Abstract
We have established a novel in vitro co-culture system of human brain endothelial cells (HBEC), Plasmodium falciparum parasitised red blood cells (iRBC) and peripheral blood mononuclear cells (PBMC), in order to simulate the chief pathophysiological lesion in cerebral malaria (CM). This approach has revealed a previously unsuspected pro-inflammatory role of the endothelial cell through potentiating the production of interferon (IFN)-γ by PBMC and concurrent reduction of interleukin (IL)-10. The IFN-γ increased the expression of CXCL10 and intercellular adhesion molecule (ICAM)-1, both of which have been shown to be crucial in the pathogenesis of CM. There was a shift in the ratio of IL-10:IFN-γ protein from >1 to <1 in the presence of HBEC, associated with the pro-inflammatory process in this model. For this to occur, a direct contact between PBMC and HBEC, but not PBMC and iRBC, was necessary. These results support HBEC playing an active role in the pathogenesis of CM. Thus, if these findings reflect the pathogenesis of CM, inhibition of HBEC and PBMC interactions might reduce the occurrence, or improve the prognosis, of the condition.
Introduction
Malaria continues to be one of the most significant infectious diseases in the world, assailing developing countries in terms of both morbidity and mortality. Cerebral malaria (CM) is the most severe manifestation of Plasmodium falciparum malaria infection with an average mortality rate of around 20% even when treated with anti-malarial drugs [1], [2]. Despite decades of study, a detailed understanding of the causative mechanisms in CM has so far not been achieved. Studies of CM can be categorised into four broad types [3]: clinical or genetic studies undertaken in malaria endemic areas, in vivo experiments utilising animal models, histopathological studies on post-mortem materials and in vitro investigations of the interactions between the cell types that contribute to the disease.
Clinical studies have often involved measuring cytokines or other biomarkers in the serum/plasma [4], [5], [6] and cerebrospinal fluid (CSF) from malaria patients [7]. They also include the study of post-mortem material (brains) from patients who succumbed to the disease. Another aspect of clinical work is investigation of the neurological sequelae in survivors of CM. Experimental in vivo studies, on the other hand, involve the use of animal models to study CM. Even though differences between human and murine CM have been described [8], [9], the animal model has proven to be versatile and revealing, in particular with gene ablation studies, where inferences can be made by comparing gene knockout mice to wild type mice in their response towards the disease. An important finding originating from this approach is that the pro-inflammatory cytokine interferon-γ (IFN-γ) is crucial for the pathogenesis of experimental CM [10], [11], [12].
In vitro cultures also have been performed, utilising selected cells observed in the CM lesion, such as brain endothelial cells, peripheral blood mononuclear cells, platelets and parasitised red blood cells [13]. This allows the study of interactions between different cell types. These studies largely have been limited to bipartite cultures, which do not fully represent the cellular components of the CM lesion. Some studies that have used human brain endothelial cells, platelets and iRBCs in vitro have revealed roles for platelets in the pathogenesis of CM in tripartite cultures [14], [15], [16], [17], [18]. However, PBMCs have yet to be included in a tripartite culture system to model the lesion in CM.
Hence, for this study, we established a novel tripartite culture, using human PBMCs, iRBCs and HBEC, in order to simulate the vascular lesion of CM. We hypothesised that PBMCs, along with HBEC, would interact with the iRBCs, leading to up-regulation of the expression of inflammatory genes.
Results
1. Endothelial cells (HBEC-5i) enhance IFN-γ production, but decrease that of IL-10, in PBMC/ 3D7 iRBC co-cultures
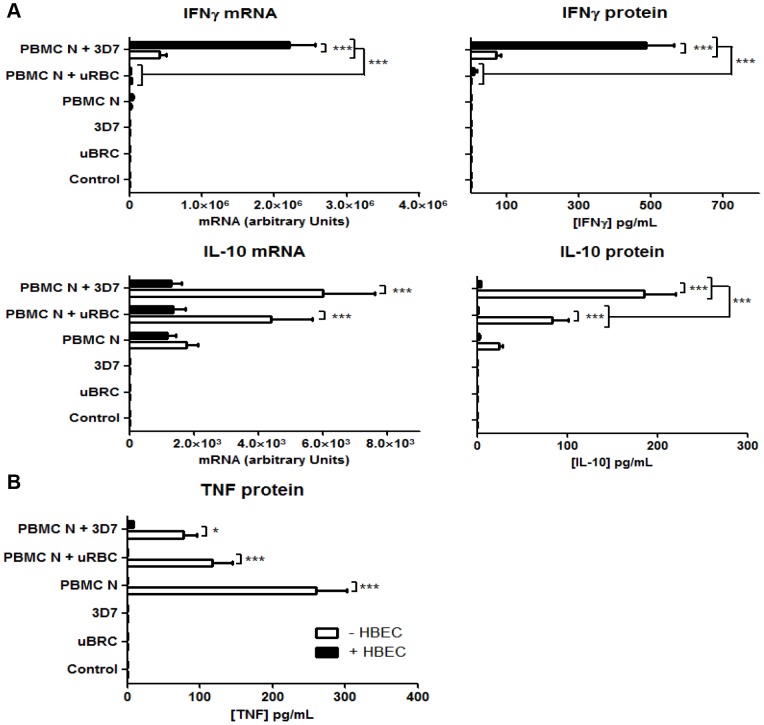
In nine separate experiments with the novel tripartite cultures of HBEC, PBMCs (from donor N) and iRBC (strain 3D7), IFN-γ mRNA expression was significantly enhanced when endothelial cells were present (PBMC N + 3D7 + HBEC, Figure 1A). IFN-γ protein expression echoed that of mRNA, with a 6.8-fold enhancement in cultures with HBEC-5i compared to PBMC + iRBC without endothelial cells (Figure 1A). This effect was parasite-dependent, since significant increases of IFN-γ mRNA and protein were not observed in the corresponding controls of HBEC + PBMC, PBMC only, HBEC + PBMC + uRBC (uRBC = uninfected red blood cells) and PBMC + uRBC. The results suggest that HBEC amplified the induction of IFN-γ expression by PBMC in this co-culture arrangement.
Figure 1. Effect of endothelial cells on cytokine production in PBMC/iRBC co-cultures.
A. Significant alterations in IFN-γ and IL-10 (mRNA and protein) production in PBMC/iRBC (P. falciparum strain 3D7) co-culture in the presence of endothelial cells (HBEC-5i). B. TNF protein production was significantly decreased in the presence of HBEC-5i. uRBC = unparasitised red blood cells. Control = no PBMC, uRBC or iRBC. Columns and horizontal bars represent means ± SEM of nine experiments. Two-way ANOVA showed significant differences among the groups (*p<0.05; ***p<0.001), identified using the Bonferroni post hoc test.
The expression of an anti-inflammatory cytokine, IL-10, in the tripartite culture system was reduced. Production of this cytokine, in terms of protein (Figure 1A), but not mRNA, was dependent on the presence of parasitised red blood cells. Both IL-10 mRNA and protein, however, were significantly suppressed in the presence of endothelial cells, again implying that HBEC exert an overall pro-inflammatory effect in this system.
Expression of the cytokine TNF, like IL-10, was significantly reduced in the presence of HBEC (Figure 1B). This was unexpected, given that TNF expression can be regulated by IFN-γ.
2. Heterogeneity between PBMC donors, but not parasite strains, in IFNγ production in co-culture
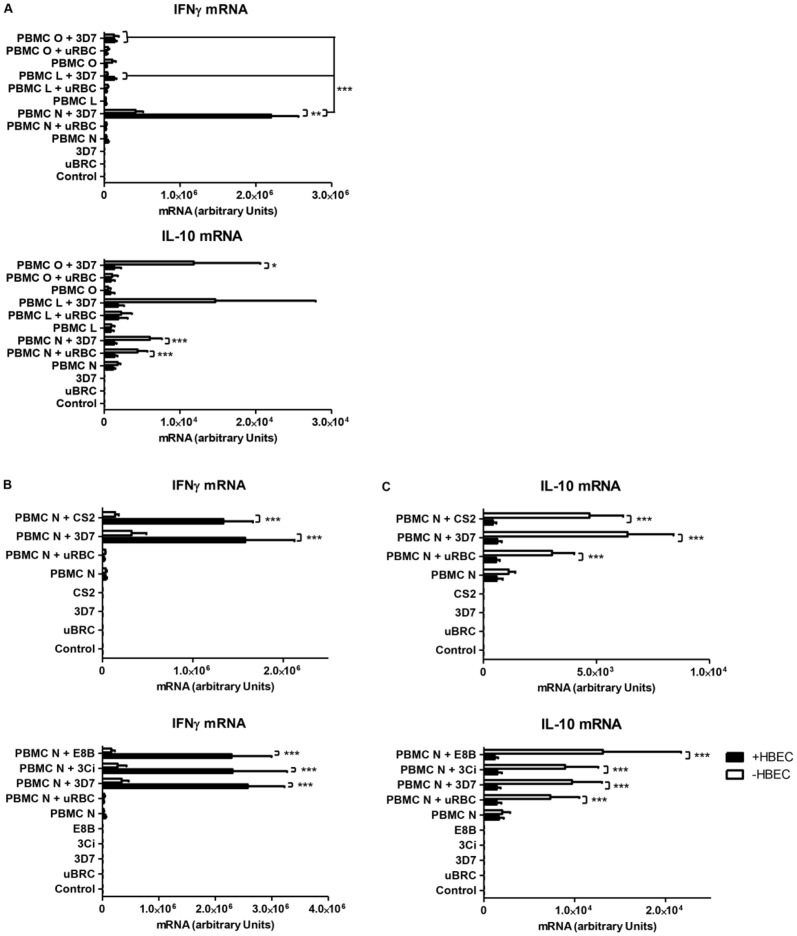
Following the assessment of the cytokine responses of the initial donor PBMC (designated “PBMC N”), two further PBMC donors (designated PBMC L and O) were tested for their capacity to induce IFN-γ in the tripartite cultures. Heterogeneity in the IFN-γ response between donors in bipartite incubations of PBMC and iRBC has been reported by others [19], [20], [21], [22]. PBMC L and O were selected from among 6 donors for their low, or lack of, reactivity towards 3D7 iRBC in a preliminary experiment in terms of IFN-γ mRNA (data not shown). As hypothesised, heterogeneity in the IFN-γ response was seen, with PBMC L and PBMC O showing initial lower induction of IFN-γ mRNA in the tripartite culture compared to PBMC N. In contrast, there was no difference in the pattern of IL-10 mRNA expression between the three donors (Figure 2A).
Figure 2. Influence of PBMC origin and malaria parasite strain on cytokine production in tripartite cultures.
A. Differences in the pattern of IFN-γ, but not IL-10, mRNA production between donor PBMCs (L, N and O) in tripartite culture. B: No difference in the pattern of IFN-γ expression in response to P. falciparum strains 3D7, CS2, 3Ci and E8B in the tripartite culture. C: Similar pattern of IL-10 expression with several P. falciparum strains in the tripartite culture. uRBC = unparasitised red blood cells. Control = no PBMC, uRBC or iRBC. Columns and horizontal bars represent means ± SEM of three to nine experiments. Two-way ANOVA showed significant differences among the groups (*p<0.05; **p<0.01; ***p<0.001), using the Bonferroni post hoc test.
Different laboratory maintained strains of P. falciparum (3D7, CS2, 3Ci and E8B) were then tested for their ability to elicit IFN-γ and IL-10 production in the tripartite culture system. No heterogeneity between the strains was observed in the context of the tripartite culture (Figures 2B and 2C), as the patterns of expression of IFN-γ and IL-10 mRNA were similar to those in Figure 1A.
3. ICAM-1 and CXCL10 expression is IFN-γ dependent
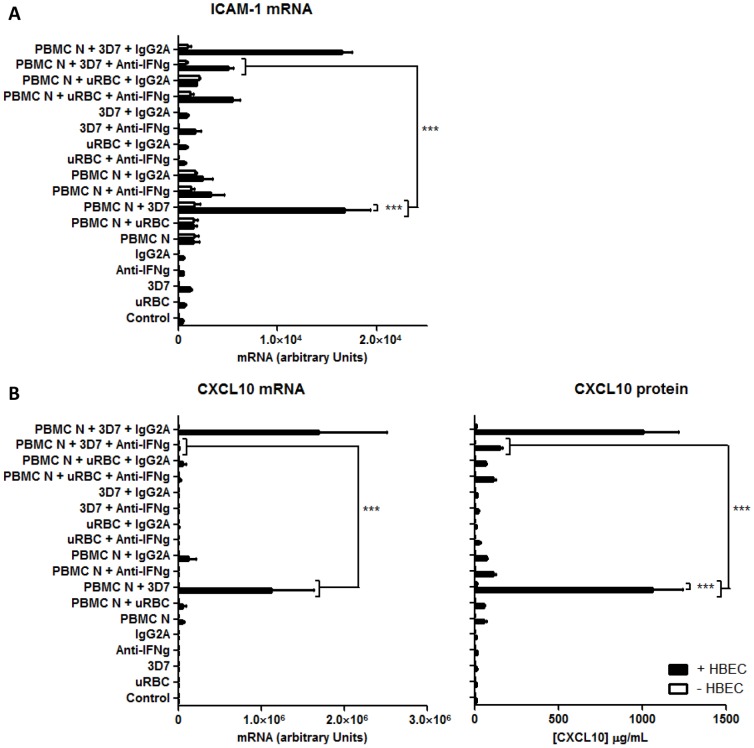
To demonstrate the functional capacity of the IFN-γ produced by the tripartite culture, the expression of two of its downstream effectors, ICAM-1 and CXCL10, was studied. Both of these are considered to be important in the pathogenesis of CM. ICAM-1 is acting as a major adhesion molecule for iRBC [23], [24] as well as leukocytes, possibly via LFA-1 [25], [26]. CXCL10 functions as a chemokine and deletion of its receptor, CXCR3, is protective in experimental cerebral malaria [27]. We employed an antibody that neutralises IFN-γ in order to determine whether production of these downstream effectors was regulated by IFN-γ in the tripartite culture.
As predicted, ICAM-1 mRNA induction was enhanced in the tripartite arrangement. This mRNA expression was reduced by 70% following the addition of IFN-γ neutralising antibody (Figure 3A), suggesting that the ICAM-1 induction is IFN-γ dependent. CXCL10 expression in PBMC induced by 3D7 iRBCs was potentiated in the presence of HBEC, with 500- and 91-fold increases of mRNA and protein respectively compared to observations in the absence of endothelial cells (Figure 3B). The addition of IFN-γ neutralising antibody abrogated CXCL10 expression. In contrast, addition of isotype-matched control antibodies did not affect ICAM-1 or CXCL10 production (Figure 3A, B).
Figure 3. HBEC-dependent induction of ICAM-1 and CXCL10 in tripartite co-cultures is inhibited by IFN-γ neutralising antibody.
A. IFN-γ neutralising antibody inhibits ICAM-1 mRNA induction in tripartite cultures. B. IFN-γ neutralising antibody inhibits expression of CXCL10 mRNA and protein in the tripartite cultures. uRBC = unparasitised red blood cells. Control = no PBMC, uRBC or iRBC. Columns and horizontal bars represent means ± SEM of three experiments. Two-way ANOVA showed that the values contained significant differences among the groups (***p<0.001), using ANOVA and the Bonferroni post hoc test.
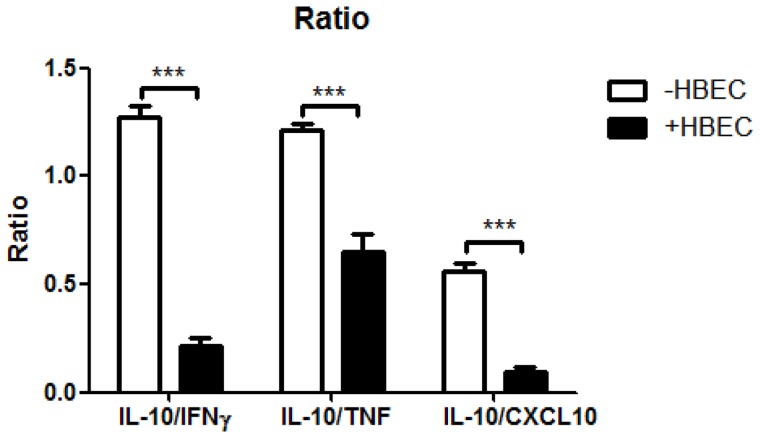
4. IL-10:pro-inflammatory cytokine ratios are decreased in the presence of HBEC
It has been suggested that a reliable predictor of malaria severity is comparison of the ratio between TNF and IL-10 protein levels in the plasma [28], [29]. A ratio of IL-10:TNF of less than 1 correlated with severe malaria whereas a ratio of more than 1 was associated with uncomplicated malaria [29]. In our study, in the culture supernates with HBEC, we observed significant decreases, from >1 to <1, in the ratio of IL-10:TNF as well as IL-10:IFN-γ proteins (Figure 4). In addition, although the ratio in the absence of HBEC is already lower than 1, we found a similar significant reduction of the IL-10: CXCL10 ratio when HBEC were added into the system.
Figure 4. Ratio of IL-10:IFN-γ, IL-10:TNF and IL-10:CXCL10 protein in the presence and absence of HBEC.
Columns and vertical bars represent means ± SEM of three experiments. Statistical significance (***p<0.001) was assessed using ANOVA and the Bonferroni post hoc test.
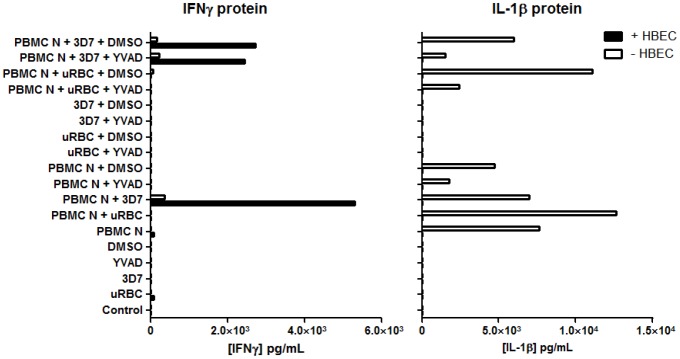
5. IFN-γ enhancement is caspase-1 independent
To study the upstream events leading to the expression of IFN-γ in this co-culture system, the potential involvement of cytokines such as IL-1β, IL-12 and IL-18 was explored. All these cytokines provide co-stimulatory signals that elicit the expression of IFN-γ from immune cells, including NK cells [30]. To determine whether IL-18 and IL-1β are crucial for IFN-γ expression in this tripartite culture model, YVAD, an inhibitor of caspase-1, was used to inhibit caspase-1-mediated activation of pro-IL-1β and pro-IL-18 to their active forms [31]. YVAD did not affect IFN-γ protein level in the tripartite cultures (PBMC + HBEC + iRBC +YVAD) (Figure 5) when compared to its DMSO control (PBMC + HBEC + iRBC + DMSO). In addition to IFN-γ, IL-1β production was analysed to verify the activity of YVAD in this system. Addition of YVAD did indeed reduce the level of IL-1β in culture supernates (Figure 5). These results imply that IFN-γ production is independent of caspase-1 activity and, hence, IL-18 in this co-culture system. We were not able to quantify IL-18, due to technical limitations of the FlowCytomix multiple analyte detection system employed. IL-12 on the other hand, was undetectable in the supernates in our model, and hence was not pursued further (data not shown).
Figure 5. Effect of caspase-1 inhibition on IFN-γ and IL-1β production in co-cultures of PBMC and iRBC.
YVAD did not affect IFN-γ production but did inhibit that of IL-1β. uRBC = unparasitised red blood cells. Control = no PBMC, uRBC or iRBC. YVAD (50 µmol/L), a caspase-1 inhibitor, was pre-incubated with PBMC and HBEC for 30 min prior to addition of the iRBCs. At 24 h, supernates were analysed for IFN-γ and IL-1β. Columns represent values from a single experiment.
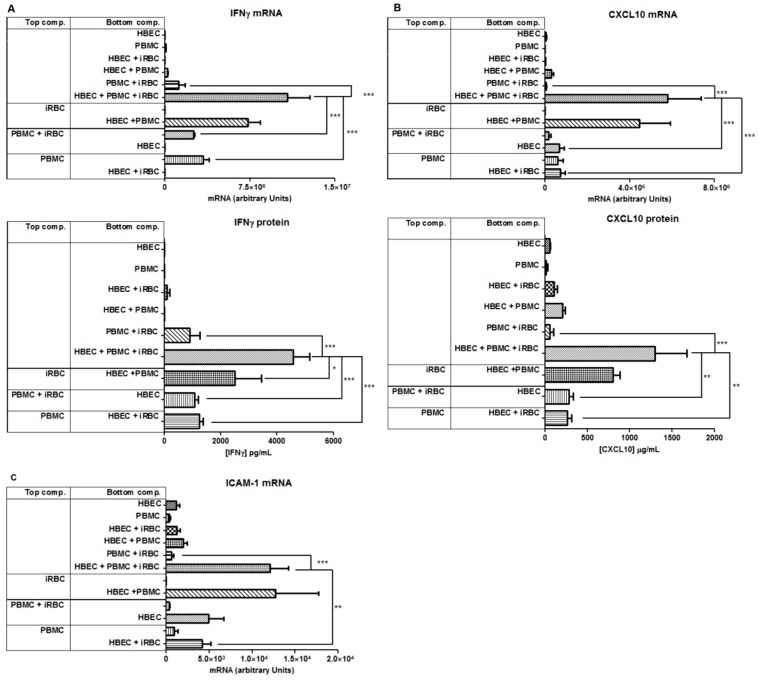
6. Enhancement of IFN-γ production by HBEC is contact dependent
As we did not find evidence for IFN-γ expression being cytokine mediated, we examined the contact dependency between the different cell types in the induction of IFN-γ in the tripartite culture, using transwell inserts (pore size of 0.4 µm). HBEC were always situated in the lower chamber. Preventing physical contact of PBMCs with other cellular components, by isolating them in the upper chamber, reduced the amount of IFN-γ mRNA by 70%, compared to control (p<0.001, Fig. 6A). This was also observed when both iRBCs and PBMCs were separated in the upper chamber (Figure 6A). The separation of the iRBCs in the upper chamber, and co-culture of PBMC and HBEC in the lower chamber, did not significantly reduce IFN-γ mRNA expression. These data imply that P. falciparum stimulates IFN-γ production in the tripartite culture in a contact independent fashion, likely through released antigens or other soluble factors. This same pattern of expression was observed at the protein level (Figure 6A), with one exception, as separation of the iRBC from the HBEC and PBMC resulted in a modest but significant reduction in IFN-γ expression, by about 40% (Figure 6A). These results indicate that PBMCs are required to be in close contact with HBEC in order to evoke maximal amounts of IFN-γ. Importantly, the data confirm that PBMCs, rather than HBEC, are the source of IFN-γ in this system.
Figure 6. Effect on immunomodulator expression of the physical separation of cellular components of the tripartite system.
The enhancement of IFN-γ (A), CXCL10 (B) and ICAM-1 (C) production was perturbed when PBMC were physically separated from HBEC. iRBCs, iRBCs + PBMCs or PBMCs were isolated in the upper chamber of the transwell insert, whereas HBEC were consistently retained in the bottom chamber. Columns and horizontal bars represent means ± SEM of three experiments. One way ANOVA showed significant differences among the groups (*p<0.05; **p<0.01; ***p<0.001), using Tukey's post hoc test.
Similar to the effects on IFN-γ, isolation of PBMC from the other culture components considerably reduced both CXCL10 and ICAM-1 levels. If the upper chamber contained either PBMC alone, or PBMC and iRBC together, the amount of CXCL10 mRNA and protein was reduced (Figure 6B), suggesting that contact between PBMC and HBEC is essential to generate the maximal amounts of CXCL10 in the presence of iRBCs. These data also suggest that the source of CXCL10 mRNA may be both PBMC and HBEC, as both cell types expressed similar levels even when separated (Figure 6B). In parallel to the patterns of expression seen with CXCL10, ICAM-1 mRNA was significantly diminished by 70% when PBMC were separated in the upper chamber compared to when all components were cultured together in the lower chamber (Figure 6C). Again, isolation of iRBCs in the upper chamber had no effect on ICAM-1 mRNA production. Culture of both iRBCs and PBMCs together in the upper chamber also resulted in an apparent, but not significant, reduction of ICAM-1 mRNA. Finally, the induction of ICAM-1 mRNA was shown to be occurring mainly in HBEC, rather than PBMCs, as demonstrated in Figure 6C when HBEC were separated from PBMCs by the transwell inserts. Overall, these data support a model where HBEC and PBMCs require close contact in order to potentiate IFN-γ, and subsequently CXCL10 and ICAM-1, expression.
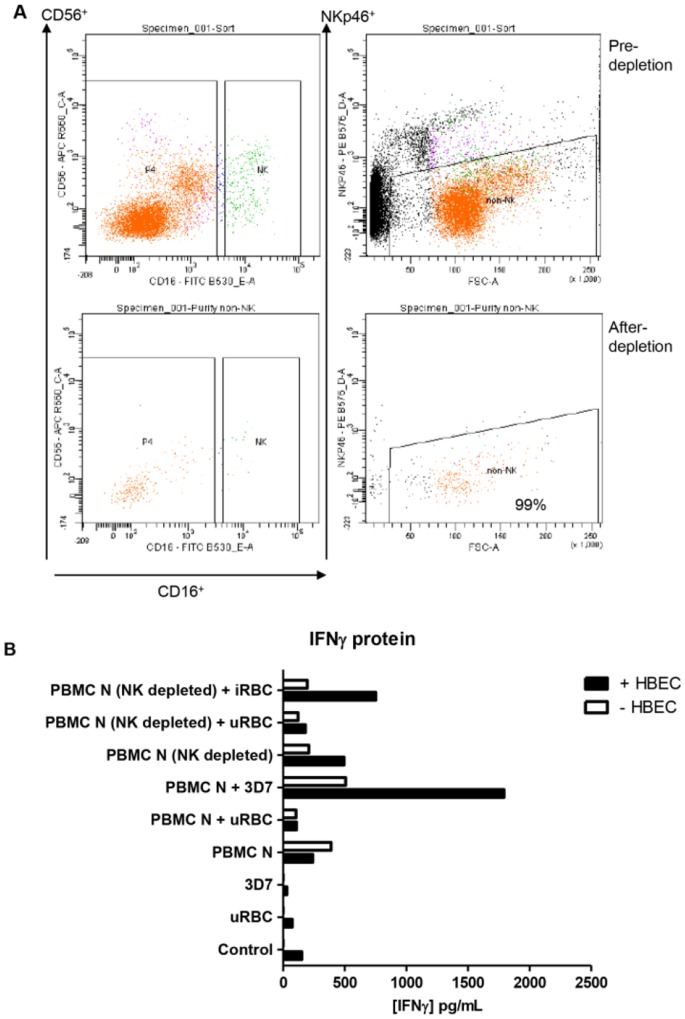
7. IFN-γ enhancement is substantially dependent on NK cells
To narrow down the possible ligands and receptors responsible for the phenomenon of endothelial cell enhancement of IFN-γ production, we used a cell-sorting approach to deplete selected subsets in the PBMC stabilates prior to our standard co-culture experiments. As the literature has described a range of cellular sources (T, NK, NKT and γδ T cells) as being responsible for IFN-γ production in the response of PBMC to parasitised red blood cells in bipartite cultures [32], [33], [34], an ideal approach would have involved depletion of all subsets in turn. However, due to limited stocks of the relevant PBMC, we focused on NK cells, as these have been the most widely-reported source. Using the NK specific markers CD16+, CD56+ and NKp46+, and the gating strategy shown in Figure 7A, PBMC were depleted of NK cells (>99% purity) and subsequently cultured with iRBC and HBEC. In two independent experiments, IFN-γ protein production was greatly reduced in NK-depleted PBMC cultures compared to the corresponding co-culture from which NK cells were not depleted, PBMC N + 3D7 + HBEC (Figure 7B). These data indicate that NK cells were involved in the production of IFN-γ in the tripartite culture.
Figure 7. Effect of NK depletion on IFN-γ production in tripartite cultures.
A. NK cell depletion strategy. B. IFN-γ protein production was decreased by NK cell depletion. uRBC = unparasitised red blood cells. Control = no PBMC, uRBC or iRBC. “PBMC N (NK depleted)” co-cultures contained PBMC that had been depleted of 99% NK cells stained with CD16, CD56 and NKp46 prior. “PBMC N” refers to co-cultures in which PBMC had not been depleted of NK cells. Co-cultures were 24 h, following which supernates were harvested and analysed for IFNγ. Columns represent means of two separate experiments.
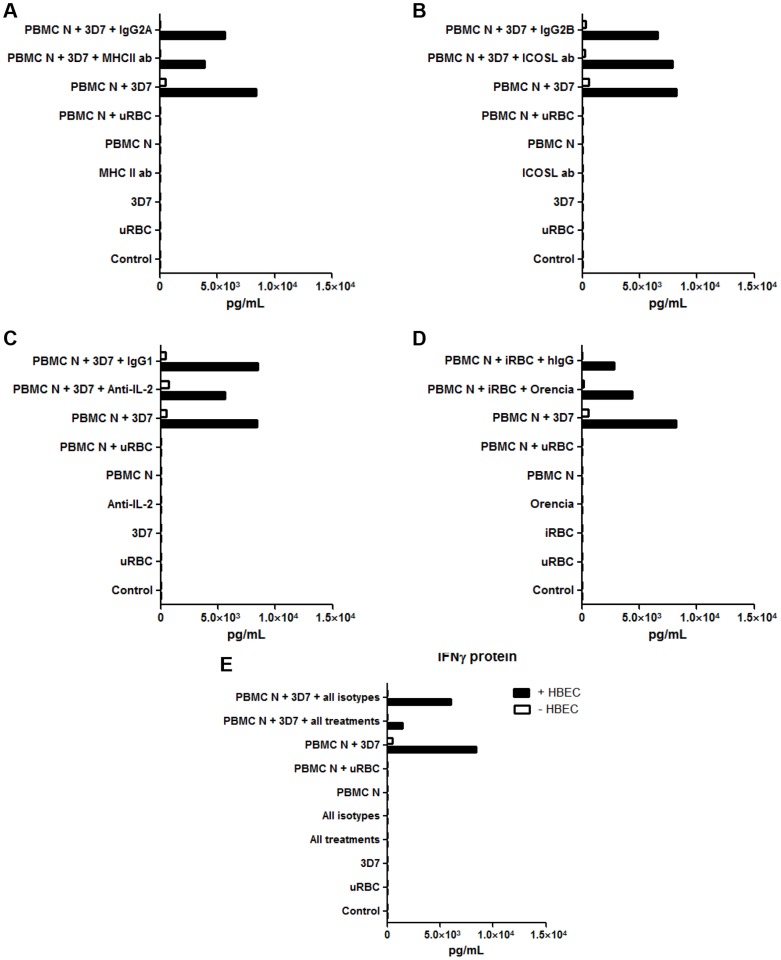
8. IFN-γ production is co-stimulated by human brain endothelial cells, potentially via MHCII, ICOSL, IL-2 and B7-1/B7-2
Having shown that NK cells were partly responsible for the increase of IFN-γ protein in the tripartite culture, we next explored the possible involvement of several molecules in this system. Those studied were the major histocompatibility complex II (MHC II), Inducible costimulator molecule ligand (ICOSL), interleukin-2 (IL-2) and B7-1/B7-2. The first three were tested by the addition to co-cultures of neutralising antibodies. B7-1/B7-2 actions were blocked with Orencia (Abatacept), a fusion protein of the Fc region of IgG1 and the extracellular domain of CTLA-4. Pooled data from two independent experiments showed that MHCII, ICOSL, IL-2 and B7-1/B7-2 inhibition individually did not affect IFNγ expression in tripartite cultures, compared to their respective isotype controls (Figure 8A-D). However, when administered together, the treatments decreased IFN-γ expression to almost control levels in two separate experiments (Figure 8E), suggesting that two or more of the four molecules may act in concert to stimulate IFN-γ expression.
Figure 8. Effects of MHC II, ICOSL, IL-2 neutralisation on IFN-γ production in the tripartite cultures.
Individually, anti-MHC II (A), anti-ICOSL (B), anti-IL-2 (C) and Orencia (D) did not affect IFN-γ production. However, when all treatments were combined they did reduce the endothelial cell-mediated enhancement of IFN-γ (E). uRBC = unparasitised red blood cells. Control = no PBMC, uRBC or iRBC. MHC II, ICOSL and IL-2 neutralising antibodies, and Orencia, were incubated with the tripartite cultures for 24 h. Supernates were then harvested and analysed for IFN-γ. Columns represent means of two separate experiments.
Discussion
The mechanisms leading to the pathology seen in CM are still the topic of considerable debate. This study presents, for the first time, a novel tripartite culture system consisting of three major cell types involved in the lesion of CM: brain endothelial cells, iRBC and PBMC. We wished to determine whether endothelial cells would modulate the production of immune mediators by PBMC stimulated by iRBC. This might throw light on the interactions of these three cell types at a critical location, the brain microvasculature. The primary focus in this model was on the local expression of IFN-γ, a pro-inflammatory cytokine that is generally accepted to be crucial in driving the pathogenesis of CM [13], [35], [36], [37] as well as being central to anti-malarial immunity [38]. Clinical studies have described a correlation between IFN-γ levels and the occurrence of CM in humans [39], [40], [41]. Based on animal studies, this IFN-γ appears to derive from immune cells that have accumulated within the brain vasculature prior to the terminal phases of pathology. Previously, innate production of IFN-γ by PBMCs in response to iRBC has been reported by a number of groups, although this has been limited to bipartite cultures consisting of PBMC and iRBC. More importantly, design and interpretation of these studies has focused primarily on understanding the cellular and molecular pathways involved in IFN-γ production, rather than any effects on pathology. Taken together these studies suggest that production of IFN-γ by leukocytes sequestered within brain microvessels, and therefore in close contact with endothelial cells, is important for CM pathology.
Since suitable human experimental systems for investigating the role of IFN-γ in the pathogenesis of CM are not available, such investigations are limited to animal models. In animal studies using P. berghei ANKA, IFN-γ has been shown to be critical for the development of experimental CM (ECM). Neutralisation of IFN-γ in mice infected with P. berghei ANKA protects against the manifestation of ECM [42], and mice that are deficient in IFN-γ were also resistant to ECM [12], [43], [44]. The mechanisms by which IFN-γ drives pathology in this model are likely to be multiple. Firstly, tissue sequestration of parasites, including to the brain, is mediated by IFN-γ [45]. More relevant to the current study, IFN-γ-induced chemokines, in particular CXCL10, are crucial for the migration of leukocytes to the brain [11], [27].
Here, in the tripartite culture model, our results showed a novel role of endothelial cells in potentiating IFN-γ production by PBMC in response to iRBC, and subsequent IFNγ-dependent processes that have been implicated in CM. It should be noted that we studied only a 24 hour co-incubation period, and it is possible that the results would have been different at other time points. An important finding of our co-culture system is that expression of both CXCL10 and ICAM-1 mRNA was enhanced in the presence of endothelial cells in an IFN-γ- and contact-dependent manner. CXCL10, also known as IP-10 (Interferon gamma induced protein 10), signals through CXCR3 and is a key chemokine involved in T helper and T cytotoxic cell migration [46], [47]. The relevance of CXCL10 to the pathogenesis of CM is highlighted by studies showing that CXCL10 is markedly increased in the plasma of fatal CM cases as compared to other non-CM cases [48]. Furthermore, mice deficient in CXCL10 or CXCR3 are partially resistant to CM [11], [27], [49], [50]. ICAM-1 is an adhesion molecule that has been implicated in the development of murine CM. ICAM-1 is a host receptor for the PfEMP1 molecule of iRBCs [51], so an increase in ICAM-1 expression is likely to lead to sequestration of iRBCs as well as the recruitment of more PBMCs, potentially leading to CM. This was supported recently by human studies in which ICAM-1 binding by iRBCs was associated with CM [23]. Although TNF has been considered the primary inducer of ICAM-1 in CM [52], [53], there are also reports that suggest that IFNγ provides a stronger signal for induction of this molecule in vitro [54], [55]. Importantly, in our study neutralisation of IFN-γ reduced expression of ICAM-1 and CXCL10 mRNA to almost control levels (Figure 3), which further supports a role for IFN-γ in the pathogenesis of CM.
The results shown here were obtained with PBMC from a naive donor that reacted strongly to iRBC in terms of IFN-γ induction. Such heterogeneity in IFN-γ responsiveness is not surprising, considering that only a very small fraction of P. falciparum-infected patients develop CM. Indeed, it is well-established that PBMC from malaria-naïve donors show a very wide range of responsiveness to iRBC in terms of IFN-γ production [41], [56], [57]. Furthermore, since a range of P. falciparum strains induced similar levels of IFN-γ in tripartite co-culture, it is likely that the strains used in this study may share a common factor that is crucial for the induction of IFN-γ and that host, rather than parasite, factors may be the dominant contributors to CM pathology.
In contrast to the clearly pro-pathogenic role of IFN-γ in CM, the influence of IL-10 and TNF on disease is unclear, but IL-10 levels in particular have been argued to be a prognostic indicator of protection from pathology. The actual role of IL-10 is debatable, as comparisons of plasma samples from children afflicted with mild and severe forms of malaria showed that IL-10 levels were significantly lower in patients with the more severe forms of malaria [58], [59], though it must be noted that another study did not support this finding [60]. Any protective effect of IL-10 is presumably a result of the anti-inflammatory activity of this cytokine [61]. TNF was initially deemed important in CM [4], [62], but abrogation of the TNF gene in the murine model of CM did not confer resistance to CM [63]. Nevertheless, the IL-10:TNF ratio in patient plasma has been shown to correlate predictively with severe disease [29]. In our tripartite co-culture system, inclusion of endothelial cells lead to diminished IL-10 production, which when coupled with the enhanced IFN-γ production, led to a dramatic inversion in the IL-10:IFN-γ ratio in the presence of HBEC. Similar, but less pronounced, changes in the IL-10:TNF and IL-10:CXCL10 ratios were also seen in our culture system, which again is consistent with a pro-pathogenic function of endothelial cells.
The pro-inflammatory activity of the endothelial cells was mediated through cell-cell contact rather than soluble mediators. When PBMCs were separated from the tripartite cultures in transwells (Figure 6A, 6B and 6C), IFN-γ mRNA and protein, as well as CXCL10 and ICAM mRNA levels, were reduced. Taken together, these data indicate that in the tripartite cultures, up regulation of IFN-γ, ICAM-1 and CXCL10 induction requires contact-dependent signals between PBMC and HBEC. Interestingly, the separation of the iRBCs from other culture components did not significantly reduce the amount of IFN-γ mRNA, suggesting that neither cytoadherence of iRBC to HBEC nor direct effects of released merozoites are important in this mechanism.
The source of IFN-γ in P. falciparum co-culture systems has been a matter of intense debate, with NK cells [21], [22], [26], [57], [64], [65], CD8+ T cells [34] and γδ T cells/ NKT cells [33] being argued to be the dominant source. Of the likely parasite factors involved in immune stimulation, it has been shown that glycosylphosphatidylinositol [66], hemozoins [67], [68], [69], uric acid [70] as well as microparticles [71] are capable of eliciting pro-inflammatory activity such as expression of IFN-γ and TNF. To determine the source of IFN-γ in our studies, we focused on NK cells as the majority of published studies support them being the major producers of this cytokine. NK depletion experiments (Figure 7A and 7B) showed that NK-depleted PBMC produced lower levels of IFN-γ protein in the tripartite culture system, when compared to NK replete PMBC cultures. Nevertheless, PBMCs that had been depleted of NK cells still produced residual amounts of IFN-γ even in the absence of other culture components. One possible explanation for this apparent heterogeneity of cellular source is that IFN-γ production by various cell types may be time-dependent, with 24 hours culture (the time point used in the present study) marking a transition from NK to CD4 T cells as the dominant source [34].
As far as interactions between endothelial cells and NK cells are concerned, potential co-stimulatory molecules on endothelial cells have been extensively reviewed [72] and these include ICOSL (inducible co-stimulator ligand) and PD-1 L (programmed death 1 ligand). On the other hand, NK cells possess a variety of receptors such as CD28, a ligand of B7-1/B7-2 molecules [73], which is expressed by endothelial cells as well as monocytes and dendritic cells. Another molecule of interest is MHC II, which, apart from being involved in antigen presentation, has also been described as being capable of synergising with Toll-like receptors in mounting innate immune responses [81], [82]. Furthermore, higher inducibility of MHC II expression in murine brain endothelial cells is associated with genetic susceptibility to CM in one model of ECM [74]. Even though we did not find any significant reduction in IFN-γ protein in the tripartite cultures with single additions of MHC II, ICOSL, IL-2 neutralising antibodies and Orencia, a B7-1/B7-2 antagonist, when these were added together IFN-γ induction was largely abolished (Figure 8E). This evidenced the potential of these molecules to act in concert for the induction of IFN-γ by HBEC in the presence of both iRBCs and PBMC. Our findings so far suggest that endothelial cells provide co-stimulatory signals in this co-culture system.
Conclusion
We describe for the first time a novel tripartite culture using HBEC, PBMC and iRBC. In this co-culture system, HBEC actively participate in the pro-inflammatory response by enhancing IFN-γ production, which in turn leads to induction of a chemokine (CXCL10) and a cell surface receptor (ICAM-1) that have been implicated in CM pathology. These results indicate a need to further investigate the role of endothelial cells in end stage CM pathology, and suggest that therapeutic interventions that target endothelial cell/leukocyte interactions may be possible.
Materials and Methods
Ethics statement
Human buffy coat preparations and outdated erythrocytes were purchased from the Red Cross Blood Service, Sydney. Donors gave written informed consent. The studies were approved by the University of Sydney Human Ethics Committee.
P. falciparum culture
P. falciparum cultures were maintained using methods modified from those described by Trager and Jensen [75]. In brief, parasites were grown in group O+ human erythrocytes in Malaria Complete Medium (MCM) consisting of RPMI 1640 fortified with 2 mmol/L glutamine (Thermo Fisher Scientific, USA), glucose (10 mmol/L, Amresco, USA), 4-(2-hydroxyethyl)-1-piperazineethanesulfonic acid (HEPES) (25 mmol/L, Research Organics, USA), sodium bicarbonate (32 mmol/L, Research Organics, USA) and albumax II (0.5%, w/v, Life Technologies, USA). Cultures were contained in sealed T25 or T75 flasks (Corning, USA) at 5% hematocrit and flushed with a gas mix of 5% O2, 5% CO2, and 90% N2 (Coregas, Yennora, New South Wales). The P. falciparum lines used in this study were 3D7 [76], CS2 [77], 3Ci [78] and E8B [79]. HBEC and the parasite strains used were tested to be mycoplasma-free throughout the experimentation by the means of a PCR detection kit (Minerva BioLabs, Germany). For co-culture experiments, schizonts and mature trophozoites were enriched via magnetic separation [80] with an AutoMACS® (Miltenyi Biotec, Germany). The studies were performed with these late stages of the cycle because they are the predominant forms that sequester in the brain microcirculation in CM [81]
Human brain endothelial cell culture
The human brain endothelial cell line 5i (HBEC) [16] was cultured in 25 cm2 (T25) or 75 cm2 (T75) flasks (NUNC, Denmark, pre-coated overnight with 0.1% gelatine (w/v in distilled water, Sigma-Aldrich, USA) using Dulbecco's Modified Eagle Media: Nutrient Mixture F-12 (Thermo Fisher Scientific, USA) enriched with 10% (v/v) FBS and 30 µg/mL Gentamycin (Life Technologies, USA) at 37°C with 5% CO2 in a humidified atmosphere.
Peripheral blood mononuclear cell preparation
PBMCs were isolated by density gradient centrifugation from buffy coats from naïve donors obtained from the Australian Red Cross Blood Service. The buffy coat layer was first overlaid carefully onto 15 mL of Ficoll Paque Plus (GE Healthcare, USA) and centrifuged at 400 G with the brake off at room temperature for 20 min. The PBMC band was then removed and washed 3 times with RPMI1640 at 450 G for 10 min at room temperature. After washing, PBMCs were mixed with freezing medium comprised of RPMI 1640, 20% (v/v) FBS and 10% (v/v) dimethylsulfoxide (DMSO), before the freezing of aliquots in liquid nitrogen.
Co-culture conditions
Co-culture experiments that incorporated P. falciparum-infected red blood cells (iRBC), peripheral blood mononuclear cells (PBMCs) and human brain endothelial cells 5i (HBEC) were performed in flat bottom microplates (Nunc, Denmark) under normoxic conditions. HBEC were seeded at 2×104 per well into a 0.1% (w/v) gelatin pre-coated microplate and left to achieve confluence. The ratios of the respective cell types were chosen to be 2∶5∶100 for HBEC: PBMC: iRBC.[20] [82]. Different cell types were added simultaneously. At the end of the 24 h incubation, the co-culture experiment was terminated by centrifuging the plate at room temperature, 300 G for 3 min. The supernatant was removed for analysis of soluble products, while cells were subjected to RNA isolation by magnetic beads, followed by reverse transcription and real time PCR as described below.
RNA isolation, reverse transcription and real time PCR
RNA was extracted using the MagMAX 96 Blood RNA isolation Kit (Life Technologies, USA) in accordance with the manufacturer's guidelines. Isolated RNA was primed with random hexamers (GeneWorks, Australia) and reverse transcribed to cDNA using Bioscript™, (Bioline, UK). Real-time PCR analyses were carried out using the Corbett Rotor-Gene 3000 (Qiagen, Germany) in KAPA SYBR® FAST Universal 1×strength qPCR Master Mix (KapaBiosystems, USA) and 100 nmol/L of each primer (see Table 1 for details). Thermal cycling conditions for the real-time PCR were: 95°C for 2 min, followed by 45 cycles of 95°C for 15 sec and 60°C for 45 sec. The purity of the PCR products was assessed by melting curve analysis and the expression of the target genes was measured using a standard curve.
Table 1. Primer sequences used.
| Forward | Reverse | |
| IFN-γ | TGACCAGAGCATCCAAAAGA | TTTCGCTTCCCTGTTTTAGC |
| IL-10 | AGAACAGCTGCACCCACT TC | GCATCACCTCCTCCAGGTAA |
| CXCL10 | AACTGTACGCTGTACCTGCATCAGC | ACACGTGGACAAAATTGGCTTGCAG |
| ICAM-1 | TTCACAATGACACTCAGCGGTC | AGTGCAAGCTCCCAGTGAAATG |
Cytometric bead array
IFN-γ, IL-10, CXCL10 and TNF were measured using human cytometric bead array flex sets (BD Biosciences, USA) according to the manufacturer's instructions, with the exception that all sample/reagent volumes were decreased 5-fold. Samples were run on an FC500 (Beckman Coulter, USA), and data were analysed using FlowJo (Treestar, OR) and Prism (Graphpad, CA) software. Limits of detection for the cytometric bead array are 3.7 pg/mL for IFN-γ and 0.5 pg/mL for CXCL10, as stated in the manufacturer's instructions.
Interventions using neutralisation antibodies and inhibitors
Neutralising antibodies for IFN-γ (Clone 25718, R&D systems, USA), MHCII (Clone TU36, Becton Dickinson, USA), ICOSL (Clone 136726, R&D systems, USA) and IL-2 (Clone 5334, R&D systems, USA), as well as Orencia (Bristol-Myers, Italy), were used at 5 µg/mL, 10 µg/mL, 25 µg/mL, 5 µg/mL and 25 µg/mL respectively to block IFNγ bioactivity and/or expression. To ensure that the effects seen with the neutralising antibodies and fusion protein were specific, isotype-matched controls, IgG2A (Clone 20102), IgG1 (Clone 11711), IgG2B (Clone 20116, R&D systems, USA) and hIgG (Intragram® P, Australian Red Cross Blood Service) were used. The antibodies were pre-incubated with endothelial cells for 15 min before adding the PBMCs. After incubating PBMCs and endothelial cells together with antibody for another 30 min, iRBCs were added into the tripartite cultures for the 24 h incubation period. YVAD (Cayman Chemical, USA), also known as Z-YVAD-FMK (fluoromethylketone), is a caspase-1 inhibitor. Inclusion of YVAD at 50 µmol/L in the tripartite cultures was similar to the neutralisation antibodies, with a vehicle control of DMSO (0.135%, v/v) being included in the experimental design.
Transwell separations
Transwell inserts of pore size 0.4 µm (Corning, USA) were used in concert with 24 well plates (Corning, USA). To optimise the growth rate of the HBEC on this artificial support, the number of cells seeded was 3.5 times more than that in a typical tripartite culture in a 96 well plate. Samples were collected after 24 h of culture, with mRNA being isolated from both the upper and lower chambers when cells were present. Concurrently, supernatants were sampled and kept at −80°C for further analysis.
NK cell depletion
PBMCs were sorted based on their surface marker staining. Briefly, PBMCs were stained with anti-CD16 (clone 3G8, Biolegend, USA), NKp46 (clone 9E2, BioLegend, USA) and CD56 antibodies (clone MEM188, eBioscience, USA). NK cells (CD16+, CD56+, NKp46+) were depleted using a FACSaria cell sorter (Becton Dickinson, USA). NK-depleted PBMC were shown to be >99% NK free before inclusion in tripartite cultures.
Funding Statement
This work was supported by a grant from the National Health and Medical Research Council of Australia to NH and a Sir Zelman Cowen Universities Fund grant to JG and NH. LTK was supported by a scholarship from the Ministry of Science, Technology and Innovation, Malaysia. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. John CC (2007) Cerebral Malaria Pathogenesis: What Can We Learn from Microarray Analysis? Am J Pathol 171: 1729–1732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Newton CR, Krishna S (1998) Severe falciparum malaria in children: current understanding of pathophysiology and supportive treatment. Pharmacol Ther 79: 1–53. [DOI] [PubMed] [Google Scholar]
- 3. Hunt NH, Golenser J, Chan-Ling T, Parekh S, Rae C, et al. (2006) Immunopathogenesis of cerebral malaria. Int J Parasitol 36: 569–582. [DOI] [PubMed] [Google Scholar]
- 4. Grau GE, Taylor TE, Molyneux ME, Wirima JJ, Vassalli P, et al. (1989) Tumor necrosis factor and disease severity in children with falciparum malaria. N Engl J Med 320: 1586–1591. [DOI] [PubMed] [Google Scholar]
- 5. Anstey NM, Weinberg JB, Hassanali MY, Mwaikambo ED, Manyenga D, et al. (1996) Nitric oxide in Tanzanian children with malaria: inverse relationship between malaria severity and nitric oxide production/nitric oxide synthase type 2 expression. J Exp Med 184: 557–567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Greene JA, Sam-Agudu N, John CC, Opoka RO, Zimmerman PA, et al. (2012) Toll-like receptor polymorphisms and cerebral malaria: TLR2 Delta22 polymorphism is associated with protection from cerebral malaria in a case control study. Malar J 11: 47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. John CC, Panoskaltsis-Mortari A, Opoka RO, Park GS, Orchard PJ, et al. (2008) Cerebrospinal fluid cytokine levels and cognitive impairment in cerebral malaria. Am J Trop Med Hyg 78: 198–205. [PMC free article] [PubMed] [Google Scholar]
- 8. Lou J, Lucas R, Grau GE (2001) Pathogenesis of cerebral malaria: recent experimental data and possible applications for humans. Clin Microbiol Rev 14: 810–820 table of contents. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. de Souza JB, Hafalla JC, Riley EM, Couper KN (2010) Cerebral malaria: why experimental murine models are required to understand the pathogenesis of disease. Parasitology 137: 755–772. [DOI] [PubMed] [Google Scholar]
- 10. Amani V, Vigario AM, Belnoue E, Marussig M, Fonseca L, et al. (2000) Involvement of IFN-gamma receptor-medicated signaling in pathology and anti-malarial immunity induced by Plasmodium berghei infection. Eur J Immunol 30: 1646–1655. [DOI] [PubMed] [Google Scholar]
- 11. Van den Steen PE, Deroost K, Van Aelst I, Geurts N, Martens E, et al. (2008) CXCR3 determines strain susceptibility to murine cerebral malaria by mediating T lymphocyte migration toward IFN-gamma-induced chemokines. Eur J Immunol 38: 1082–1095. [DOI] [PubMed] [Google Scholar]
- 12. Sanni LA, Thomas SR, Tattam BN, Moore DE, Chaudhri G, et al. (1998) Dramatic changes in oxidative tryptophan metabolism along the kynurenine pathway in experimental cerebral and noncerebral malaria. Am J Pathol 152: 611–619. [PMC free article] [PubMed] [Google Scholar]
- 13. Schofield L, Grau GE (2005) Immunological processes in malaria pathogenesis. Nat Rev Immunol 5: 722–735. [DOI] [PubMed] [Google Scholar]
- 14. Bridges DJ, Bunn J, van Mourik JA, Grau G, Preston RJ, et al. (2010) Rapid activation of endothelial cells enables Plasmodium falciparum adhesion to platelet-decorated von Willebrand factor strings. Blood 115: 1472–1474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Wassmer S, Lepolard C, Traore B, Pouvelle B, Gysin J, et al. (2004) Platelets Reorient Plasmodium falciparum-Infected Erythrocyte Cytoadhesion to Activated Endothelial Cells. J Infect Dis 189: 180–189. [DOI] [PubMed] [Google Scholar]
- 16. Wassmer SC, Combes V, Candal FJ, Juhan-Vague I, Grau GE (2006) Platelets potentiate brain endothelial alterations induced by Plasmodium falciparum. Infect Immun 74: 645–653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Faille D, Combes V, Mitchell AJ, Fontaine A, Juhan-Vague I, et al. (2009) Platelet microparticles: a new player in malaria parasite cytoadherence to human brain endothelium. FASEB J 23: 3449–3458. [DOI] [PubMed] [Google Scholar]
- 18. Barbier M, Faille D, Loriod B, Textoris J, Camus C, et al. (2011) Platelets alter gene expression profile in human brain endothelial cells in an in vitro model of cerebral malaria. PLoS One 6: e19651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Korbel DS, Newman KC, Almeida CR, Davis DM, Riley EM (2005) Heterogeneous human NK cell responses to Plasmodium falciparum-infected erythrocytes. J Immunol 175: 7466–7473. [DOI] [PubMed] [Google Scholar]
- 20. Walther M, Woodruff J, Edele F, Jeffries D, Tongren JE, et al. (2006) Innate immune responses to human malaria: heterogeneous cytokine responses to blood-stage Plasmodium falciparum correlate with parasitological and clinical outcomes. J Immunol 177: 5736–5745. [DOI] [PubMed] [Google Scholar]
- 21. Artavanis-Tsakonas K, Riley EM (2002) Innate Immune Response to Malaria: Rapid Induction of IFN-{gamma} from Human NK Cells by Live Plasmodium falciparum-Infected Erythrocytes. J Immunol 169: 2956–2963. [DOI] [PubMed] [Google Scholar]
- 22. D′Ombrain MC, Voss TS, Maier AG, Pearce JA, Hansen DS, et al. (2007) Plasmodium falciparum erythrocyte membrane protein-1 specifically suppresses early production of host interferon-gamma. Cell Host Microbe 2: 130–138. [DOI] [PubMed] [Google Scholar]
- 23. Ochola LB, Siddondo BR, Ocholla H, Nkya S, Kimani EN, et al. (2011) Specific receptor usage in Plasmodium falciparum cytoadherence is associated with disease outcome. PLoS One 6: e14741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Berendt AR, Simmons DL, Tansey J, Newbold CI, Marsh K (1989) Intercellular adhesion molecule-1 is an endothelial cell adhesion receptor for Plasmodium falciparum. Nature 341: 57–59. [DOI] [PubMed] [Google Scholar]
- 25. Mannel DN, Grau GE (1997) Role of platelet adhesion in homeostasis and immunopathology. Mol Pathol 50: 175–185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Baratin M, Roetynck S, Pouvelle B, Lemmers C, Viebig NK, et al. (2007) Dissection of the role of PfEMP1 and ICAM-1 in the sensing of Plasmodium-falciparum-infected erythrocytes by natural killer cells. PLoS One 2: e228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Miu J, Mitchell AJ, Muller M, Carter SL, Manders PM, et al. (2008) Chemokine Gene Expression during Fatal Murine Cerebral Malaria and Protection Due to CXCR3 Deficiency. J Immunol 180: 1217–1230. [DOI] [PubMed] [Google Scholar]
- 28. May J, Lell B, Luty AJ, Meyer CG, Kremsner PG (2000) Plasma interleukin-10:Tumor necrosis factor (TNF)-alpha ratio is associated with TNF promoter variants and predicts malarial complications. J Infect Dis 182: 1570–1573. [DOI] [PubMed] [Google Scholar]
- 29. Othoro C, Lal AA, Nahlen B, Koech D, Orago AS, et al. (1999) A low interleukin-10 tumor necrosis factor-alpha ratio is associated with malaria anemia in children residing in a holoendemic malaria region in western Kenya. J Infect Dis 179: 279–282. [DOI] [PubMed] [Google Scholar]
- 30. Caligiuri MA (2008) Human natural killer cells. Blood 112: 461–469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Kordes M, Matuschewski K, Hafalla JC (2011) Caspase-1 activation of interleukin-1beta (IL-1beta) and IL-18 is dispensable for induction of experimental cerebral malaria. Infect Immun 79: 3633–3641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Hansen DS, Schofield L (2004) Regulation of immunity and pathogenesis in infectious diseases by CD1d-restricted NKT cells. Int J Parasitol 34: 15–25. [DOI] [PubMed] [Google Scholar]
- 33. D′Ombrain MC, Hansen DS, Simpson KM, Schofield L (2007) gammadelta-T cells expressing NK receptors predominate over NK cells and conventional T cells in the innate IFN-gamma response to Plasmodium falciparum malaria. Eur J Immunol 37: 1864–1873. [DOI] [PubMed] [Google Scholar]
- 34. Horowitz A, Newman KC, Evans JH, Korbel DS, Davis DM, et al. (2010) Cross-talk between T cells and NK cells generates rapid effector responses to Plasmodium falciparum-infected erythrocytes. J Immunol 184: 6043–6052. [DOI] [PubMed] [Google Scholar]
- 35. Hunt NH, Grau GE (2003) Cytokines: accelerators and brakes in the pathogenesis of cerebral malaria. Trends Immunol 24: 491–499. [DOI] [PubMed] [Google Scholar]
- 36. de Souza JB, Riley EM (2002) Cerebral malaria: the contribution of studies in animal models to our understanding of immunopathogenesis. Microbes Infect 4: 291–300. [DOI] [PubMed] [Google Scholar]
- 37. Good MF, Xu H, Wykes M, Engwerda CR (2005) Development and regulation of cell-mediated immune responses to the blood stages of malaria: implications for vaccine research. Annu Rev Immunol 23: 69–99. [DOI] [PubMed] [Google Scholar]
- 38. McCall MB, Sauerwein RW (2010) Interferon-gamma--central mediator of protective immune responses against the pre-erythrocytic and blood stage of malaria. J Leukoc Biol 88: 1131–1143. [DOI] [PubMed] [Google Scholar]
- 39. John CC, Opika-Opoka R, Byarugaba J, Idro R, Boivin MJ (2006) Low Levels of RANTES Are Associated with Mortality in Children with Cerebral Malaria. J Infect Dis 194: 837–845. [DOI] [PubMed] [Google Scholar]
- 40. Sam-Agudu NA, Greene JA, Opoka RO, Kazura JW, Boivin MJ, et al. (2010) TLR9 polymorphisms are associated with altered IFN-gamma levels in children with cerebral malaria. Am J Trop Med Hyg 82: 548–555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Chizzolini C, Grau GE, Geinoz A, Schrijvers D (1990) T lymphocyte interferon-gamma production induced by Plasmodium falciparum antigen is high in recently infected non-immune and low in immune subjects. Clin Exp Immunol 79: 95–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Grau GE, Heremans H, Piguet PF, Pointaire P, Lambert PH, et al. (1989) Monoclonal antibody against interferon gamma can prevent experimental cerebral malaria and its associated overproduction of tumor necrosis factor. Proc Natl Acad Sci U S A 86: 5572–5574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Amante FH, Haque A, Stanley AC, Rivera Fde L, Randall LM, et al. (2010) Immune-mediated mechanisms of parasite tissue sequestration during experimental cerebral malaria. J Immunol 185: 3632–3642. [DOI] [PubMed] [Google Scholar]
- 44. Yanez DM, Manning DD, Cooley AJ, Weidanz WP, van der Heyde HC (1996) Participation of lymphocyte subpopulations in the pathogenesis of experimental murine cerebral malaria. J Immunol 157: 1620–1624. [PubMed] [Google Scholar]
- 45. Claser C, Malleret B, Gun SY, Wong AY, Chang ZW, et al. (2011) CD8+ T cells and IFN-gamma mediate the time-dependent accumulation of infected red blood cells in deep organs during experimental cerebral malaria. PLoS One 6: e18720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Dufour JH, Dziejman M, Liu MT, Leung JH, Lane TE, et al. (2002) IFN-gamma-inducible protein 10 (IP-10; CXCL10)-deficient mice reveal a role for IP-10 in effector T cell generation and trafficking. J Immunol 168: 3195–3204. [DOI] [PubMed] [Google Scholar]
- 47. Booth V, Keizer DW, Kamphuis MB, Clark-Lewis I, Sykes BD (2002) The CXCR3 binding chemokine IP-10/CXCL10: structure and receptor interactions. Biochemistry 41: 10418–10425. [DOI] [PubMed] [Google Scholar]
- 48. Wilson NO, Jain V, Roberts CE, Lucchi N, Joel PK, et al. (2011) CXCL4 and CXCL10 predict risk of fatal cerebral malaria. Dis Markers 30: 39–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Campanella GS, Tager AM, El Khoury JK, Thomas SY, Abrazinski TA, et al. (2008) Chemokine receptor CXCR3 and its ligands CXCL9 and CXCL10 are required for the development of murine cerebral malaria. Proc Natl Acad Sci U S A 105: 4814–4819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Nie CQ, Bernard NJ, Norman MU, Amante FH, Lundie RJ, et al. (2009) IP-10-mediated T cell homing promotes cerebral inflammation over splenic immunity to malaria infection. PLoS Pathog 5: e1000369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Rowe JA, Claessens A, Corrigan RA, Arman M (2009) Adhesion of Plasmodium falciparum-infected erythrocytes to human cells: molecular mechanisms and therapeutic implications. Expert Rev Mol Med 11: e16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Favre N, Da Laperousaz C, Ryffel B, Weiss NA, Imhof BA, et al. (1999) Role of ICAM-1 (CD54) in the development of murine cerebral malaria. Microbes Infect 1: 961–968. [DOI] [PubMed] [Google Scholar]
- 53. Rudin W, Eugster HP, Bordmann G, Bonato J, Muller M, et al. (1997) Resistance to cerebral malaria in tumor necrosis factor-alpha/beta-deficient mice is associated with a reduction of intercellular adhesion molecule-1 up-regulation and T helper type 1 response. Am J Pathol 150: 257–266. [PMC free article] [PubMed] [Google Scholar]
- 54. Most J, Schwaeble W, Drach J, Sommerauer A, Dierich MP (1992) Regulation of the expression of ICAM-1 on human monocytes and monocytic tumor cell lines. J Immunol 148: 1635–1642. [PubMed] [Google Scholar]
- 55. Ishikura H, Takahashi C, Kanagawa K, Hirata H, Imai K, et al. (1991) Cytokine regulation of ICAM-1 expression on human renal tubular epithelial cells in vitro. Transplantation 51: 1272–1275. [DOI] [PubMed] [Google Scholar]
- 56. Artavanis-Tsakonas K, Riley EM (2002) Innate immune response to malaria: rapid induction of IFN-gamma from human NK cells by live Plasmodium falciparum-infected erythrocytes. J Immunol 169: 2956–2963. [DOI] [PubMed] [Google Scholar]
- 57. Baratin M, Roetynck S, Lepolard C, Falk C, Sawadogo S, et al. (2005) Natural killer cell and macrophage cooperation in MyD88-dependent innate responses to Plasmodium falciparum. Proc Natl Acad Sci U S A 102: 14747–14752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Kurtzhals JA, Adabayeri V, Goka BQ, Akanmori BD, Oliver-Commey JO, et al. (1998) Low plasma concentrations of interleukin 10 in severe malarial anaemia compared with cerebral and uncomplicated malaria. Lancet 351: 1768–1772. [DOI] [PubMed] [Google Scholar]
- 59. Day NP, Hien TT, Schollaardt T, Loc PP, Chuong LV, et al. (1999) The prognostic and pathophysiologic role of pro- and antiinflammatory cytokines in severe malaria. J Infect Dis 180: 1288–1297. [DOI] [PubMed] [Google Scholar]
- 60. Ho M, Sexton MM, Tongtawe P, Looareesuwan S, Suntharasamai P, et al. (1995) Interleukin-10 inhibits tumor necrosis factor production but not antigen-specific lymphoproliferation in acute Plasmodium falciparum malaria. J Infect Dis 172: 838–844. [DOI] [PubMed] [Google Scholar]
- 61. Golenser J, Domb A, Mordechai-Daniel T, Leshem B, Luty A, et al. (2006) Iron chelators: correlation between effects on Plasmodium spp. and immune functions. J Parasitol 92: 170–177. [DOI] [PubMed] [Google Scholar]
- 62. Kwiatkowski D, Hill AV, Sambou I, Twumasi P, Castracane J, et al. (1990) TNF concentration in fatal cerebral, non-fatal cerebral, and uncomplicated Plasmodium falciparum malaria. Lancet 336: 1201–1204. [DOI] [PubMed] [Google Scholar]
- 63. Engwerda CR, Mynott TL, Sawhney S, De Souza JB, Bickle QD, et al. (2002) Locally up-regulated lymphotoxin alpha, not systemic tumor necrosis factor alpha, is the principle mediator of murine cerebral malaria. J Exp Med 195: 1371–1377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Horowitz A, Riley EM (2009) Activation of human NK cells by malaria-infected red blood cells. Methods Mol Biol 612: 429–446. [DOI] [PubMed] [Google Scholar]
- 65. Artavanis-Tsakonas K, Eleme K, McQueen KL, Cheng NW, Parham P, et al. (2003) Activation of a subset of human NK cells upon contact with Plasmodium falciparum-infected erythrocytes. J Immunol 171: 5396–5405. [DOI] [PubMed] [Google Scholar]
- 66. Schofield L, McConville MJ, Hansen D, Campbell AS, Fraser-Reid B, et al. (1999) CD1d-restricted immunoglobulin G formation to GPI-anchored antigens mediated by NKT cells. Science 283: 225–229. [DOI] [PubMed] [Google Scholar]
- 67. Griffith JW, Sun T, McIntosh MT, Bucala R (2009) Pure Hemozoin is inflammatory in vivo and activates the NALP3 inflammasome via release of uric acid. J Immunol 183: 5208–5220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Shio MT, Eisenbarth SC, Savaria M, Vinet AF, Bellemare MJ, et al. (2009) Malarial hemozoin activates the NLRP3 inflammasome through Lyn and Syk kinases. PLoS Pathog 5: e1000559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Dostert C, Guarda G, Romero JF, Menu P, Gross O, et al. (2009) Malarial hemozoin is a Nalp3 inflammasome activating danger signal. PLoS One 4: e6510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Orengo JM, Evans JE, Bettiol E, Leliwa-Sytek A, Day K, et al. (2008) Plasmodium-induced inflammation by uric acid. PLoS Pathog 4: e1000013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Couper KN, Barnes T, Hafalla JC, Combes V, Ryffel B, et al. (2010) Parasite-derived plasma microparticles contribute significantly to malaria infection-induced inflammation through potent macrophage stimulation. PLoS Pathog 6: e1000744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Kroczek RA, Mages HW, Hutloff A (2004) Emerging paradigms of T-cell co-stimulation. Curr Opin Immunol 16: 321–327. [DOI] [PubMed] [Google Scholar]
- 73. Newman KC, Riley EM (2007) Whatever turns you on: accessory-cell-dependent activation of NK cells by pathogens. Nat Rev Immunol 7: 279–291. [DOI] [PubMed] [Google Scholar]
- 74. Monso-Hinard C, Lou JN, Behr C, Juillard P, Grau GE (1997) Expression of major histocompatibility complex antigens on mouse brain microvascular endothelial cells in relation to susceptibility to cerebral malaria. Immunology 92: 53–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Trager W, Jensen JB (1976) Human malaria parasites in continuous culture. Science 193: 673–675. [DOI] [PubMed] [Google Scholar]
- 76. Walliker D, Quakyi IA, Wellems TE, McCutchan TF, Szarfman A, et al. (1987) Genetic analysis of the human malaria parasite Plasmodium falciparum. Science 236: 1661–1666. [DOI] [PubMed] [Google Scholar]
- 77. Beeson JG, Brown GV (2004) Plasmodium falciparum-infected erythrocytes demonstrate dual specificity for adhesion to hyaluronic acid and chondroitin sulfate A and have distinct adhesive properties. J Infect Dis 189: 169–179. [DOI] [PubMed] [Google Scholar]
- 78. Noviyanti R, Brown GV, Wickham ME, Duffy MF, Cowman AF, et al. (2001) Multiple var gene transcripts are expressed in Plasmodium falciparum infected erythrocytes selected for adhesion. Mol Biochem Parasitol 114: 227–237. [DOI] [PubMed] [Google Scholar]
- 79. Beeson JG, Rogerson SJ, Cooke BM, Reeder JC, Chai W, et al. (2000) Adhesion of Plasmodium falciparum-infected erythrocytes to hyaluronic acid in placental malaria. Nat Med 6: 86–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Jambou R, Combes V, Jambou MJ, Weksler BB, Couraud PO, et al. (2010) Plasmodium falciparum adhesion on human brain microvascular endothelial cells involves transmigration-like cup formation and induces opening of intercellular junctions. PLoS Pathog 6: e1001021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Milner DA, Valim C, Luo R, Playforth KB, Kamiza S, et al. (2012) Supraorbital Postmortem Brain Sampling for Definitive Quantitative Confirmation of Cerebral Sequestration of Plasmodium falciparum Parasites. Journal of Infectious Diseases 205: 1601–1606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Tripathi AK, Sha W, Shulaev V, Stins MF, Sullivan DJ Jr (2009) Plasmodium falciparum-infected erythrocytes induce NF-kappaB regulated inflammatory pathways in human cerebral endothelium. Blood 114: 4243–4252. [DOI] [PMC free article] [PubMed] [Google Scholar]