Abstract
The restricted and repetitive behaviors of children with autism can interfere with family functioning as well as learning and socialization opportunities for the child. To date, neither pharmacological nor comprehensive behavioral treatments have been found to be consistently effective at significantly reducing children’s engagement in repetitive behaviors. We developed Family-Implemented Treatment for Behavioral Inflexibility (FITBI) to target the full variety of repetitive behaviors found in autism. For the current study, a therapist and parents of five children with autism (mean age = 48 months) co-implemented FITBI in a clinic setting over a 12-week treatment period. Using single case design methodology, significant reductions in repetitive behaviors were found for all participants and maintenance of treatment effects for 4 of 5 participants.
Keywords: Autism spectrum disorders, Repetitive behaviors, Treatment
Introduction
The restricted and repetitive patterns of behavior frequently dominate the daily activities of children with autism, and often significantly impact their learning and development of adaptive behaviors and skills (Koegel and Covert 1972; Rutter 1978; Varni et al. 1979; Pierce and Courchesne 2001). It is now clear that a variety of forms of repetitive behavior are present in many cases of autism by 2–3 years of age (Mooney et al. 2006; Honey et al. 2008; Richler et al. 2007), and present with sufficient severity at this age to warrant early intervention (Bishop et al. 2007). Further, repetitive behaviors persist into adulthood and can be the “residual symptom” of autism once social-communication symptoms improve (Piven et al. 1996).
Repetitive behaviors also have been found to be strongly associated with the occurrence of mood and behavior problems in children with autism (Lam et al. 2005; Gabriels et al. 2005; Leyfer et al. 2006). Researchers involved in large scale studies on the well-being and functioning of families of children with autism have reported that repetitive and related problem behaviors are associated with elevated parent stress (Bishop et al. 2007; Lounds et al. 2007), engender negative parenting styles (Greenberg et al. 2004), and are among the most difficult aspects of autism that parents must deal with on a daily basis (Mercier et al. 2000). There are a variety of discrete types of repetitive behaviors that occur in autism (Lam and Aman 2007; Cuccaro et al. 2003; Bodfish et al. 1999, 2000; Turner 1999). This broad range of behavior has been subdivided into at least two conceptual categories: “lower-order” motor actions (stereotyped movements, repetitive manipulation of objects, and repetitive forms of self-injurious behavior) that are characterized by repetition of movement; and more complex or “higher-order” cognitive behaviors (compulsions, rituals and routines, insistence on sameness, and circumscribed interests) that are characterized by a rigid adherence to some rule or mental set (e.g., needing to have things “just so”) (Bodfish et al. 1995; Cuccaro et al. 2003; Turner 1999; Lewis and Bodfish 1998; Rutter 1978; Szatmari et al. 2006; Lam et al. 2008). This is important from the perspective of treatment development because proposed interventions for repetitive behavior in autism should be capable of targeting the full variety of repetitive behavior symptoms (Bodfish 2004).
Despite indicators of poorer functional skills associated with the expression of repetitive behaviors, parents and clinicians sometimes have debated whether or not to make repetitive behaviors the target of intervention. Some parents are struck by how “proficient” their children are in certain areas (e.g., memorizing facts, working on the computer) and how this stands in contrast with all the other things their children may not able to do (e.g., socialize with peers, communicate clearly, adapt to preschool, etc.). In these situations, parents sometimes express a fear to tread on these “islands of ability” (Mercier et al. 2000). However, another common scenario has involved parents who have seen the “meltdowns” and other negative side effects that are related to preventing the child from engaging in these repetitive behaviors and interests (Mercier et al. 2000). This appears to be a function of an underlying behavioral rigidity/lack of flexibility whereby situations that involve lack of or limited access to repetitive, ritualistic behaviors or interests can trigger bouts of severe irritability, aggression, or other problem behaviors (Green et al. 2006; Peters-Scheffer et al. 2008). From a treatment perspective, it is apparent that the generalized rigidity/inflexibility associated with repetitive patterns of behaviors and interests can significantly interfere with learning and socialization, and can become a motivating factor underneath the development of severe mood and behavior problems. Thus, repetitive behaviors and interests have the potential for interfering with child development and family well-being, and treatment can be seen as necessary when viewed as an approach to expand the child’s behavioral repertoire rather than simply thwarting or punishing the child’s repetitive behaviors and interests.
Recent controlled trials of joint attention and symbolic play interventions have demonstrated that these types of focused interventions can significantly impact core autism deficits in the area of social communication (Schertz and Odom 2007; Kasari et al. 2006). To date, a similar approach has not been applied to the development of focused interventions for restricted, repetitive behaviors, which has resulted in a lack of evidence-based treatments for these behaviors. A recent multisite, randomized controlled trial of the serotonin reuptake inhibitor, Citalopram, for the treatment of repetitive behaviors in autism failed to find significant treatment effects (King et al. 2009), and thus presently there are few established evidenced-based pharmacotherapies indicated for the treatment of repetitive behaviors in autism (cf. Wink et al., in press). There is evidence, however, that early behavioral treatment is an effective form of intervention for autism (Bodfish 2004; Dawson 2008). Indeed, a recent landmark study of the Early Start Denver Model (ESDM) for the treatment of toddlers with autism found significant treatment-related improvements for a large variety of clinical outcomes (e.g., IQ, adaptive behavior, language, and socialization); yet, the comprehensive ESDM treatment package failed to impact repetitive behaviors (Dawson et al. in press). Thus, interventions are still needed to address the full variety of repetitive behaviors, preoccupations, and fixated interests exhibited in autism. Although no clear approach has emerged to date from studies of either pharmacotherapy or comprehensive behavioral treatments, a body of well-controlled single-case design behavior analytic studies has shown that certain reinforcement-based/functional analytic forms of intervention can effectively treat stereotyped movements and self-injurious behaviors in children with developmental disabilities including autism (Gorman-Smith and Matson 1985; Bodfish 2004). Although these behavioral approaches to treatment have demonstrated efficacy in use with individuals with developmental disorders, key issues remain to be addressed, namely (a) validity with respect to higher-order repetitive behaviors characteristic of autism (e.g., rituals/sameness, preoccupations, restricted interests), and (b) translational utility with respect to routine application by parents across settings.
Our treatment approach, Family-Implemented Treatment for Behavioral Inflexibility (FITBI), used both direct instruction (e.g., discrete trials) and naturalistic behavioral teaching methods (e.g., embedded learning strategies) to treat the range of repetitive behaviors in autism. Overall the goals of FITBI were to (a) teach parents and caregivers to view repetitive behaviors using a neurodevelopmental model that approached these symptoms as part of a brain-based disorder that could be changed through specific experiential and learning exercises; (b) teach parents how to conduct FITBI treatment sessions—parents learned to identify high probability environmental cues that elicited the children’s symptoms, and subsequently taught their children to inhibit repetitive behaviors in the presence of these cues and replace them with alternative, adaptive behaviors; and (c) teach parents how to embed FITBI into their children’s everyday routines as a way to both diminish parental accommodation/reinforcement of repetitive behaviors and increase the overall dosage of FITBI their children received.
FITBI: Empirical Rationale and Description of Intervention
Response Interruption and Redirection (RIR) and Differential Reinforcement of Variability in behavioral responding (DRV) are the two behavior intervention strategies that comprise the FITBI treatment approach. These interventions are linked to the two categories of repetitive behavior in autism (i.e., higher order and lower order behaviors). RIR is designed to substantially decrease children’s engagement in repetitive behaviors, and is primarily used with lower order behaviors that are typically non-functional or purposeless (e.g., repetitively spinning objects, prolonged visual inspection of parts of objects). In contrast, DRV is designed to shape and increase the child’s novel engagement with repetitive behavior stimuli, and is primarily used with higher order behaviors that are perserverative but potentially functional (e.g., child repetitively watching a video, or only playing with Disney characters).
As a behavioral strategy, RIR has involved physically or verbally blocking/interfering with children’s engagement in inappropriate behavior and redirecting them to engage in an alternative behavior. RIR has been used to treat vocal stereotypies (Ahearn et al. 2007), self-injury (Azrin et al. 1988), and self-stimulatory behaviors in individuals with developmental disabilities (Koegel et al. 1974). In comparison, differential reinforcement involves reinforcing the child for engaging in any other behavior besides the targeted, inappropriate behavior while ignoring occurrences of the inappropriate behavior (Newman et al. 1997; Piazza et al. 1996). DRV is one specific type of differential reinforcement. The rationale for using this approach is that children with autism can be taught to vary their behavioral responses by directly reinforcing variability/novelty of responses, and that engaging in variable behavior is incompatible with engaging in perserverative responses (Miller and Neuringer 2000; Neuringer 2004). Previous research has shown that variability can be increased by directly reinforcing it (Holman et al. 1977; Machado 1989; Napolitano et al. 2010; Neuringer 1986; Pryor et al. 1969).
FITBI Overview
For the present study, FITBI implementation occurred across 12 weekly sessions with the first session solely focused on parent education and training, hence, the child may or may not have been present. Each of the subsequent treatment sessions lasted approximately 60–120 min during which time the therapist-parent–child triad completed two or three blocks of FITBI instructional trials. Initial treatment sessions involved more parent instruction and preparation and thus only 1–2 FITBI teaching blocks typically were conducted. Within each FITBI block, 8–10 consecutive teaching trials were attempted with the child being presented with items or situations that trigger the repetitive behavior (i.e., antecedent stimuli) followed by a prompt that the child not contact the item and/or engage in repetitive behavior with the item (i.e., RIR) or to appropriately engage with the item (i.e., DRV). The procedures were initially presented in a repeated discrete trials manner to facilitate practice and learning, and then moved to a naturalistic teaching approach (e.g., embedding teaching trials into play-based activities) to facilitate maintenance and generalization. To assist with the demand that habitual repetitive behaviors be inhibited, we taught the child an alternative behavior. Often early in FITBI, the child must be physically prompted to engage in the alternative behavior or to appropriately engage with the repetitive behavior-inducing/antecedent stimulus. If needed, an individualized behavior management plan was developed to help parents work through problem behaviors (e.g., extinction bursts) that may have resulted from physically redirecting the child to engage in the alternative behavior instead of repetitive behavior. Further, if more than one antecedent stimulus could evoke a specific repetitive behavior (e.g., presence of toy cars, puzzles, and toy blocks all were associated with lining up objects) then the stimuli were randomly interspersed throughout the FITBI teaching trials. Finally, parents were asked to implement FITBI strategies at home with their child.
The goal of treatment was for the child to immediately begin to engage in the alternative/appropriate behavior as soon as the evocative stimulus (i.e., stimulus that triggered repetitive behavior) was presented instead of repetitive behavior. A graduated time delay procedure was used to facilitate this goal whereby after presentation of the evocative stimulus the therapist waited for increasing amounts of time (e.g., 2 s, 5 s, 10 s, etc.) to see if the child self-initiated the alternative behavior. Graduated time delay continued until the child could spontaneously self-initiate and sustain engagement in the alternative behavior across three consecutive blocks of FITBI treatment trials.
In conclusion, there is a lack of focused, evidenced-based behavioral interventions to treat the full variety of repetitive behaviors in autism. We developed FITBI to target the clinical heterogeneity often associated with autism and the expression of repetitive behaviors. The purpose of this article is to present clinical outcome data on the FITBI treatment approach using experimental, single case design methodology.
Method
Participants
Five preschool aged children (M = 48 months of age; range 39–65 months) with a diagnosis of Autistic Disorder participated in the study. All participants had been diagnosed by an independent, licensed psychologist or psychiatrist prior to study enrollment. Participants were recruited through the distribution of fliers to local childcare centers, diagnostic clinics, and through the Autism Research Subject Registry at UNC-Chapel Hill. Once families expressed interest in the study, a research assistant conducted an initial screening over the phone to ensure participants met relevant inclusion/exclusion criteria, and if so, on-site assessments were then scheduled. Research staff administered the Autism Diagnostic Observation Schedule (ADOS; Lord et al. 2002) to confirm each participant’s diagnostic status. The survey forms version of the Vineland Adaptive Behavior Scales, second edition (VABS-II; Sparrow et al. 2005) was used to assess children’s developmental functioning; and the Repetitive Behavior Scale-Revised (RBS-R; Bodfish et al. 1999), a psychometrically-valid, informant-based measure, was used to assess repetitive behaviors. See Table 1 for participant and caregiver demographic information.
Table 1.
Child and family demographics
| Child | CA months | Sex | Race | VABS standard score |
RBS-R score | ADOS |
Maternal educationb | |
|---|---|---|---|---|---|---|---|---|
| Module | Severity scorea | |||||||
| Joshua | 40 | M | White | 62 | 33 | 1 | 10 | BA/BS |
| Barry | 39 | M | White | 67 | 17 | 1 | 9 | MA/MS |
| Sam | 44 | M | Black | 74 | 32 | 3 | 6 | MA/MS |
| Harry | 65 | M | Biracial | 88 | 36 | 3 | 6 | AA/AS |
| Rick | 53 | M | White | 84 | 38 | 2 | 6 | BA/BS |
CA chronological age, VABS Vineland Adaptive Behavior Scales (Standard Score: M = 100; SD = 15); RBS-R Repetitive Behavior Scale-Revised (higher scores indicate greater severity of repetitive behavior symptoms)
ADOS severity scores are based on a 1–10 rating scale, with higher scores indicating greater symptom severity (Gotham et al. 2009)
Degree status: AA/AS = Associate of Arts/Science, BA/BS = Bachelor of Arts/Science, MA/MS = Master of Arts/Science
For purposes of study enrollment, participants had to meet the following inclusion criteria: (a) between 2 to 6 years of age, (b) previous diagnosis of an autism spectrum disorder, and (c) parent identification of at least 2 repetitive behaviors that were frequent in occurrence and/or interfered with the child’s participation in everyday activities or routines (e.g., child lined up his toys for prolonged periods of time). Exclusionary criteria included (a) repetitive behavior occurred intermittently or was difficult to elicit in a clinic-based setting, (b) children with co-existing genetic or psychiatric disorders strongly associated with autism (e.g., FXS) or the presence of repetitive behaviors (e.g., OCD), (c) presence of a seizure disorder, and (d) parent refusal or inability to participate in 12 weeks of treatment. Concurrent behavioral therapies or medications were not exclusionary criteria. None of the children were taking medication at the time of study enrollment. Two children were excluded because their behaviors occurred infrequently and did not interfere with ongoing family routines, and one child was excluded because his repetitive behavior would have been difficult to elicit in the clinic (i.e., child wanted parent to drive the same direction each time they left home). The University of North Carolina at Chapel Hill IRB approved this study.
Experimental Procedures
Single-case research methodology was used to evaluate the effects of FITBI on the repetitive behaviors of five study participants. This methodology allows causal interpretations to be drawn with small N studies because each participant serves as his/her own control (Horner et al. 2005). Specifically, we used a multiple baseline across behaviors design with two behaviors targeted for each participant. Baseline and treatment session data were collected during a series of 5 min probes that occurred at the beginning of the family’s clinic visit. The clinic visit, itself, lasted from 60–120 min depending upon child cooperation. The first session (week 1 of 12) served as a psychoeducation session whereby the therapist described the treatment to the care-giver(s) and provided relevant information on repetitive behaviors in autism. In subsequent sessions for each child, a total of 20 min of probe data were collected—a 5 min therapist probe was conducted for each of the two target behaviors; and similarly, two, 5 min parent probes were conducted for those same behaviors. The order of parent and therapist probes was counterbalanced across the 5 children. In general, baseline sessions were conducted until therapist data appeared stable; however, in some cases we decided to move the child into the treatment phase early for ethical reasons since the treatment was only scheduled to be a total of 12 weeks. The decision to move children from the baseline to treatment phase primarily was based on therapist probe data as it took time for some parents to become comfortable conducting the probe sessions. In addition, given that the first 20 min of the clinic visit focused on the collection of probe data, which involved behavioral presses to elicit children’s repetitive behaviors, there were occasions where children refused to participate. One primary caregiver, all of whom were female, participated in the treatment sessions and probe data collection, although on some occasions both caregivers attended the session.
Setting, Materials, and Therapist
All sessions were conducted on-site at UNC-Chapel Hill in a clinic room equipped with a one-way observational mirror. The room contained a child-sized table and two child-sized chairs. In addition, two adult chairs were available for parents to sit and observe while the therapist interacted with the child or vice versa. Further, a carpeted area with age appropriate toys was available to the child during breaks between instructional trials. During the instructional trials, the stimuli that elicited the child’s repetitive behavior and stimuli that could be used to elicit more appropriate behavior were made available. The repetitive behavior stimuli were identified via parent report, and to conduct the trials the parent either brought the stimuli from home or we purchased replicas of the stimuli. The second author served as the therapist for all children; he holds a master’s degree in child development and previously worked with children with behavioral disorders.
Baseline Probe Sessions
For each targeted behavior, the parent and therapist conducted separate baseline sessions. During the baseline probe, the stimuli that elicited the child’s repetitive behavior was available and an equal number of neutrally-preferred tangible stimuli. The neutral stimuli were chosen using a direct preference assessment format. The specific procedures for conducting the preference assessment have been described elsewhere (Boyd et al. 2007). During the 5 min session, if the child was engaged in repetitive behavior, the parent or therapist was instructed to verbally prompt the child, using succinct prompts, every 30-seconds to redirect him/her to more appropriate play (e.g., “Let’s try to drive the car.”). If the child did not comply with the verbal request then it was followed by a hand-over-hand physical prompt. No other prompts were provided until the next 30-second interval. Throughout the probe session, however, the therapist or parent interacted with the child and verbally praised him/her when the child engaged in appropriate play while ignoring instances of repetitive behavior except those that occurred at the 30-second interval mark. A hand-held, digital timer was used to help the parent and therapist keep track of the time intervals. Further, the therapist would verbally remind the parent if the parent failed to deliver the child prompt.
Treatment Probe Sessions
The treatment probes were conducted in the same manner as the baseline probes with the exception being the addition of a stimulus to evoke an alternative, appropriate behavior. Thus, in addition to the presence of the repetitive behavior and neutral stimuli, an alternative behavior stimulus also was present during the treatment probes. This alternative stimulus also was used in the actual instructional trials that followed probe data collection to teach the child an appropriate behavior that could be engaged in while in the presence of the repetitive behavior stimulus. The alternative stimulus/behavior was selected either because of its functional incompatibility with the repetitive behavior, that is, it would be extremely difficult for the child to simultaneously engage in the repetitive and alternative behaviors (e.g., clapping hands together is incompatible with hand-flapping), or based on parent nomination of an alternative skill the parent wanted the child to learn. See Table 2 for a description of participants’ targeted repetitive behaviors and selected alternative behaviors. Follow-up data for participants were collected by conducting the treatment probes in the family’s home at 2-week and 4-week time points occurring after the completion of the 12 week clinic sessions. The duration of the follow-up probes was 3 min instead of 5 min, and only the parent conducted the probes.
Table 2.
Types of repetitive and alternative behaviors targeted with FITBI
| Repetitive behavior 1 | Treatment approach |
Alternative behavior 1 | Repetitive behavior 2 | Treatment approach |
Alternative behavior 2 |
|
|---|---|---|---|---|---|---|
| Joshua | Lining up objects | RIR | Taught functional play skills | Object attachment to outdoor sticks | RIR | Taught to hold other objects in his hand |
| Barry | Repetitive touching of flags | RIR | Taught to squeeze hands together | Repetitive touching of wind chimes | RIR | Taught to wait and ask adult to touch wind chime |
| Sam | Perseveration with cars | DRV | Taught to expand play routines with cars | Hoarding Toothbrushes | RIR | Gradual reduction of toothbrush collection |
| Harry | Fixated interest with drawing and writing bank checks | RIR | Taught to play with other toys in presence of bank checks | Preoccupation with drawing signs and labeling objects with those signs | DRV | Gradually reduced the amount of time he engaged in the activity |
| Rick | Perseveration with real and pretend elevators | RIR | Taught to play with other toys in presence of toy elevators, and taught to remain calm, wait and ask to push button for real-life elevators | Repeatedly watched the same movie | DRV | Taught to watch video only during scheduled video time |
Measures
Behavioral Coding
The authors developed the Direct Observation of Repetitive Behaviors in Autism (DORBA) coding system (Boyd et al. 2010). The coding system contained state/duration and point/event codes to capture a participant’s engagement in repetitive behavior, appropriate behavior, and/or problem behaviors (e.g., tantrums, aggression). The specific operational definitions for each of these behavioral categories can be obtained from the first author. Behavioral raters, naı¨ve to the purposes of the study, coded videotapes from the baseline, treatment, and follow-up probe sessions post-hoc. All coders were trained to a reliability criterion of ≥ 0.80, using a kappa statistic, based on training tapes from a separate pilot trial of FITBI. In addition to coding discrete categories of behavior, at the end of each 5 min probe session the coder also rated the interference level of the child’s repetitive behavior on a 0 (no interference) to 3 (severe interference) scale, indicating the degree to which the child’s repetitive behavior interfered with his/her ability to engage in alternative activities. The videos were coded using Observer XT 7.0 (Noldus 1991), a behavior coding software program that allowed for real time coding of frequency and duration-based behaviors. For each participant, reliability was calculated for at least 30% of the sessions across each study phase (i.e., baseline, treatment, and follow-up). For the probe sessions, a kappa statistic was used to compute the reliability of participant data for baseline (M = 0.81, range = 0.53–1.00), intervention (M = 0.84, range = 0.53–1.00), and follow-up (M = 0.85, range = 0.76–1.00). For the interference ratings, Pearson correlation coefficients were used to determine inter-rater reliability for parent (r = 0.74, p > 0.0001) and therapist (r = 0.82, p > 0.0001) sessions.
Effect Sizes
There has been some controversy over whether effect sizes, which are based on aggregated data, should be used with single-case research, which is based on individual subjects (Scruggs and Mastropieri 1998; Strain et al. 1998). We have chosen to report the simple effect size calculation of mean baseline reduction (MBLR) to reflect participants’ average amount of reduction in repetitive behavior. The data will be reported for each participant to retain individual subject effects instead of being averaged across participants. The formula used to calculate MBLR was subtracting the mean of the treatment data from the mean of the baseline data then dividing that number by the mean of the baseline data and multiplying by 100 (Campbell 2004).
Therapist and Parent Adherence
Data were collected on therapist and parent implementation of FITBI procedures using project-created fidelity checklists. Specifically, data were collected on the number of FITBI steps implemented correctly (0 = not implemented correctly, 1 = implemented correctly), thus, the fidelity checklists only reflect quantity and not quality of implementation. The first author (co-developer of FITBI) was the primary observer of therapist adherence and completed the 8-item therapist adherence checklist for 20% of each participant’s treatment sessions. The second author (therapist) was the primary observer of parent adherence and completed the 7-item parent checklist for 20% of participant’s sessions. Across participants, reliability data were collected using an exact agreement formula (dividing number of agreements by number of agreements plus disagreements multiplied by 100) for 50% of parent (M = 100%) and therapist (M = 97.5%) sessions, respectively. On average, parents implemented 88.5% of steps correctly and the therapists’ average was 87.5%.
Results
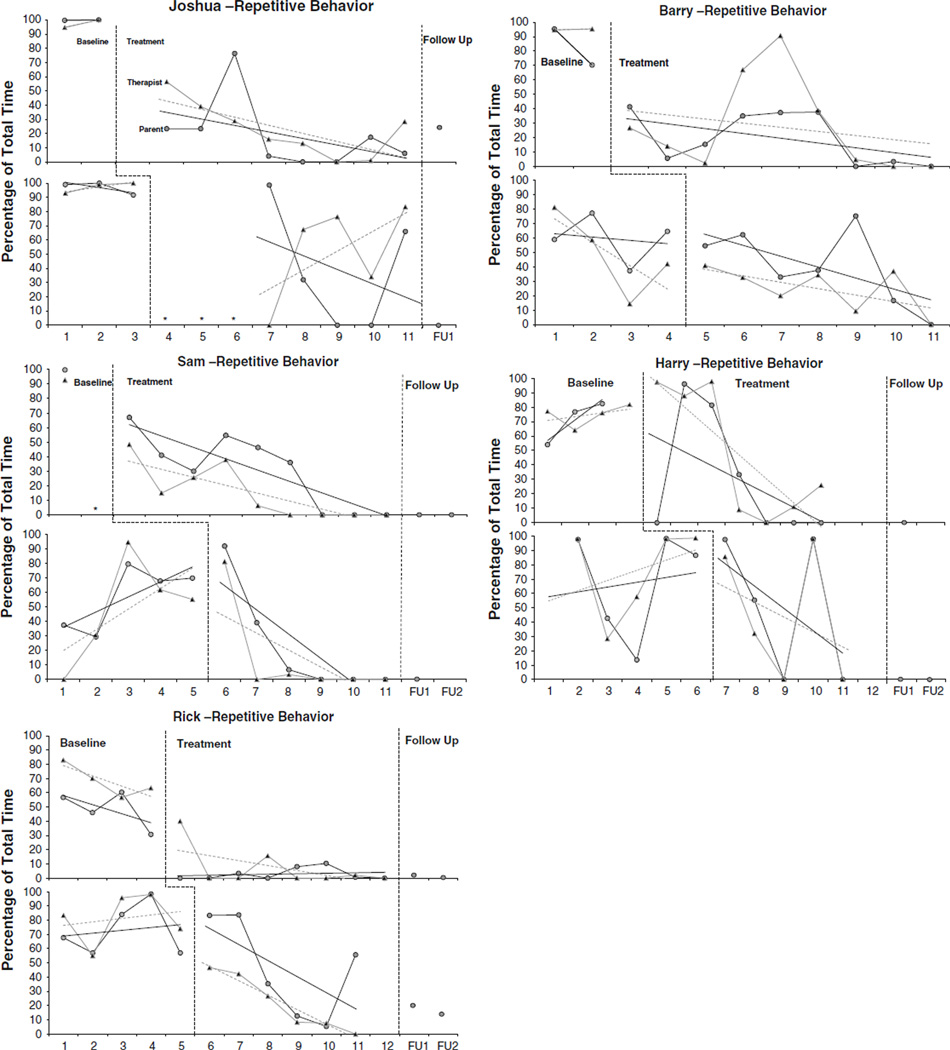
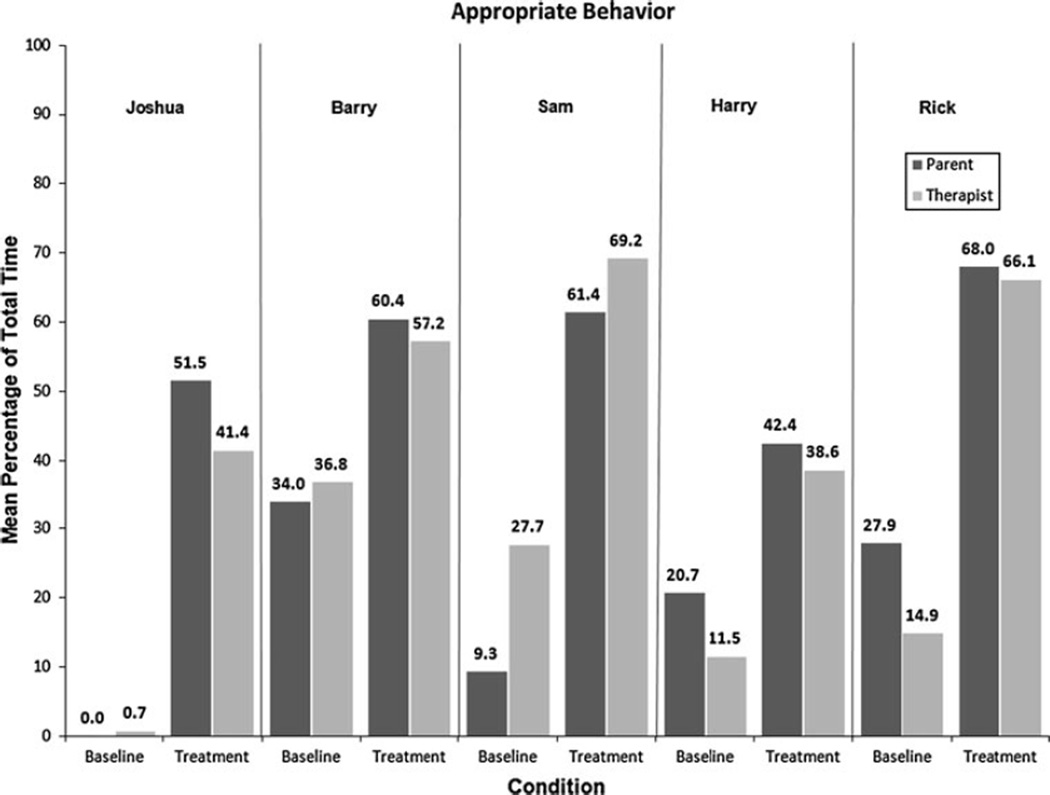
Based on recently published guidelines from the What Works Clearinghouse, there are at least six features of visual analysis of data that can be used to evaluate participant outcomes for single case design research (see Kratochwill et al. 2010). We have elected to directly report on four of those criteria—level (mean score for each phase), variability (range of data points within a phase), trend (slope of the best-fitting line for the data), and consistency of data patterns across phases/participants; however, the remaining two criteria (immediacy of effect and data overlap) can be gleaned from the line graphs in Fig. 1. We have reported these data for the primary outcome of reductions in repetitive behaviors. It is important to note that the data are reported separately for parent and therapist probe sessions; however, the data are averaged across the two target behaviors to lessen the redundancy with the line graphs in Fig. 1.
Fig. 1.
Child engagement in repetitive behavior. The graphs reflect the percentage of time the child engaged in repetitive behavior during the session. The dashed lines reflect data trend lines for the therapist and the solid lines reflect trend lines for the parent. In baseline sessions with only 2–3 data points, the trend lines directly overlap the lines for the actual data. Note. The asterisk indicates we were unable to collect data during a particular session, which primarily occurred because of child noncompliance
Level and Variability of Baseline Data
Averaged across the two target behaviors, the mean percentage of time Joshua engaged in repetitive behavior was 98% (range: 92–100%) during parent probes and 97% (range: 93–100%) during therapist probes. During these same probes, the mean amount of time Joshua engaged in appropriate behavior (i.e., engaged with neutrally-preferred stimuli) was 0% and 0.7% of the time during parent and therapist probe sessions, respectively (see Fig. 2). Barry engaged in repetitive behavior 66% (range: 37–95%) of the time during parent probes, 63% (range: 14–95%) of the time during therapist probes, and mean engagement in appropriate behavior was 34% and 37%, respectively. Sam engaged in repetitive behavior for 68% (range: 37–100%) of the time during parent probes and 59% (range: 0–94%) of the time during therapist probes. His engagement in appropriate behavior averaged 9% for parent and 28% for therapist probes. For Sam, only one baseline data point is reported for target behavior 1 because of child non-compliance, which subsequently affected the rater’s ability to code subsequent baseline sessions. For Harry, the mean amount of time he engaged in repetitive behavior during parent probes was 69% (range: 14–98%) and it was 76% (range: 28–99%) for therapist probes; he engaged in appropriate behavior during 21% and 12% of those same probes, respectively. Rick engaged in repetitive behavior 62% (range: 31–98%) of the time and appropriate behavior 28% of the time during parent probes, and engaged in repetitive versus appropriate behavior 75% (range: 55–98%) and 15% of the time during therapist probes.
Fig. 2.
Child engagement in appropriate behavior
Level and Variability of Treatment Data
The mean percentage of time Joshua engaged in repetitive behavior decreased to 27% (range: 0–99%) for parent probes and 34% (range: 0–83%) for therapist treatment probes. The mean percentage of time he engaged in appropriate behavior (i.e., engaged either with neutrally-preferred stimuli or the alternative behavior stimulus) during parent and therapist probes increased to 52% and 41%, respectively. Averaged across the two target behaviors, Barry’s engagement in repetitive behavior decreased to 29% (range: 0–75%) for parent probes and 26% (range: 0–91%) for therapist probes. His engagement in appropriate behavior increased to 60% for parent probes and 57% for therapist probes. Sam engaged in repetitive behavior 23% (range: 0–67%) of the time during the parent probes and 10% (range: 0–48%) of the time during therapist probes, and engaged in appropriate behavior 61% and 69% of the time during those respective probes. Harry’s engagement in repetitive behavior decreased to 39% (range: 0–98%) for parent probes and 45% (range: 0–97%) for therapist probes, and for appropriate behavior, increased to 42% for parent probes and 39% for therapist probes. Rick’s engagement in repetitive behavior declined to 21% (range: 0–84%) in the parent probes and 24% (range: 0–47%) in the therapist probes. His engagement in appropriate behavior increased to 68% and 66%, respectively, for parent and therapist probes.
Level and Variability of Follow-up Data
We attempted to collect follow-up data at 2 and 4 week time points after the 12-week treatment period. The reported follow-up data have been averaged across the two behaviors and the two time points for parsimony. For Joshua, data were only collected for the 4 week time point, and we were unable to collect follow-up data for Barry. At the 4 week follow-up time point, Joshua engaged in repetitive behavior 15% (range: 0–30%) of the time and engaged in appropriate behavior 46% of the time. Sam engaged in no repetitive behavior at follow-up and engaged in appropriate behavior for 77% of the time. Harry also engaged in no repetitive behavior at follow-up, and the average amount of time he engaged in appropriate behavior was 95%. Finally, Rick’s average amount of engagement in repetitive behavior was 10% (range: 0–21%) versus 83% for appropriate behavior.
Data Trends and Consistency of Effects
The trend lines in Fig. 1 show baseline data trends in the expected direction for Joshua, with engagement in repetitive behavior accelerating during this phase. The opposite effect, as expected, is primarily found for his treatment data with engagement in repetitive behavior decelerating; however, an exception is that the trend line for the therapist data for target behavior 2 is increasing over time. For Barry, there is already a decelerating data trend for either parent (target behavior 1) or therapist (target behavior 2) baseline sessions that continues into the treatment phase. Baseline trend lines for Sam show an increasing trend for target behavior 2; it is difficult to gauge the true trend of target behavior 1 as there is only one data point. Yet, his treatment data show trend lines that decelerate to 0% engagement in repetitive behavior for both target behaviors. For Harry, his trend lines are in the expected direction for the baseline (i.e., accelerating) and treatment (i.e., decelerating) phases. Rick’s data show the expected effect for target behavior 2; however, there is a decelerating baseline trend for target behavior 1. Based on the trend lines, a functional relationship between the intervention and change in the dependent variable can only be established for Joshua, Sam, and Harry.
Effect Sizes and Interference Ratings
Based on MBLR effect size calculations, Joshua’s engagement in repetitive behavior resulted in a reduction of 69% from baseline to treatment for parent probes and 60% for therapist probes. On average, the behavior coder rated the interference of his repetitive behavior a 3 (out of a scale of 0 to 3; range: 3) during both baseline parent and therapist probes; however, during treatment his average rating was 1.4 (range: 0–3) for parent probes and 1.5 (range: 0–3) for therapist probes. Average reductions in repetitive behavior based on MBLR scores for Barry were 58% for parent and 61% for therapist probes. Barry’s interference ratings were 2.2 (range: 2–3) and 2 (range: 2) during respective parent and therapist baseline probes, and his ratings were 1.3 (range: 0–2) and 1.4 (range: 0–2) during parent and therapist treatment probes. Effect size calculations for Sam resulted in a 52% reduction in repetitive behavior for parent and 71% for therapist probes, with his interference ratings being 1.9 (range: 0–3) for parent baseline and 1.1 (range: 0–2) for parent treatment, and 1.8 (range: 0 −3) for therapist baseline and 0.8 (range: 0 −3) for therapist treatment. The MBLR scores for Harry showed a 44% reduction across parent sessions and a 40% reduction across therapist sessions. His interference ratings were 2.1 (range: 1–3) and 2.3 (range: 2–3) for parent and therapist baseline, and 1.3 (range: 0–3) and 1.3 (range: 0–3) for parent and therapist treatment probes. Finally, for Rick, the average amount of reduction in repetitive behavior was 68% for parent probes and 66% for therapist probes, with interference scores being 2.1 (range: 2–3) and 2.2 (range: 2–3) in parent and therapist baseline, respectively, and 0.9 (range: 0–2) and 0.9 (range: 0–2) in parent and therapist treatment.
Discussion
Overall we found substantial reductions in the occurrence of repetitive behaviors for all participants involved in the FITBI trial. Further, concurrent increases were found for children’s engagement in alternative activities, which suggests the treatment also may be effective at targeting behavioral inflexibility. It is this underlying deficit in behavioral inflexibility that is thought to be associated with the expression of repetitive and problem behavior in autism (Green et al. 2006). It is reasonable to presume that a child who is more flexible in their ways of thinking and engaging with their environment will have more opportunities to explore and learn a variety of adaptive skills and behaviors (Pierce and Courchesne 2001).
In examining specific data patterns, again, we found that the mean amount of time children engaged in repetitive behavior decreased while the mean amount of time they engaged in appropriate behavior increased. It should be noted that the percentage of time children engaged in repetitive or appropriate behavior did not always total to 100% of the time because the child may have been engaged in other behaviors (e.g., social overture) or off-camera during a coding interval. For participants, there remained quite a bit of variability in the data across baseline and treatment phases suggesting that there continued to be day-to-day fluctuations in the occurrence of these behaviors. Across the treatment sessions we attempted to intersperse different antecedent stimuli that elicited the child’s repetitive behavior in order to work on decreasing these behaviors across situations. The variability in the findings, however, may suggest that other contextual determinants of the behavior exist and/or that undetermined sensory (i.e., non-tangible) aspects of the environment or those intrinsic to the child may have continued to elicit these behaviors (Boyd et al. 2009). In evaluating data trends, it appears that for two participants (Barry and Rick) there were decelerating trends in the baseline phase, which suggests their engagement in repetitive behavior was decreasing prior to implementation of the intervention. Thus, intervention effects are based on the three participants for whom more consistent data patterns were found in terms of an accelerating trend in baseline followed by reductions in repetitive behavior upon intervention implementation. Based on the What Works Clearinghouse guidelines at least three demonstrations of an effect must be found to determine a functional or causal relationship between the independent and dependent variable in single case research (Kratochwill et al. 2010). The effect size calculations reflected significant reductions in repetitive behaviors for all participants; however, this finding may be related to the difficulty of using and interpreting effect sizes with single case designs (Jenson et al. 2007). Finally, the parent adherence and follow-up data suggest that caregivers can reliably implement FITBI strategies with and without on-going guidance from a therapist. This is important from a treatment development perspective as ultimately we want to develop interventions that are sustainable across settings and intervention agents.
FITBI has the potential to be a cost-effective treatment for repetitive behaviors because it is designed to target both lower and higher order repetitive behaviors, be useful for individuals with autism across the range of intellectual functioning, and be implemented by different intervention agents. Our focus on a behavioral treatment for higher order repetitive behaviors found in autism is one extension of current behavioral analytic studies, which have mainly focused on the treatment of stereotypic and self-injurious behaviors (Bodfish 2004). However, even if a child exhibits clinically significant levels of repetitive behaviors it is not entirely clear that FITBI is always the most appropriate form of treatment. It is possible that lack of response to FITBI or other behavioral approaches may provide a justification for the use of psychopharmacological treatments, especially for young children.
Finally, the use of single case design introduces study design strengths, such as increased internal validity; however, it also introduces limitations. Obviously, the small sample size limits the study’s external validity. Further, the implementation of FITBI in a clinic setting under the guidance of a skilled therapist helped to ensure parents followed a standard treatment protocol, yet, reduces the generalizability and potentially the replication, of the findings. The follow-up data collected in the home in which the parents conducted the probes on their own suggest that parents continued to successfully use the treatment strategies on their own. Still it cannot be ruled out that the continued reductions in repetitive behavior found in the home are a by-product of transfer of stimulus control, that is, the child learned to inhibit repetitive behavior in the presence of the therapist and parent because he associated them with directives to stop engaging in those behaviors. Future research should involve a larger randomized clinical trial and examine if the child also inhibits repetitive behavior in the presence of a novel person or when left to his own devices.
Acknowledgments
Development of this paper was partially supported with internal funding from the Frank Porter Graham Child Development Institute at the University of North Carolina at Chapel Hill.
Contributor Information
Brian A. Boyd, Email: brian_boyd@med.unc.edu, Division of Occupational Science, Department of Allied Health Sciences, University of North Carolina at Chapel Hill, CB# 7122, Bondurant Hall, Chapel Hill, NC 27599-7120, USA.
Stephen G. McDonough, FPG Child Development Institute, University of North Carolina at Chapel Hill, Chapel Hill, NC, USA
Betty Rupp, Carolina Institute for Developmental Disabilities, University of North Carolina at Chapel Hill, Chapel Hill, NC, USA.
Faraaz Khan, Division of Occupational Science, Department of Allied Health Sciences, University of North Carolina at Chapel Hill, CB# 7122, Bondurant Hall, Chapel Hill, NC 27599-7120, USA.
James W. Bodfish, Carolina Institute for Developmental Disabilities, University of North Carolina at Chapel Hill, Chapel Hill, NC, USA
References
- Ahearn WH, Clark KM, MacDonald RPF, Chung B. Assessing and treating vocal stereotypy in children with autism. Journal of Applied Behavior Analysis. 2007;40:263–275. doi: 10.1901/jaba.2007.30-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Azrin NH, Besalel V, Jamner JP, Caputa JN. Comparative study of behavioral methods of treating severe self-injury. Behavior Resident Treatment. 1988;3:119–152. [Google Scholar]
- Bishop S, Reichler J, Cain A, Lord C. Predictors of perceived negative impact in mothers of children with autism spectrum disorders. American Journal on Mental Retardation. 2007;112:450–461. doi: 10.1352/0895-8017(2007)112[450:POPNII]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- Bodfish JW. Treating the core features of autism: Are we there yet? Mental Retardation and Developmental Disabilities Research Reviews. 2004;10:318–326. doi: 10.1002/mrdd.20045. [DOI] [PubMed] [Google Scholar]
- Bodfish JW, Crawford TW, Powell SB, Parker DE, Golden RN, Lewis MH. Compulsions in adults with mental retardation: Prevalence, phenomenology, and comorbidity with stereotypy and self-injury. American Journal of Mental Retardation. 1995;100:183–192. [PubMed] [Google Scholar]
- Bodfish JW, Symons FJ, Lewis MH. The Repetitive Behavior Scales (RBS). Western Carolina Center Research Reports. 1999. [Google Scholar]
- Bodfish JW, Symons FJ, Parker DE, Lewis MH. Varieties of repetitive behavior in autism: Comparison to mental retardation. Journal of Autism and Developmental Disabilities. 2000;30:237–243. doi: 10.1023/a:1005596502855. [DOI] [PubMed] [Google Scholar]
- Boyd BA, Conroy MA, Mancil GR, Nakao T, Alter P. Effects of circumscribed interests on the social behaviors of children with autism spectrum disorders. Journal of Autism and Developmental Disorders. 2007;37:1550–1561. doi: 10.1007/s10803-006-0286-8. [DOI] [PubMed] [Google Scholar]
- Boyd BA, McBee M, Holtzclaw T, Baranek GT, Bodfish JW. Relationships among repetitive behaviors, sensory features, and executive functions in high functioning autism. Research in Autism Spectrum Disorders. 2009;3:959–966. doi: 10.1016/j.rasd.2009.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyd BA, Rupp B, Bodfish JW. Direct observation of repetitive behaviors in autism. University of North Carolina at Chapel Hill; 2010. Unpublished manual. [Google Scholar]
- Campbell JM. Statistical comparison of four effect sizes for single-subject designs. Behavior Modification. 2004;28:234–246. doi: 10.1177/0145445503259264. [DOI] [PubMed] [Google Scholar]
- Cuccaro ML, Shao Y, Grubber J, Slifer M, Wolpert CM, Donnelly SL, et al. Factor analysis of restricted and repetitive behaviors in autism using the Autism Diagnostic Interview-R. Child Psychiatry and Human Development. 2003;34(1):3–17. doi: 10.1023/a:1025321707947. [DOI] [PubMed] [Google Scholar]
- Dawson G. Early behavioral intervention, brain plasticity, and the prevention of autism spectrum disorder. Development and Psychopathology. 2008;20:775–803. doi: 10.1017/S0954579408000370. [DOI] [PubMed] [Google Scholar]
- Dawson G, Rogers R, Munson J, Smith M, Winter J, Greenson J, et al. Randomized, controlled trial of the Early Start Denver Model, a developmental behavioral intervention for toddlers with autism: Effects on IQ, adaptive behavior, and autism diagnosis. Pediatrics. doi: 10.1542/peds.2009-0958. (in press). published online. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gabriels RL, Cuccaro ML, Hill DE, Ivers BJ, Goldson E. Repetitive behaviors in autism: Relationships with associated clinical features. Research in Developmental Disabilities. 2005;26:169–181. doi: 10.1016/j.ridd.2004.05.003. [DOI] [PubMed] [Google Scholar]
- Gorman-Smith D, Matson J. A review of treatment research for self-injurious and stereotyped responding. Journal of Mental Deficiency Research. 1985;29:295–308. doi: 10.1111/j.1365-2788.1985.tb00357.x. [DOI] [PubMed] [Google Scholar]
- Gotham K, Pickles A, Lord C. Standardizing ADOS scores for a measure of symptom severity in autism spectrum disorders. Journal of Autism and Developmental Disorders. 2009;39:693–705. doi: 10.1007/s10803-008-0674-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green V, Sigafoos J, Pituch K, Itchon J, O’Reilly M, Lancioni G. Assessing behavioral inflexibility in individuals with developmental disabilities. Focus on Autism and Developmental Disabilities. 2006;4:230–236. [Google Scholar]
- Greenberg JS, Seltzer MM, Krauss MW, Chou RJ, Hong J. The effect of quality of the relationship between mothers and adult children with disabilities: The mediating role of optimism. American Journal of Orthopsychiatry. 2004;74:14–25. doi: 10.1037/0002-9432.74.1.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holman J, Goetz EM, Baer DM. The training of creativity as an operant and an examination of its generalization characteristics. In: Etzel BC, LeBlanc JM, Baer DM, editors. New developments in behavior research, theory, method and application. Hillsdale, NJ: Lawrence Erlbaum Associates; 1977. [Google Scholar]
- Honey E, McConachie H, Randle V, Shearer H, Couteur AS. One-year change in repetitive behaviours [sic] in young children with communication disorders including autism. Journal of Autism and Developmental Disorders. 2008;38:1439–1450. doi: 10.1007/s10803-006-0191-1. [DOI] [PubMed] [Google Scholar]
- Horner RH, Carr EG, Halle J, McGee G, Odom S, Wolery M. The use of single subject research to identify evidence-based practice in special education. Exceptional Children. 2005;71:165–179. [Google Scholar]
- Jenson WR, Clark E, Kircher JC, Kristjansson SD. Statistical reform: Evidence-based practice, meta-analyses, and single subject designs. Psychology in the Schools. 2007;44:483–493. [Google Scholar]
- Kasari C, Freeman S, Paparella T. Joint attention and symbolic play in young children with autism: A randomized controlled intervention study. Journal of Child Psychology and Psychiatry. 2006;47:611–620. doi: 10.1111/j.1469-7610.2005.01567.x. [DOI] [PubMed] [Google Scholar]
- King B, Hollander E, Sikich L, McCraken J, Scahill L, Bregman J, et al. Lack of efficacy of citalopram in children with autism spectrum disorders and high levels of repetitive behavior. Archives of General Psychiatry. 2009;66:583–590. doi: 10.1001/archgenpsychiatry.2009.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koegel RL, Covert A. The relationship of self-stimulation to learning in autistic children. Journal of Applied Behavior Analysis. 1972;5:381–387. doi: 10.1901/jaba.1972.5-381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koegel RL, Firestone PB, Kramme KW, Dunlap G. Increasing spontaneous play by suppressing self-stimulation in autistic children. Journal of Applied Behavior Analysis. 1974;7:521–528. doi: 10.1901/jaba.1974.7-521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kratochwill TR, Hitchcock J, Horner RH, Levin JR, Odom SL, Rindskopf DM, et al. Single-case designs technical documentation. 2010 Retrieved from What Works Clearinghouse website: http://ies.ed.gov/ncee/wwc/pdf/wwc_scd.pdf.
- Lam KSL, Aman MG. The Repetitive Behavior Scale—revised: Independent validation in individuals with autism spectrum disorders. Journal of Autism and Developmental Disorders. 2007;37:855–866. doi: 10.1007/s10803-006-0213-z. [DOI] [PubMed] [Google Scholar]
- Lam KSL, Holtzclaw TN, Baranek GT, Bodfish JW. Early developmental patterns of repetitive behavior, aberrant behavior, and executive function deficits in autism spectrum disorders. Paper presented at thirty-ninth annual meeting of the Gatlinburg conference. 2005 [Google Scholar]
- Lam KSL, Piven J, Bodfish JW. Evidence for three subtypes of repetitive behavior in autism that differ in familiarity and association with other symptoms. Journal of Child Psychology and Psychiatry. 2008;49:1193–1200. doi: 10.1111/j.1469-7610.2008.01944.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis MH, Bodfish JW. Repetitive behavior disorders in autism. Mental Retardation and Developmental Disabilities Research Reviews. 1998;4:80–89. [Google Scholar]
- Leyfer OT, Folstein S, Bacalman S, Davis NO, Dinh E, Morgan J, et al. Comorbid psychiatric disorders in children with autism: interview development and rates of disorders. Journal of Autism and Developmental Disorders. 2006;36:849–861. doi: 10.1007/s10803-006-0123-0. [DOI] [PubMed] [Google Scholar]
- Lord C, Rutter M, DiLavore PC, Risi S. Autism diagnostic observation schedule. Los Angeles, CA: Western Psychological Services; 2002. [Google Scholar]
- Lounds J, Seltzer MM, Greenberg J, Shattuck P. Transition and change in adolescents and young adults with autism: Longitudinal effects on maternal well-being. American Journal on Mental Retardation. 2007;112:401–417. doi: 10.1352/0895-8017(2007)112[401:TACIAA]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- Machado A. Operant conditioning of behavioral variability using a percentile reinforcement schedule. Journal of the Experimental Analysis of Behavior. 1989;52:155–166. doi: 10.1901/jeab.1989.52-155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mercier C, Mottron L, Belleville S. A psychosocial study on restricted interest in high functions persons with pervasive developmental disorders. Autism. 2000;4:406–425. [Google Scholar]
- Miller N, Neuringer A. Reinforcing variability in adolescents with autism. Journal of Applied Behavior Analysis. 2000;33:151–165. doi: 10.1901/jaba.2000.33-151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mooney EL, Gray KM, Tonge BJ. Early features of autism: Repetitive behaviours [sic] in young children. European Child and Adolescent Psychiatry. 2006;15:12–18. doi: 10.1007/s00787-006-0499-6. [DOI] [PubMed] [Google Scholar]
- Napolitano DA, Smith T, Zarcone JR, Goodkin K, McAdam DB. Increasing response diversity in children with autism. Journal of Applied Behavior Analysis. 2010;43:265–271. doi: 10.1901/jaba.2010.43-265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neuringer A. Can people behave “randomly?” The role of feedback. Journal of Experimental Psychology: General. 1986;115:62–75. [Google Scholar]
- Neuringer A. Reinforced variability in animals and people: Implications for adaptive action. American Psychologist. 2004;59(9):891–906. doi: 10.1037/0003-066X.59.9.891. [DOI] [PubMed] [Google Scholar]
- Newman B, Tuntigian L, Ryan C, Reinecke D. Self-management of a DRO procedure by three students with autism. Behavioral Interventions. 1997;12(3):149–156. [Google Scholar]
- Noldus. The observer Wageningen. The Netherlands: Noldus Information Technology; 1991. [Google Scholar]
- Peters-Scheffer N, Didden R, Green VA, Sigafoos J, Korzilius H, et al. The behavior flexibility rating scale-revised (BFRS-R): Factor analysis, internal consistency, inter-rater and intra-rater reliability, and convergent validity. Research in Developmental Disabilities. 2008;29:398–407. doi: 10.1016/j.ridd.2007.07.004. [DOI] [PubMed] [Google Scholar]
- Piazza CC, Moes DR, Fisher WW. Differential reinforcement of alternative behavior and demand fading in the treatment of escape-maintained destructive behavior. Journal of Applied Behavior Analysis. 1996;29:569–572. doi: 10.1901/jaba.1996.29-569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pierce K, Courchesne E. Evidence for a cerebellar role in reduced exploration and stereotyped behavior in autism. Biological Psychiatry. 2001;49:655–664. doi: 10.1016/s0006-3223(00)01008-8. [DOI] [PubMed] [Google Scholar]
- Piven J, Harper J, Palmer P, Arndt S. Course of behavioral change in autism: A retrospective study high-IQ adolescents and adults. Journal of the American Academy of Child and Adolescent Psychiatry. 1996;35:523–539. doi: 10.1097/00004583-199604000-00019. [DOI] [PubMed] [Google Scholar]
- Pryor KW, Haag R, O’Reilly J. The creative porpoise: Training for novel behavior. Journal of the Experimental Analysis of Behavior. 1969;12:653–661. doi: 10.1901/jeab.1969.12-653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richler J, Bishop S, Kleinke J, Lord C. Restricted and repetitive behaviors in young children with autism spectrum disorders. Journal of Autism and Developmental Disorders. 2007;37:73–85. doi: 10.1007/s10803-006-0332-6. [DOI] [PubMed] [Google Scholar]
- Rutter M. Diagnosis and definitions of childhood autism. Journal of Autism and Childhood Schizophrenia. 1978;8(2):139–161. doi: 10.1007/BF01537863. [DOI] [PubMed] [Google Scholar]
- Schertz HH, Odom SL. Promoting joint attention in toddlers with autism: A parent-mediated developmental model. Journal of Autism and Developmental Disorders. 2007;37:1562. doi: 10.1007/s10803-006-0290-z. [DOI] [PubMed] [Google Scholar]
- Scruggs TE, Mastropieri MA. Summarizing single-subject research: Issues and applications. Behavior Modification. 1998;22:221–242. doi: 10.1177/01454455980223001. [DOI] [PubMed] [Google Scholar]
- Sparrow S, Cicchetti D, Balla D. Vineland Adaptive Behavior Scales, second edition: Survey forms manual. Minneapolis, MN: Pearson, Inc.; 2005. [Google Scholar]
- Strain PS, Kohler FW, Gresham F. Problems in logic and interpretation with quantitative syntheses of single-case research: Mathur and colleagues (1998) as a case in point. Behavioral Disorders. 1998;24(1):74–85. [Google Scholar]
- Szatmari P, Georgiades S, Bryson S, Zwaigenbaum L, Roberts W, Mahoney W, et al. Investigating the structure of the restricted, repetitive behaviours and interests domain of autism. Journal of Child Psychology and Psychiatry. 2006;47(6):582–590. doi: 10.1111/j.1469-7610.2005.01537.x. [DOI] [PubMed] [Google Scholar]
- Turner M. Annotation: Repetitive behavior in autism: A review of psychological research. Journal of Child Psychology and Psychiatry. 1999;40:839–849. [PubMed] [Google Scholar]
- Varni JW, Lovaas OI, Koegel R, Everett N. An analysis of observational learning in autistic and normal children. Journal of Abnormal Child Psychology. 1979;7:31–43. doi: 10.1007/BF00924508. [DOI] [PubMed] [Google Scholar]
- Wink LK, Erickson CA, McDougle CJ. Pharmacologic treatment of behavioral symptoms associated with autism and other pervasive developmental disorders. Current Treatment Options in Neurology. doi: 10.1007/s11940-010-0091-8. (in press). [DOI] [PubMed] [Google Scholar]