Abstract
Rift Valley fever is a mosquito-borne zoonotic disease endemic to sub-Saharan Africa. Rift Valley fever virus (RVFV; genus Phlebovirus, family Bunyaviridae) causes high rates of abortion and fetal malformation in pregnant ruminants, and haemorrhagic fever, neurological disorders or blindness in humans. The MP-12 strain is a highly efficacious and safe live-attenuated vaccine candidate for both humans and ruminants. However, MP-12 lacks a marker to differentiate infected from vaccinated animals. In this study, we originally aimed to characterize the efficacy of a recombinant RVFV MP-12 strain encoding Toscana virus (TOSV) NSs gene in place of MP-12 NSs (rMP12-TOSNSs). TOSV NSs promotes the degradation of dsRNA-dependent protein kinase (PKR) and inhibits interferon-β gene up-regulation without suppressing host general transcription. Unexpectedly, rMP12-TOSNSs increased death in vaccinated outbred mice and inbred BALB/c or C57BL/6 mice. Immunohistochemistry showed diffusely positive viral antigens in the thalamus, hypothalamus and brainstem, including the medulla. No viral antigens were detected in spleen or liver, which is similar to the antigen distribution of moribund mice infected with MP-12. These results suggest that rMP12-TOSNSs retains neuroinvasiveness in mice. Our findings demonstrate that rMP12-TOSNSs causes neuroinvasion without any hepatic disease and will be useful for studying the neuroinvasion mechanism of RVFV and TOSV.
Introduction
Rift Valley fever (RVF), which was first reported in sheep and humans in Kenya in 1931 (Daubney et al., 1931), has spread into many areas of sub-Saharan Africa, as well as Egypt, Madagascar, the Comoros and the Arabian Peninsula (Cětre-Sossah et al., 2012; Grobbelaar et al., 2011; Schmaljohn & Nichol, 2007; Swanepoel & Coetzer, 2004). The causative agent, Rift Valley fever virus (RVFV) (family Bunyaviridae, genus Phlebovirus) is transovarially transmitted by floodwater species of mosquitoes (Linthicum et al., 1985) and horizontally transmitted to ruminants and humans by many different species of mosquitoes during outbreaks (Pepin et al., 2010). RVFV infection of pregnant ruminants causes high rates of abortion and fetal malformations (Swanepoel & Coetzer, 2004), while human RVF patients typically suffer a biphasic febrile illness with occasional complications, such as haemorrhagic fever, encephalitis or blindness (Ikegami & Makino, 2011). Currently, no established therapeutic regimens are available for RVF patients, and no commercial vaccines are available for veterinary or human use in non-endemic countries. In the USA, RVFV is an overlap select agent by the Departments of Health and Human Services (HHS) and Agriculture (USDA) and is classified as a National Institute of Allergy and Infectious Diseases (NIAID) Category A Priority Pathogen. Safe handling of RVFV requires bio-safety level (BSL)3+ or BSL4 laboratories.
The RVFV genome is comprised of tripartite negative-stranded RNA: Small (S)-, Medium (M)- and Large (L)-segments. The S-segment encodes N and NSs genes in an ambi-sense manner. The M-segment encodes NSm, a 78-kDa protein, and Gn and Gc proteins, and the L-segment encodes the RNA-dependent RNA polymerase (Ikegami, 2012; Schmaljohn & Nichol, 2007). Both NSs and NSm proteins are non-structural, and the former is a major virulence factor for RVF (Bouloy et al., 2001). The NSs protein inhibits host transcription by sequestering transcription factor (TF) IIH p44 subunits (Le May et al., 2004) and by promoting post-translational degradation of TFIIH p62 subunits (Kalveram et al., 2011a). In addition, NSs specifically interacts with Sin3A-associated protein (SAP30) on the interferon (IFN)-β promoter, and inhibits the activation of the IFN-β promoter at the transcriptional level during viral replication (Le May et al., 2008). NSs interacts with the pericentromeric γ-satellite sequence and induces defects of chromosome cohesion and segregation (Mansuroglu et al., 2010). NSs is responsible for cell cycle arrest at either the G0/G1 or S phase and for DNA damage responses via ataxia-telangiectasia mutation (ATM) (Austin et al., 2012; Baer et al., 2012). RVFV NSs can also promote post-translational proteasomal degradation of dsRNA-dependent protein kinase PKR (Habjan et al., 2009; Ikegami et al., 2009). In response to viral RNA replication, PKR induces eukaryotic initiation factor-α (eIF2α) phosphorylation, and subsequently, causes shutoff of the host translational initiation process (Gale et al., 2000). Thus, degradation of PKR by RVFV NSs prevents the eIF2α phosphorylation, which promotes efficient viral replication (Ikegami et al., 2009; Kalveram et al., 2013).
MP-12 is a live-attenuated vaccine candidate for RVF. MP-12 was generated by 12 serial passages of wt RVFV ZH548 strain in human diploid lung (MRC-5) cells in the presence of the chemical mutagen 5-fluorouracil (Caplen et al., 1985; Lokugamage et al., 2012). MP-12 is sufficiently safe and highly efficacious in ruminants (Morrill et al., 1987, 1991, 1997a, b). However, it lacks a marker to differentiate infected from vaccinated animals (DIVA). Therefore, we aim to develop second-generation MP-12 vaccines that encode DIVA markers while retaining strong immunogenicity. MP-12 NSs is fully functional (Billecocq et al., 2008; Ikegami et al., 2006, 2009; Kalveram et al., 2011a) and is dispensable for vaccine efficacy in mice (Lihoradova et al., 2012). Potential disadvantages of MP-12 lacking NSs is a slightly lower level of neutralizing antibody in vaccinated ruminants (Morrill et al., 2013) and inefficient replication in MRC-5 cells, which have been used for MP-12 amplification for vaccine manufacturing (Ikegami et al., 2006; Lokugamage et al., 2012). Therefore, we attempted to replace MP-12 NSs with that of a serologically distinct phlebovirus. We recently found that the NSs protein of Toscana virus (TOSV), which is genetically close to RVFV among the highly variable phleboviruses (Xu et al., 2007), promotes PKR degradation (Kalveram & Ikegami, 2013). Our previous studies have shown that inhibiting PKR by expressing a dominant-negative form increases the efficacy of MP-12 (Lihoradova et al., 2012). Therefore, we hypothesized that recombinant MP-12 encoding TOSV NSs in place of RVFV NSs (rMP12-TOSNSs) has increased vaccine efficacy and is also useful for DIVA. However, we encountered neurological disease in mice vaccinated with rMP12-TOSNSs. In this study, we describe the unexpected mouse death caused by the replacement of MP-12 NSs with TOSV NSs.
Results
Generation of recombinant MP-12 encoding TOSV NSs
A lack of a DIVA marker in MP-12 vaccine motivated us to explore a second-generation vaccine for RVF that encodes a DIVA marker with high efficacy. The NSs of MP-12 is dispensable for viral replication and vaccine efficacy (Lihoradova et al., 2012). On the other hand, MP-12 lacking functional NSs (rMP12-C13type) does not replicate efficiently in type-I IFN-competent cells, including MRC-5 cells, which were used for amplification of the MP-12 vaccine (Ikegami et al., 2006; Lokugamage et al., 2012). Recently, we found that TOSV NSs promotes PKR degradation (Kalveram & Ikegami, 2013). In addition, RVFV encoding TOSV NSs is known to inhibit IFN-β up-regulation (Gori Savellini et al., 2011). We hypothesized that recombinant MP-12 encoding TOSV NSs (rMP12-TOSNSs) replicates efficiently in type-I IFN-competent cells, including MRC-5 cells, and retains strong immunogenicity (Fig. 1a) (Ikegami et al., 2006; Kalveram & Ikegami, 2013). Cells infected with rMP12-TOSNSs showed clear cytopathic effects (CPE), and the plaque phenotype was very similar to that of parental MP-12 (Fig. 1b).
Fig. 1.
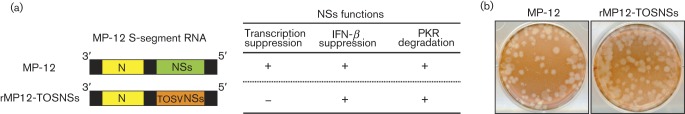
Generation of rMP12-TOSNSs. (a) Schematics of MP-12 S-segments encoding TOSV NSs in place of MP-12 NSs. The expected phenotype corresponding to each S-segment is also presented. (b) Plaque phenotypes of MP-12 and rMP12-TOSNSs at 4 days post-infection (p.i.).
Functional characterization of recombinant MP-12 encoding TOSV NSs
We have recently shown that rMP12-TOSNSs promotes PKR degradation in Vero E6 cells and does not suppress host general transcription (Kalveram & Ikegami, 2013). To determine if rMP12-TOSNSs inhibits the induction of IFN-β, mouse embryonic fibroblast (MEF) cells were mock-infected or infected with MP-12, rMP12-C13type or rMP12-TOSNSs at an m.o.i. of 3, and total RNA was extracted at 7 h post-infection (p.i.). Cells infected with rMP12-C13type accumulated abundant IFN-β and ISG56 mRNA, compared with those infected with MP-12 (Fig. 2). Cells infected with rMP12-TOSNSs inhibited IFN-β and ISG56 mRNA accumulation (Fig. 2). This result suggests that rMP12-TOSNSs promotes PKR degradation and largely inhibits IFN-β induction without inhibiting host general transcription.
Fig. 2.
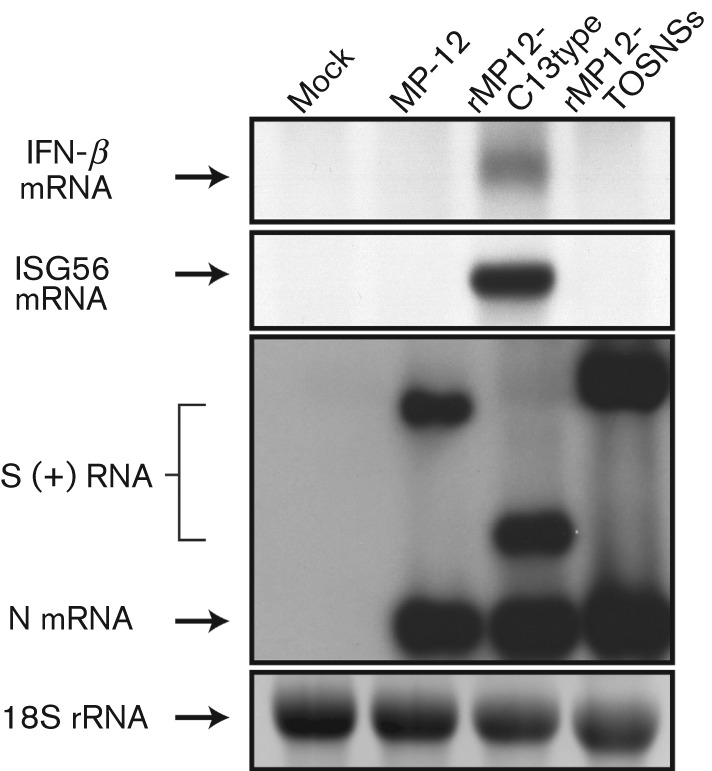
IFN-β gene suppression by rMP12-TOSNSs. MEF cells were mock-infected or infected with MP-12, rMP12-C13type or rMP12-TOSNSs at an m.o.i. of 3. Total RNA was collected at 7 h p.i., and the presence of mouse IFN-β mRNA, ISG56 mRNA, antiviral-sense S-segment and N mRNA of RVFV were tested by Northern blot (Lihoradova et al., 2012).
To evaluate the efficiency of replication in cultured cells, VeroE6 cells or MEF cells were infected with MP-12 or rMP12-TOSNSs at an m.o.i. of 0.01, and the virus titres of the culture supernatants were measured by plaque assay (Kalveram et al., 2011b). The rMP12-TOSNSs replicated 8.7- to 12.5-fold more efficiently than MP-12 in MEF cells at 96 and 120 h p.i., respectively (Fig. 3a). On the other hand, in VeroE6 cells and MRC-5 cells, rMP12-TOSNSs replication kinetics were almost identical to those of MP-12 (Fig. 3b, c).
Fig. 3.
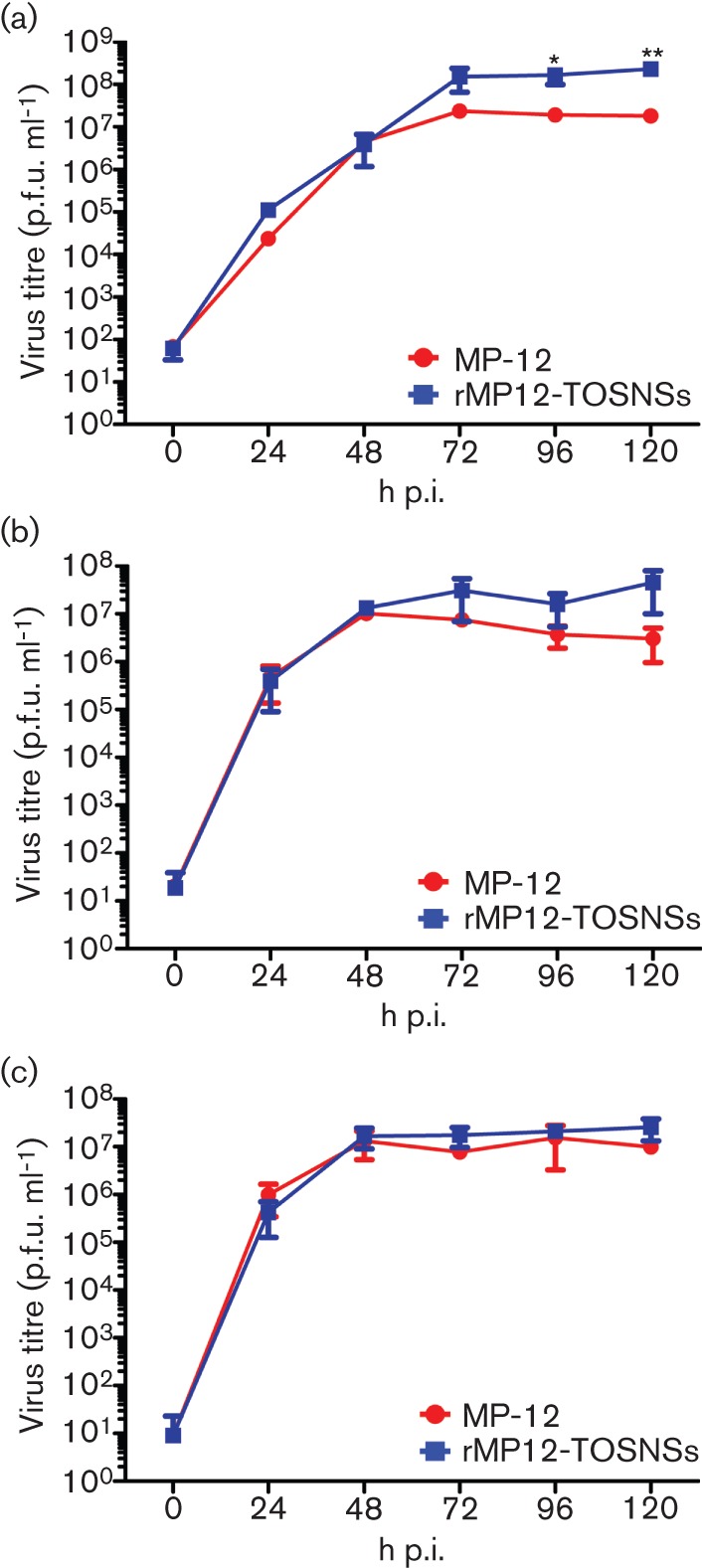
Replication of rMP12-TOSNSs in cell culture. (a) MEF cells, (b) VeroE6 cells or (c) MRC-5 cells were mock-infected or infected with MP-12 or rMP12-TOSNSs at an m.o.i. of 0.01. Culture supernatants were collected at indicated time points, and virus titre was determined by plaque assay with VeroE6 cells. Means±sd of at least three independent experiments are shown in each graph. Asterisks represent statistical significance (Unpaired Student's t-test, *P<0.05 and **P<0.01 vs MP-12).
Vaccine efficacy of rMP12-TOSNSs in outbred CD1 mice
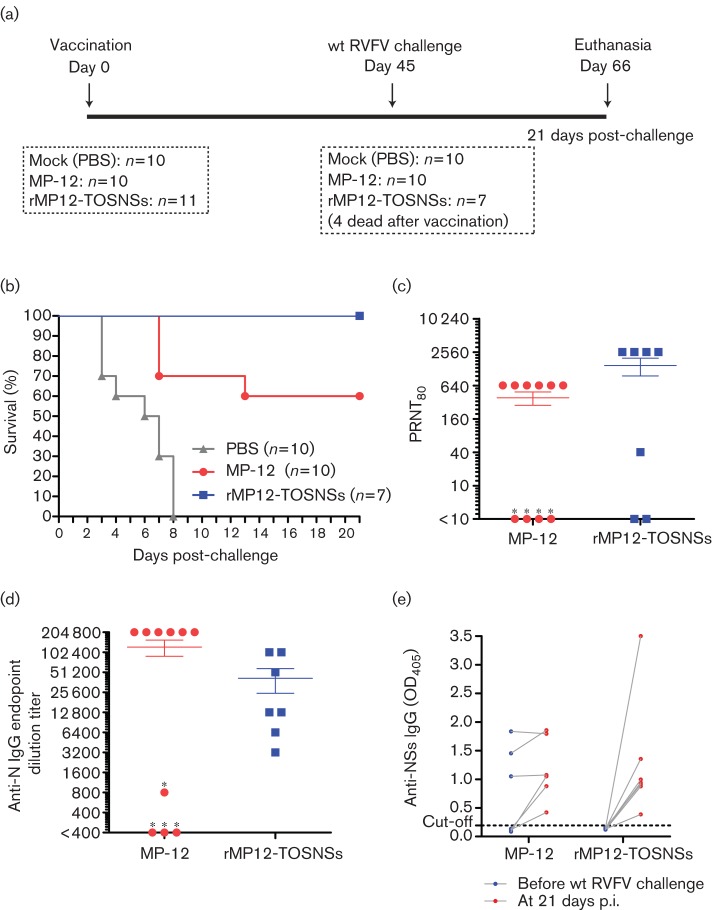
To evaluate the efficacy of rMP12-TOSNSs, 5- to 6-week-old outbred CD1 mice were subcutaneously (s.c.) vaccinated with 1×105 p.f.u. of MP-12 (n = 10) or rMP12-TOSNSs (n = 11) and observed for 45 days prior to challenge with wt RVFV ZH501 strain (Fig. 4a). At 3 days post-vaccination, 3 of 10 mice vaccinated with MP-12 developed a low level of viremia (200–500 p.f.u. ml-1), while none of the mice vaccinated with rMP12-TOSNSs developed detectable viremia at days 1, 2 and 3 (data not shown). Mice vaccinated with MP-12 all survived the vaccination for 45 days, whereas 4 of 11 (36%) mice vaccinated with rMP12-TOSNSs became moribund or died at day 12, 13 or 18 post-vaccination. CD1 outbred mice mock-vaccinated with PBS (n = 10) or vaccinated with MP-12 (n = 10) or rMP12-TOSNSs (n = 7) were challenged with RVFV ZH501 strain [1×103 p.f.u., intraperitoneally (i.p.)] at day 45 post-vaccination (Fig. 4a). All mock-vaccinated mice became moribund or died by 8 days p.i., and 4 out of 10 (40%) mice vaccinated with MP-12 became moribund or died at 7 or 13 days p.i. (Fig. 4b). Importantly, all mice vaccinated with rMP12-TOSNSs survived wt RVFV challenge (Fig. 4b). All of the mice vaccinated with MP-12 that succumbed to disease during challenge with wt RVFV lacked detectable levels of neutralizing antibodies (Fig. 4c) and had no or relatively low levels of anti-N antibody at day 42 post-vaccination (Fig. 4d). Mice vaccinated with rMP12-TOSNSs consisted of two groups: one group with a relatively high level of neutralizing antibodies (i.e. 1:2560) and the other with poor neutralizing antibody responses (i.e. 1:40 or less) (Fig. 4c). In contrast to mice vaccinated with MP-12, all mice vaccinated with rMP12-TOSNSs had high levels of anti-N antibodies (Fig. 4d). We also tested whether rMP12-TOSNSs is applicable to DIVA using a lack of anti-NSs antibody response as a negative DIVA marker (Fernandez et al., 2012; Lihoradova et al., 2012; McElroy et al., 2009). As expected, 3 of 10 (30%) mice vaccinated with MP-12 induced anti-NSs antibody before wt RVFV challenge, while none of mice vaccinated with rMP12-TOSNSs elicited anti-RVFV NSs antibody (Fig. 4e). Thus, rMP12-TOSNSs is highly efficacious and applicable to DIVA. However, although rMP12-TOSNSs is immunogenic, 4 out of 11 mice were dead after vaccination. Thus, we further analysed the safety of rMP12-TOSNSs.
Fig. 4.
Efficacy and immunogenicity of rMP12-TOSNSs in CD1 mice. (a) Schematics of vaccination and challenge schedule. CD1 mice mock-vaccinated with PBS or vaccinated with MP-12 or rMP12-TOSNSs (1×105 p.f.u., s.c.) were i.p. challenged with 1×103 p.f.u. of wt RVFV ZH501 strain at day 45 post-vaccination and observed for 21 days. (b) Kaplan−Meier survival curves of CD1 mice challenged with ZH501 strain. (c) Neutralizing antibody (plaque reduction neutralization test, PRNT80) titre at day 42 post-vaccination. Asterisk (*) represents dead mice after wt RVFV challenge. (d) Titre of anti-N IgG measured by IgG ELISA at day 42 post-vaccination. Asterisk (*) represents dead mice after wt RVFV challenge. (e) Anti-RVFV NSs IgG measured by IgG ELISA at day 42 post-vaccination (before wt RVFV challenge) and day 21 post-wt RVFV challenge. Note that this IgG ELISA does not distinguish antibodies to ZH501 NSs or MP-12 NSs. Optical density (OD405) values for 1:100 of each serum sample were plotted. The cut-off value (0.193) is shown as a dotted line.
Analysis of residual virulence of rMP12-TOSNSs
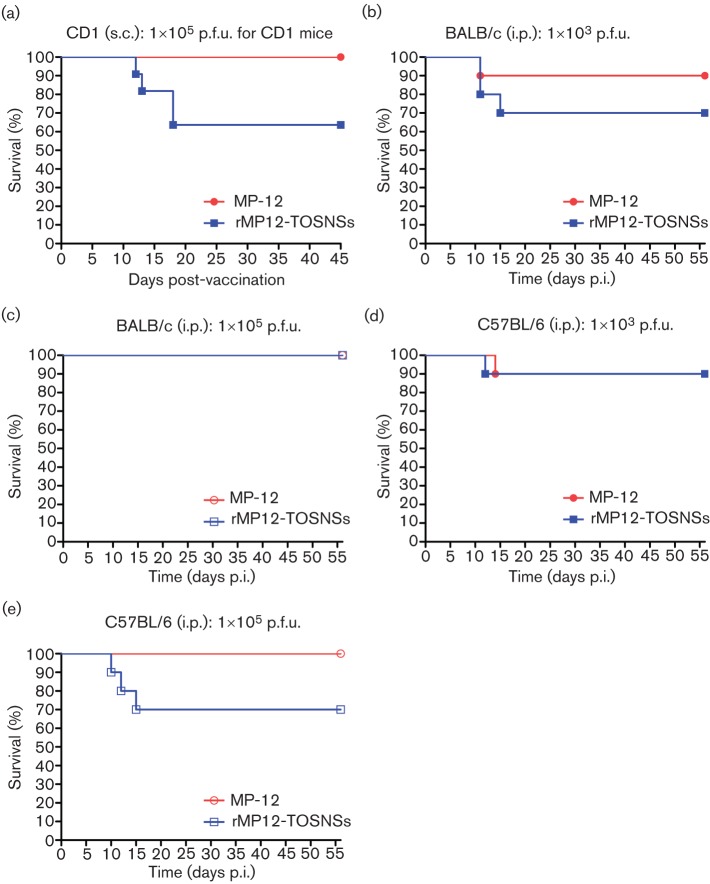
As described above, 36% of outbred CD1 mice vaccinated with rMP12-TOSNSs were dead or became moribund and were euthanized at days 12, 13 and 18 (Fig. 5a). For safety evaluation, we used genetically homogeneous inbred BALB/c and C57BL/6 mice and changed the inoculation route from s.c. to i.p. inoculation to ensure rapid systemic viral spread. BALB/c or C57BL/6 mice (4 weeks old) were mock-infected or infected with 1×103 or 1×105 p.f.u. of MP-12 or rMP12-TOSNSs (i.p.) and observed daily for 56 days. We noted that apparently healthy mice suddenly became sick (rough hair coat, less appetite, dehydration, slow moving with paralysis and/or closed eyes) and then became moribund within 24 h after onset of clinical signs of disease. Moribund animals were euthanized, and distributions of viral antigens in the liver, spleen and brain were evaluated. One out of 10 (10%) BALB/c mice inoculated with 1×103 p.f.u. of MP-12 was dead at day 11, while 3 out of 10 (30%) BALB/c mice inoculated with rMP12-TOSNSs were dead at days 11 and 15 (Fig. 5b). On the other hand, all BALB/c mice inoculated with 1×105 p.f.u. of MP-12 or rMP12-TOSNSs survived for 56 days (Fig. 5c). Thus, a higher dose of rMP12-TOSNSs did not cause disease in BALB/c mice. Meanwhile, 1 out of 10 (10%) of C57BL/6 mice inoculated with 1×103 p.f.u. MP-12 or rMP12-TOSNSs died at day 14 or day 12, respectively (Fig. 5d). At the higher dose (1×105 p.f.u.), 3 out of 10 (30%) of C57BL/6 mice were dead at days 10, 12 and 15, while all C57BL/6 mice inoculated with MP-12 survived for 56 days (Fig. 5e). In contrast to BALB/c mice, the susceptibility of C57BL/6 mice was high at 1×105 p.f.u. Although it was not statistically different, rMP12-TOSNSs induced higher mortality in mice than MP-12 with specific combinations: BALB/c mice with 1×103 p.f.u. or C57BL/6 with 1×105 p.f.u.
Fig. 5.
Survival of mice after vaccination with MP-12 or rMP12-TOSNSs. Kaplan−Meier survival curves of outbred CD1 mice (5–6 weeks old) s.c. vaccinated with 1×105 p.f.u. of MP-12 or rMP12-TOSNSs (a), those of BALB/c mice (4 weeks old) i.p. vaccinated with 1×103 (b) or 1×105 p.f.u. (c) of MP-12 or rMP12-TOSNSs, and those of C57BL/6 mice (4 weeks old) i.p. vaccinated with 1×103 (d) or 1×105 p.f.u. (e) of MP-12 or rMP12-TOSNSs.
Next, we analysed viral N antigen distribution in moribund inbred mice. Reagent negative controls that consisted of samples in which primary antibody was replaced with rabbit IgG did not produce detectable signals (data not shown). We noted that the viral antigen distribution of mice infected with parental MP-12 was similar to that of infected with rMP12-TOSNSs. No viral antigen was detected in liver or spleen but was most abundantly detected in the thalamus, hypothalamus and brainstem around the medulla (Fig. 6a, b). Viral antigens were sporadically or focally found in cerebral cortex (Fig. 6c, d), hippocampus (Fig. 6j) and cerebellum (Fig.6i). Viral antigens were also diffusely detected throughout the thalamus (Fig. 6e, f), hypothalamus and medulla (Fig. 6g, h). We did not observe prominent perivascular cuffing or meningitis in the moribund mice. These results suggest that rMP12-TOSNSs retains a neurovirulence similar to that of parental MP-12.
Fig. 6.
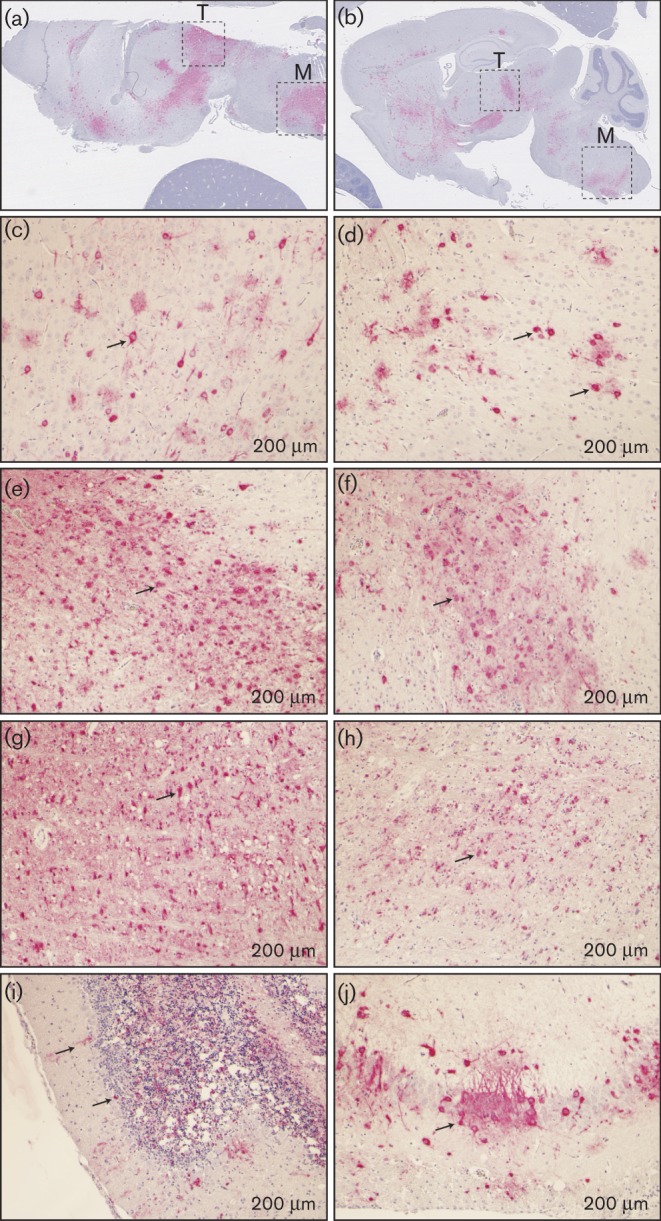
RVFV antigen distribution in mouse brain after vaccination. Brain tissues derived from euthanized moribund inbred mice after vaccination with MP-12 (a, c, e and g) or rMP12-TOSNSs (b, d, f, h, i and j) were subjected to immunohistochemistry using anti-RVFV N antibody. Signal specific to RVFV N antigen was developed as red, while counterstain with haematoxylin is shown as blue. (a and b) Overall antigen distributions in brain tissue are shown as red signals. T, Thalamus, M, medulla. Antigen distribution in cerebral cortex (c and d), thalamus (e and f), medulla (g and h), cerebellum (i) and hippocampus (j) are shown. Arrows indicate cells with RVFV N antigens. Bars, 200 μm.
To further evaluate the presence of MP-12 or rMP12-TOSNSs in the brain, we performed reverse transcription (RT)-PCR to amplify 522 bp of the 3′ end of the viral-sense S-segment, including a part of the N ORF. Although all brain samples derived from moribund mice contained viral RNA, no PCR products were amplified from brain samples derived from mice that survived (56 days p.i.) (Fig. S1, available in JGV Online). The results suggest that MP-12 and rMP12-TOSNSs did not replicate in brains of mice that survived through 56 days p.i.
Among the survivors, neutralizing antibodies were detected in 6 of 9 (67%) or 9 of 10 (90%) BALB/c mice inoculated with 1×103 or 1×105 p.f.u. of MP-12, respectively (Fig. S2a). Neutralizing antibodies were also detected in 6 of 7 (86%) or 10 of 10 (100%) BALB/c mice inoculated with 1×103 or 1×105 p.f.u. of rMP12-TOSNSs, respectively (Fig. S2a). In C57BL/6 mice, neutralizing antibodies were detected in 5 of 9 (43%) or 10 of 10 (100%) of mice inoculated with 1×103 or 1×105 p.f.u. of MP-12, respectively, and neutralizing antibodies were detected in 9 of 9 (100%) or 7 of 7 (100%) of the mice inoculated with 1×103 or 1×105 p.f.u. of rMP12-TOSNSs, respectively (Fig. S2b). These results suggest that rMP12-TOSNSs induces neutralizing antibodies in the majority of vaccinated mice at both 1×103 and 1×105 p.f.u. doses, whereas MP-12 does not efficiently induce neutralizing antibodies at the 1×103 p.f.u. dose.
Discussion
The NSs protein has been identified as the major virulence factor for RVFV (Bouloy et al., 2001). The NSs proteins of the other phleboviruses have been poorly characterized due to the lack of virulent animal models (Tesh, 1988) and reverse-genetics systems. Previous studies have suggested that authentic TOSV weakly induces IFN-β in infected cells, while a recombinant RVFV ZH548 strain encoding TOSV NSs could inhibit the induction of IFN-β (Gori Savellini et al., 2011). Thus, the neuroinvasiveness of TOSV among phleboviruses and the involvement of NSs has been an enigma. We recently found that TOSV NSs can promote PKR degradation (Kalveram & Ikegami, 2013). We subsequently found that recombinant MP-12 encoding TOSV NSs (rMP12-TOSNSs) is viable, inhibits IFN-β induction and promotes PKR degradation. MP-12 does not cause liver damage in vaccinated mice, but it sometimes enters the brain and causes lethal encephalitis (approximately 5%). Although MP-12 consists of genetic subpopulations different from recombinant MP-12 (rMP-12) (Lokugamage et al., 2012), outbred CD1 mice infected with rMP-12 do not exhibit any increase in neurological diseases compared to those inoculated with MP-12 vaccine (J. C. Morrill, personal communication). Unexpectedly, we found that rMP12-TOSNSs could increase viral neuroinvasion by approximately 30% in both outbred and inbred mice compared with the parental MP-12 strain. Our results suggest that NSs serves as a major virulence factor of TOSV.
Viral RNA and antigens were found in the brain but not the liver of moribund mice. Parental MP-12 caused neurological diseases at a frequency of approximately 5%. The MP-12 S-segment is virulent with intact NSs functions, while the M- and L-segment encode presumable attenuation mutations (Billecocq et al., 2008; Lokugamage et al., 2012). Such infrequent occurrence of neurological disease is similar to human RVF (Ikegami & Makino, 2011). Neurological disorder occurs weeks or months after clinical symptom onset in less than 2% of RVF patients, and neutralizing antibodies are usually detectable before the onset of neurological disease (Ikegami & Makino, 2011). On the other hand, mice are highly susceptible to wt RVFV, and most die from acute hepatitis. However, mice that survive lethal hepatitis subsequently develop lethal encephalitis (Smith et al., 2010). In the gerbil model, wt RVFV causes mainly encephalitis with minimal liver injury (Anderson et al., 1988). RVFV lacking 78 kDa/NSm or that encodes a point mutation at nt 847 in the M-segment that substitutes Ala with Gly in Gn induce neurological diseases rather than hepatic diseases (Bird et al., 2007; Morrill et al., 2010). However, animal models using wt RVFV require the use of a high containment facility, and detailed analysis of the neuroinvasion mechanism demands special facilities and personnel. Our mouse model infected with rMP12-TOSNSs causes neurological disease 1–2 weeks after inoculation without liver damage in BSL2 level facilities and will be useful for the study of neuroinvasion mechanisms of RVFV or TOSV. We believe that this model is also useful for screening antivirals or post-exposure vaccines for reducing neurological sequelae in RVF patients.
The mechanism of increased neuroinvasion of rMP12-TOSNSs compared with parental MP-12 remains largely unknown as the only difference between the two viruses is the NSs protein. A major difference between the function of RVFV NSs and TOSV NSs is host general transcription suppression. RVFV NSs sequesters TFIIH p44 subunits (Le May et al., 2004) and promotes the degradation of TFIIH p62 (Kalveram et al., 2011a), which leads to the inhibition of host RNA polymerases I and II. Our study suggests that rMP12-TOSNSs does not inhibit host general transcription. Also, we found that CD11c-positive dendritic cells are primarily infected with MP-12 upon vaccination (Lihoradova et al., 2012). Dendritic cells infected with MP-12 lacking NSs (rMP12-C13type) accumulated in local draining lymph nodes upon infection, while those infected with parental MP-12 were not found in draining lymph nodes (Lihoradova et al., 2012). Thus, it is likely that cells infected with rMP12-TOSNSs induce cytokines/chemokines that are distinct from those induced by parental MP-12. West Nile virus is known to compromise the integrity of the blood–brain barrier by stimulating Toll-like receptor 3, which induces tumor necrosis factor-α and interleukin-6 in sera (Wang et al., 2004). It is also possible that unknown TOSV NSs function(s) might play a role in neuroinvasion. Interestingly, a 1×105 p.f.u. dose of rMP12-TOSNSs did not induce neurological disease in BALB/c mice. Host defence systems specific to BALB/c mice might be important for the protection of neuroinvasion induced by rMP12-TOSNSs. Further studies will be required to elucidate the mechanism of neuroinvasion by rMP12-TOSNSs.
Our initial goal was to develop a highly efficacious MP-12 mutant that encoded a DIVA marker and replicated efficiently in MRC-5 cells. The rMP12-TOSNSs was, in fact, highly efficacious in mice and replicated efficiently in MRC-5 cells, and the lack of the MP-12 NSs gene was useful as a DIVA marker. As far as we know, the rMP12-TOSNSs is one of the most efficacious MP-12 mutants in the outbred CD1 mouse model. We previously showed that MP-12 encoding a dominant-negative form of mouse PKR (rMP12-mPKRN167) is highly efficacious without residual virulence (Lihoradova et al., 2012). The rMP12-mPKRN167, which inhibits the activation of mouse PKR, still induces abundant type-I IFNs (Lihoradova et al., 2012). The suppression of PKR by rMP12-mPKRN167 is species-specific. Thus, we expected that rMP12-TOSNSs could be highly efficacious by promoting PKR degradation. However, we encountered an unexpected increase in rMP12-TOSNSs neuroinvasiveness in mice. Future studies might improve on this vaccine candidate by abolishing this effect.
Methods
Media, cells and viruses.
VeroE6 cells [American Tissue Culture Collection (ATCC) CRL-1586], MRC-5 cells (ATCC CCL-171) and MEF cells (Yang et al., 1995) were maintained in Dulbecco's modified Eagle medium containing 10% FCS. BHK/T7-9 cells that stably express T7 RNA polymerase (Ito et al., 2003) were maintained in minimal essential medium-alpha (Life Technologies) containing 10% FCS with 600 μg ml-1 hygromycin. Penicillin (100 U ml-1) and streptomycin (100 μg ml-1) were added to the culture media. MP-12 vaccine Lot 7-2-88 (kindly provided by Dr J. C. Morrill at the University of Texas Medical Branch: UTMB) was amplified twice in MRC-5 cells for experiments. Generation of rMP12-TOSNSs was described previously (Kalveram & Ikegami, 2013), and passaged once in VeroE6 cells. RVFV ZH501 strain stock was generated after one VeroE6 cell passage of an original ZH501 reference collection vial at UTMB (Morrill et al., 2010).
Northern blot analysis.
Northern blot analysis was performed as described previously (Kalveram et al., 2013). ssRNA probes specific to mouse IFN-β mRNA, mouse ISG56 mRNA or RVFV antiviral-sense S-segment were used for detection (Kalveram et al., 2013).
Analysis of virus replication.
VeroE6 cells, wt MEF cells or MRC-5 cells were infected with MP-12 or rMP12-TOSNSs at an m.o.i. of 0.01 at 37 °C for 1 h, washed twice with media, and incubated at 37 °C. Culture supernatants were collected at indicated time points, and titrated by plaque assay (Ikegami et al., 2006; Kalveram et al., 2011b).
Vaccination and virus challenge using outbred CD1 mice.
For efficacy testing of rMP12-TOSNSs, 5- to 6-week-old female CD1 outbred mice (Charles River, North Franklin, CT) were inoculated s.c. with PBS (mock) (n = 10) or 1×105 p.f.u. of MP-12 (n = 10) or rMP12-TOSNSs (n = 10). Sera were collected from mice by retro-orbital bleeding at 1, 2, 3 and 42 days p.i., and mice were challenged with 1×103 p.f.u. of wt RVFV ZH501 strain (i.p.) at 45 days p.i. The challenge experiment was performed at the UTMB Robert E. Shope animal BSL4 facility. Mice were observed for 21 days, and body weight was monitored daily. Survival curves of mice (Kaplan−Meier method) were analysed using Graphpad Prism 5.03 (Graphpad Software).
Evaluation of neuroinvasiveness of MP-12 and rMP12-TOSNSs using inbred mice.
For testing the neuroinvasiveness of MP-12 and rMP12-TOSNSs, 4-week-old BALB/c mice and C57BL/6 mice were i.p. mock-vaccinated (n = 5 each), or vaccinated with MP-12 (n = 10 each) or rMP12-TOSNSs (n = 10 each) (1×103 or 1×105 p.f.u.). Following vaccination, mice were observed daily for 56 days. Mice with paralysis in all four limbs were defined as moribund. Moribund mice were euthanized and all organs including brains were fixed in 10% buffered formalin for immunohistochemistry.
Reverse transcription (RT)-PCR.
Total RNA was extracted from brain tissues from all the surviving mice vaccinated with MP-12 or rMP12-TOSNSs using TRIzol reagent (Invitrogen). Then, first-stranded cDNA was synthesized by using High Capacity cDNA Reverse Transcription Kit (Applied Biosystems). RT-PCR was performed by using the primer pair S20F (nt 1−20) and S522R (nt 501 −522), which can amplify the 522 nt at the 3′ end of viral-sense S-segment RNA, including a partial N ORF (Lokugamage et al., 2012). PCR was performed by using Phusion DNA polymerase (New England BioLabs) with the following conditions: 98 °C for 2 min, followed by 35 cycles of 98 °C for 10 s, 55 °C for 30 s and 72 °C for 30 s. As positive controls, pProT7-S(+) plasmid or cDNA derived from VeroE6 cells infected with MP-12 were used.
Plaque reduction neutralization test.
The PRNT80 was determined as described previously (Lihoradova et al., 2012). Eighty percent of the average number of plaques in six different wells that had mock-immunized mice sera was used as the cut-off number (typically 8−9). The highest dilution of sera that produced the number of plaques below the cut-off number was designated as the PRNT80 neutralizing antibody titre.
IgG-ELISA.
IgG-ELISAs using His-tagged RVFV N proteins or purified GST-tagged RVFV NSs C-terminal 48 aa were described previously (Lihoradova et al., 2012). 2, 2'-azino-bis(3-ethylbenzthiazoline-6-sulphonic acid) (ABTS) was used as substrate, and the optical density (OD) at 405 nm was determined. The cut-off value, 0.176, was defined as the mean + 2× sd of 24 normal mouse serum samples (1:400) for anti-N IgG, while the cut-off value of 0.193 was defined as the mean + 3× sd of 48 normal mouse serum samples for anti-NSs IgG. The highest dilution of sera that generated an OD405 value larger than the cut-off was designated as the anti-N antibody titre. Because the anti-NSs antibody level was low, an OD405 value of a 1:100 dilution was used for demonstrating its presence.
Immunohistochemistry.
Immunohistochemistry of brain, liver and spleen sections were performed using anti-RVFV N antibody. Tissues of the euthanized mice were fixed with 10% buffered formalin, and paraffin blocks were generated for pathological evaluation. Deparaffinized sections were incubated for 2 h with anti-RVFV N rabbit polyclonal antibody (Lihoradova et al., 2012), followed by incubation for 30 min with biotinylated anti-rabbit IgG (BA-1000, Vector Laboratories). Signals were detected by using an UltraVision Alk-Phos kit (TS-060-AP, Thermo Scientific). Vector Red Alkaline Phosphatase substrate (SK-5100, Vector Laboratories) was used as a chromogen, and counter-staining was performed with haematoxylin.
Statistical analysis.
Statistical analyses were performed with the Graphpad Prism 5.03 program (Graphpad Software). Unpaired Student's t-test or Mann−Whitney U test was used for the comparison of two groups. Survival curves of mice were analysed by log-rank (Mantel−Cox) test.
Ethics statement.
Mouse studies were performed in facilities accredited by the Association for Assessment and Accreditation of Laboratory Animal Care (AAALAC) in accordance to the Animal Welfare Act, NIH guidelines and USA federal law. The animal protocol was approved by the UTMB Institutional Animal Care and Use Committee (IACUC). All recombinant DNA and RVFV were created upon the approval of the Notification of Use by the Institutional Biosafety Committee at UTMB. The wt RVFV ZH501 strain was used at the Robert E. Shope BSL4 laboratory at UTMB in accordance with NIH guidelines and USA federal law.
Acknowledgements
We thank Dr R. B. Tesh (UTMB) for providing TOSV and mouse antisera against TOSV or RVFV and Dr S. Makino (UTMB) for the anti-RVFV N antibody. We thank Dr J. C. Morrill for helpful discussion regarding the mouse experiment using recombinant MP-12. This study was supported through the Western Regional Center of Excellence by 5 U54 AI057156, NIH grant R01 AI08764301 and funding from the Sealy Center for Vaccine Development at UTMB. B. K. was supported by the James W. McLaughlin Fellowship Fund at UTMB. O.A.L. was supported by the Maurice R. Hilleman Early-Stage Career Investigator Award. The funders had no role in study design, data collection and analysis or the decision to publish.
Footnotes
Two supplementary figures are available with the online version of this paper.
References
- Anderson G. W., Jr, Slone T. W., Jr, Peters C. J. (1988). The gerbil, Meriones unguiculatus, a model for Rift Valley fever viral encephalitis. Arch Virol 102, 187–196 10.1007/BF01310824 [DOI] [PubMed] [Google Scholar]
- Austin D., Baer A., Lundberg L., Shafagati N., Schoonmaker A., Narayanan A., Popova T., Panthier J. J., Kashanchi F. & other authors (2012). p53 Activation following Rift Valley fever virus infection contributes to cell death and viral production. PLoS ONE 7, e36327 10.1371/journal.pone.0036327 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baer A., Austin D., Narayanan A., Popova T., Kainulainen M., Bailey C., Kashanchi F., Weber F., Kehn-Hall K. (2012). Induction of DNA damage signaling upon Rift Valley fever virus infection results in cell cycle arrest and increased viral replication. J Biol Chem 287, 7399–7410 10.1074/jbc.M111.296608 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Billecocq A., Gauliard N., Le May N., Elliott R. M., Flick R., Bouloy M. (2008). RNA polymerase I-mediated expression of viral RNA for the rescue of infectious virulent and avirulent Rift Valley fever viruses. Virology 378, 377–384 10.1016/j.virol.2008.05.033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bird B. H., Albariño C. G., Nichol S. T. (2007). Rift Valley fever virus lacking NSm proteins retains high virulence in vivo and may provide a model of human delayed onset neurologic disease. Virology 362, 10–15 10.1016/j.virol.2007.01.046 [DOI] [PubMed] [Google Scholar]
- Bouloy M., Janzen C., Vialat P., Khun H., Pavlovic J., Huerre M., Haller O. (2001). Genetic evidence for an interferon-antagonistic function of rift valley fever virus nonstructural protein NSs. J Virol 75, 1371–1377 10.1128/JVI.75.3.1371-1377.2001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caplen H., Peters C. J., Bishop D. H. (1985). Mutagen-directed attenuation of Rift Valley fever virus as a method for vaccine development. J Gen Virol 66, 2271–2277 10.1099/0022-1317-66-10-2271 [DOI] [PubMed] [Google Scholar]
- Cêtre-Sossah C., Zeller H., Grandadam M., Caro V., Pettinelli F., Bouloy M., Cardinale E., Albina E. (2012). Genome analysis of Rift Valley fever virus, Mayotte. Emerg Infect Dis 18, 969–971 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daubney R., Hudson J. R., Garnham P. C. (1931). Enzootic hepatitis or Rift Valley fever: an undescribed virus disease of sheep cattle and man from east Africa. J Pathol Bacteriol 34, 545–579 10.1002/path.1700340418 [DOI] [Google Scholar]
- Fernandez J. C., Billecocq A., Durand J. P., Cêtre-Sossah C., Cardinale E., Marianneau P., Pépin M., Tordo N., Bouloy M. (2012). The nonstructural protein NSs induces a variable antibody response in domestic ruminants naturally infected with Rift Valley fever virus. Clin Vaccine Immunol 19, 5–10 10.1128/CVI.05420-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gale M., Jr, Tan S. L., Katze M. G. (2000). Translational control of viral gene expression in eukaryotes. Microbiol Mol Biol Rev 64, 239–280 10.1128/MMBR.64.2.239-280.2000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gori Savellini G., Weber F., Terrosi C., Habjan M., Martorelli B., Cusi M. G. (2011). Toscana virus induces interferon although its NSs protein reveals antagonistic activity. J Gen Virol 92, 71–79 10.1099/vir.0.025999-0 [DOI] [PubMed] [Google Scholar]
- Grobbelaar A. A., Weyer J., Leman P. A., Kemp A., Paweska J. T., Swanepoel R. (2011). Molecular epidemiology of Rift Valley fever virus. Emerg Infect Dis 17, 2270–2276 10.3201/eid1712.111035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Habjan M., Pichlmair A., Elliott R. M., Overby A. K., Glatter T., Gstaiger M., Superti-Furga G., Unger H., Weber F. (2009). NSs protein of rift valley fever virus induces the specific degradation of the double-stranded RNA-dependent protein kinase. J Virol 83, 4365–4375 10.1128/JVI.02148-08 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ikegami T. (2012). Molecular biology and genetic diversity of Rift Valley fever virus. Antiviral Res 95, 293–310 10.1016/j.antiviral.2012.06.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ikegami T., Makino S. (2011). The pathogenesis of Rift Valley fever. Viruses 3, 493–519 10.3390/v3050493 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ikegami T., Won S., Peters C. J., Makino S. (2006). Rescue of infectious rift valley fever virus entirely from cDNA, analysis of virus lacking the NSs gene, and expression of a foreign gene. J Virol 80, 2933–2940 10.1128/JVI.80.6.2933-2940.2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ikegami T., Narayanan K., Won S., Kamitani W., Peters C. J., Makino S. (2009). Rift Valley fever virus NSs protein promotes post-transcriptional downregulation of protein kinase PKR and inhibits eIF2alpha phosphorylation. PLoS Pathog 5, e1000287 10.1371/journal.ppat.1000287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ito N., Takayama-Ito M., Yamada K., Hosokawa J., Sugiyama M., Minamoto N. (2003). Improved recovery of rabies virus from cloned cDNA using a vaccinia virus-free reverse genetics system. Microbiol Immunol 47, 613–617 [DOI] [PubMed] [Google Scholar]
- Kalveram B., Ikegami T. (2013). Toscana Virus NSs Protein Promotes Degradation of Double-Stranded RNA-Dependent Protein Kinase. J Virol 87, 3710–3718 10.1128/JVI.02506-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalveram B., Lihoradova O., Ikegami T. (2011a). NSs protein of rift valley fever virus promotes posttranslational downregulation of the TFIIH subunit p62. J Virol 85, 6234–6243 10.1128/JVI.02255-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalveram B., Lihoradova O., Indran S. V., Ikegami T. (2011b). Using reverse genetics to manipulate the NSs gene of the Rift Valley fever virus MP-12 strain to improve vaccine safety and efficacy. J Vis Exp 57, e3400 10.3791/3400 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalveram B., Lihoradova O., Indran S. V., Lokugamage N., Head J. A., Ikegami T. (2013). Rift Valley fever virus NSs inhibits host transcription independently of the degradation of dsRNA-dependent protein kinase PKR. Virology 435, 415–424 10.1016/j.virol.2012.09.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Le May N., Dubaele S., De Santis L. P., Billecocq A., Bouloy M., Egly J. M. (2004). TFIIH transcription factor, a target for the Rift Valley hemorrhagic fever virus. Cell 116, 541–550 10.1016/S0092-8674(04)00132-1 [DOI] [PubMed] [Google Scholar]
- Le May N., Mansuroglu Z., Léger P., Josse T., Blot G., Billecocq A., Flick R., Jacob Y., Bonnefoy E., Bouloy M. (2008). A SAP30 complex inhibits IFN-beta expression in Rift Valley fever virus infected cells. PLoS Pathog 4, e13 10.1371/journal.ppat.0040013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lihoradova O., Kalveram B., Indran S. V., Lokugamage N., Juelich T. L., Hill T. E., Tseng C. T., Gong B., Fukushi S. & other authors (2012). The dominant-negative inhibition of double-stranded RNA-dependent protein kinase PKR increases the efficacy of Rift Valley fever virus MP-12 vaccine. J Virol 86, 7650–7661 10.1128/JVI.00778-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linthicum K. J., Davies F. G., Kairo A., Bailey C. L. (1985). Rift Valley fever virus (family Bunyaviridae, genus Phlebovirus). Isolations from Diptera collected during an inter-epizootic period in Kenya. J Hyg (Lond) 95, 197–209 10.1017/S0022172400062434 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lokugamage N., Freiberg A. N., Morrill J. C., Ikegami T. (2012). Genetic subpopulations of Rift Valley fever virus strains ZH548 and MP-12 and recombinant MP-12 strains. J Virol 86, 13566–13575 10.1128/JVI.02081-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mansuroglu Z., Josse T., Gilleron J., Billecocq A., Leger P., Bouloy M., Bonnefoy E. (2010). Nonstructural NSs protein of rift valley fever virus interacts with pericentromeric DNA sequences of the host cell, inducing chromosome cohesion and segregation defects. J Virol 84, 928–939 10.1128/JVI.01165-09 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McElroy A. K., Albariño C. G., Nichol S. T. (2009). Development of a RVFV ELISA that can distinguish infected from vaccinated animals. Virol J 6, 125 10.1186/1743-422X-6-125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morrill J. C., Jennings G. B., Caplen H., Turell M. J., Johnson A. J., Peters C. J. (1987). Pathogenicity and immunogenicity of a mutagen-attenuated Rift Valley fever virus immunogen in pregnant ewes. Am J Vet Res 48, 1042–1047 [PubMed] [Google Scholar]
- Morrill J. C., Carpenter L., Taylor D., Ramsburg H. H., Quance J., Peters C. J. (1991). Further evaluation of a mutagen-attenuated Rift Valley fever vaccine in sheep. Vaccine 9, 35–41 10.1016/0264-410X(91)90314-V [DOI] [PubMed] [Google Scholar]
- Morrill J. C., Mebus C. A., Peters C. J. (1997a). Safety and efficacy of a mutagen-attenuated Rift Valley fever virus vaccine in cattle. Am J Vet Res 58, 1104–1109 [PubMed] [Google Scholar]
- Morrill J. C., Mebus C. A., Peters C. J. (1997b). Safety of a mutagen-attenuated Rift Valley fever virus vaccine in fetal and neonatal bovids. Am J Vet Res 58, 1110–1114 [PubMed] [Google Scholar]
- Morrill J. C., Ikegami T., Yoshikawa-Iwata N., Lokugamage N., Won S., Terasaki K., Zamoto-Niikura A., Peters C. J., Makino S. (2010). Rapid accumulation of virulent Rift Valley Fever virus in mice from an attenuated virus carrying a single nucleotide substitution in the m RNA. PLoS ONE 5, e9986 10.1371/journal.pone.0009986 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morrill J. C., Laughlin R. C., Lokugamage N., Pugh R., Sbrana E., Weise W. J., Adams L. G., Makino S., Peters C. J. (2013). Safety and immunogenicity of recombinant Rift Valley Fever MP-12 vaccine candidates in sheep. Vaccine 31, 559–565 10.1016/j.vaccine.2012.10.118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pepin M., Bouloy M., Bird B. H., Kemp A., Paweska J. (2010). Rift Valley fever virus (Bunyaviridae: Phlebovirus): an update on pathogenesis, molecular epidemiology, vectors, diagnostics and prevention. Vet Res 41, 61 10.1051/vetres/2010033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmaljohn C., Nichol S. T. (2007). Bunyaviridae . In Fields Virology, 5th edn, pp. 1741–1789. Edited by Knipe D. M., Howley P. M., Griffin D. E., Lamb R. A., Martin M. A., Roizman B., Straus. S. E. Philadelphia, PA: Lipincott, Williams & Wilkins [Google Scholar]
- Smith D. R., Steele K. E., Shamblin J., Honko A., Johnson J., Reed C., Kennedy M., Chapman J. L., Hensley L. E. (2010). The pathogenesis of Rift Valley fever virus in the mouse model. Virology 407, 256–267 10.1016/j.virol.2010.08.016 [DOI] [PubMed] [Google Scholar]
- Swanepoel R., Coetzer J. A. W. (2004). Rift Valley fever. In Infectious Diseases of Livestock with Special Reference to Southern Africa, 2nd edn, pp. 1037–1070 Edited by Coetzer J. A. W., Tustin R. C. Cape Town, South Africa: Oxford University Press [Google Scholar]
- Tesh R. B. (1988). The genus Phlebovirus and its vectors. Annu Rev Entomol 33, 169–181 10.1146/annurev.en.33.010188.001125 [DOI] [PubMed] [Google Scholar]
- Wang T., Town T., Alexopoulou L., Anderson J. F., Fikrig E., Flavell R. A. (2004). Toll-like receptor 3 mediates West Nile virus entry into the brain causing lethal encephalitis. Nat Med 10, 1366–1373 10.1038/nm1140 [DOI] [PubMed] [Google Scholar]
- Xu F., Chen H., Travassos da Rosa A. P., Tesh R. B., Xiao S. Y. (2007). Phylogenetic relationships among sandfly fever group viruses (Phlebovirus: Bunyaviridae) based on the small genome segment. J Gen Virol 88, 2312–2319 10.1099/vir.0.82860-0 [DOI] [PubMed] [Google Scholar]
- Yang Y. L., Reis L. F., Pavlovic J., Aguzzi A., Schäfer R., Kumar A., Williams B. R., Aguet M., Weissmann C. (1995). Deficient signaling in mice devoid of double-stranded RNA-dependent protein kinase. EMBO J 14, 6095–6106 [DOI] [PMC free article] [PubMed] [Google Scholar]