Sir,
We describe isolation of Epstein-Barr virus by aqueous PCR in a case of fulminant retinochoroiditis with prominent choroidal effusions as an atypical feature.
Case report
A sixty-five-year-old woman with primary open-angle glaucoma and previous bilateral augmented trabeculectomies presented with a painful, red left eye with decreased vision. She had been diagnosed with aplastic anaemia 1 year previously and was undergoing systemic immunosuppression (mycophenolate mofetil) in preparation for an anti-thymocyte globulin transfusion, receiving long-term prophylactic ciprofloxacin, acyclovir, and itraconazole. At presentation she had neutropaenia (0.07 × 109/l), thrombocytopaenia (13 × 109/l), and low reticulocytes (3 × 109/l).
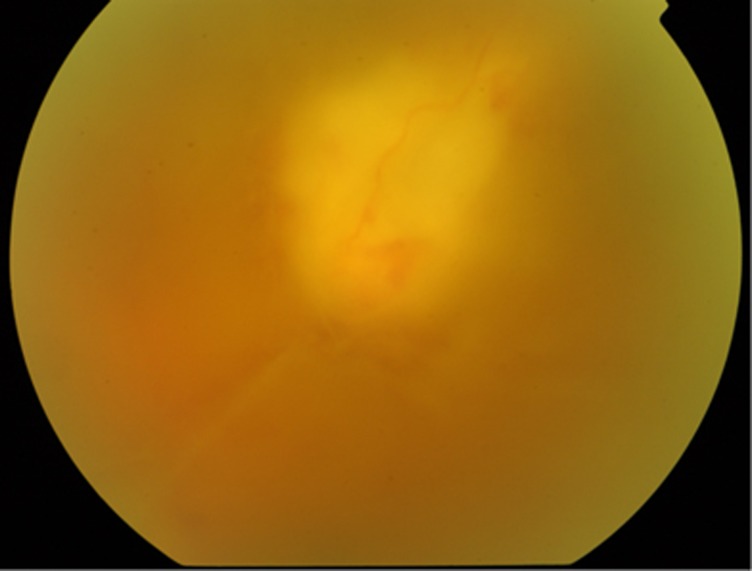
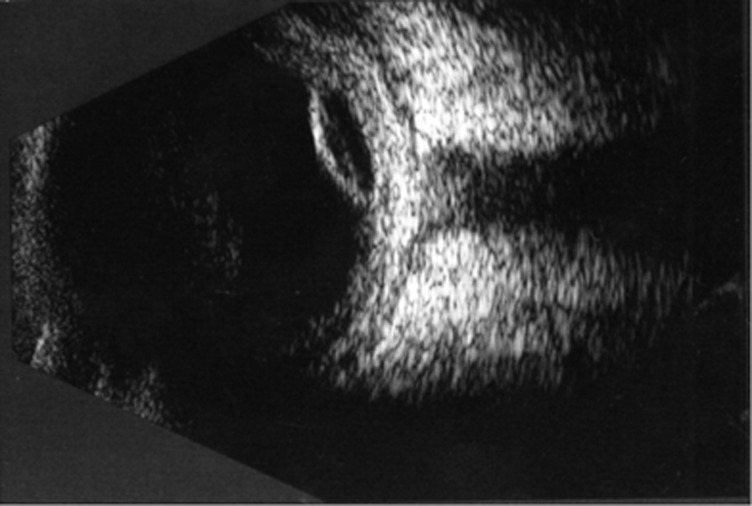
Visual acuity in the right eye was 6/6, while the left was light perception. A left afferent pupillary defect was present with anterior uveitis and hypotony (intraocular pressure right eye 11 mm Hg, left 7 mm Hg). There was no associated blebitis. Fundal examination revealed vitritis, focal retinitis (Figure 1) and localised choroidal effusions (Figure 2). A diagnosis of retinochoroiditis was made.
Figure 1.
Focal retinitis with haemorrhagic arteriolitis in the region of the superotemporal vascular arcade. The view is partially obscured by marked vitiritis.
Figure 2.
Localised choroidal effusion at presentation.
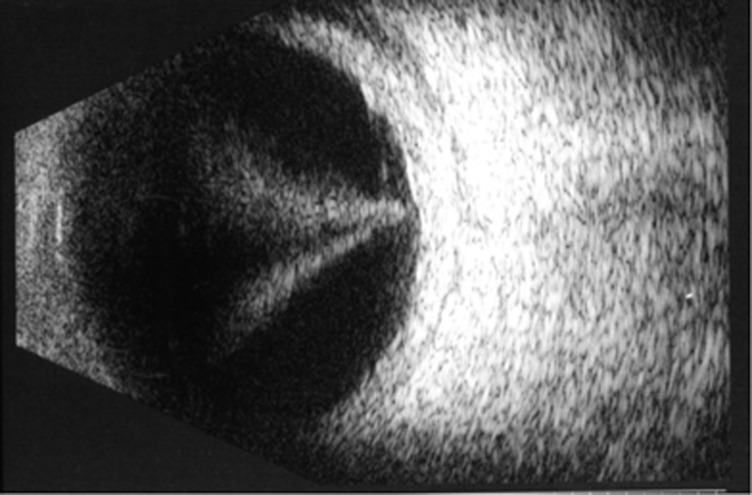
Empirical intravenous acyclovir 10 mg/kg tds was commenced along with topical dexamethazone 0.1% and cyclopentolate. An anterior chamber paracentesis was performed and quantitative aqueous polymerase chain reaction (PCR) analysis detected Epstein–Barr Virus (EBV) DNA. PCR was negative for toxoplasma, herpes simplex virus, varicella zoster virus, and cytomegalovirus. EBV was not detected in peripheral blood PCR. She was known to have EBV carrier status at the time aplastic anaemia was first diagnosed. Despite adjuvant high-dose oral prednisolone the choroidal effusions progressed to involve the posterior pole (Figure 3). Final acuity in the left eye remained at perception of light only. The effusions resolved but the eye remained hypotonous. The right eye remains unaffected at follow-up and she is maintained on a 1-year prophylactic course of oral famciclovir.
Figure 3.
Progression of funnel-shaped retinochoroidal effusions to involve entire posterior pole 3 weeks after presentation.
Comment
Clinical features of multifocal retinochoroiditis have been described in association with presumptive ocular EBV infection,1 but diagnosis is usually based on serologic evidence of specific EBV antibodies.2, 3 Lau et al4 identified EBV by vitreous sample PCR in two patients with acute retinal necrosis, however, to our knowledge there are no previous reports of EBV having been isolated from aqueous PCR. With our patient, choroidal effusions were a prominent feature along with focal retinitis; infiltration by cytotoxic polyclonal EBV-infected lymphocytes in the acute phase may be responsible.5 EBV is a rare cause of retinochoroiditis and the most of the described cases have occurred in conjunction with haematological disease. Aciclovir has relatively low efficacy against EBV, as such our patient was commenced on famciclovir prophylaxis. It is, therefore, important for clinicians to include EBV in the PCR panel of such patients in order to optimise therapy.
The authors declare no conflict of interest.
References
- Kelly SP, Rosenthal AR, Nicholson KG, Woodward CG. Retinochoroiditis in acute Epstein-Barr Virus infection. Br J Ophthalmol. 1989;73:1002–1003. doi: 10.1136/bjo.73.12.1002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kramer S, Brummer C, Zierhut M. Epstein-Barr Virus associated acute retinal necrosis. Br J Ophthalmol. 2001;85:114. doi: 10.1136/bjo.85.1.110d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tran THC, Rozenberg F, Cassoux N, Rao NA, LeHoang P, Bodaghi B. Polymerase chain reaction analysis of aqueous humour samples in necrotising retinitis. Br J Ophthalmol. 2003;87 (1:79–83. doi: 10.1136/bjo.87.1.79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lau CH, Missotten T, Salzmann J, Lightman SL. Acute retinal necrosis features, management, and outcomes. Ophthalmology. 2007;114 (4:756–762. doi: 10.1016/j.ophtha.2006.08.037. [DOI] [PubMed] [Google Scholar]
- Hershberger VS, Hutchins RK, Witte DP, Schneider S, Harris RE, McGonegle SJ. Epstein Barr Virus-related bilateral acute retinal necrosis in a patient with X-linked lymphoproliferative disorder. Arch Ophthalmol. 2003;121:1047–1049. doi: 10.1001/archopht.121.7.1047. [DOI] [PubMed] [Google Scholar]