Abstract
Purpose
Fatigue is one of the most common complaints experienced among the general population. Because fatigue is recognized as a biobehavioral occurrence, a biobehavioral intervention such as guided imagery may be effective in reducing self-reported fatigue. Therefore, the purpose of this study was to explore the research literature related to the use of guided imagery as a nonpharmacological mind-body intervention for the symptom of fatigue.
Method
The electronic databases MEDLINE, CINAHL, PsychInfo, Psychology and Behavioral Sciences Collection and the Cochrane Library were searched from January 1980 to June 2010.
Findings
Of 24 articles retrieved, eight met the inclusion criteria and were included in this systematic literature review. Findings were inconsistent regarding the effectiveness of guided imagery on fatigue. Studies varied in study length, duration of the applied guided imagery intervention, dosage, and whether the images were targeted to the purpose of the intervention.
Implications
Guided imagery is a simple, economic intervention with the potential to effectively treat fatigue, thus further research is warranted using systematic, well-designed methodologies Standardizing guided imagery interventions according to total duration of exposure and targeted imagery in a variety of different populations adequately powered to detect changes will contribute to and strengthen nursing’s symptom-management armamentarium.
Keywords: guided imagery, fatigue, literature review
Fatigue is one of the most common complaints experienced among the general population (Purcell, Fleming, Haines, & Bennett, 2009) and has become a focal point in patient-centered outcome measures across interdisciplinary research domains. Based on primary care and community-based samples, fatigue may affect anywhere from 20% to 40% of the U.S. population (DeLuca, Genova, Capili, & Wylie, 2009; Portenoy, 2003). According to the National Institutes of Health (2010), fatigue is considered “an overwhelming, debilitating, and sustained sense of exhaustion that is likely to decrease one’s ability to carry out daily activities, including the ability to work effectively and to function at one’s usual level in family or social roles.” Researchers have identified fatigue as a subjective state that is difficult to objectively define (Rasker, 2009). As a symptom that affects both physical and intellectual ability, the experience of fatigue often results in negative consequences for an individual’s quality of life (Al-Majid & Gray, 2009).
Factors contributing to fatigue may include medical conditions, disease activity, medication and treatment for diseases, stress, depression, anxiety, pregnancy, environmental factors, poor nutrition, poor coping strategies, and poor sleep quantity as well as quality (Corwin, Klein, & Rickelman, 2002; Ream & Richardson, 1996). Because any one of these factors may influence the occurrence of fatigue independently, patients experiencing more than one factor concurrently may be at even geater risk of experiencing fatigue (Lewis & Wessely, 1992). Fatigue is a multidimensional, biobehavioral phenomenon caused by a complex imbalance and interplay of biological, psychobehavioral, and Cunctional mechanisms (Al-Majid & Gray, 2009). Recommended treatment options for fatigue include both pharmacologic and nonpharmacologic strategies (Romani, 2008). Given the psychophysiological and psychobehavioral nature of the causes or consequences of fatigue, a mind–body intervention, such as guided imagery, merits consideration as a symptom management strategy for reducing self-reported levels of fatigue.
Guided imagery is a mental function that expresses itself as a dynamic, quasi-real, psychophysiological process that engages all of the senses to bring about individual changes in behavior, perception, or physiologic responses (Author, 2004; Freeman, 2009). Responses to mental images may be similar to that which occurs when the actual stimulus is present (Eller, 1999). From a neuroendocrine perspective, guided imagery helps downregulate the hypothalamic–pituitary–adrenal axis, which may result in decreased glucocoriticoid and catecholamine levels. From the perspective of the autonomic nervous system, there is an interactive relationship between the sympathetic and parasympathetic nervous system that occurs in response to stimuli, whether real or imagined (Lowenstein, 2002; Schaub & Dossey, 2009). Such physiologic changes may help explain the biological mechanisms underlying the imagery process. When used as a clinical tool, guided imagery has been shown to relieve levels of perceived stress and anxiety or improve physical function as well as enhance one’s sense of self-efficacy for managing symptoms related to chronic pain conditions (Jallo et al., 2008, 2009; Menzies et al., 2006). Although guided imagery has been used in clinical settings as part of multidisciplinary intervention programs used in combination with other nonpharmacologic interventions, it is unknown how often it has been applied as a therapeutic intervention for conditions in which fatigue is a dependent variable of interest. Therefore, the purpose of this study was to explore the research literature related to the use of guided imagery as a nonpharmacological mind–body intervention for the symptom of fatigue.
Literature Review
Method
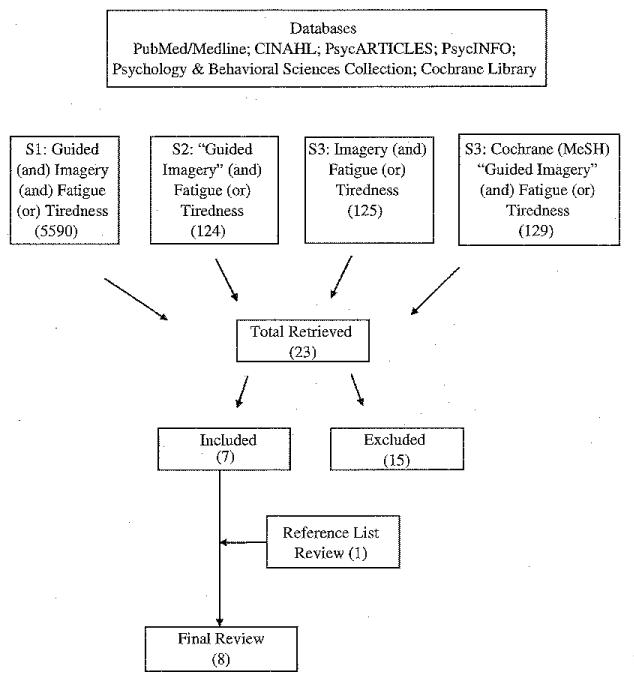
The electronic databases PubMed/Medline, CINAHL, PsycARTICLES, PsychINFO, and Psychology and Behavioral Sciences Collection were searched from January 1980 to June 2008. Criteria for literature retrieval were quantitative studies that emerged using the keywords, “fatigue,” “tiredness,” “imagery,” “guided,” and “guided imagery.” Results were limited to studies published in English. Exclusion criteria included dissertations, studies using music alone or combined with guided imagery, studies using relaxation alone or studies using hypnosis as an intervention. Because music alone has been shown to have a relaxing and potentially analgesic-inducing effect (Aldridge, 1993), research articles that explored the effect of guided imagery with music as part of the intervention were excluded. Additionally, because guided imagery may induce a physiological relaxation response as part of the process but is not always used as part of a relaxation induction (Utay & Miller, 2006), the term “relaxation” was excluded as a keyword among the search terms for our literature review. If, however, any reviewed article included guided imagery with relaxation or defined guided imagery as relaxation guided imagery and also included the term “fatigue,” the article was reviewed for potential inclusion in our systematic literature review. Because hypnosis is a specialized psychotherapeutic modality that uses imagery to purpose-fully induce trance states but requires specialized training to either practice or to train others to self-hypnotize for psychophysiological health–related purposes (Gruzelier, 2002; Hammond, 1990), the term “hypnosis” was also excluded as a keyword for our literature review. Finally, although fatigue may have been among several variables under investigation in each of the reviewed studies, our literature review focuses on reported results related only to fatigue as the dependent variable.
Abstracts were reviewed and articles were selected for inclusion if the studies tested guided imagery as an intervention and measured and reported fatigue as an outcome variable. Because of the limited number of retrieved articles that met the inclusion criteria for our literature review, a MeSH search of the Cochrane Database of Systematic Reviews was conducted using the term “Search All Text” with keywords “guided imagery,” [MeSH: fatigue] or “tiredness.” The search produced 129 Cochrane reviews, out of which only one article met the original review criteria for our study. To complete the literature search, the reference lists of qualifying articles were reviewed; one article met the original review criteria. Out of 24 articles retrieved via all of these search methods, 8 articles met the inclusion criteria for our study and are included in this systematic literature review. Our strategy for choosing research articles for review is depicted in Figure 1.
Studies were reviewed in detail, using a narrative approach. We did not compute study quality scores because our intent was to briefly summarize studies in order to illustrate the frequency and diversity of the use of guided imagery as a treatment option for fatigue. Summaries also included the diversity of guided imagery approaches, study aims, participant characteristics, the nature and duration of guided imagery interventions, experimental designs, and instruments used to capture levels of fatigue.
Results
Of the eight articles included in the final review, each study explored some aspect of fatigue, most often measuring it as a subscale among a variety of larger measures. For example, in four of the eight studies, researchers measured fatigue as a subscale of the larger instrument, the Profile of Mood States (POMS; McNair, Lorr, & Droppelman, 1992). In two of the eight studies, however, fatigue was measured using either a 100-mm visual analogue scale (VAS) or the Brief Fatigue Inventory (BFI; Mendoza et al., 1999). Clinical conditions in which fatigue was identified as a measurable concern included asthma, bronchitis and emphysema, cancer, congestive heart failure, multiple sclerosis, or HIV.
Bridge, Benson, Pietroni, and Priest (1988) used a randomized controlled study design to investigate the effect of relaxation or relaxation-plus-guided-imagery, as compared with a control group, on fatigue in women being treated for early breast cancer. A total of 154 women provided informed consent as well as met inclusion criteria and 139 completed the study (ages 41-64 years). Fatigue was measured as a subscale of the POMS. One of the study’s researchers visited each participant once a week for 6 weeks. Participants in the control group (n = 48) were encouraged to talk about themselves; participants in the relaxation-alone group (n = 47) were taught muscle relaxation, and participants in the relaxation-plus-guided-imagery group (n = 44) were taught muscle relaxation and imaging a peaceful scene. Participants in the relaxation group and the relaxation-plus-guided-imagery group received an audiotape repeating intervention instructions and were requested to practice at least 15 minutes each day. Data were collected from participants on their entry into the study and again at the end of their 6-week treatment period. The POMS fatigue subscale did not demonstrate a statistically significant difference among the three groups of participants. Study limitations included participant attrition (n = 15) and lack of data related to participants’ race or ethnicity. In addition, a potential confounder to study findings was the social support provided to individuals in the control group who met weekly with researchers to “talk about themselves”.
Moody, Fraser, and Yarandi (1993) tested the effects of guided imagery and maximal inspiratory muscle training (MITT) on fatigue in Caucasian participants diagnosed with moderate chronic bronchitis and emphysema. A total of 30 study participants consented and enrolled in the study and 19 participants (9 females and 10 males, age 56-75 years) completed h e study. Using a repeated measures design, the researchers first assigned the participants to the treatment of guided imagery. During the first 4 weeks, participants met weekly with the researchers to practice guided imagery. Participants were asked to practice the technique two times a day for 15 minutes. At the end of the initial 4 weeks, participants were then taught MITT and asked to use the device two times a day for 15 minutes. Fatigue, one of seven response variables of the Chronic Disease Assessment Tool (Moody, 1989), was measured at the first session, at the end of the initial 4 weela, and at the end of the MITT 4-week period. Repeated measure analysis revealed no significant differences in fatigue within subjects over time. Study limitations included an attrition rate of 36% because of participants’ problems with transportation and difficulty in using MITT and to acute exacerbation of the disease process. It was unclear if participants were asked to continue using guided imagery during the 4 weeks of MITT use.
Using a pretest–posttest experimental research design, Arathuzik (1994) compared treatment outcomes in 24 women, ranging in age from 31 to 8O years, who were diagnosed with metastatic breast cancer. Participants were assigned to one of three groups: a control group (n = 8), in which participants received routine treatment and pain medication, or one of two treatment groups. One treatment group (n = 8) received instruction and practice in a 20-minute progressive muscle relaxation (PMR) exercise and a 20-minute guided imagery exercise aimed at pain reduction; total treatment time was 75 minutes. The other treatment group (n = 8) received the same PMR exercise and guided imagery training with additional instruction and practice in cognitive coping skills; total treatment Lime was 120 minutes. Arathuzik found no significant reductions in the subscale of POMS fatigue scores in either of the two treatment groups as compared to the routine treatment and pain medication control group. Study limitations included absence of reported race or ethnicity of the participants, small sample size, and brevity of the intervention.
To examine the effects of guided imagery or relaxation alone on fatigue, depression, and three measures of cellular immunity, Eller (1995) compared three treatment conditions in persons across the HIV spectrum. In all, 81 participants were recruited and 69 completed the study (9 females and 60 males, ranging in age from 22 to 76 years). Overall, 42 participants were reported as Caucasian, 24 as African American, 2 as Latino/a, and 1 as Native American. Participants were assigned to one of three groups: a control group (n = 24), in which participants received standard treatment, and two intervention groups. In one of the intervention groups, participants (n = 23) received a 6-week treatment of guided imagery; participants (n = 22) of the second intervention group received a 6-week treatment of PMR. Both interventions, used daily for 6 weeks, were delivered via audiotape following an initial, brief, face-to-face session of instructions. Fatigue was measured using the Rest and Sleep subscale of the Sickness Impact Profile (Bergner, Bobbitt, Carter, & Gilson, 1981) and a 100-mm VAS. Only the participants in the guided imagery intervention group demonstrated significant reductions in fatigue (p = .04), compared with participants in both the PMR intervention group and the standard treatment control group. Study limitations included use of a convenience sample and lack of any follow-up data.
Maguire (1996) compared treatment outcomes in two groups of patients with multiple sclerosis (N = 33). The control group (n = 18; 13 females and 5 males) followed typical medical protocol and completed pretest and posttest measures. The intervention group (n = 15; 12 females and 3 males) received a six-session group process that included relaxation training and biologically oriented imagery that was practiced at home between sessions. Study participants’ age ranged from 26 to 60 years; race or ethnicity was not reported. Fatigue was measured as a subscale score of the POMS. Study findings revealed no statistically significant differences between groups for fatigue. Study limitations included lack of reported study length (i.e., the six sessions were not defined as occurring over a set period of time) and lack of reported race or ethnicity of the participants.
In a quasi-experimental research study, using a pretest–posttest design, Klaus et al. (2000) explored the effect of guided imagery on outcomes of fatigue, dyspnea, mood, self-efficacy, and exercise capacity among individuals with severe heart Failure (N = 8). The authors did not report the study participants’age, gender, race, or ethnicity. Prior to initiating the guided imagery intervention protocol, participants completed pretest questionnaires and exercise testing. The guided imagery intervention consisted of three 1.5-hour weeldy group guided imagery training sessions during which study participants were instructed in and practiced guided imagery techniques. Participants received audiotapes of the exercises taught at each weekly session, along with instructions to use the audiotapes for at least 10 minutes per use for a minimum of twice daily. At the end of the final group session, participants were then instructed to continue to use the guided imagery audiotapes from the group imagery training sessions for another 2 weeks for at least 10 minutes per use for a minimum of twice daily. Participants were also asked to keep a diary of the frequency and length of their practice times, which the researchers identified as the participants’ level of “compliance” with the study protocol. At the end of Week 6, participants completed follow-up exercise testing and posttest measures. Measuring fatigue as a subscale of the modified Borg Scale (Borg, 1982), the authors found perceived fatigue improved in the 6-minute walk but worsened during Vo2, testing to determine exercise performance. The researchers concluded their pilot study was underpowered to identify statistically significant effects on outcome variables, and they recommended future larger studies of longer duration. Study limitations, as acknowledged by the authors, were small sample size, lack of a control group, low level of reported compliance (participants’ use of the intervention), and the potential confounder of group sessions as a form of social support. Other limitations to the study included the absence of reported age, gender, race or ethnicity of the study participants.
In a randomized controlled clinical trial, Freeman and Welton (2005) explored the effects of biologically targeted imagery (BTI) and critical thinking asthma management (CTAM) coupled with asthma education on fatigue among 70 adults with asthma. Study participants’ age ranged from 35 to 59 years. Participants were randomized either to the BTI intervention group or to the wait-list control group, who were later assigned to the CTAM intervention group. A total of 25 individuals completed the BTJ full treatment and 20 individuals completed the CTAM full treatment. For 6 weeks, participants attended two 2-hour weekly sessions of asthma education and BTI or asthma education and CTAM. Participants in both intervention groups were requested to spend 30 minutes a day, 5 days a week, practicing either BTI or CTAM outside of class, depending on their group assignment. Fatigue was measured as a subscale of the POMS, pre- and postintervention. The authors reported the pre–post intervention POMS fatigue subscale scores for participants in the BTI group significantly improved (p =.002). Study limitations included a lack of data related to the participants’ race or ethnicity.
Haase, Schwenk, Hermann, and Müller (2005) investigated the effects of guided imagery on fatigue after conventional resection of colorectal carcinoma in elderly cancer patients. In total, 74 participants consented and enrolled in the study; however, 13 were excluded because of surgical complications. Additionally, one individual in the PMR group refused to participate one day before surgery and dropped out of the study, leaving a sample of 60 (23 females and 37 males; reported age, 54-76 years). Using a randomized, controlled clinical design the researchers compared the effects of usual care (n = 18) with a 12-minute guided imagery audiotape intervention (n = 20) or to a 12-minute PMR audiotape intervention (n = 22) on postoperative fatigue and analgesic use. Researchers recommended participants listen to the audiotapes at least three times a day every day for at least 2 days before and 1 week after surgery. Participants randomized to the guided imagery group or the PMR group reported using the intervention an average of five times prior to surgery and 10 times within the first hospitalized postoperative week. Using a 100-mm VAS, fatigue was measured daily between 6:00 a.m. and 8:00 a.m. Postopcrative fatigue was not influenced by either the guided imagery or the PMR audio-taped intervention as compared to the control group. Study limitations included absence of reported race or ethnicity of the participants, lack of complete reporting of enrolled participant demographics, and absence of rationale to explain the selection of the 6:00 a.m. to 8:00 a.m. time period for assessing fatigue.
Out of the eight studies reviewed, two demonstrated significant reductions in levels of fatigue after a guided imagery intervention (Eller, 1995; Freeman & Welton, 2005) and one study reported mixed findings (Klaus et al., 2000). For those studies in which race or ethnicity was reported (n = 2), only one study reported minority participants (Eller, 1995).
Discussion
Findings, Issues and Gaps Identified
Findings across the eight reviewed studies were inconsistent regarding the effects of guided imagery on fatigue. Using measures of self-reported scores of fatigue, researchers reported a variety of effects with the use of guided imagery: no effect (Arathuzik, 1994; Bridge et al., 1988; Haase et al., 2005; Maguire, 1996; Moody et al., 1993), a mixed effect (Klaus et al., 2000), or a long-term effect (Eller, 1995; Freeman & Welton, 2005). Moreover, treatment protocols and details of images used in guided imagery strategies were not comparable across the studies while reported sample sizes varied. By examining these inconsistencies, the disparate findings across the eight studies may be explained.
An important component of treatment protocol is the total duration of exposure, which may be defined as a combination of (a) study length, (b) duration of the applied intervention, and (c) frequency (dosage) of the intervention use. Researchers have suggested that total duration of exposure to guided imagery has an impact on study outcomes (Jallo et al., 2008; Watanabe, Fukuda, & Shirakawa, 2005). This view-point is plausible because an individual’s skill in using imagery increases with practice, and practicing imagery regularly over a period of time may be more likely to produce a change in symptoms (Maguire, 1996). Among the eight reviewed studies that included information related to duration of exposure to guided imagery, study lengths ranged from a minimum of one session (Arathuzik, 1994) to a maximum of 6 weeks (Bridge et al., 1988; Eller, 1995; Freeman & Welton, 2005; Maguire, 1996). The duration of the applied interventions ranged from a minimum of 10 minutes (Klaus et al., 2000) to a maximum of 30 minutes (Freeman & Welton, 2005). Frequency of use (dosage) ranged from a minimum of once (Arathuzik, 1994) to a maximum of 5 to 7 times daily over 6 weeks (Eller, 1995; Freeman & Welton, 2005; Maguire, 1996). The studies demonstrating significant improvement in long-term fatigue scores were investigations that included the greatest total duration of exposure to a guided imagery intervention (Eller, 1995; Freeman & Welton, 2005).
Because guided imagery links perception, emotion, and physiologic responses, the selection of images is important (Eller, 1995). Epstein (1989) suggested that the selection of images should be related to what one wants to accomplish or achieve. Thus, if the intention of the intervention is to decrease the symptom of fatigue, images targeted to fatigue should be included in the intervention. Among the reviewed studies that provided details of the imagery, selected images included biologically targeted imagery of damaged myelin being repaired (Maguire, 1996); biologically targeted imagery of healthy lung functioning (Freeman & Welton, 2005); and imagining a peaceful place (Bridge et al., 1988; Haase et al., 2005). Selected images also included imagery targeting the symptom of fatigue, such as “feel the growing surge of energy” (Eller, 1995, p. 343) and “place the sun on your body to give you energy … enjoy your newfound energy” (Klaus et al., 2000, p. 103). The studies demonstrating significant improvement in long-term fatigue scores included biologically targeted imaging of healthy lung functioning (Freeman & Welton, 2005) and fatigue-focused imagery (Eller, 1995).
The sample sizes of participants who completed the studies reviewed ranged from 8 participants (Klaus et al., 2000) to 139 participants (Bridge et al., 1988). Although it is difficult to make any conclusions about the effects of sample size in this review, it is worth noting that the studies with a sample of 30 or more participants completing the data collection were more likely to demonstrate significant findings (Eller, 1995; Freeman & Welton, 2005) compared to studies with fewer than 30 participants completing the study (Arathuzik, 1994; Klaus et al., 2000; Moody et al., 1993). Power analysis data were not included in any of the studies. Exceptions to this observation may be explained by examining sample size and the selection of images. For example, Bridge et al.’s (1988) study, with a sample of 139 participants, and Maguire’s (1996) study, with a sample of 33 participants completing the study, did not include fatigue-focused imagery as an intervention, and neither study elicited significant findings. Conversely, Klaus et al.’s (2000) study included fatigue-focused imagery in an intervention that lasted 5 weeks but had only 8 participants. Taken together, these three studies demonstrate the potential for a treatment protocol consisting of fatigue-focused images over an adequate period of exposure in an appropriately powered sample to result in a significant reduction of self-reported fatigue scores.
Implications for Nursing Research, Practice, and Knowledge Development
Fatigue is one of the most common symptoms experienced among the general population and is associated with numerous factors, such as multiple medical and psychological conditions, environmental factors, pregnancy, ability to cope, and treatment for diseases. Because fatigue is recognized as a biobehavioral occurrence, a biobehavioral intervention such as guided imagery may be effective in reducing self-reported fatigue. However, despite the potential benefits of guided imagery, few research studies have tested its effects on fatigue.
Across the eight studies we reviewed, findings were inconsistent regarding the effectiveness of guided imagery on fatigue. The differences were likely because of incongruent elements among the investigations. The studies varied in total duration of exposure (study length, duration of the applied guided imagery intervention, dosage) and whether the images were targeted to the purpose of the intervention. Also, some of the studies did not include an adequately powered sample size. These inconsistencies highlight the relevance of research methodology in advancing the science of nonpharmacologic symptom management strategies. Standardizing guided imagery interventions according to total duration of exposure and targeted imagery across patient populations and in studies adequately powered to detect changes will contribute to the successful transfer of research from the metaphorical bench to its application at the patient’s bedside.
Because guided imagery is a powerful, simple, and economic intervention with the potential to treat fatigue effectively, Further research is warranted using systematic, well-designed methodologies that incorporate a guided imagery intervention using fatigue-focused images with sufficient exposure in a variety of different populations adequately powered to detect statistically significant changes. More extensive research in this arena will contribute to the science exploring the potential effectiveness of guided imagery on fatigue and, in turn, will contribute to and strengthen nursing’s symptom management armamentarium.
Figure 1.
Literature Search Method
Acknowledgments
This study is supported by the National Institute of Nursing Research through Grant No. P30 NR011403 (R. Pickler, Principal Investigator).
References
- Aldridge D. The music of the body: Music therapy in medical settings. ADVANCES: The Journal of Mind-Body Health. 1993;9:17–35. [Google Scholar]
- Al-Majid S, Gray DP. A biobehavioral model for the study of exercise interventions in cancer-related fatigue. Biological Research for Nursing. 2009;10:381–391. doi: 10.1177/1099800408324431. [DOI] [PubMed] [Google Scholar]
- Arathuzik Effects of cognitive-behavioral strategies on pain in cancer patients. Cancer Nursing. 1994;17:207–214. [PubMed] [Google Scholar]
- Bergner M, Bobbitt RA, Carter WB, Gilson BS. The sickness impact profile: Development and final revision of a health status measure. Medical Care. 1981;19:787–805. doi: 10.1097/00005650-198108000-00001. [DOI] [PubMed] [Google Scholar]
- Borg GAV. Psychophysical bases of perceived exertion. Medicine & Science in Sports & Exercise. 1982;14:377–381. [PubMed] [Google Scholar]
- Bridge LR, Benson P, Pietroni PC, Priest RG. Relaxation and imagery in the treatment of breast cancer. British Medical Journal. 1988;297:1169–1172. doi: 10.1136/bmj.297.6657.1169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corwin EJ, Klein LC, Rickelman K. Predictors of fatigue in healthy young adults: Moderating effects of cigarette smoking and gender. Biological Research for Nursing. 2002;3:222–233. doi: 10.1177/109980040200300407. [DOI] [PubMed] [Google Scholar]
- DeLuca J, Genova HM, Capili EJ, Wylie GR. Functional neuroimaging of fatigue. Physical Medicine and Rehabilitation Clinics of North America. 2009;20:325–337. doi: 10.1016/j.pmr.2008.12.007. doi:10.1016.j.pmr.2008.12.007. [DOI] [PubMed] [Google Scholar]
- Eller LS. Effects of two cognitive-behavioral interventions on immunity and symptoms in person with HIV. Annals of Behavioral Medicine. 1995;17:339–348. doi: 10.1007/BF02888599. [DOI] [PubMed] [Google Scholar]
- Epstein G. Healing visualizations: Creating health through imagery. Bantam; New York, NY: 1989. [Google Scholar]
- Freeman L. Mosby’s complementary & medicine: A research-based approach. 3rd ed. Mosby Elsevier; St. Louis, MO: 2009. [Google Scholar]
- Freeman LW, Welton D. Effects of imagery, critical thinking, and asthma education on symptoms and mood state in adult asthma patients: A pilot study. Journal of Alternative and Complementary Medicine. 2005;11:57–68. doi: 10.1089/acm.2005.11.57. doi:10.1089/acm.2005.11.57. [DOI] [PubMed] [Google Scholar]
- Gruzelier JH. A review of the impact of hypnosis, relaxation, guided imagery and individual differences on aspects or immunity and health. Stress. 2002;5:147–163. doi: 10.1080/10253890290027877. [DOI] [PubMed] [Google Scholar]
- Haase O, Schwenk W, Hermann C, Müller M. Guided imagery and relaxation in conventional colorectal resections: A randomized, controlled, partially blinded trial. Diseases of the Colon & Rectum. 2005;48:1955–1963. doi: 10.1007/s10350-005-0114-9. [DOI] [PubMed] [Google Scholar]
- Hammond DC. Introduction. In: Hammond DC, editor. Handbook of hypnotic suggestions and metaphors. W. W. Norton; New York, NY: 1990. pp. 1–9. [Google Scholar]
- Jallo N, Bourguignon C, Taylor AG, Utz SW, Snyder AE. Stress management during pregnancy: Designng and evaluating a mind-body intervention. Family & Community Health. 2008;31:190–203. doi: 10.1097/01.FCH.0000324476.48083.41. [DOI] [PubMed] [Google Scholar]
- Jallo N, Bourguignon C, Taylor AG, Ruiz J, Goehler L. The biobehavioral effects of relaxation guided imagery on maternal stress. Advances in Mind Body Medicine. 2009;24:12–22. [PubMed] [Google Scholar]
- Klaus L, Beniaminovitz A, Choi L, Greenfield F, Whitworth GC, Oz MC, Mancini DM. Pilot study of guided imagery use in patients with severe heart Failure. American Journal of Cardiology. 2000;86:101–104. doi: 10.1016/s0002-9149(00)00838-9. [DOI] [PubMed] [Google Scholar]
- Lewis G, Wessely S. The epidemiology of fatigue: More questions than answers. Journal of Epidemiology and Community Health. 1992;46:92–97. doi: 10.1136/jech.46.2.92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lowenstein KG. Meditation and self-regulatory techniques. In: Shannon S, editor. Handbook of complementary and alternative therapies in mental health. Academic Press; San Diego, CA: 2002. pp. 159–181. [Google Scholar]
- Maguire BL. The effects of imagery on attitudes and moods in multiple sclerosis patients. Alternative Therapies. 1996;2(5):75–79. [PubMed] [Google Scholar]
- McNair D, Lorr M, Droppelman L. Manual for the profile of mood states. Educational and Industrial Testing Service; San Diego, CA: 1992. [Google Scholar]
- Mendoza T, Wang XS, Cleeland CS, Morrissey M, Johnson BA, Wendt JK, Huber SL. The rapid assessment of fatigue severity in cancer patients: Use of the Brief Fatigue Inventory. Cancer. 1999;85:1186–1196. doi: 10.1002/(sici)1097-0142(19990301)85:5<1186::aid-cncr24>3.0.co;2-n. [DOI] [PubMed] [Google Scholar]
- Menzies V, Taylor AG, Bourguignon C. Effects of guided imagery on outcomes of pain, functional status, and self-efficacy in persons diagnosed with fibromyalgia. Journal of Alternative and Complementary Medicine. 2006;12:23–30. doi: 10.1089/acm.2006.12.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Menzies V, Taylor AG. The idea of imagination: an analysis of “imagery”. Advances in Mind-Body Medicine. 2004;20(2):4–10. [PubMed] [Google Scholar]
- Moody LE. Measurement of psychophysiologic response variables in chronic bronchitis and emphysema. Applied Nursing Research. 1989;3:36–38. doi: 10.1016/s0897-1897(05)80153-3. [DOI] [PubMed] [Google Scholar]
- Moody LE, Fraser M, Yarandi H. Effects of guided imagery in patients with chronic bronchitis and emphysema. Clinical Nursing Research. 1993;2:478–486. doi: 10.1177/105477389300200409. [DOI] [PubMed] [Google Scholar]
- National Institutes of Health . Domain frameworks–physical health. 2010. Retrieved from http://www.nihpromis.org/measures/domainframeworkI. [Google Scholar]
- Portenoy RK. Fatigue in medical illness: Research issues. In: Portenoy RK, Bruera E, editors. Issues in palliative care research. Oxford University Press; New York, NY: 2003. pp. 151–171. [Google Scholar]
- Purcell A,, Fleming J, Haines T, Bennett S. Cancer-related fatigue: A review and a conceptual framework to guide therapists’ understanding. British Journal of Occupational Therapy. 2009;72:79–86. [Google Scholar]
- Rasker JJ. The enigma of fatigue. Journal of Rheumatology. 2009;36:2630–2632. doi: 10.3899/jrheum.091036. doi:10.3899/jrheum.091036. [DOI] [PubMed] [Google Scholar]
- Ream E, Richardson A. Fatigue: A concept analysis. International Journal of Nursing Studies. 1996;33:519–529. doi: 10.1016/0020-7489(96)00004-1. [DOI] [PubMed] [Google Scholar]
- Romani A. The treatment of fatigue. Neurological Sciences. 2008;29(Suppl. 2):S247–S249. doi: 10.1007/s10072-008-0952-z. [DOI] [PubMed] [Google Scholar]
- Schaub BG, Dossey BM. Imagery. In: Dossey BM, Keegan L, editors. Holostic nursing: A handbook for practice. 5th ed. Jones & Bartlett; Sudbury, MA: 2009. pp. 295–326. [Google Scholar]
- Utay J, Miller M. Guided imagery as an effective therapeutic technique: A brief review of its history and efficacy research. Journal of Instructional Psychology. 2006;33:40–43. [Google Scholar]
- Watanabe E, Fukuda S, Shirakawa T. Effects among healthy subjects of the duration of regularly practicing a guided imagery program. BMC Complementary and Alternative Medicine. 2005;5(1) doi: 10.1186/1472-6882-5-21. doi:l0.1186/1472-6882-5-21. [DOI] [PMC free article] [PubMed] [Google Scholar]