Abstract
Marburg virus (MARV) and Ebola virus, members of the family Filoviridae, cause lethal haemorrhagic fever in humans and non-human primates. Although the outbreaks are concentrated mainly in Central Africa, these viruses are potential agents of imported infectious diseases and bioterrorism in non-African countries. Recent studies demonstrated that non-human primates passively immunized with virus-specific antibodies were successfully protected against fatal filovirus infection, highlighting the important role of antibodies in protective immunity for this disease. However, the mechanisms underlying potential evasion from antibody mediated immune pressure are not well understood. To analyse possible mutations involved in immune evasion in the MARV envelope glycoprotein (GP) which is the major target of protective antibodies, we selected escape mutants of recombinant vesicular stomatitis virus (rVSV) expressing MARV GP (rVSVΔG/MARVGP) by using two GP-specific mAbs, AGP127-8 and MGP72-17, which have been previously shown to inhibit MARV budding. Interestingly, several rVSVΔG/MARVGP variants escaping from the mAb pressure-acquired amino acid substitutions in the furin-cleavage site rather than in the mAb-specific epitopes, suggesting that these epitopes are recessed, not exposed on the uncleaved GP molecule, and therefore inaccessible to the mAbs. More surprisingly, some variants escaping mAb MGP72-17 lacked a large proportion of the mucin-like region of GP, indicating that these mutants efficiently escaped the selective pressure by deleting the mucin-like region including the mAb-specific epitope. Our data demonstrate that MARV GP possesses the potential to evade antibody mediated immune pressure due to extraordinary structural flexibility and variability.
Introduction
Marburg virus (MARV), like the closely related Ebola virus (EBOV), belongs to the family Filoviridae, a family of viruses that have non-segmented, negative-sense, ssRNA. These viruses can cause severe haemorrhagic fever in humans and non-human primates (Sanchez et al., 2007). Eight sporadic outbreaks of Marburg haemorrhagic fever have been reported, mainly in Central Africa (Nakayama & Takada, 2011), with the largest outbreak in Angola in 2004 to 2005 in which 329 fatalities were reported from 374 confirmed cases (case fatality rate 88 %). While MARV circulation among Egyptian fruit bats (Rousettus aegyptiacus) was recently suggested (Amman et al., 2012; Towner et al., 2009), the transmission routes to humans and non-human primates and the mechanisms underlying MARV perpetuation in nature are largely unknown. Therefore, MARV is one of the major pathogens posing a significant public health threat for imported infectious disease and bioterrorism.
Today, neither an approved prophylaxis nor a treatment is available for filovirus diseases. Recently, however, it was shown that passive immunization with virus-specific antibodies protected non-human primates from fatal filovirus infection (Dye et al., 2012; Marzi et al., 2012; Olinger et al., 2012; Qiu et al., 2012), highlighting the pivotal role of antibodies in protective immunity. The only target of the protective antibodies is likely to be the MARV glycoprotein (GP), since GP is the only viral protein on the virion surface and is therefore the primary mediator of viral entry into host cells. Although MARV entry is not fully understood, it is most likely to be triggered by attachment to its cell surface receptor(s), followed by uptake via endocytosis, which finally results in fusion between the viral envelope and the endosomal membrane (Takada et al., 1997; Wool-Lewis & Bates, 1998). Due to its essential functions, GP is thought to be the key factor in MARV growth, cell tropism, host range and pathogenicity.
Before its assembly into progeny virions, the precursor GP is post-translationally modified in the host cells. While trafficking through the trans-Golgi network, immature GP is proteolytically cleaved into two subunits, GP1 and GP2, by the ubiquitous host proprotein convertase furin (Volchkov et al., 2000). The subunits GP1 and GP2 are covalently linked via a disulphide bond, and three GP1/GP2 heterodimers form a chalice-like trimetric structure (Lee et al., 2008). The canonical furin-recognition sequence (Arg-X-Lys/Arg-Arg in which X is any amino acid) is highly conserved among GPs of all known MARV and EBOV with the exception of Reston virus, whose GP possesses a suboptimal furin-recognition motif (Arg-Lys-Gln-Lys-Arg). Interestingly, this motif is also present in the GP of Lloviu virus, a putative novel member of the family Filoviridae, whose genome was detected in carcasses of insectivorous bats (Miniopterus schreibersii) in roosting caves in Europe (Negredo et al., 2011). Although the high conservation of the furin-recognition motif among filoviruses implies some biological significance for GP cleavage, studies employing reverse genetics have demonstrated that the cleavage is not essential for virus replication in vitro and pathogenicity in non-human primates (Ito et al., 2001; Neumann et al., 2002, 2007; Wool-Lewis & Bates, 1999).
It is also well documented that filovirus GPs are extensively modified with both N- and O-linked glycans during transport through the endoplasmic reticulum and Golgi apparatus (Feldmann et al., 1991, 1994). Most of the O-linked glycans are concentrated in the middle one-third of GP (amino acid positions 289–501), the region that is highly divergent among filovirus GPs and designated the mucin-like region. The mucin-like region is predicted spatially to cover a huge portion of the mature trimeric GP molecule (Lee et al., 2008). It is therefore believed that the mucin-like region masks the putative receptor-binding sites from neutralizing antibodies by steric shielding of the antibody-specific epitopes (Brindley et al., 2007; Dube et al., 2009; Francica et al., 2010; Kuhn et al., 2006; Lee & Saphire, 2009; Lee et al., 2008; Manicassamy et al., 2005; Reynard et al., 2009). The mucin-like region also plays an important role in virion attachment to the preferred target cells (e.g. hepatocytes, endothelial cells, dendritic cells and macrophages), which express a wide array of lectins and are probably involved in filovirus pathogenesis (Matsuno et al., 2010; Simmons et al., 2002; Takada et al., 2004). Interestingly, passive transfer of anti-EBOV GP mAb 12B5-1-1, which recognizes an epitope in the mucin-like region, is protective in a mouse model of lethal EBOV infection (Wilson et al., 2000).
While information regarding the protective role of anti-filovirus antibodies is gradually being accumulated, the possible mechanisms underlying evasion from antibody mediated inhibition of viral infectivity are not well understood. We previously demonstrated that MARV GP-specific mAbs AGP127-8 (IgG1) and MGP72-17 (IgM), which do not inhibit GP-mediated entry of MARV into host cells, have the ability to drastically reduce budding and release of progeny viruses from MARV-infected cells (Kajihara et al., 2012). In this study, we utilized a recombinant vesicular stomatitis virus (rVSV) whose surface glycoprotein gene was replaced with the MARV GP gene (rVSVΔG/MARVGP) to obtain escape variants from immune selection with the MARV GP-specific mAbs AGP127-8 and MGP72-17 (Schnell et al., 1996; Takada et al., 2003). Sequence data revealed that the GPs of some of these escape variants had an altered furin-recognition motif resulting from point mutations, although the mAbs do not recognize epitopes within this motif. More surprisingly, the mucin-like region containing the epitope of mAb MGP72-17 was largely lacking in the GP of some variants that escaped immune selection. Here, we report novel mechanisms by which MARV evades antibody mediated immune pressure.
Results
Inhibitory effect of mAbs AGP127-8 and MGP72-17 on plaque formation of rVSVΔG/MARVGP
Two clones of MARV GP-specific mAbs, AGP127-8 and MGP72-17, were used in this study (Kajihara et al., 2012; Nakayama et al., 2011). Previously, we reported that mAbs AGP127-8 and MGP72-17 had the potential to inhibit budding of MARV from infected cells (Kajihara et al., 2012). In this study, we first evaluated the ability of these mAbs to suppress plaque formation of rVSVΔG/MARVGP on Vero E6 cells. We found that the size of plaques formed in the presence of mAb AGP127-8 or MGP72-17 was significantly reduced compared with treatment with an irrelevant control antibody, APH159-1-3, or without any antibody, although the virus could still form tiny plaques that were barely visible on stained cells (Fig. 1a, b). Neither mAb decreased the number of plaques (Fig. 1c), a finding in line with the previous observation that MARV GP-mediated entry into cells is not impaired by these mAbs (Kajihara et al., 2012). Taken together, these data suggest that the plaque size of rVSVΔG/MARVGP was reduced by the inhibitory effect of mAbs AGP127-8 and MGP72-17 on virus budding.
Fig. 1.
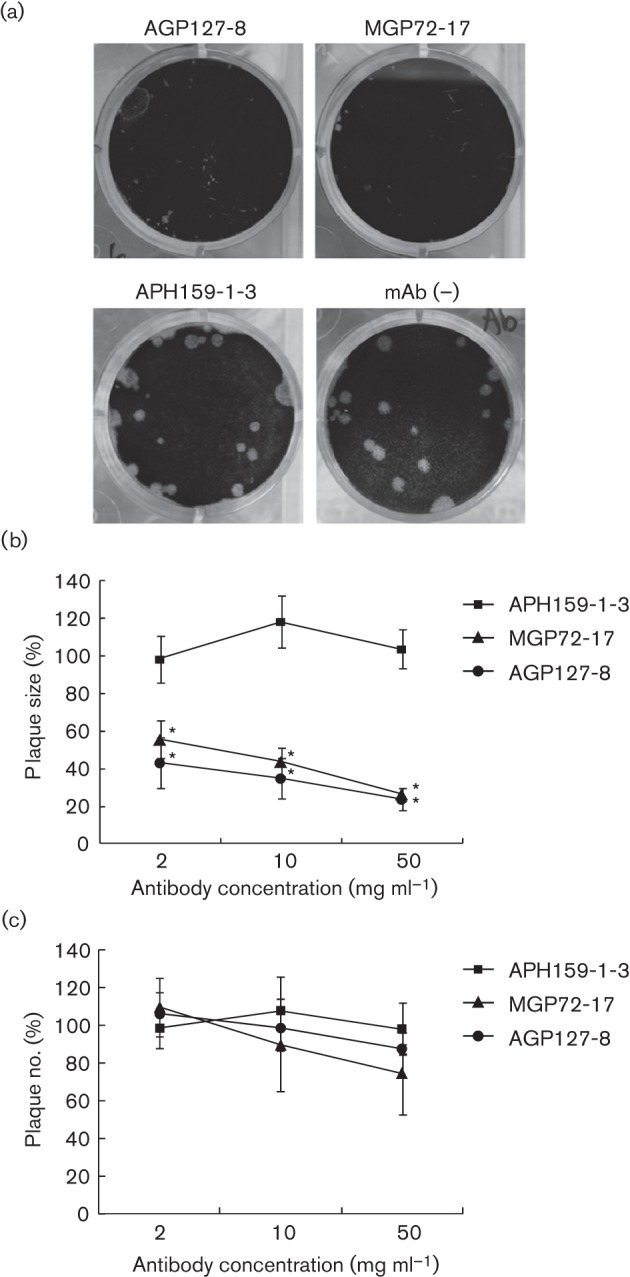
Inhibition of rVSVΔG/MARVGP plaque formation by MARV GP-specific mAbs. rVSVΔG/MARVGP was inoculated onto confluent Vero E6 cells and incubated at 37 °C for 2 days with 1.0 % agarose in maintenance medium in the presence (2, 10 or 50 µg ml−1) or absence of each mAb. Cells were stained with crystal violet. mAbs AGP127-8 and MGP72-17 are MARV GP specific. mAb APH159-1-3 was used as an irrelevant negative control. (a) Plaque formation of rVSVΔG/MARVGP in the presence (50 µg ml−1) or absence of mAbs. The size (b) and number (c) of rVSVΔG/MARVGP plaques are shown relative to the size and number of plaques in the absence of mAbs. This assay was performed at least three times; mean values and sd are shown. Data were statistically analysed by Student’s paired t-test and asterisks represent significant differences. *, P<0.001 for the difference of the plaque size in the presence of MARV GP-specific mAbs or control APH159-1-3.
Cloning of mutant rVSVΔG/MARVGP that escapes from mAbs AGP127-8 and MGP72-17 selective pressure
In the present study, we utilized rVSVΔG/MARVGP to select escape mutants of mAbs AGP127-8 and MGP72-17. Previously, chimeric rVSV expressing EBOV GP was used to identify the epitopes of neutralizing EBOV GP-specific mAbs by sequencing the EBOV GP genes of cloned escape variants (Takada et al., 2003). The study demonstrated that rVSV was a useful tool for the selection of GP antigenic variants, since rVSV replicates more rapidly in cultured cells than wild-type (WT) MARV and the RNA polymerase of VSV has a high mutation rate (Holland et al., 1990). These properties of rVSVΔG/MARVGP led us to expect that escape mutants would be efficiently rescued in the presence of mAbs. Serial passaging and plaque purification in the presence of these mAbs allowed us to obtain multiple escape variants. These mutants could form large plaques even in the presence of mAb AGP127-8 or MGP72-17, and the plaques were comparable in size to those formed in the absence of the mAbs (data not shown).
Mutations found in the GPs of escape rVSVΔG/MARVGP mutants
Sequence analyses of the escape mutants revealed that rVSVΔG/MARVGP acquired mutations at several different positions in the MARV GP sequence to evade the selective pressure of mAbs AGP127-8 and MGP72-17 (Fig. 2). The control virus cultured similarly in the absence of antibodies had no mutations in its GP compared with the parent strain (data not shown), indicating that acquired mutations in the presence of mAbs AGP127-8 and MGP72-17 were not the result of propagation in Vero E6 cells. A variant selected with mAb AGP127-8 (A127 variant #5) acquired three amino acid substitutions: Val at position 407, Leu at position 428 and Val at position 429 were replaced with Ala, Pro and Ala, respectively (Fig. 2b). Another mutant selected with mAb MGP72-17 (M72 variant #2) acquired a single amino acid substitution: Tyr at position 430 was replaced with Asp (Fig. 2b). Interestingly, AGP127-8 variants #1 and #4 had a single amino acid substitution at the furin-recognition motif (432Arg-Arg-Lys-Arg435): Lys at position 434 mutated to Asn, and Arg at position 435 mutated to Gln, respectively (Fig. 2b). M72 variants #1 and #6 also acquired a single amino acid substitution at the furin-recognition motif (Fig. 2b): Args at position 435 and 432 were changed to Gln and Gly, respectively. It is well established that the furin cleaves proteins just downstream of its recognition sequence Arg-X-Lys/Arg-Arg, suggesting that MARV GP variants that acquired the point mutation in this motif had decreased furin-cleavability. Another interesting finding was that two rVSVΔG/MARVGP variants which escaped from mAb MGP72-17 selective pressure had extensive deletion in their GPs (Fig. 2c). M72 variant #7 had deletion of amino acids 341–429 in the mucin-like region in the GP1 subunit: M72 variant #11 lacked amino acids 256–433, which is more than 25 % of GP, and notably the mucin-like region in GP1 was totally eliminated. Finally, we confirmed by ELISA that all the obtained MARV GP mutants showed a remarkable reduction in binding ability to the respective selection mAbs while there was no significant difference in overall expression levels between the mutant and parental GPs (Fig. 3).
Fig. 2.

(a) A schematic diagram of parental MARV GP. SP, Signal peptide; RBR, putative receptor-binding region; MLR, mucin-like region; FP, fusion peptide; TM, transmembrane domain. The furin-cleavage site and a disulphide bond between the GP1 and GP2 subunits are indicated by the arrow and line, respectively. (b) Point mutations found in the MARV GPs of escape variants selected by mAb AGP127-8 or MGP72-17. The substituted amino acid residues and furin-recognition motif are shown in boldface and underlined, respectively. The putative epitopes of mAbs AGP127-8 and MGP72-17 (details in Fig. 4) are shown in the box. (c) The deletions found in the MARV GPs of escape variants selected by mAb MGP72-17. Deleted regions are highlighted with lines. The mucin-like region is shown in grey.
Fig. 3.
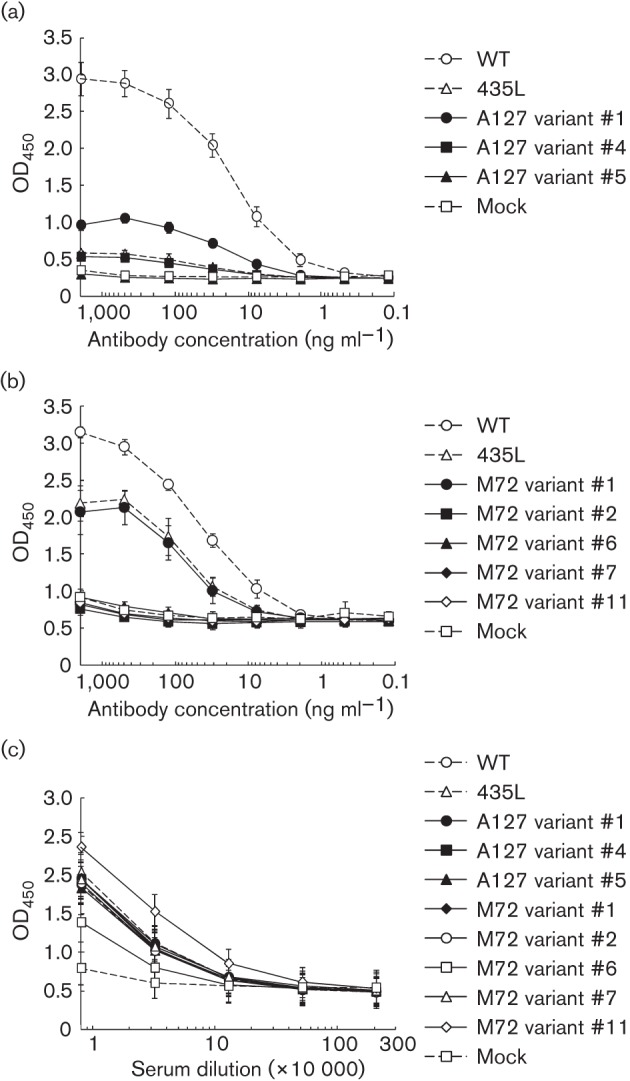
Binding activity of mAbs AGP127-8 and MGP72-17 and anti-MARV GP rabbit serum to WT and mutant MARV GPs in ELISA. Serially fourfold diluted mAbs AGP127-8 (a) and MGP72-17 (b) and anti-MARV GP rabbit serum (FS0505) (c) were examined for their binding activities to HEK293T cells expressing WT or variant MARV GPs. Cells transfected with the vector only (pCAGGS) were used as the mock control antigen. Rabbit serum FS0505 was used to examine the expression levels of GPs because it recognizes the epitope (aa residues 67–81 of MARV GP) separately from the region where the mutations were found in the GP of escape variants. Experiments were performed three (a and b) or two (c) times; mean values and sd are shown.
Identification of the epitopes of mAbs AGP127-8 and MGP72-17
The mutations found in the MARV GP variants selected with mAb AGP127-8 or MGP72-17 were concentrated in the C-terminal region of GP1, as shown in Fig. 2. To identify the specific epitopes of mAbs AGP127-8 and MGP72-17, the reactivities of both mAbs to synthetic peptides derived from MARV GP (amino acid positions 401–420, 411–430 and 421–435) were tested. We found that both mAbs bound strongly to a peptide corresponding to amino acids 411–430, but not to any of the other peptides tested, despite the ten overlapping amino acids between each of the peptides (Fig. 4). Finally, we confirmed by immunostaining that mAbs AGP127-8 and MGP72-17 did not bind to recombinant MARV GP whose amino acids 410–430 were artificially deleted (data not shown). The data indicated that the specific, linear epitope of each mAb was located between aa 411 and 430, and that the furin-cleavage motif itself was not essential for epitope conformation.
Fig. 4.
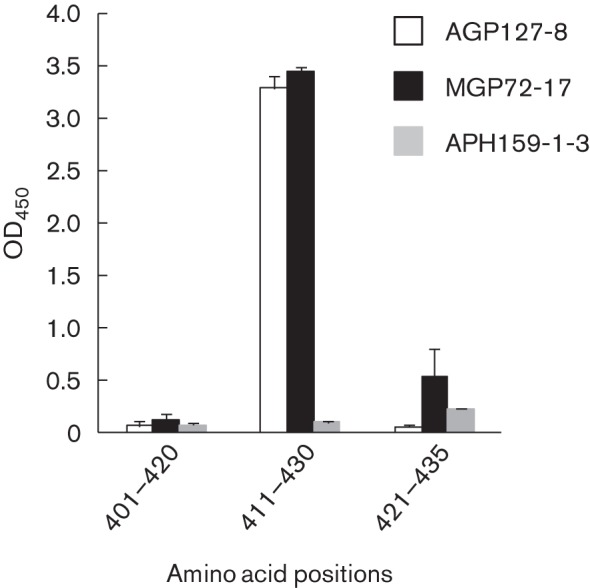
Identification of the AGP127-8 and MGP72-17 epitopes on MARV GP. The reactivities of mAbs AGP127-8 and MGP72-17 (2 µg ml−1) to synthetic peptides corresponding to aa positions 401–420, 411–430 and 421–435 of the MARV GP were analysed by ELISA. The experiment was performed three times; mean values and sd are shown.
Reduced cleavability of MARV GPs with mutations in the furin-cleavage motif
To determine the cleavability of the mutant GPs that possessed point mutation(s) found in or near the furin-recognition motif, Marburg virus-like particles (VLPs) consisting of the viral major matrix protein VP40 and the WT or mutant GP were subjected to Western blotting, and the relative band intensities between uncleaved GPs and GP2 subunits were compared (Fig. 5). These VLPs containing WT or variant GPs were indeed similarly produced from transfected cells (data not shown), suggesting that cell surface expression levels of these GPs and their incorporation into VLPs were not significantly affected by the mutations. We found that MARV GP2, but not uncleaved MARV GP, was detected in WT GP, indicating that WT GP was completely cleaved by host proteases including furin (Fig. 5), a finding in line with previously published data (Volchkov et al., 2000). A127 variant #5, which acquired point mutations at three positions outside the furin-recognition motif, was also completely processed into the GP1 and GP2 subunits (Fig. 5). In contrast, substantial amounts of uncleaved GP were detected in mutant GPs (A127 variant #4 and M72 variant #1) that acquired a point mutation at amino acid position 435 (Arg to Gln) and, accordingly, reduced amounts of GP2 were detected (Fig. 5). Similarly, uncleaved GP was detected on VLPs bearing GP of A127 variant #1 and M72 variant #6, which had point mutations in the furin-recognition motif at positions 434 and 431, respectively, indicating decreased proteolytic processing of these variant GPs. Although the mutation found in the GP of M72 variant #2 was not located in the furin-recognition motif, only a faint band of uncleaved GP was detected, suggesting that the mutation at position 430 might influence furin cleavage. Since the cleavage efficiency of mutant MARV GPs correlated directly with binding activity to mAbs AGP127-8 and MGP72-17 (Figs 3 and 5), point mutations in the furin-recognition motif probably recessed the epitopes in the uncleaved GP molecule and contributed to rVSVΔG/MARVGP escape from antibody selective pressure.
Fig. 5.
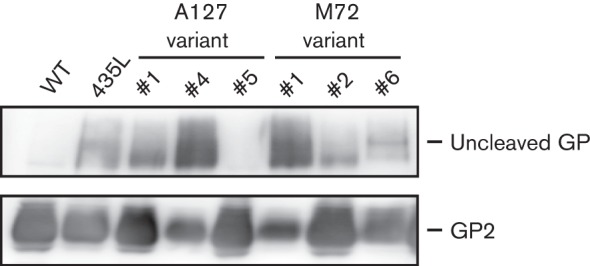
Proteolytic cleavability of WT and mutant MARV GPs. HEK293T cells were co-transfected with pCAGGS expressing MARV GP and VP40. Produced VLPs bearing WT or mutant MARV GPs were analysed by 7.5 % SDS-PAGE, followed by Western blotting. The uncleaved GP and the GP2 subunit were detected using mAb MGP14-22 that recognizes the epitope located in the GP2 subunit. The experiment was performed three times; a representative dataset is shown.
Discussion
In general, viruses possess the ability to escape antibody mediated neutralization (Hangartner et al., 2006). Substitutions at amino acid residues directly involved in contact with neutralizing antibodies often result in the loss of antibody recognition, which is a common mechanism by which viruses escape antibody mediated neutralization. However, alternative mechanisms to escape antibody recognition were reported for hepatitis C virus, where amino acid substitutions located outside the antibody-specific epitope in the surface glycoprotein altered receptor usage (Fofana et al., 2012). Another example is provided by human respiratory syncytial virus: the antibody specific epitope is destroyed by deletion of a nucleotide from the viral genome, resulting in a frameshift of the protein sequence in the glycoprotein C-terminal region eliminating the epitope (García-Barreno et al., 1990).
In this study, we investigated other mechanisms for viral evasion from antibody mediated immune pressure. We found that some of the rVSVΔG/MARVGP variants selected in the presence of mAbs AGP127-8 and MGP72-17 (A127 variants #1 and #4 and M72 variants #1 and #6) acquired a point mutation that altered the optimal furin-recognition motif at the C terminus of GP1. However, the furin-recognition motif itself is unlikely to serve as the antibody-specific epitope sequence for both mAbs (Figs 2 and 4). The antibody-specific epitopes were indeed identified near the C terminus of GP1, adjacent to the furin-recognition motif, but no amino acid substitutions were found in this epitope sequence of these escape variants. Our findings lead to the hypothesis that the mutant MARV GPs are not efficiently cleaved by furin and therefore the mAb-specific epitope is not exposed on the surface of the uncleaved GP molecule (Fig. 5). Subsequently, mAbs AGP127-8 and MGP72-17 are unable to access their specific epitopes, although the epitope sequence itself remains intact (Fig. 3). Further supporting our hypothesis is the finding that the binding activity of both mAbs to the mutant GPs correlated positively with the cleavage efficacy of these GPs (Figs 3 and 5). Notably, proteolytic processing of GP by furin is dispensable for EBOV replication in vitro and in vivo (Ito et al., 2001; Neumann et al., 2002, 2007; Wool-Lewis & Bates, 1999). It was also suggested that furin cleavage is not essential for the fundamental function of MARV GP (i.e. mediating virus entry and incorporation into virions in vitro) (Matsuno et al., 2010). Therefore, it may be possible that MARV can lose the optimal furin-recognition motif in GP without changing their biological phenotype, at least in non-human primate hosts. However, since cleaved form GP molecules were detected to some extent despite the dramatic loss of binding ability to the mAbs (Figs 3 and 5), alternative or additional mechanisms of virus escape from mAb pressure may also be considered, e.g. that the point mutation in the motif may affect the epitope conformation by changing electric charge or glycosylation pattern around the epitopes. Different electric mobilities among GP variants in Fig. 5 may be explained by assuming that a point mutation in the furin-cleavage motif influences glycosylation.
Interestingly, some of the MARV GP variants selected with mAb MGP72-17 acquired a more severe mutation, a complete or partial deletion of the mucin-like region in GP1 including the MGP72-17-specific epitope (Figs 2c and 4). The mechanism underlying the deletion of the mucin-like region in MARV GP is unclear. However, it was reported that parts of the spike protein of mouse hepatitis virus were deleted during persistent infection in the central nervous system (Rowe et al., 1997a); these deletions were frequently observed in regions where the RNA was predicted to form a stem–loop secondary structure (Rowe et al., 1997b). Therefore, it is possible that such secondary structures in RNA are required for the deletion of the mucin-like region in MARV GP under antibody mediated immune pressure. Similarly to the furin-recognition motif, it has also been shown that the mucin-like region is not essential for the MARV GP function to mediate cellular entry in vitro (Matsuno et al., 2010; Simmons et al., 2002; Takada et al., 2004). Our data also support the idea that the mucin-like region is dispensable for virus replication in vitro. However, it still needs to be clarified by using a reverse genetics approach whether the deletion of the mucin-like region changes the filovirus phenotype, both in vitro and in vivo.
While the direct inhibition of GP attachment to cell surface or endosomal receptor(s) and blocking fusion of the virus and host cell membranes are likely to be key mechanisms of classical neutralization of filovirus infectivity (Lee & Saphire, 2009; Shedlock et al., 2010; Takada et al., 2003), we have previously shown that non-neutralizing mAbs such as AGP127-8 and MGP72-17 inhibit MARV budding (Kajihara et al., 2012). Accordingly, amino acid substitutions found in the escape EBOV GP selected with anti-EBOV neutralizing mAbs were completely different from those identified in this study (Takada et al., 2003). Although the mechanisms of MARV budding inhibition by mAbs AGP127-8 and MGP72-17 are not fully understood, our data show that non-neutralizing antibodies may also serve as factors driving MARV evolution.
Taken together, the findings in the present study suggest that MARV GP has extraordinary flexibility and variability to evade antibody mediated immune pressure. Although recent studies have demonstrated that antibody therapy is a promising approach for the treatment of filovirus infections (Dye et al., 2012; Marzi et al., 2012; Olinger et al., 2012; Qiu et al., 2012), the emergence of escape mutants has not been fully discussed. Further information on the mechanisms underlying antibody mediated inhibition of MARV infectivity and evasion from antibody recognition will provide important information for the development of prophylactic and/or therapeutic countermeasures utilizing antibodies with higher protective efficacy and reduced risk of generating escape variants.
Methods
Viruses and cells.
rVSVΔG/MARVGP, recombinant replication-competent chimeric VSV whose glycoprotein gene was replaced with MARV (strain Angola) GP, was generated as described previously (Takada et al., 2003). All infectious work with rVSVΔG/MARVGP was performed at the Integrated Research Facility in the Rocky Mountain Laboratories, Division of Intramural Research, National Institute of Allergy and Infectious Diseases, National Institutes of Health, Hamilton, Montana, USA. Vero E6 and human embryonic kidney 293T (HEK293T) cells were grown in Dulbecco’s modified Eagle’s medium. Mouse myeloma P3-U1 cells and hybridoma cell lines were maintained in Roswell Park Memorial Institute 1640 medium. The media were supplemented with FCS and antibiotics.
mAbs.
MARV GP-specific murine mAbs AGP127-8 (IgG1), MGP14-22 (IgG1) and MGP72-17 (IgM) were generated as described previously (Kajihara et al., 2012; Nakayama et al., 2011). Protein A agarose columns (Bio-Rad) and KAPTIVE-M (Tecnogen) were used to purify the IgG1 (AGP127-8 and MGP14-22) and IgM mAbs (MGP72-17), respectively, from mouse ascites. mAb APH159-1-3 (murine IgM) specific to influenza A virus haemagglutinin, was used as an irrelevant control antibody. Animal studies were carried out in strict accordance with the Guidelines for Proper Conduct of Animal Experiments of the Science Council of Japan. The animal protocol was approved by the Hokkaido University Animal Care and Use Committee.
Plaque assay using rVSVΔG/MARVGP.
Conventional plaque assays were performed as described previously (Takada et al., 2003). Briefly, confluent Vero E6 cells infected with rVSVΔG/MARVGP mixed with or without a mAb were incubated at 37 °C for 2 days with 1.0 % agarose in maintenance medium in the presence (2, 10 or 50 µg ml−1) or absence of mAbs. The cells were stained with crystal violet and then the number and size of rVSVΔG/MARVGP plaques were determined. The relative plaque number and size were calculated by comparison with those in the absence of the mAb to 100.
Selection of escape mutants.
Tenfold serial dilutions of rVSVΔG/MARVGP were inoculated into Vero E6 cells and cultured with mouse ascites (1 : 100–1 : 200 dilutions). Mutant viruses growing in the presence of the mAbs were harvested from the highest dilution of the virus. This procedure was repeated and the growth of the virus in the presence of the antibodies was confirmed. Finally, escape variants were cloned through plaque purification in the presence of mAbs. Viral RNAs were extracted and the nucleotide sequences of the GP genes were determined using standard procedures. cDNAs of WT and mutant MARV GPs were cloned into the mammalian expression plasmid pCAGGS as described elsewhere (Matsuno et al., 2010). The mutation at aa 435, Arg to Leu, which was reported to hinder the proteolytic cleavage of GP (Volchkov et al., 2000), was introduced into the WT GP gene by site-directed mutagenesis with the QuikChange Site-Directed Mutagenesis kit (Stratagene).
ELISA.
The binding activities of mAbs AGP127-8 and MGP72-17 to MARV GPs were tested using HEK293T cells grown on 96-well plates and transfected with pCAGGS expressing WT or mutant GPs. Following 48 h incubation at 37 °C, cells were fixed with 4 % paraformaldehyde and permeabilized with 1 % Triton X-100. For identification of mAb epitopes, 96-well plates were coated with synthetic peptides (1.25 µg per well) corresponding to aa 401–420 (SPTTTVPNTTNKYSTSPSPT), 411–430 (NKYSTSPSPTPNSTAQHLVY) and 421–435 (PNSTAQHLVYFRRKR) of MARV GP, strain Angola. Non-specific binding of the antibodies was avoided by blocking with PBS containing 1 % BSA fraction V (Roche). After several washes, 50 µl of mAbs AGP127-8, MGP72-17 and APH159-1-3 at the indicated concentration was added to each well and incubated for 1 h at room temperature. After washing, the IgG and IgM mAbs bound to antigens were detected using goat anti-mouse IgG (Jackson ImmunoResearch) and anti-mouse IgM (KPL)-conjugated HRP, respectively. After incubation for 1 h at room temperature and four washes, 50 µl of 3,3′,5,5′-tetramethylbenzidine (Sigma) was added and the mixture was incubated for 15 min at room temperature. The reaction was stopped by adding 1 N sulphuric acid and the optical density (OD) at 450 nm was measured. Similar expression levels of each mutant GP were confirmed with anti-MARV GP rabbit serum FS0505 produced by immunization with a synthetic peptide corresponding to aa 67–81 (SKRWAFRTGVPPKNV) of MARV Gp, cross-reactive for all mutant MARV GPs.
SDS-PAGE and Western blotting.
HEK293T cells were co-transfected with pCAGGS expression plasmids encoding the WT or mutant MARV GP gene and major matrix protein VP40 gene. At 48 h post-transfection, the supernatants were collected and cleared from cell debris. VLPs consisting of MARV GP and VP40 in the supernatant were concentrated by performing ultracentrifugation through a 25 % sucrose cushion. The harvested VLPs were then analysed by 7.5 % SDS-PAGE and subsequent Western blotting, as described previously (Kajihara et al., 2012). Briefly, VLPs were mixed with SDS-PAGE sample buffer with 5 % 2-mercaptoethanol for detection of cleaved or uncleaved GPs and heated for 5 min at 98 °C. After electrophoresis, the separated proteins were blotted on a polyvinylidene difluoride membrane (Millipore). mAb MGP14-22 recognizing an epitope located in GP2 was used as the primary antibody to detect both the uncleaved GP and the GP2 subunit. The bound antibody was detected with peroxidase-conjugated goat anti-mouse IgG, followed by visualization with Immobilon Western (Millipore).
Acknowledgements
We thank Hiroko Miyamoto and Ayaka Yokoyama (Hokkaido University Research Center for Zoonosis Control), and Dr Hideki Ebihara (National Institute of Allergy and Infectious Diseases, National Institutes of Health, Rocky Mountain Laboratories) for technical assistance and valuable advice, and Kim Barrymore for editing the manuscript. This work was supported by the Japan Initiative for Global Research Network on Infectious Diseases (J-GRID), the Global COE Program and a Grant-in-Aid from the Ministry of Education, Culture, Sports, Science and Technology (MEXT). Funding was also provided by a Grant-in-Aid from the Ministry of Health, Labour and Welfare of Japan and in part by the Intramural Research Program of the National Institute of Allergy and Infectious Diseases (NIAID), National Institutes of Health (NIH).
References
- Amman B. R., Carroll S. A., Reed Z. D., Sealy T. K., Balinandi S., Swanepoel R., Kemp A., Erickson B. R., Comer J. A. & other authors (2012). Seasonal pulses of Marburg virus circulation in juvenile Rousettus aegyptiacus bats coincide with periods of increased risk of human infection. PLoS Pathog 8, e1002877 10.1371/journal.ppat.1002877 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brindley M. A., Hughes L., Ruiz A., McCray P. B., Jr, Sanchez A., Sanders D. A., Maury W. (2007). Ebola virus glycoprotein 1: identification of residues important for binding and postbinding events. J Virol 81, 7702–7709 10.1128/JVI.02433-06 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dube D., Brecher M. B., Delos S. E., Rose S. C., Park E. W., Schornberg K. L., Kuhn J. H., White J. M. (2009). The primed ebolavirus glycoprotein (19-kilodalton GP1,2): sequence and residues critical for host cell binding. J Virol 83, 2883–2891 10.1128/JVI.01956-08 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dye J. M., Herbert A. S., Kuehne A. I., Barth J. F., Muhammad M. A., Zak S. E., Ortiz R. A., Prugar L. I., Pratt W. D. (2012). Postexposure antibody prophylaxis protects nonhuman primates from filovirus disease. Proc Natl Acad Sci U S A 109, 5034–5039 10.1073/pnas.1200409109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feldmann H., Will C., Schikore M., Slenczka W., Klenk H. D. (1991). Glycosylation and oligomerization of the spike protein of Marburg virus. Virology 182, 353–356 10.1016/0042-6822(91)90680-A [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feldmann H., Nichol S. T., Klenk H. D., Peters C. J., Sanchez A. (1994). Characterization of filoviruses based on differences in structure and antigenicity of the virion glycoprotein. Virology 199, 469–473 10.1006/viro.1994.1147 [DOI] [PubMed] [Google Scholar]
- Fofana I., Fafi-Kremer S., Carolla P., Fauvelle C., Zahid M. N., Turek M., Heydmann L., Cury K., Hayer J. & other authors (2012). Mutations that alter use of hepatitis C virus cell entry factors mediate escape from neutralizing antibodies. Gastroenterology 143, 223–233 10.1053/j.gastro.2012.04.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Francica J. R., Varela-Rohena A., Medvec A., Plesa G., Riley J. L., Bates P. (2010). Steric shielding of surface epitopes and impaired immune recognition induced by the Ebola virus glycoprotein. PLoS Pathog 6, e1001098 10.1371/journal.ppat.1001098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- García-Barreno B., Portela A., Delgado T., López J. A., Melero J. A. (1990). Frame shift mutations as a novel mechanism for the generation of neutralization resistant mutants of human respiratory syncytial virus. EMBO J 9, 4181–4187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hangartner L., Zinkernagel R. M., Hengartner H. (2006). Antiviral antibody responses: the two extremes of a wide spectrum. Nat Rev Immunol 6, 231–243 10.1038/nri1783 [DOI] [PubMed] [Google Scholar]
- Holland J. J., Domingo E., de la Torre J. C., Steinhauer D. A. (1990). Mutation frequencies at defined single codon sites in vesicular stomatitis virus and poliovirus can be increased only slightly by chemical mutagenesis. J Virol 64, 3960–3962 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ito H., Watanabe S., Takada A., Kawaoka Y. (2001). Ebola virus glycoprotein: proteolytic processing, acylation, cell tropism, and detection of neutralizing antibodies. J Virol 75, 1576–1580 10.1128/JVI.75.3.1576-1580.2001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kajihara M., Marzi A., Nakayama E., Noda T., Kuroda M., Manzoor R., Matsuno K., Feldmann H., Yoshida R. & other authors (2012). Inhibition of Marburg virus budding by nonneutralizing antibodies to the envelope glycoprotein. J Virol 86, 13467–13474 10.1128/JVI.01896-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuhn J. H., Radoshitzky S. R., Guth A. C., Warfield K. L., Li W., Vincent M. J., Towner J. S., Nichol S. T., Bavari S. & other authors (2006). Conserved receptor-binding domains of Lake Victoria Marburgvirus and Zaire Ebolavirus bind a common receptor. J Biol Chem 281, 15951–15958 10.1074/jbc.M601796200 [DOI] [PubMed] [Google Scholar]
- Lee J. E., Saphire E. O. (2009). Neutralizing Ebolavirus: structural insights into the envelope glycoprotein and antibodies targeted against it. Curr Opin Struct Biol 19, 408–417 10.1016/j.sbi.2009.05.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee J. E., Fusco M. L., Hessell A. J., Oswald W. B., Burton D. R., Saphire E. O. (2008). Structure of the Ebola virus glycoprotein bound to a human survivor antibody. Nature 454, 177–182 10.1038/nature07082 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manicassamy B., Wang J., Jiang H., Rong L. (2005). Comprehensive analysis of Ebola virus GP1 in viral entry. J Virol 79, 4793–4805 10.1128/JVI.79.8.4793-4805.2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marzi A., Yoshida R., Miyamoto H., Ishijima M., Suzuki Y., Higuchi M., Matsuyama Y., Igarashi M., Nakayama E. & other authors (2012). Protective efficacy of neutralizing monoclonal antibodies in a nonhuman primate model of Ebola hemorrhagic fever. PLoS ONE 7, e36192 10.1371/journal.pone.0036192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matsuno K., Kishida N., Usami K., Igarashi M., Yoshida R., Nakayama E., Shimojima M., Feldmann H., Irimura T. & other authors (2010). Different potential of C-type lectin-mediated entry between Marburg virus strains. J Virol 84, 5140–5147 10.1128/JVI.02021-09 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakayama E., Takada A. (2011). Ebola and Marburg viruses. J Disast Res 6, 381–389 [Google Scholar]
- Nakayama E., Tomabechi D., Matsuno K., Kishida N., Yoshida R., Feldmann H., Takada A. (2011). Antibody-dependent enhancement of Marburg virus infection. J Infect Dis 204 (Suppl. 3), S978–S985 10.1093/infdis/jir334 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Negredo A., Palacios G., Vázquez-Morón S., González F., Dopazo H., Molero F., Juste J., Quetglas J., Savji N. & other authors (2011). Discovery of an Ebolavirus-like filovirus in europe. PLoS Pathog 7, e1002304 10.1371/journal.ppat.1002304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neumann G., Feldmann H., Watanabe S., Lukashevich I., Kawaoka Y. (2002). Reverse genetics demonstrates that proteolytic processing of the Ebola virus glycoprotein is not essential for replication in cell culture. J Virol 76, 406–410 10.1128/JVI.76.1.406-410.2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neumann G., Geisbert T. W., Ebihara H., Geisbert J. B., Daddario-DiCaprio K. M., Feldmann H., Kawaoka Y. (2007). Proteolytic processing of the Ebola virus glycoprotein is not critical for Ebola virus replication in nonhuman primates. J Virol 81, 2995–2998 10.1128/JVI.02486-06 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olinger G. G., Jr, Pettitt J., Kim D., Working C., Bohorov O., Bratcher B., Hiatt E., Hume S. D., Johnson A. K. & other authors (2012). Delayed treatment of Ebola virus infection with plant-derived monoclonal antibodies provides protection in rhesus macaques. Proc Natl Acad Sci U S A 109, 18030–18035 10.1073/pnas.1213709109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qiu X., Audet J., Wong G., Pillet S., Bello A., Cabral T., Strong J. E., Plummer F., Corbett C. R. & other authors (2012). Successful treatment of Ebola virus-infected cynomolgus macaques with monoclonal antibodies. Sci Transl Med 4, 138ra81 10.1126/scitranslmed.3003876 [DOI] [PubMed] [Google Scholar]
- Reynard O., Borowiak M., Volchkova V. A., Delpeut S., Mateo M., Volchkov V. E. (2009). Ebolavirus glycoprotein GP masks both its own epitopes and the presence of cellular surface proteins. J Virol 83, 9596–9601 10.1128/JVI.00784-09 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rowe C. L., Baker S. C., Nathan M. J., Fleming J. O. (1997a). Evolution of mouse hepatitis virus: detection and characterization of spike deletion variants during persistent infection. J Virol 71, 2959–2969 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rowe C. L., Fleming J. O., Nathan M. J., Sgro J. Y., Palmenberg A. C., Baker S. C. (1997b). Generation of coronavirus spike deletion variants by high-frequency recombination at regions of predicted RNA secondary structure. J Virol 71, 6183–6190 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanchez A., Geisbert T. W., Feldmann H. (2007). Filoviridae: Marburg and Ebola viruses. In Fields Virology, 5th edn, pp. 1409–1448 Edited by Knipe D. M., Howley P. M. Philadelphia, PA: Lippincott Williams & Wilkins [Google Scholar]
- Schnell M. J., Buonocore L., Kretzschmar E., Johnson E., Rose J. K. (1996). Foreign glycoproteins expressed from recombinant vesicular stomatitis viruses are incorporated efficiently into virus particles. Proc Natl Acad Sci U S A 93, 11359–11365 10.1073/pnas.93.21.11359 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shedlock D. J., Bailey M. A., Popernack P. M., Cunningham J. M., Burton D. R., Sullivan N. J. (2010). Antibody-mediated neutralization of Ebola virus can occur by two distinct mechanisms. Virology 401, 228–235 10.1016/j.virol.2010.02.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simmons G., Wool-Lewis R. J., Baribaud F., Netter R. C., Bates P. (2002). Ebola virus glycoproteins induce global surface protein down-modulation and loss of cell adherence. J Virol 76, 2518–2528 10.1128/jvi.76.5.2518-2528.2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takada A., Robison C., Goto H., Sanchez A., Murti K. G., Whitt M. A., Kawaoka Y. (1997). A system for functional analysis of Ebola virus glycoprotein. Proc Natl Acad Sci U S A 94, 14764–14769 10.1073/pnas.94.26.14764 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takada A., Feldmann H., Stroeher U., Bray M., Watanabe S., Ito H., McGregor M., Kawaoka Y. (2003). Identification of protective epitopes on Ebola virus glycoprotein at the single amino acid level by using recombinant vesicular stomatitis viruses. J Virol 77, 1069–1074 10.1128/JVI.77.2.1069-1074.2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takada A., Fujioka K., Tsuiji M., Morikawa A., Higashi N., Ebihara H., Kobasa D., Feldmann H., Irimura T., Kawaoka Y. (2004). Human macrophage C-type lectin specific for galactose and N-acetylgalactosamine promotes filovirus entry. J Virol 78, 2943–2947 10.1128/JVI.78.6.2943-2947.2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Towner J. S., Amman B. R., Sealy T. K., Carroll S. A., Comer J. A., Kemp A., Swanepoel R., Paddock C. D., Balinandi S. & other authors (2009). Isolation of genetically diverse Marburg viruses from Egyptian fruit bats. PLoS Pathog 5, e1000536 10.1371/journal.ppat.1000536 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Volchkov V. E., Volchkova V. A., Ströher U., Becker S., Dolnik O., Cieplik M., Garten W., Klenk H. D., Feldmann H. (2000). Proteolytic processing of Marburg virus glycoprotein. Virology 268, 1–6 10.1006/viro.1999.0110 [DOI] [PubMed] [Google Scholar]
- Wilson J. A., Hevey M., Bakken R., Guest S., Bray M., Schmaljohn A. L., Hart M. K. (2000). Epitopes involved in antibody-mediated protection from Ebola virus. Science 287, 1664–1666 10.1126/science.287.5458.1664 [DOI] [PubMed] [Google Scholar]
- Wool-Lewis R. J., Bates P. (1998). Characterization of Ebola virus entry by using pseudotyped viruses: identification of receptor-deficient cell lines. J Virol 72, 3155–3160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wool-Lewis R. J., Bates P. (1999). Endoproteolytic processing of the Ebola virus envelope glycoprotein: cleavage is not required for function. J Virol 73, 1419–1426 [DOI] [PMC free article] [PubMed] [Google Scholar]


