a poor agreement between MDCT, MRI and histology (kappa 0.06-0.15) in 42 patients treated with a short course of radiotherapy (5 Gy × 5 Gy) or surgery only.[50] No study up to date compared the degree of agreement of MDCT and EUS in pre-operative staging of rectal cancer.
Although, the number of patients included in our study is not high, our aim was to know the utility and reliability of MDCT for pre-operative rectal cancer staging under usual daily conditions in our center with our experience, and we found that MDCT had a low diagnostic accuracy with poor agreement compared to EUS in T-staging.
Based on the current evidence, we feel that even with the advancement in imaging using MDCT, its accuracy is not optimal compared to EUS. Larger studies with different tumor invasion depths are needed.
CONCLUSION
MDCT has a poor accuracy for the identification of the tumor invasion of rectal cancer and moderate accuracy in nodal staging.
Footnotes
Source of Support: This project is supported by College of Medicine Research Center, Deanship of Scientific Research, King Saud University.
Conflict of Interest: None declared
REFERENCES
- 1.Akin O, Nessar G, Agildere AM, Aydog G. Preoperative local staging of rectal cancer with endorectal MR imaging: Comparison with histopathologic findings. Clin Imaging. 2004;28:432–8. doi: 10.1016/S0899-7071(03)00314-0. [DOI] [PubMed] [Google Scholar]
- 2.Gulf Center for Cancer Control and Prevention. 10-Year Cancer Incidence Among Nationals of the GCC States 1998-2007. 2011. [Accessed on 2012 Oct 3]. Available at http://rc.kfshrc.edu.sa/GCCCP2.asp .
- 3.Kim CK, Kim SH, Chun HK, Lee WY, Yun SH, Song SY, et al. Preoperative staging of rectal cancer: Accuracy of 3-Tesla magnetic resonance imaging. Eur Radiol. 2006;16:972–80. doi: 10.1007/s00330-005-0084-2. [DOI] [PubMed] [Google Scholar]
- 4.Wolberink SV, Beets-Tan RG, Nagtegaal ID, Wiggers T. Preoperative assessment of the circumferential margin in rectal cancer is more informative in treatment planning than the T stage. Tech Coloproctol. 2006;10:171–6. doi: 10.1007/s10151-006-0275-0. [DOI] [PubMed] [Google Scholar]
- 5.Bakx R, Visser O, Josso J, Meijer S, Slors JF, van Lanschot JJ. Management of recurrent rectal cancer: A population based study in greater Amsterdam. World J Gastroenterol. 2008;14:6018–23. doi: 10.3748/wjg.14.6018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Palmer G, Martling A, Cedermark B, Holm T. A population-based study on the management and outcome in patients with locally recurrent rectal cancer. Ann Surg Oncol. 2007;14:447–54. doi: 10.1245/s10434-006-9256-9. [DOI] [PubMed] [Google Scholar]
- 7.Harewood GC, Wiersema MJ, Nelson H, Maccarty RL, Olson JE, Clain JE, et al. A prospective, blinded assessment of the impact of preoperative staging on the management of rectal cancer. Gastroenterology. 2002;123:24–32. doi: 10.1053/gast.2002.34163. [DOI] [PubMed] [Google Scholar]
- 8.NIH Consensus Conference. Adjuvant therapy for patients with colon and rectal cancer. JAMA. 1990;264:1444–50. [PubMed] [Google Scholar]
- 9.Kapiteijn E, Marijnen CA, Nagtegaal ID, Putter H, Steup WH, Wiggers T, et al. Preoperative radiotherapy combined with total mesorectal excision for resectable rectal cancer. N Engl J Med. 2001;345:638–46. doi: 10.1056/NEJMoa010580. [DOI] [PubMed] [Google Scholar]
- 10.Siddiqui AA, Fayiga Y, Huerta S. The role of endoscopic ultrasound in the evaluation of rectal cancer. Int Semin Surg Oncol. 2006;3:36. doi: 10.1186/1477-7800-3-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Beets-Tan RG, Beets GL. Rectal cancer: How accurate can imaging predict the T stage and the circumferential resection margin? Int J Colorectal Dis. 2003;18:385–91. doi: 10.1007/s00384-003-0480-5. [DOI] [PubMed] [Google Scholar]
- 12.Harewood GC. Assessment of publication bias in the reporting of EUS performance in staging rectal cancer. Am J Gastroenterol. 2005;100:808–16. doi: 10.1111/j.1572-0241.2005.41035.x. [DOI] [PubMed] [Google Scholar]
- 13.Halefoglu AM, Yildirim S, Avlanmis O, Sakiz D, Baykan A. Endorectal ultrasonography versus phased-array magnetic resonance imaging for preoperative staging of rectal cancer. World J Gastroenterol. 2008;14:3504–10. doi: 10.3748/wjg.14.3504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Balthazar EJ, Megibow AJ, Hulnick D, Naidich DP. Carcinoma of the colon: Detection and preoperative staging by CT. AJR Am J Roentgenol. 1988;150:301–6. doi: 10.2214/ajr.150.2.301. [DOI] [PubMed] [Google Scholar]
- 15.Earls JP, Colon-Negron E, Dachman AH. Colorectal carcinoma in young patients: CT detection of an atypical pattern of recurrence. Abdom Imaging. 1994;19:441–5. doi: 10.1007/BF00206935. [DOI] [PubMed] [Google Scholar]
- 16.Freeny PC, Marks WM, Ryan JA, Bolen JW. Colorectal carcinoma evaluation with CT: Preoperative staging and detection of postoperative recurrence. Radiology. 1986;158:347–53. doi: 10.1148/radiology.158.2.3941861. [DOI] [PubMed] [Google Scholar]
- 17.Gazelle GS, Gaa J, Saini S, Shellito P. Staging of colon carcinoma using water enema CT. J Comput Assist Tomogr. 1995;19:87–91. doi: 10.1097/00004728-199501000-00017. [DOI] [PubMed] [Google Scholar]
- 18.Thompson WM, Halvorsen RA, Foster WL, Jr, Roberts L, Gibbons R. Preoperative and postoperative CT staging of rectosigmoid carcinoma. AJR Am J Roentgenol. 1986;146:703–10. doi: 10.2214/ajr.146.4.703. [DOI] [PubMed] [Google Scholar]
- 19.Guinet C, Buy JN, Ghossain MA, Sézeur A, Mallet A, Bigot JM, et al. Comparison of magnetic resonance imaging and computed tomography in the preoperative staging of rectal cancer. Arch Surg. 1990;125:385–8. doi: 10.1001/archsurg.1990.01410150107019. [DOI] [PubMed] [Google Scholar]
- 20.Maizlin ZV, Brown JA, So G, Brown C, Phang TP, Walker ML, et al. Can CT replace MRI in preoperative assessment of the circumferential resection margin in rectal cancer? Dis Colon Rectum. 2010;53:308–14. doi: 10.1007/DCR.0b013e3181c5321e. [DOI] [PubMed] [Google Scholar]
- 21.Habr-Gama A, de Souza PM, Ribeiro U, Jr, Nadalin W, Gansl R, Sousa AH, Jr, et al. Low rectal cancer: Impact of radiation and chemotherapy on surgical treatment. Dis Colon Rectum. 1998;41:1087–96. doi: 10.1007/BF02239429. [DOI] [PubMed] [Google Scholar]
- 22.Pucciarelli S, Toppan P, Friso ML, Russo V, Pasetto L, Urso E, et al. Complete pathologic response following preoperative chemoradiation therapy for middle to lower rectal cancer is not a prognostic factor for a better outcome. Dis Colon Rectum. 2004;47:1798–807. doi: 10.1007/s10350-004-0681-1. [DOI] [PubMed] [Google Scholar]
- 23.Chari RS, Tyler DS, Anscher MS, Russell L, Clary BM, Hathorn J, et al. Preoperative radiation and chemotherapy in the treatment of adenocarcinoma of the rectum. Ann Surg. 1995;221:778–86. doi: 10.1097/00000658-199506000-00016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Theodoropoulos G, Wise WE, Padmanabhan A, Kerner BA, Taylor CW, Aguilar PS, et al. T-level downstaging and complete pathologic response after preoperative chemoradiation for advanced rectal cancer result in decreased recurrence and improved disease-free survival. Dis Colon Rectum. 2002;45:895–903. doi: 10.1007/s10350-004-6325-7. [DOI] [PubMed] [Google Scholar]
- 25.Hayne D, Brown RS, McCormack M, Quinn MJ, Payne HA, Babb P. Current trends in colorectal cancer: Site, incidence, mortality and survival in England and Wales. Clin Oncol (R Coll Radiol) 2001;13:448–52. doi: 10.1053/clon.2001.9311. [DOI] [PubMed] [Google Scholar]
- 26.Salerno G, Daniels IR, Moran BJ, Wotherspoon A, Brown G. Clarifying margins in the multidisciplinary management of rectal cancer: The MERCURY experience. Clin Radiol. 2006;61:916–23. doi: 10.1016/j.crad.2006.06.005. [DOI] [PubMed] [Google Scholar]
- 27.Kumar A, Scholefield JH. Endosonography of the anal canal and rectum. World J Surg. 2000;24:208–15. doi: 10.1007/s002689910034. [DOI] [PubMed] [Google Scholar]
- 28.Beynon J, Mortensen NJ, Foy DM, Channer JL, Virjee J, Goddard P. Pre-operative assessment of local invasion in rectal cancer: Digital examination, endoluminal sonography or computed tomography? Br J Surg. 1986;73:1015–7. doi: 10.1002/bjs.1800731228. [DOI] [PubMed] [Google Scholar]
- 29.Horton KM, Abrams RA, Fishman EK. Spiral CT of colon cancer: Imaging features and role in management. Radiographics. 2000;20:419–30. doi: 10.1148/radiographics.20.2.g00mc14419. [DOI] [PubMed] [Google Scholar]
- 30.Lindmark G, Gerdin B, Påhlman L, Bergström R, Glimelius B. Prognostic predictors in colorectal cancer. Dis Colon Rectum. 1994;37:1219–27. doi: 10.1007/BF02257785. [DOI] [PubMed] [Google Scholar]
- 31.Nicholls RJ, Mason AY, Morson BC, Dixon AK, Fry IK. The clinical staging of rectal cancer. Br J Surg. 1982;69:404–9. doi: 10.1002/bjs.1800690716. [DOI] [PubMed] [Google Scholar]
- 32.Skandarajah AR, Tjandra JJ. Preoperative loco-regional imaging in rectal cancer. ANZ J Surg. 2006;76:497–504. doi: 10.1111/j.1445-2197.2006.03744.x. [DOI] [PubMed] [Google Scholar]
- 33.Garcia-Aguilar J, Pollack J, Lee SH, Hernandez de Anda E, Mellgren A, Wong WD, et al. Accuracy of endorectal ultrasonography in preoperative staging of rectal tumors. Dis Colon Rectum. 2002;45:10–5. doi: 10.1007/s10350-004-6106-3. [DOI] [PubMed] [Google Scholar]
- 34.Marusch F, Koch A, Schmidt U, Zippel R, Kuhn R, Wolff S, et al. Routine use of transrectal ultrasound in rectal carcinoma: Results of a prospective multicenter study. Endoscopy. 2002;34:385–90. doi: 10.1055/s-2002-25292. [DOI] [PubMed] [Google Scholar]
- 35.Hildebrandt U, Klein T, Feifel G, Schwarz HP, Koch B, Schmitt RM. Endosonography of pararectal lymph nodes. In vitro and in vivo evaluation. Dis Colon Rectum. 1990;33:863–8. doi: 10.1007/BF02051923. [DOI] [PubMed] [Google Scholar]
- 36.Guinet C, Ghossain M, Buy JN, Sézeur A, Mallet A, Bigot JM, et al. Comparative study of MRI and X-ray computed tomography in the preoperative evaluation of rectal carcinoma. J Radiol. 1990;71:357–63. [PubMed] [Google Scholar]
- 37.Bipat S, Glas AS, Slors FJ, Zwinderman AH, Bossuyt PM, Stoker J. Rectal cancer: Local staging and assessment of lymph node involvement with endoluminal US, CT, and MR imaging: A meta-analysis. Radiology. 2004;232:773–83. doi: 10.1148/radiol.2323031368. [DOI] [PubMed] [Google Scholar]
- 38.Fernández-Esparrach G, Ayuso-Colella JR, Sendino O, Pagés M, Cuatrecasas M, Pellisé M, et al. EUS and magnetic resonance imaging in the staging of rectal cancer: A prospective and comparative study. Gastrointest Endosc. 2011;74:347–54. doi: 10.1016/j.gie.2011.03.1257. [DOI] [PubMed] [Google Scholar]
- 39.Kim JC, Kim HC, Yu CS, Han KR, Kim JR, Lee KH, et al. Efficacy of 3-dimensional endorectal ultrasonography compared with conventional ultrasonography and computed tomography in preoperative rectal cancer staging. Am J Surg. 2006;192:89–97. doi: 10.1016/j.amjsurg.2006.01.054. [DOI] [PubMed] [Google Scholar]
- 40.Thoeni RF, Moss AA, Schnyder P, Margulis AR. Detection and staging of primary rectal and rectosigmoid cancer by computed tomography. Radiology. 1981;141:135–8. doi: 10.1148/radiology.141.1.7291518. [DOI] [PubMed] [Google Scholar]
- 41.van Waes PF, Koehler PR, Feldberg MA. Management of rectal carcinoma: Impact of computed tomography. AJR Am J Roentgenol. 1983;140:1137–42. doi: 10.2214/ajr.140.6.1137. [DOI] [PubMed] [Google Scholar]
- 42.Hodgman CG, MacCarty RL, Wolff BG, May GR, Berquist TH, Sheedy PF, 2nd, et al. Preoperative staging of rectal carcinoma by computed tomography and 0.15T magnetic resonance imaging. Preliminary report. Dis Colon Rectum. 1986;29:446–50. doi: 10.1007/BF02561581. [DOI] [PubMed] [Google Scholar]
- 43.Shank B, Dershaw DD, Caravelli J, Barth J, Enker W. A prospective study of the accuracy of preoperative computed tomographic staging of patients with biopsy-proven rectal carcinoma. Dis Colon Rectum. 1990;33:285–90. doi: 10.1007/BF02055469. [DOI] [PubMed] [Google Scholar]
- 44.Goldman S, Arvidsson H, Norming U, Lagerstedt U, Magnusson I, Frisell J. Transrectal ultrasound and computed tomography in preoperative staging of lower rectal adenocarcinoma. Gastrointest Radiol. 1991;16:259–63. doi: 10.1007/BF01887361. [DOI] [PubMed] [Google Scholar]
- 45.Cova M, Frezza F, Pozzi-Mucelli RS, Ukmar M, Tarjan Z, Melato M, et al. Computed tomography and magnetic resonance in the preoperative staging of the spread of rectal cancer. A correlation with the anatomicopathological aspects. Radiol Med. 1994;87:82–9. [PubMed] [Google Scholar]
- 46.Butch RJ, Stark DD, Wittenberg J, Tepper JE, Saini S, Simeone JF, et al. Staging rectal cancer by MR and CT. AJR Am J Roentgenol. 1986;146:1155–60. doi: 10.2214/ajr.146.6.1155. [DOI] [PubMed] [Google Scholar]
- 47.Adams DR, Blatchford GJ, Lin KM, Ternent CA, Thorson AG, Christensen MA. Use of preoperative ultrasound staging for treatment of rectal cancer. Dis Colon Rectum. 1999;42:159–66. doi: 10.1007/BF02237121. [DOI] [PubMed] [Google Scholar]
- 48.Matsuoka H, Nakamura A, Masaki T, Sugiyama M, Takahara T, Hachiya J, et al. A prospective comparison between multidetector-row computed tomography and magnetic resonance imaging in the preoperative evaluation of rectal carcinoma. Am J Surg. 2003;185:556–9. doi: 10.1016/s0002-9610(03)00067-9. [DOI] [PubMed] [Google Scholar]
- 49.Kulinna C, Eibel R, Matzek W, Bonel H, Aust D, Strauss T, et al. Staging of rectal cancer: Diagnostic potential of multiplanar reconstructions with MDCT. AJR Am J Roentgenol. 2004;183:421–7. doi: 10.2214/ajr.183.2.1830421. [DOI] [PubMed] [Google Scholar]
- 50.Taylor A, Slater A, Mapstone N, Taylor S, Halligan S. Staging rectal cancer: MRI compared to MDCT. Abdom Imaging. 2007;32:323–7. doi: 10.1007/s00261-006-9081-4. [DOI] [PubMed] [Google Scholar]


