SUMMARY
Rhinoplasty is one of the most difficult aesthetic surgery procedures with a high rate of revision. In revision rhinoplasty the surgeon should explore the patient's concerns and then verify the possibility to satisfy expectations after complete internal and external examination of the nose. For the vast majority of complex secondaries, an open approach is the only reasonable method. In fact, in secondary nasal surgery, because of the scarring process following the primary operation, dissection is tedious, and landmarks are lost. One of the main objectives for the surgeon who approaches secondary rhinoplasty is to restore the structural support of the nose and to replace the lost volume of soft tissues. To achieve this purpose, the surgeon must often rely on grafts. An ideal grafting material must be easy to sculpt, resistant to trauma, infection and extrusion, mechanically stable, inert and readily available. For all these reasons, autogenous cartilage grafts harvested from septum, auricular concha and rib represent the first choice in rhinoplasty. In order to obtain a camouflage graft that provides natural contouring to the nose, temporalis fascia can be used. All these carefully trimmed grafts are useful in tip revision surgery, in secondary surgery of the dorsum and to resolve or reduce functional problems.
KEY WORDS: Revision rhinoplasty, Open technique, Autogenous cartilage grafts, Tip plasty, Dorsum revision
RIASSUNTO
La rinoplastica è una delle procedure più complesse della chirurgia estetica e pertanto risulta gravata da un alto tasso di revisioni. Nella rinoplastica di revisione il chirurgo deve indagare le preoccupazioni del paziente e quindi verificare la possibilità di soddisfarne le aspettative con un'accurata valutazione pre-operatoria estetica e funzionale del naso. Nella maggioranza dei casi di rinoplastiche secondarie, l'approccio aperto risulta l'unico ragionevole. Infatti i processi di cicatrizzazione successivi al primo intervento rendono la dissezione difficoltosa e non consentono una facile identificazione dei reperi anatomici. Uno degli obiettivi principali del chirurgo che approccia la rinoplastica secondaria è il ripristino del supporto strutturale del naso per restituire il volume perso dai tessuti molli. Per raggiungere tale scopo spesso il chirurgo deve affidarsi a innesti. L'innesto ideale deve essere facile da scolpire, resistente a traumi, infezioni ed estrusioni, meccanicamente stabile, inerte e facilmente prelevabile. Per questi motivi, gli innesti di cartilagine autologa prelevati dal setto, dalla conca auricolare e dalla costa, rappresentano la prima scelta in rinoplastica. Inoltre la fascia temporale risulta utile per ottenere un effetto di "camouflage" degli innesti conferendo un aspetto più naturale al naso. Tutti questi innesti, adeguatamente preparati e rifiniti sulla base delle specifiche esigenze, trovano largo impiego nella chirurgia di revisione della punta e del dorso e nel risolvere o ridurre eventuali problemi funzionali.
Introduction
There is no doubt that any secondary operation is typically more challenging that the primary event. What makes secondary rhinoplasty so difficult? Certain factors are obvious: number of prior operations, number of different surgeons, availability of septum, skin thickness, etc. The critical issue is that there is little idea of what was done or available in a secondary case until the area is exposed. There is consensus that rhinoplasty is one of the most difficult aesthetic surgery procedures with a high rate of revision (up to 21%) 1-4.
Preoperative evaluation
The most important consideration in revision rhinoplasty is determining what the patient's concerns are and then verifying the validity of the complaint with complete internal and external examination of the nose. Clearly, there are instances where patient's expectations or complaints are less than reasonable or appropriate.
Once the patient's complaints have been determined, a full examination of the nose is performed. The surgeon begins with external examination. Quality and thickness of the skin must be recorded. A thick skin envelope has always been considered a major limiting factor for achieving both tip definition and the desired profile line. In case of thick skin, every imperfection shows, and nothing is hidden. When the tip is extremely thin, a "fascial blanket" is placed beneath the dorsum and over the entire tip lobule 5.
Presence of abnormalities such as bossae, convexities or concavities along dorsal side walls, degree of projection and rotation of the nose, and dorsal profile must be addressed. Another important consideration is the status of the septum: is it still there? Most revision rhinoplasty procedures require grafting. If the nasal septum is still present, then it can be used.
Assessment of the inferior turbinates must also be done during internal examination of the nose, since hypertrophic turbinates often cause airflow restriction. Midvault narrowing following a rhinoplasty can collapse the internal nasal valve leading to restriction of airflow. During consultation, a treatment plan should be formulated regarding the sequence of revision surgery. A road map can be created (Fig. 1).
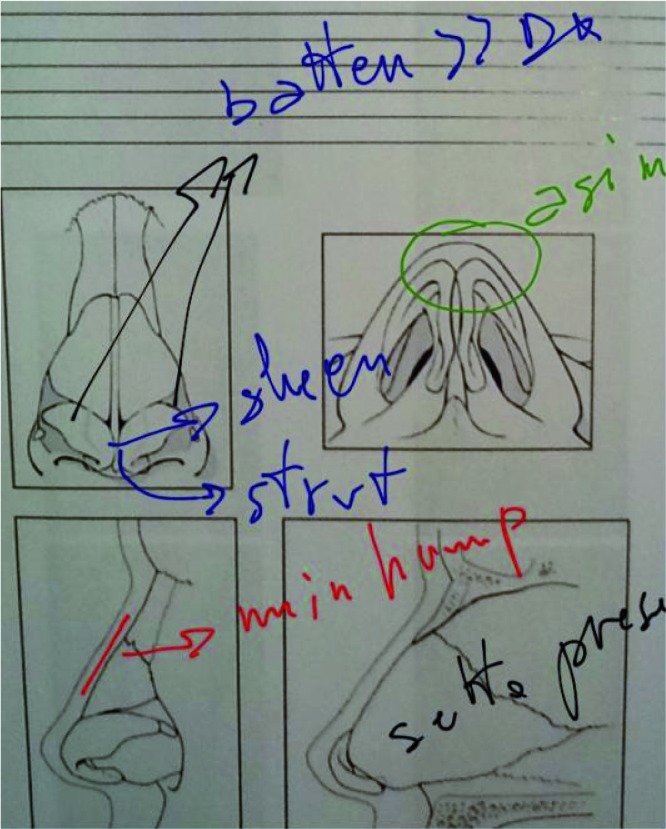
Fig. 1.
Example of personal note table: demolition/resection (red), correction (green), graft insertion (blue).
Grafting materials
In revision rhinoplasty, one of the goals for the surgeon is to restore the structural support of the nose and to replace lost soft tissue volume 6. In order to achieve this goal, the surgeon must often rely on grafts. Numerous graft materials are available in revision rhinoplasty, and each has unique chemical, physical and biological properties. An ideal grafting material must be easy to sculpt, resistant to trauma, infection and extrusion, mechanically stable, inert and readily available. Available grafts are classified as non-synthetic grafts (including autogenous and homologous grafts) and alloplast implants.
In our experience, the autogenous graft represents the first choice in rhinoplasty because of its favourable long-term clinical outcome and the low immunologic response. Autogenous grafts are harvested from tissues of the same individual and include cartilage, bone and subcutaneous tissue.
Autogenous cartilage grafts remain the primary choice in rhinoplasty surgery. These grafts cause minimal inflammatory response and graft infection, and resorption and extrusion rates are low 7 8. Cartilage characteristics make the graft useful for augmenting soft tissue and for restoring nasal architecture. It can be harvested from septum, auricular concha and rib. Septal cartilage remains, in our experience, the graft of choice in revision rhinoplasty, but obviously this donor site is often limited 9 10 (Fig. 2). It is not uncommon to examine a patient for revision surgery and realize that the patient no longer has any nasal septum available for grafting 11 12. This is a difficult situation, since most revision rhinoplasties require some level of augmentation to correct what has been taken away. For this reason, conchal cartilage is typically a precious site in secondary rhinoplasty. This cartilage is pliable and its thickness is highly variable 13 (Fig. 3).
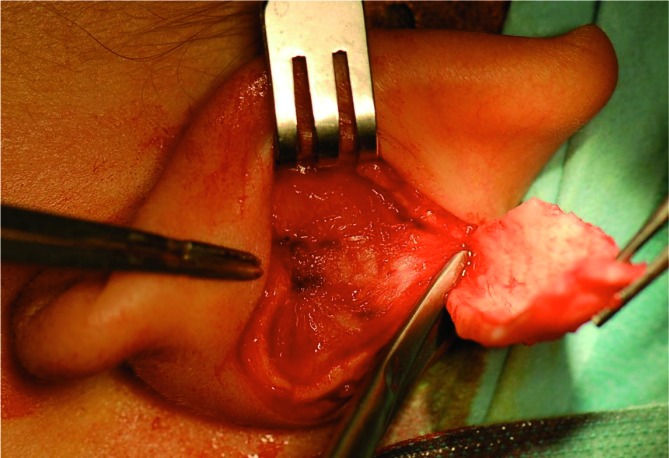
Fig. 2.
Septal cartilage.
Fig. 3.
Auricular cartilage.
Costal cartilage provides ample quantities of autogenous cartilage, but is frequently associated with warping. It is harvested from the sixth or seventh rib with an inframammary incision 14. An important limitation in the use of costal cartilage depends on its ossification in the elderly. The potential complications associated with costal cartilage include pneumothorax, post-operative pain, chest wall deformities and untoward scarring 15. In our hands, rib cartilage is a third choice solution, and its use is advisable only in the case that multilayer harvesting is feasible.
In order to obtain a camouflage graft that provides natural contouring to the nose, temporalis fascia can also be used.
This fascia can be harvested via postauricular incision and can be laid over grafts obtaining soft tissue augmentation in dorsum and tip 16. The fascia graft can also be harvested through a 2.5 cm incision anterior to the auricle 17.
In our opinion, the use of homologous grafts (irradiated rib and alloderm) and alloplast implants (expanded-porous polytetrafluoroethylene, porous high-density polyethylene and silicone) must be avoided in rhinoplasty surgery. All these materials are less physiological and elicit an immunological response that can cause damage to surrounding tissues and extrusion of the foreign body 18-20 (Fig. 4).
Fig. 4.
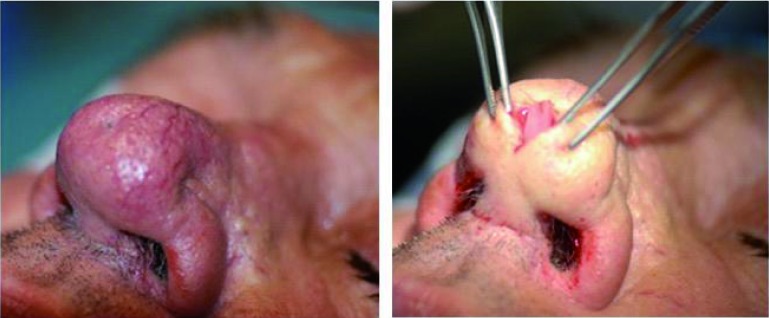
Alloplast implant extrusion.
Surgical technique
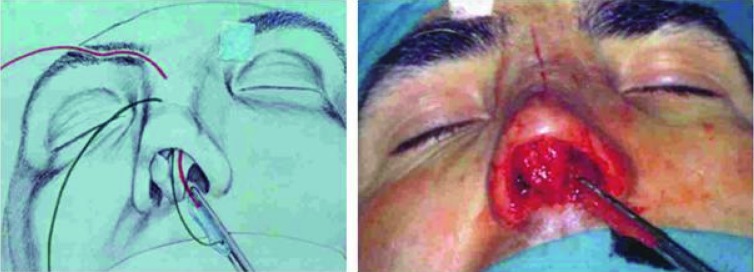
Revision nasal surgery is a difficult operation because of the scarring process following the primary operation; dissection is tedious, and landmarks are lost 21 22. For the vast majority of complex secondaries, an open approach is the only reasonable method. There is no question that an open technique will offer an extended view and access to nearly the entire nasal complex, thereby allowing precise manoeuvres and placement of sutures and grafts (Fig. 5). The natural plane of dissection between the lower cartilages and overlying skin envelope is lost. Once the nasal complex has been degloved via an open technique, a clear view of the underlying anatomy becomes evident.
Fig. 5.

Open approach in primary rhinoplasty and revision rhinoplast.
Revision septoplasty
First of all, every primary septal deformity that was not treated previously must be corrected. The structures are often distorted and scarred from previous manipulation, prior resections may have weakened the critical L-shape strut, and a maximum amount of graft materials is needed. The actual indications for septal surgery are somewhat constant: correction of anatomical obstruction and/or harvest of graft material 5.
Tip revision
Tip surgery can vary enormously in secondary cases from literally nothing to total reconstruction. Tip plasty can be done through cephalic trim of the lateral crura to achieve tip rotation, along with transdomal suturing and placement of shield grafts. To combat or avoid tip ptosis, columellar strut grafts should always be used. This is especially true in revision surgery if lack of tip support and projection is noted preoperatively. Columellar struts are an essential part of all secondary tip surgeries (Fig. 6).
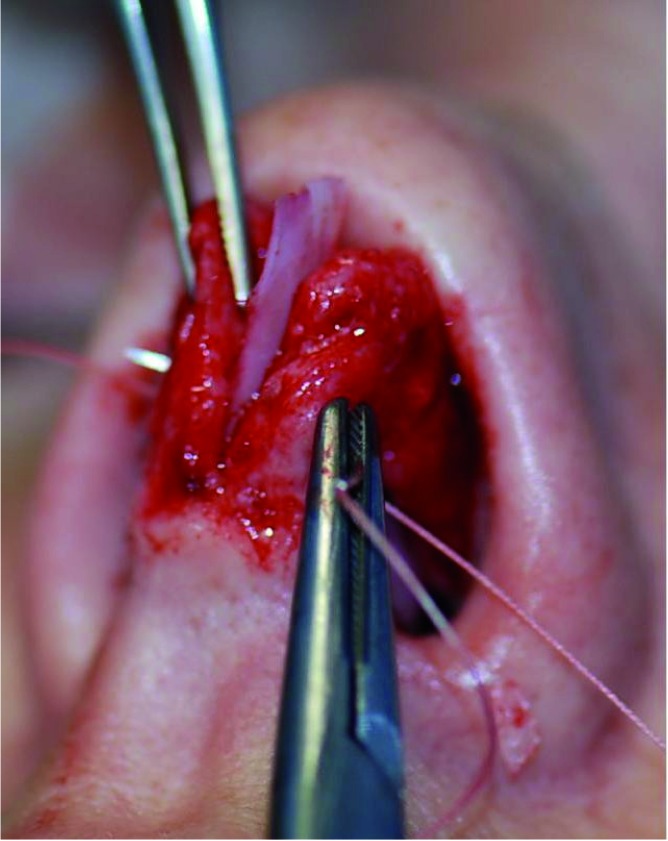
Fig. 6.
Columellar graft.
The alar cartilages are often highly scarred or distorted and often need to be reinforced. Whenever possible, septal cartilage is the donor material of choice. Rigidity and structural support is essential. Tip grafts are designed to change definition or projection or to show a distinct change in the tip and to overcome a scarred or thick skin envelope 5. A strong solid shield tip graft is the graft of choice. In primary cases, the tip graft can always be made from septal cartilage, whereas in secondary cases conchal cartilage may be necessary. To overcome the convexity of the conchae, a double piece of cartilage (which is usually very thin) sutured together in a symmetrical way can be used.
The graft is tapered to fit within the divergence of the crura. Graft placement can vary from integration to high projection depending upon the desired tip definition. As the graft rises above the alar domes, a solid "backstop" or cap graft must be added. Since in secondary procedures more than one parameter appears to be wrong, tip grafting is mandatory, highly valuable and generally multiple. In our hands, a shield graft is most often employed, and it must be tailored to a bigger size than needed (to be trimmed and corrected up to the desired dimensions), but it is often insufficient to overcome the whole range of defects. Thereby, one has to be familiar with other good solutions, to be used in addition, such as a Peck graft, a Sheen graft or one/multiple camouflage grafts (Fig. 7).
Fig. 7.
Tip shield graft before definitive trimming (a) and double cross graft to define the tip-columellar relationship (b).
Dorsum revision
When planning secondary surgery of the dorsum, one must add straightening, smoothing and camouflage of the dorsum to the primary choices of reduction, augmentation or balance. The skin envelope over the dorsum becomes a critical issue, usually revealing thinness over the rhinion or thickness in the supratip area.
A polly beak deformity is one of the most common reasons for revision rhinoplasty. The deformity is seen when the area of the supratip break projects ahead of the nasal tip in the plane of the nasal dorsum. This gives the illusion of a bulbous ptotic tip with no supratip break 23. Two reasons are primarily responsible for this: underresection of the dorsum in the region of the supratip (anterior septal angle) and distruption of the tip supporting structures resulting in depression of the nasal tip postoperatively. In cases of underresection at the anterior septal angle, reduction can be easily performed. In cases of disruption of tip supporting structures, tip support must be obtained. Support may be lost during primary rhinoplasty for several reasons, such as overresected lower lateral cartilages, disarticulation of lower later cartilages from the caudal septum, scroll area violation, or simply a lack of additional supporting struts when indicated for poor tissue quality 24. The loss of tip projection and resultant supratip fullness may lead the surgeon to resect more anterior caudal septum, when it may actually be necessary to increase tip projection with grafting techniques. Incorrect planning in this field can place the surgeon in a tricky situation, having reduced every single dimension of the nose, with a completely unsatisfactory outcome. As a consequence, meticulous analyses of the preoperative situation is needed through a thorough examination and a complete series of pictures. In our hands, computer simulation through a large series of measures and dedicated software is mandatory and personally recommended.
The nasal dorsum is often excessively reduced. One of the more difficult sequelae resulting from overresection is a saddle nose deformity. Restoration of form often involves nasal dorsal reconstruction in the form of a dorsal onlay graft 25 (Figs. 8, 9).
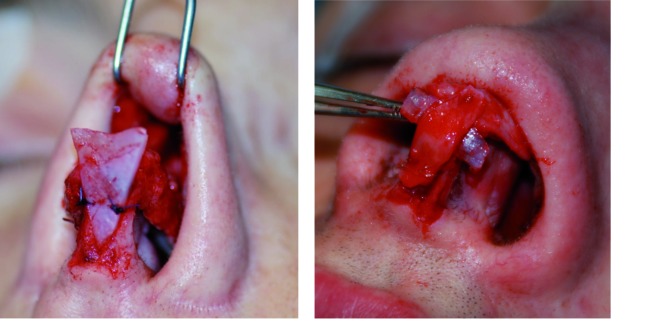
Fig. 8.

Overlay multilayer dorsal graft sutured to the cartilagineous dorsum.
Fig. 9.
Dorsal graft sutured to the dorsal skin.
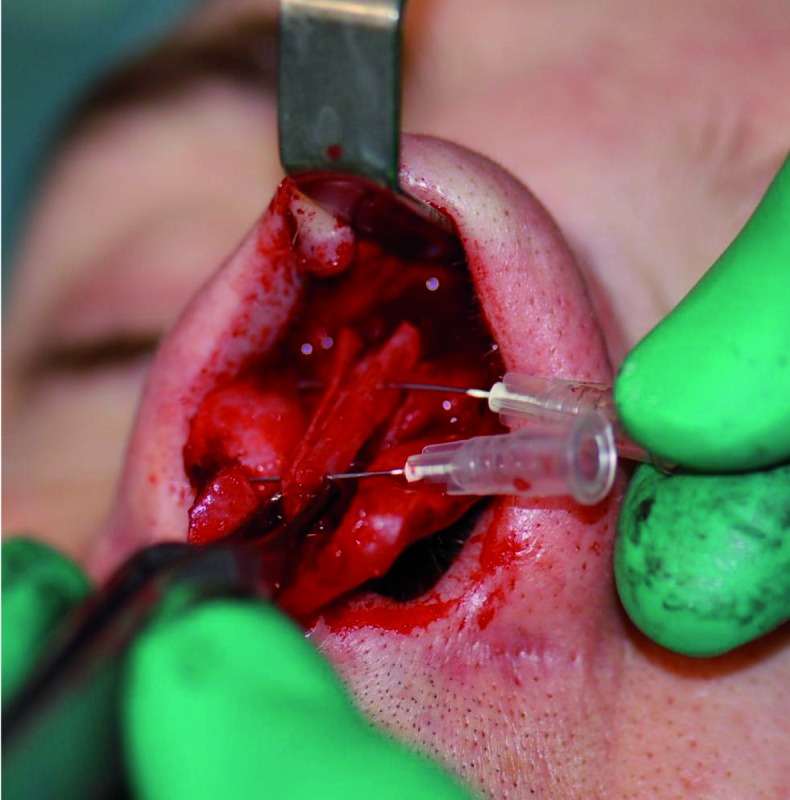
Several different solutions are available, starting with a very simple overlay graft (in a single or multilayer slice), which we suggest to suture very carefully to the upper lateral cartilages to avoid any kind of shifting or, at the end of the procedure, to the dorsal skin. When substantial rebuilding is requested the best choice is a combined graft that can be prepared with a piece of temporalis fascia, gently sutured on itself in a tube shape (an insulin syringe can help to guide this step), filled with crushed cartilage. This preparation is rather time-consuming, as some rules must be respected to get a good result. These include: 1. Some degree of resorption (up to 30%) must be expected; 2. The fascia tube must be well designed and well sutured, to be right in its shape, proof enough to avoid any loss of cartilage; 3. The needed quantity of cartilage must be in excess at the beginning and then trimmed and crushed in a very thin particulate. This is a delicate and long step that permits to "inject" the crushed cartilage into the prepared tube-shaped bag. 4. The final fixation to the dorsum has to be very careful, not invading the tip area, neither the nasofrontal angle, not exceeding the upper lateral width, neither creating a step-like deformity that will be too narrow.
In cases of excessive middle vault resection, the placement of spreader grafts may be necessary to recreate the natural flare seen in the topography of the middle vault 23. Spreader cartilaginous grafts placed between the septum and upper lateral cartilages may be used in patients who are at risk for internal nasal valve collapse 26 27 (Fig. 10). If the nose is twisted, we must determine its cause. If the septum is still present, it must be addressed to ensure that it is in fact in the midline and not twisted. If it is twisted, it can be harvested and used as donor material for rebuilding the nose. Lateral and medial osteotomies can also be used.
Fig. 10.
Spreader graft.
Functional aspects
Surgery of the middle vault will often compromise the internal nasal valve 28. Performing a Cottle test preoperatively will confirm the need for reconstitution of the internal valve dimension. Placement of spreader grafts will either prevent or ameliorate this problem. Excessive removal of the lower lateral cartilages results in alar retraction, which is often a cause of external valve collapse. Correction of this deformity almost always involves grafting. Auricular cartilage has a better natural shape for alar reconstruction 29. These grafts can be easily harvested from the cymba conchae. They may be placed as alar battens on top of existing cartilage. If the alar rim contour is questionable, an alar rim graft may also be used to restore natural alar curvature (Fig. 11).
Fig. 11.
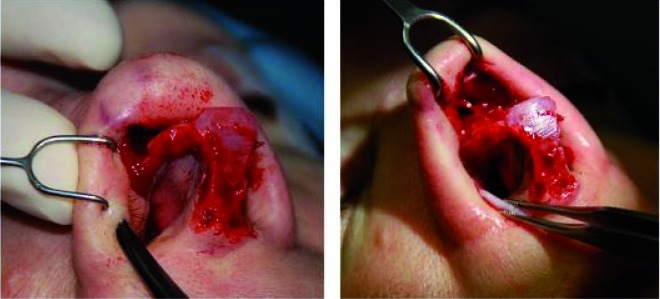
Pocket preparation and rim graft positioning.
Conclusions
Any secondary rhinoplasty is typically difficult due to obvious factors such as the number of prior operations, number of different surgeons, availability of septum and skin thickness. However, a critical issue is that there is little idea of what was done or is available in a secondary case until the area is exposed.
First of all, it is mandatory to determine what the patient's concerns are, and then verify the validity of the complaint with complete internal and external examination of the nose. One of the goals for the surgeon is to restore the structural support of the nose and to replace lost soft tissue volume. In order to achieve this goal, often the surgeon must rely on grafts. For the vast majority of complex secondaries, an open approach will offer an extended view and access to nearly the entire nasal complex, thereby allowing precise manoeuvres and placement of sutures and grafts.
Tip plasty can be done through cephalic trim of the lateral crura, along with transdomal suturing and placement of shield grafts. To combat or avoid tip ptosis, columellar strut grafts should always be used. Whenever possible, septal cartilage is the donor material of choice.
When planning secondary surgery of the dorsum, one must add straightening, smoothing and camouflage of the dorsum to the primary choices of reduction, augmentation or balance. Analyses of the preoperative situation is needed through a careful examination and a complete series of pictures. In our hands, computer simulation is mandatory and personally recommended.
Appendix 1
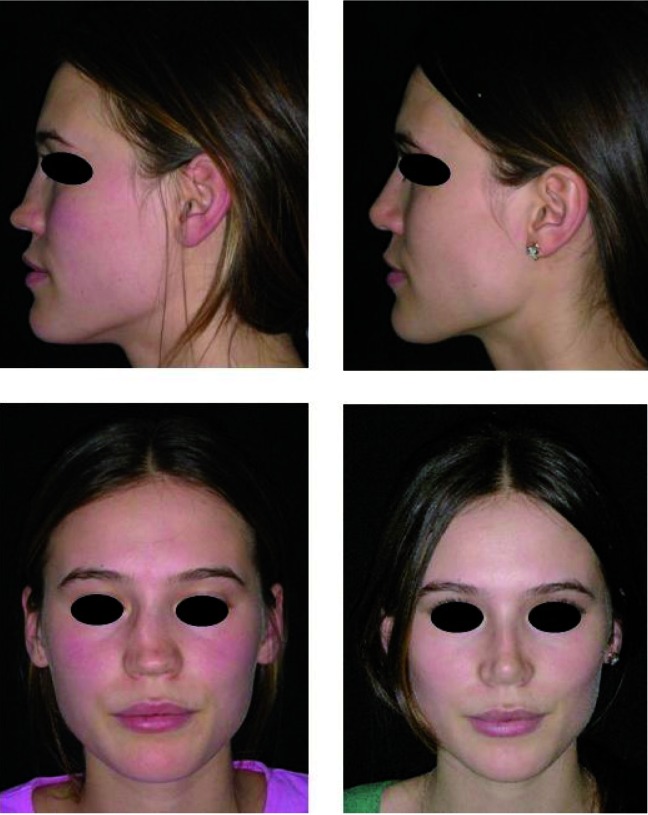
Fig. 12.
(A, B, C). Personal cases. In older patients, very careful structural grafting is required.
References
- 1.Warner J, Gutowski K, Shama L, et al. National interdisciplinary rhinoplasty. Aesthet Surg J. 2009;29:295–301. doi: 10.1016/j.asj.2009.04.005. [DOI] [PubMed] [Google Scholar]
- 2.Parkes ML, Kanodia R, Machida BK. Revision rhinoplasty. An analysis of aesthetic deformities. Arch Otolaryngol Head Neck Surg. 1992;118:695–701. doi: 10.1001/archotol.1992.01880070025005. [DOI] [PubMed] [Google Scholar]
- 3.Kamer FM, McQuown SA. Revision rhinoplasty: analysis and treatment. Arch Otolaryngol Head Neck Surg. 1988;114:257–266. doi: 10.1001/archotol.1988.01860150039014. [DOI] [PubMed] [Google Scholar]
- 4.Wright MR. Management of patient dissatisfation with results of cosmetic procedures. Arch Otolaryngol. 1980;106:466–471. doi: 10.1001/archotol.1980.00790320018005. [DOI] [PubMed] [Google Scholar]
- 5.Daniel RK. Mastering in rhinoplasty: a comprehensive atlas of surgical techniques with integrated video clips. 2nd edition. Berlin, Germany: Springer; 2010. [Google Scholar]
- 6.Romo T, 3rd, Kwak ES. Nasal grafts and implants in revision rhinoplasty. Facial Plast Surg Clin North Am. 2006;14:373–387. doi: 10.1016/j.fsc.2006.06.006. [DOI] [PubMed] [Google Scholar]
- 7.Cárdenas-Camarena L, Guerrero MT. Use of cartilaginous autografts in nasal surgery: 8 years of experience. Plast Reconstr Surg. 1999;103:1003–1014. doi: 10.1097/00006534-199903000-00039. [DOI] [PubMed] [Google Scholar]
- 8.Ortiz-Monasterio F, Olmedo A, Oscoy LO. The use of cartilage grafts in primary aesthetic rhinoplasty. Plast Reconstr Surg. 1981;67:597–605. doi: 10.1097/00006534-198105000-00003. [DOI] [PubMed] [Google Scholar]
- 9.Tardy ME, Jr, Denneny J, 3rd, Fritsch MH. The versatile cartilage autograft in reconstruction of the nose and face. Laryngoscope. 1985;95:523–533. doi: 10.1288/00005537-198505000-00003. [DOI] [PubMed] [Google Scholar]
- 10.Gunter JP, Rohrich RJ. Augmentation rhinoplasty: dorsal onlay grafting using shaped autogenous septal cartilage. Plast Reconstr Surg. 1990;86:39–45. [PubMed] [Google Scholar]
- 11.Byrd HS, Constantian MB, Guyuron B, et al. Revision Rhinoplasty. Aesthet Surg J. 2007;27:175–187. doi: 10.1016/j.asj.2007.02.001. [DOI] [PubMed] [Google Scholar]
- 12.Constantian MB. Indication and use of composite grafts in 100 consecutive secondary and tertiary rhinoplasty patients: introduction of the axial orientation. Plast Reconstr Surg. 2002;110:1116–1133. doi: 10.1097/01.PRS.0000021870.72613.FC. [DOI] [PubMed] [Google Scholar]
- 13.Adamson PA. Grafts in rhinoplasty: autogenous grafts are superior to alloplastic. Arch Otolaryngol Head Neck Surg. 2000;126:561–562. doi: 10.1001/archotol.126.4.561. [DOI] [PubMed] [Google Scholar]
- 14.Toriumi DM. Autogenous grafts are worth the extra time. Arch Otolaryngol Head Neck Surg. 2000;126:562–564. doi: 10.1001/archotol.126.4.562. [DOI] [PubMed] [Google Scholar]
- 15.Daniel RK. Rhinoplasty and rib grafts: evolving a flexible operative technique. Plast Reconstr Surg. 1994;94:597–609. [PubMed] [Google Scholar]
- 16.Guerrerosantos J. Nose and paranasal augmentation: autogenous, fascia, and cartilage. Clin Plast Surg. 1991;18:65–89. [PubMed] [Google Scholar]
- 17.Besharatizadeh R, Ozkan BT, Tabrizi R. Complete or a partial sheet of deep temporal fascial graft as a radix graft for radix augmentation. Eur Arch Otorhinolaryngol. 2011;268:1449–1453. doi: 10.1007/s00405-011-1565-3. [DOI] [PubMed] [Google Scholar]
- 18.Maas CS, Monhian N, Shah SB. Implants in rhinoplasty. Facial Plast Surg. 1997;13:279–290. doi: 10.1055/s-0028-1082427. [DOI] [PubMed] [Google Scholar]
- 19.Batniji RK, Hutchison JL, Dahiya R, et al. Tissue response to expanded polytetrafluoroethylene and silicone implants in a rabbit model. Arch Facial Plast Surg. 2002;4:111–113. doi: 10.1001/archfaci.4.2.111. [DOI] [PubMed] [Google Scholar]
- 20.Achauer BM. A serious complication following medicalgrade silicone injection of the face. Plast Reconstr Surg. 1983;71:251–254. doi: 10.1097/00006534-198302000-00020. [DOI] [PubMed] [Google Scholar]
- 21.Becker DG, Bloom J. Five techniques that I cannot live without in revision rhinoplasty. Facial Plast Surg. 2008;24:358–364. doi: 10.1055/s-0028-1083089. [DOI] [PubMed] [Google Scholar]
- 22.Thomson C, Mendelsohn M. Reducing the incidence of revision rhinoplasty. J Otolaryngol. 2007;36:130–134. doi: 10.2310/7070.2007.0012. [DOI] [PubMed] [Google Scholar]
- 23.Cuzalina A, Qaqish C. Revision rhinoplasty. Oral Maxillofacial Surg Clin N Am. 2012;24:119–130. doi: 10.1016/j.coms.2011.10.003. [DOI] [PubMed] [Google Scholar]
- 24.Chrostophl JJ, Park SS. Complications in rhinoplasty. Facial Plast Surg Clin North Am. 2009;17:145–156. doi: 10.1016/j.fsc.2008.09.012. [DOI] [PubMed] [Google Scholar]
- 25.Papel ID. Facial plastic and reconstructive surgery. 3rd edition. New York: Thieme; 2009. [DOI] [PubMed] [Google Scholar]
- 26.Park SS, Becker SS. Becker DG, Park SS. Revision rhinoplasty. New York: Thieme; 2008. Repair of nasal airway obstruction in revision rhinoplasty. [Google Scholar]
- 27.Sheen J. Spreader graft: a method of reconstructing the middle nasal vault following rhinoplasty. Plast Reconstr Surg. 1984;73:230–239. [PubMed] [Google Scholar]
- 28.Fischer H, Gubisch W. Nasal valves importance and surgical procedures. Facial Plast surg. 2006;22:49–54. doi: 10.1055/s-2006-954845. [DOI] [PubMed] [Google Scholar]
- 29.Murrell GL. Auricular cartilage grafts and nasal surgery. Laryngoscope. 2004;114:2092–2102. doi: 10.1097/01.mlg.0000149440.20608.7c. [DOI] [PubMed] [Google Scholar]