Abstract
Intrafractional setup errors during hypofractionated stereotactic radiotherapy (SRT) were investigated on the patient under voluntary breath-holding conditions with non-invasive immobilization on the CT-linac treatment table. A total of 30 patients with primary and metastatic lung tumors were treated with the hypofractionated SRT with a total dose of 48–60 Gy with four treatment fractions. The patient was placed supine and stabilized on the table with non-invasive patient fixation. Intrafractional setup errors in Right/Left (R.L.), Posterior/Anterior (P.A.), and Inferior/Superior (I.S.) dimensions were analyzed with pre- and post-irradiation CT images. The means and one standard deviation of the intrafractional errors were 0.9 ± 0.7mm (R.L.), 0.9 ± 0.7mm (P.A.) and 0.5 ± 1.0 mm (I.S.). Setup errors in each session of the treatment demonstrated no statistically significant difference in the mean value between any two sessions. The frequency within 3mm displacement was 98% in R.L., 98% in P.A. and 97% in I.S. directions. SRT under the non-invasive patient fixation immobilization system with a comparatively loose vacuum pillow demonstrated satisfactory reproducibility of minimal setup errors with voluntary breath-holding conditions that required a small internal margin.
Keywords: intrafractional setup errors, hypofractionated stereotactic radiotherapy, lung cancers, non-invasive patient fixation immobilization
INTRODUCTION
Minimizing intrafractional setup errors is a fundamental requirement in tumor targeting in lung stereotactic radiotherapy (SRT). The intrafractional setup error is defined as displacement of distance of the patient trunk during the irradiation therapy. Historically, various rigid immobilization devices were introduced to stabilize the patient on the treatment coach during lung SRT [1–2], which eventually minimizes intrafractional setup errors. However, rigid immobilization devices tend to be costly, to cause pain to the patients, and to limit patient respiration. On the other hand, non-invasive patient fixation using a comparatively loose vacuum pillow allows a patient to breathe naturally on the coach without any restriction to the patient's chest wall motion, which may be preferable in lung SRT for those with impaired pulmonary function.
The effectiveness of using a respiration-synchronizing device has been reported previously. Most of them provide quality assurance, shorten treatment time, and increase safety and consistency [2–3]. With the respiration-synchronizing device, controlling target movement during irradiation is achieved by breath-holding. Voluntary breath-holding is crucial to achieve a precise targeting of irradiation. A voluntary breath-holding technique with the respiration-synchronizing device is preferable, and is increasingly used for lung SRT [4].
A high degree of respiratory control with the respiration-synchronizing device requires patient cooperation during the procedure. In order to maximize patient cooperation, non-invasive patient fixation using a comparatively loose vacuum pillow is preferred to rigid patient fixation when the respiration-synchronizing device is used. A rigid patient fixation device may cause pain to the patient on the coach and cause the patient to move due to the pain. Particularly, patients with higher age, and/or with poor pulmonary function receive benefits from the use of non-invasive patient fixation of the chest.
Various devices and techniques, such as breath-holding [5–7], respiratory gating [8], or beam tracking [9], can be used to minimize internal motion during SRT. As mentioned above, we have been using a respiration-synchronizing device and a voluntary breath-holding technique with a non-invasive patient fixation system for lung SRT.
When a non-invasive patient fixation system is used during lung SRT with a combination of a respiration-synchronizing device, it is crucial to minimize intrafractional setup errors in order to maximize the effect of breath-holding, which minimizes internal motion.
Although intrafractional setup errors under rigid immobilization devices have been reported [2], little has been known about the intrafractional setup errors during lung SRT with a non-invasive patient fixation system. In the present study, we retrospectively analyzed intrafractional setup errors with a non-invasive patient fixation system during lung SRT.
MATERIALS AND METHODS
Eligibility criteria
Eligibility criteria for the patients reviewed in this study were as follows: (i) identification of Stage IA (T1N0M0) or IB (T2N0M0) primary lung cancer, or a single lung lesion of metastasis, confirmed on chest and abdominal CT, bronchoscopy, bone scintigram, and brain magnetic resonance imaging; (ii) histologically confirmed NSCLC; (iii) demonstrated ability to understand and perform self-breath-hold with aid of a respiratory monitoring device; (iv) demonstrated ability to maintain breath-hold for more than 10 seconds. Patients were informed of the rationale for this treatment including the concept and methodology.
Patient characteristics
A total of 36 patients with early stage lung cancer (Stage IA and IB) or an oligometastatic lung tumor received 4-fraction SRT between May 2009 and April 2010. Six patients were excluded from this study, as their protocol included 10 fractions of radiotherapy, thus requiring a shorter period of time of radiation. Since the pulmonary tumor was located adjacent to significant organs in these patients, the 10-fraction procedure was applied instead of the 4-fraction procedure.
A summary of the patients' characteristics is shown in Table 1. A total of 30 patients with lung tumors were treated with SRT with a total dose of 48–60 Gy and four treatment fractions. The patients' ages ranged from 59–86 years old (median age of 78). Of the 30, 27 patients had primary pulmonary tumors (Stage IA: T1N0, n = 19, Stage IB:T2N0, n = 8) and three patients had a single lung metastasis. Three patients were treated with both arms placed alongside the body trunk due to the difficulty in keeping their arms held up for various reasons. The remaining 27 patients' arms were held up throughout setup and treatment. Profiles, indication for therapy, and risk factors for these 30 patients were discussed by the tumor board of the hospital. An informed consent for radiation therapy was obtained from all the patients, who were either considered inoperable due to risk factors for thoracic surgery, or who had refused surgery and been advised to select SRT by medical oncologists.
Table 1.
Characteristics of the patients
| Total number of the patients |
30 | |
|---|---|---|
| Age | ||
| Median | 78 | |
| Range | 59–86 | |
| Gender | ||
| Male | 16 | |
| Female | 14 | |
| Tumor stage (primary NSCLC) | ||
| IA (T1N0) | 19 | |
| IB (T2N0) | 8 | |
| Position of the patient's arms | ||
| Up | 27 | |
| Down | 3 | |
Patient immobilization method
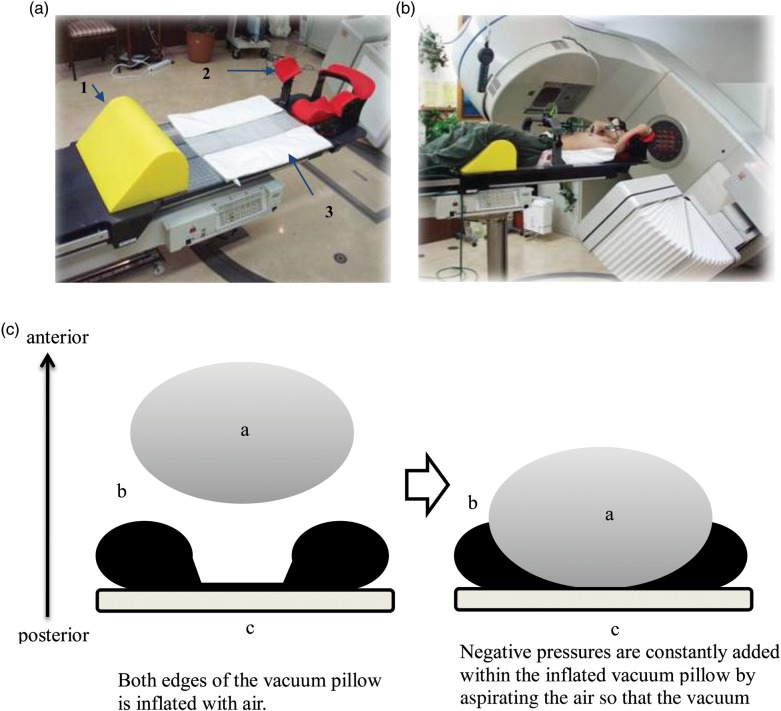
In order to control internal organ motion, an FDA-approved respiration-synchronizing device [3], was used in all cases. This device has two sensors (Fig. 1a), which are designed to be in contact with the chest and the abdomen during irradiation. The device was set up over the patient, as seen in Fig. 1b. Due to the nature of the device, any rigid patient fixation device that comes between the treatment coach and the radiation therapy unit was not used. As seen in Figs 1c and 2a, a non-invasive patient immobilization system is comprised of an arm holder (Posirest, Symmed bv, Amsterdam, Netherland), a leg rest (Round FOAM, Moriyama X-ray Equipments Co., Ltd, Tokyo, Japan), and a vacuum pillow (Engineering System, Co., Ltd, Matsumoto, Japan). The patient was placed supine (Figs 1d and 2b), typically with the arms being raised and the knees resting on the leg rest in a semiflexed position. The lateral/posterior portion of the upper trunk was supported by an inflated vacuum pillow, which offered sufficient support posterolaterally (Fig. 2c), but simultaneously allowed the patient to breathe naturally throughout the processes of setup and irradiation. No other device was used to immobilize the body of the patient.
Fig. 1.
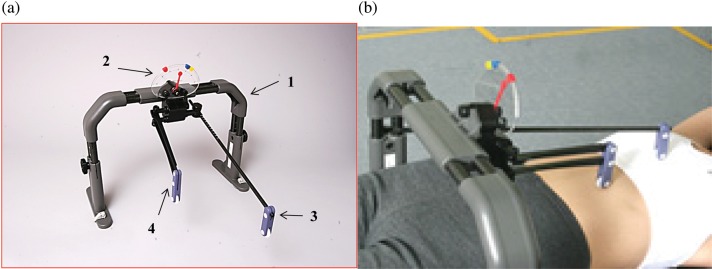
A respiration-synchronizing device. (a) A general view of the respiration-synchronizing device comprised of a respiratory level indicator panel (1) mounted on the main body (2). Vertical motion of the chest and abdomen associated with breathing is detected by thoracic (3) and abdominal (4) contacts. (b) View of the main body of the device in use on a patient. Two contacts are placed on the chest and abdomen of a patient lying in a supine position.
Fig. 2.
An axial view of the trunk, the treatment table, and the vacuum pillow, including the mounting of the respiration-synchronizing device (c). (a) The figure shows a non-invasive patient immobilization setup, which is comprised of an arm-holder (1) (Posirest, Symmed bv, Amsterdam, Netherland), a leg rest (2) (Round FOAM, Moriyama X-ray Equipments Co., Ltd, Tokyo, Japan), and a vacuum pillow (3) (Engineering System, Co., Ltd, Matsumoto, Japan). The vacuum pillow is designed to be inflated to support the lateral and posterior portion of the upper trunk. (b) The patient is placed supine with both arms raised and placed on the arm holder, and the knees on the leg rest in a semiflexed position. The lateral/posterior portion of the upper trunk was firmly attached to a vacuum pillow. This non-invasive immobilization system allows the patient to breathe comfortably on the coach without too much restraint. (c) Both side edges of the vacuum pillow are inflated by air (left). When the patient is placed in the supine position, negative pressures are constantly added within the pillow so that the vacuum pillow fits the posterolateral portion of the patient's chest, which offers sufficient support posterolaterally (right). a, b and c in the drawings indicate the patient chest, a vacuum pillow and a treatment table, respectively.
Instructions on breath-holding
Sufficient instructions were given to the patients in the preliminary practice sessions.
The patients were routinely instructed to maintain smooth and regular breathing before breath-holding, and not to use abdominal muscles to adjust the indicator. Applicability of the device was evaluated for each patient during preliminary practice sessions. If a patient deviated from these instructions, the patient was to be excluded from this treatment and provided with other treatments.
Treatment methods
The patients were treated using the radiation therapy unit, comprising a linear accelerator (linac) (EXL-15DP, Mitsubishi Electric, Tokyo, Japan) coupled to a CT scanner (Hi-Speed DX/I, GE Yokogawa Medical Systems, Tokyo, Japan).
The isocenter of the planning target volume (PTV) was visually adjusted with CT images of 2-mm thickness taken before every radiotherapy fraction to correspond to the planned isocenter with patient self-breath-hold using the CT scanner unified with the linac. The couch was rotated 180 degrees so that the rotational center of the CT-gantry corresponded to the isocenter of the linac. When alignment was obtained a signal indicating readiness to start irradiation was given by a radiation technologist.
Evaluation
The patients' electronic medical records and cross-sectional images were retrospectively analyzed. The pre- and post-radiation CT images at each session were reviewed following completion of the procedures by a radiologist who was not directly involved in the management of the patients. Among CT scan images taken immediately before irradiation with the patient on the CT-linac system, a slice from the pre-radiation CT images demonstrating the maximum tumor diameter was chosen. In the selected CT slice, a certain bony landmark in the thoracic vertebrae, which was easily identifiable and reproducible, was preferentially selected. The position of the bony landmark was recorded three-dimensionally, or on the x-, y-, and z-axes.
Immediately after radiation therapy, post-radiation CT images were taken while the patient was still on the couch of the CT-linac. The selected bony landmark on the post-radiation CT was manually identified by the observer. The position of the body landmark was recorded in the same way as the pre-radiation CT image.
An intrafractional setup error was defined as displacement of the distance (in mm) of the selected bony landmarks between pre- and post-CT images. The shift of the landmark position was recorded on the basis of Right/Left (R.L.), Posterior/Anterior (P.A.), and Inferior/Superior (I.S.) shift. Shifts to the left, anterior and superior directions were considered to be positive, while right-sided, posterior, and inferior shift were considered negative.
The observed intrafractional setup errors in each patient over four sessions were presented in a dot plot. Frequency of the intrafractional setup error values in all three directions was presented in a histogram. The means and one standard deviation of the intrafractional setup errors from all treatment fractions were calculated and presented as overall intrafractional setup errors, while those parameters of each patient were calculated and presented as individual overall intrafractional setup errors. The means and one standard deviation of the intrafractional setup errors in three directions in each session were compared and presented in a dot plot. Statistical analysis was performed using GraphPad Prism (GraphPad Software Inc. CA) and Microsoft Excel (Microsoft, WA).
RESULTS
All the 30 patients completed the treatment as planned with no interruptions. No patients were lost to follow-up evaluation. In 27 patients, CT images from four sessions were available, while records of the three sessions among the four full treatments were available in the remaining 3 patients. A total of 234 images were analyzed including 216 images of the 27 patients and 18 images of the remaining 3 patients.
The duration of each fraction of the lung SRT ranged from 21–58 min, with a mean of 36 ± 9 (SD).
A summary of the means and one standard deviation of the intrafractional errors (in mm) were 0.9 ± 0.7 (R.L.), 0.9 ± 0.7 (P.A.) and 0.5 ± 1.0 (I.S.) in general, as shown in Table 2. The mean value of the intrafractional setup errors in the I.S. direction was smaller, when compared with the R.L. and P.A. directions (P < 0.01). Population setup errors, systematic errors (Σ) and random errors (σ), in three directions were calculated and shown in Table 3.
Table 2.
Average intrafractional setup errors in inferior/superior (I.S.), right/left (R.L.) and posterior/anterior (P.A.) directions (mm)
Intrafractional error (mm) general
| Intrafractional error (mm) general | ||||
|---|---|---|---|---|
| Direction | Mean | SD | Min | Max |
| R.L. | 0.9 | 0.7 | 0.1 | 3.4 |
| P.A. | 0.9 | 0.7 | 0.1 | 3.5 |
| I.S. | 0.5 | 1.0 | 0.1 | 4.0 |
Table 3.
Population setup errors
| Direction | Systematic (Σ) | Random (σ) |
|---|---|---|
| R.L. | 0.4 | 0.7 |
| P.A. | 0.5 | 0.6 |
| I.S. | 0.6 | 0.9 |
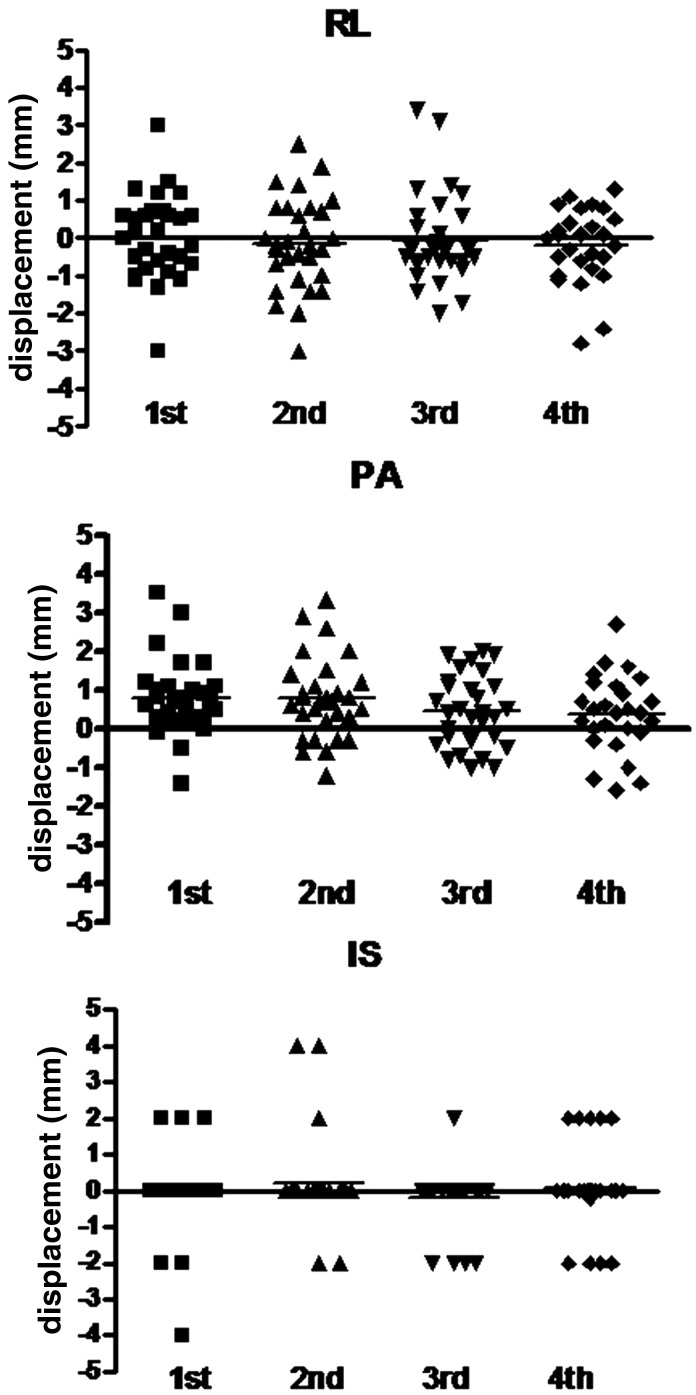
Intrafractional setup errors in all patients in the 1st, 2nd, 3rd and 4th sessions of the treatment are shown in Fig. 3. In each direction, no statistical significance was observed in the mean value of any two sessions (paired t-test).
Fig. 3.
Intrafractional setup errors (mm) in each session in all patients.
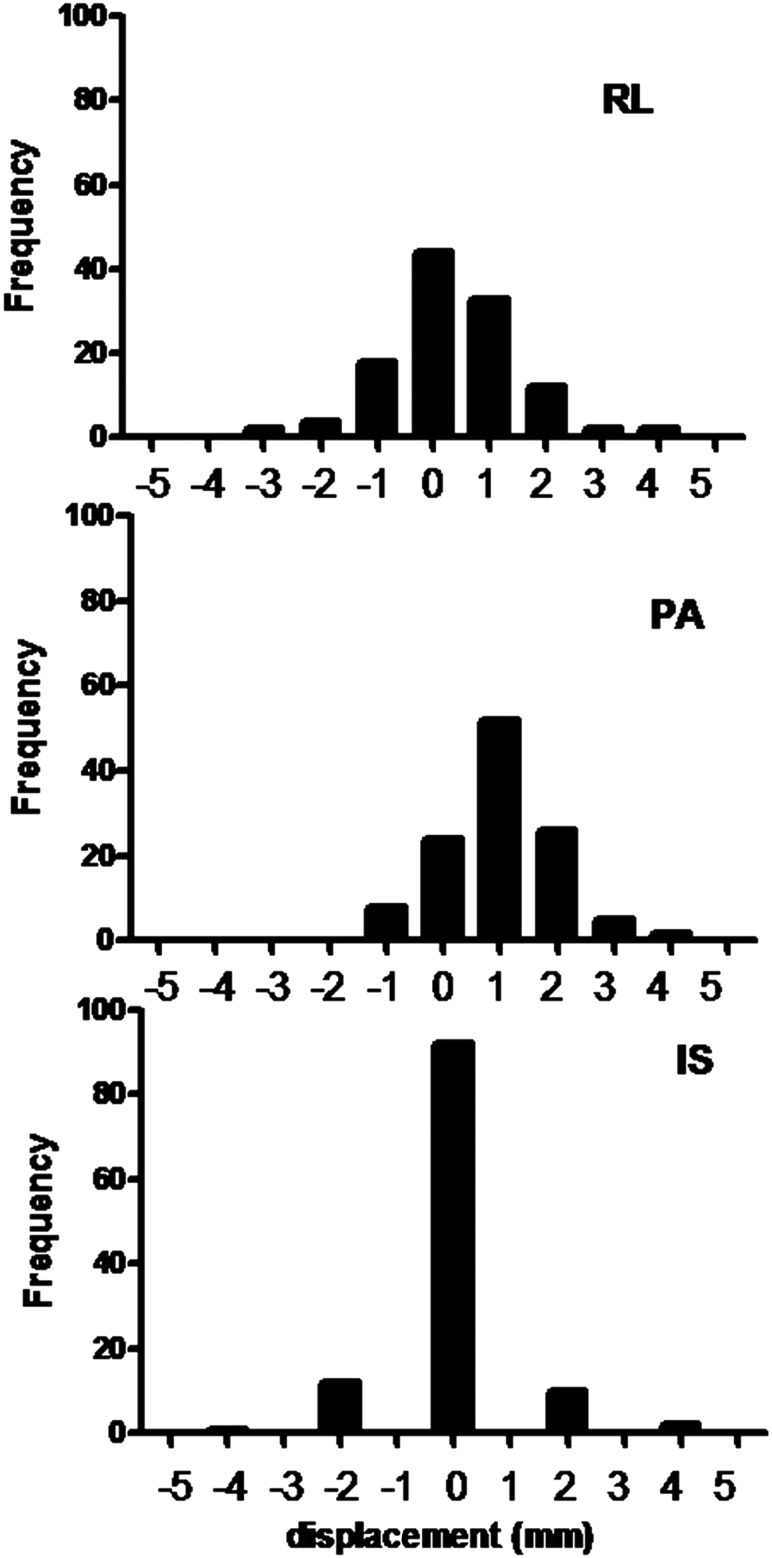
Histograms of the intrafractional setup errors observed in all three directions are shown in Fig. 4. The frequency within 3mm displacement was 98% in R.L., 98% in P.A. and 97% in I.S. directions.
Fig. 4.
Histograms of the intrafractional setup errors in all three directions.
DISCUSSION
SRT is a treatment option for lung cancer. It has been reported that the 5-year survival rates of lung SRT range approximately from 60–75% for Stage IA and 40–60% for Stage IB [10–12], which are potentially comparable to that of surgical resection [13]. In addition to the survival rates, lung SRT demonstrated very low incidence of treatment-related complications in the septuagenarian in our experience.
Since the introduction of a unit for radiotherapy using a common treatment couch for CT and linac [14, 15], interfractional setup errors have been minimized. We have been using an integrated CT-linac irradiation system which connects a CT scanner and a linac via a common treatment coach. The patient on the treatment couch was placed supine with a respiration-synchronizing device on the patient's chest and abdomen to control internal motion of the target [3]. In order to use the respiration-synchronizing device most effectively, non-invasive patient fixation with a comparably loose vacuum pillow is essential.
However, in this treatment system, a concern is raised about the intrafractional setup errors, which should be evaluated fully for the safety and reproducibility for precise targeting. Various fixation devices are used for lung SRT, such as a customized body pillow formed by vacuum suction, a fixation sheet, a stereotactic body frame [1], or a BodyLoc localizer, which uses rigid, firm and strict immobilization of the patient trunk. With a BodyLoc system, intrafractional shifts, the mean set-up errors and standard deviations were–0.1 ± 0.7 mm,–0.3 ± 2.0 mm, and 0.5 ±1.1 mm for the lateral, longitudinal and vertical shifts, respectively [2]. However, strict immobilization of the patient body can limit patient respiration due to the tightness of the device located around the chest during lung SRT. This may cause significant discomfort to patients with higher age and/or with poor pulmonary function. It is these patients who especially benefit from the use of non-invasive fixation of the chest.
In this report, intrafractional setup error was analyzed in the patients treated using a voluntary breath-hold technique, with non-invasive patient fixation on the linac-CT coach. None of the patients in this series complained of difficulty in breathing during the SRT. This non-invasive method benefited the patients with a limited pulmonary function. In addition, the benefits of applying non-invasive patient fixation include low cost and feasibility in management. The intrafractional setup errors observed in the patients in this series were ≤4 mm, which was less than the margin added to the PTV. Also, the frequency of the observed intrafractional setup errors being ≤3 mm was >97% in all three directions.
Hypofractionated SRT substantially requires a high radiation dose in one session of treatment. In order to deliver a high dose of irradiation, a period of one session becomes lengthy. In this study, the average treatment time was 36 minutes ±9 (SD), and ranged from 21–58 minutes. Approximately 60 minutes were taken in the preparation and the treatment for one fraction. Despite the longer period of irradiation, intrafractional setup errors during lung SRT with non-invasive patient fixation were ≤4mm in all three directions. Although the difference of the position between just before and just after the irradiation may not represent the maximum difference in all of the cases, the observed intrafractional setup errors in this study in all three directions were within the limit of the margin between the clinical target volume (CTV) and the PTV for lung SRT.
Intrafractional setup errors, including calculated values such as averages and standard deviations in all three dimensions, were analyzed in each session and compared with one another. Prior to the series of treatment, we initially had a hypothesis that the intrafractional setup errors should be altered as the sessions progressed and the patients became familiarized with the treatment system including the body fixation device and breath-holding technique. In fact, no statistically significant differences were seen between any two sessions in all three dimensions. It may be partially due to the fact that all the patients spent enough time in the planning session to be able to synchronize the radiation therapy and become well-familiarized with the positioning for radiotherapy before the first treatment, or that there were not enough patients to show statistically significant differences. At the same time, the results demonstrated that minimal intrafractional setup error was achieved even in the first session, and that this was maintained throughout the following sessions.
Our results suggest that non-invasive patient fixation using the immobilization system with vacuum pillow was appropriately administered for the patients to stay on the coach and breathe without feeling restricted. There are several possible reasons for the small intrafractional setup errors. One is that the patients in this study spent time in a practice session before the actual irradiation treatment. In the practice sessions, the patients obtained tips on how to breathe naturally and hold their breath in an unforced fashion. The assisting respiration-synchronizing device for breath-holding, and the patient immobilization system we employed in this study, required the patients to participate in the treatment voluntarily. This positive involvement in the treatment may have provided benefit to the patients in terms of giving them greater motivation, thus contributing to the achievement of minimal intrafractional setup errors. In any case, it is important that patients are voluntarily involved in the treatment and understand the importance of staying still on the linac-CT coach.
There were some limitations to this study. First, it was a retrospective study with a limited number of the patients. Second, we did not use an automatic imaging detection system to measure the setup error. In general, manually measured values can include observer bias. Finally, rotational errors were not measured in the study.
CONCLUSION
In conclusion, observed intrafractional setup errors during SRT using non-invasive patient fixation in the form of an immobilization system with a comparatively loose vacuum pillow were ≤ 4 mm, which was within the range of the setup margin added to the CTV in the general radiation planning. The lung SRT under this type of non-invasive patient fixation demonstrates satisfactory reproducibility with minimal intrafractional setup errors using voluntary breath-holding that fall within a small internal margin.
REFERENCES
- 1.Wang L, Jacob R, Chen L, et al. Stereotactic IMRT for prostate cancer: setup accuracy of a new stereotactic body localization system. J Appl Clin Med Phys. 2004;5:18–28. doi: 10.1120/jacmp.v5i2.1947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhou J, Uhl B, Dewitt K, et al. Image-guided stereotactic body radiotherapy for lung tumors using BodyLoc with tomotherapy: clinical implementation and set-up accuracy. Med Dosim. 2010;35:12–8. doi: 10.1016/j.meddos.2008.12.003. [DOI] [PubMed] [Google Scholar]
- 3.Onishi H, Kawakami H, Marino K, et al. A simple respiratory indicator for irradiation during voluntary breath holding: a one-touch device without electronic materials. Radiology. 2010;255:917–23. doi: 10.1148/radiol.10090890. [DOI] [PubMed] [Google Scholar]
- 4.Nagata Y, Hiraoka M, Mizowaki T, et al. Survey of stereotactic body radiation therapy in Japan by the Japan 3-D Conformal External Beam Radiotherapy Group. Int J Radiat Oncol Biol Phys. 2009;75:343–7. doi: 10.1016/j.ijrobp.2009.02.087. [DOI] [PubMed] [Google Scholar]
- 5.Hanley J, Debois MM, Mah D, et al. Deep inspiration breath-hold technique for lung tumors: the potential value of target immobilization and reduced lung density in dose escalation. Int J Radiat Oncol Biol Phys. 1999;45:603–11. doi: 10.1016/s0360-3016(99)00154-6. [DOI] [PubMed] [Google Scholar]
- 6.Wong JW, Sharpe MB, Jaffray DA, et al. The use of active breathing control (ABC) to reduce margin for breathing motion. Int J Radiat Oncol Biol Phys. 1999;44:911–9. doi: 10.1016/s0360-3016(99)00056-5. [DOI] [PubMed] [Google Scholar]
- 7.Garcia R, Oozeer R, Le Thanh H, et al. Radiotherapy of lung cancer: the inspiration breath hold with spirometric monitoring. Cancer Radiother. 2002;6:30–8. doi: 10.1016/s1278-3218(01)00132-9. [DOI] [PubMed] [Google Scholar]
- 8.Shen S, Duan J, Fiveash JB, et al. Validation of target volume and position in respiratory gated CT planning and treatment. Med Phys. 2003;30:3196–205. doi: 10.1118/1.1626121. [DOI] [PubMed] [Google Scholar]
- 9.Keall PJ, Joshi S, Vedam SS, et al. Four-dimensional radiotherapy planning for DMLC-based respiratory motion tracking. Med Phys. 2005;32:942–51. doi: 10.1118/1.1879152. [DOI] [PubMed] [Google Scholar]
- 10.Uematsu M, Shioda A, Suda A, et al. Computed tomography-guided frameless stereotactic radiotherapy for stage I non-small cell lung cancer: a 5-year experience. Int J Radiat Oncol Biol Phys. 2001;51:666–70. doi: 10.1016/s0360-3016(01)01703-5. [DOI] [PubMed] [Google Scholar]
- 11.Nagata Y, Takayama K, Matsuo Y, et al. Clinical outcomes of a phase I/II study of 48 Gy of stereotactic body radiotherapy in 4 fractions for primary lung cancer using a stereotactic body frame. Int J Radiat Oncol Biol Phys. 2005;63:1427–31. doi: 10.1016/j.ijrobp.2005.05.034. [DOI] [PubMed] [Google Scholar]
- 12.Onishi H, Araki T, Shirato H, et al. Stereotactic hypofractionated high-dose irradiation for stage I non-small cell lung carcinoma: clinical outcomes in 245 subjects in a Japanese multi-institutional study. Cancer. 2004;101:1623–31. doi: 10.1002/cncr.20539. [DOI] [PubMed] [Google Scholar]
- 13.Onishi H, Shirato H, Nagata Y, et al. Stereotactic body radiotherapy (SBRT) for operable stage I non-small-cell lung cancer: can SBRT be comparable to surgery? Int J Radiat Oncol Biol Phys. 2011;81:1352–8. doi: 10.1016/j.ijrobp.2009.07.1751. [DOI] [PubMed] [Google Scholar]
- 14.Uematsu M, Shioda A, Tahara K, et al. Focal, high dose, and fractionated modified stereotactic radiation therapy for lung carcinoma patients: a preliminary experience. Cancer. 1998;82:1062–70. doi: 10.1002/(sici)1097-0142(19980315)82:6<1062::aid-cncr8>3.0.co;2-g. [DOI] [PubMed] [Google Scholar]
- 15.Kuriyama K, Onishi H, Sano N, et al. A new irradiation unit constructed of self-moving gantry-CT and linac. Int J Radiat Oncol Biol Phys. 2003;55:428–35. doi: 10.1016/s0360-3016(02)03987-1. [DOI] [PubMed] [Google Scholar]