Summary
An accurate diagnosis of osteoporosis and a proper treatment are today recognized to be the most important facts for prevention and for a correct arrangement and treatment of fragility fractures. In the text the Authors describe a case of severe osteoporosis aggravated by 2 femur fractures and 2 periprosthetic fractures occurred in 2 months. In such cases the orthopaedic surgeon needs to formulate first a clinical osteoporotic pattern, than its treatment together with a surgery suitable choice, that has to take into consideration of the bone structural characteristics. In the case described one can note that fractures healing occurred thanks to both an improvement in surgical techniques and antiosteoporotic pharmacological support; in the specific case the Authors used strontium ranelate for its osteoinductive capacity. In our opinion is crucial that the treatment used by orthopaedic surgeons is not related only to the “by-hand” treatment but take into consideration both the underlying disease and the possibility of positively affect bone healing with specific drug therapy.
Keywords: osteoporosis, periprosthetic fractures, bone healing
Introduction
The bones fragility, typical of osteoporosis, is a main risk factor for the occurrence of first episodes of fractures and re-fractures (1–4).
An accurate diagnosis of osteoporosis (5) and a proper treatment are today recognized to be the most important facts for prevention and for a correct arrangement and treatment of fragility fractures.
In spite of the high incidence of osteoporosis, mainly due to the increase in life expectancy, especially in females, and to the high socio-economic impact of fragility fractures, we are currently often in front of cases of fractures, that repeat in the same patient who, to the detriment of the clinical picture, was never framed in terms of bone metabolism (6).
In the text the Authors describe a case of severe osteoporosis aggravated by 2 femur fractures and 2 periprosthetic fractures. The incidence of periprosthetic hip fractures is increasing (7–9); so far it is estimated that the incidence is approximately 1% after primary THA and about 4% after revision THA (10). This incidence increase is due both to longer term life expectancy, with serious osteoporosis consequences (11) and to the increase of the number of implants (12, 13).
Periprosthetic fractures in particular affect women in a ratio of 2:1 towards man and the average age is 68 years.
Various risk factor have been identified for the occurrence of these fractures: they can be classified in general risk facts, among them osteoporosis and neurological diseases that alterate the ambulatory pattern, and local risk factors such as periprostheticosteolysis or cortical iatrogenic intra and perioperative defects.
The Vancouver classification, developed by Duncan and Masri in 1985, is one of the most commonly used classification. It considers the quality of the bone, the fracture site and the implant stability (14).
Case report
The case describes a female patient of 80 years old with significant comorbidities like atrial fibrillation, heart failure with a high surgical risk (ASA 4).
In 2006 and 2007 the patient had 2 fractures: right and left femoral neck, for which she was submitted to surgery for bilateral hip prosthetization (Figure 1).
Figure 1.
Pelvis X-Ray with bilateral hip prosthesis.
In August 2008, after an accidental fall at home, the patient reported a new fragility fracture: a periprosthetic right femur fracture a type C (Figures 2, 3) according to Vancouver classification (15).
Figures 2, 3.


Periprosthetic fractures of the right femur.
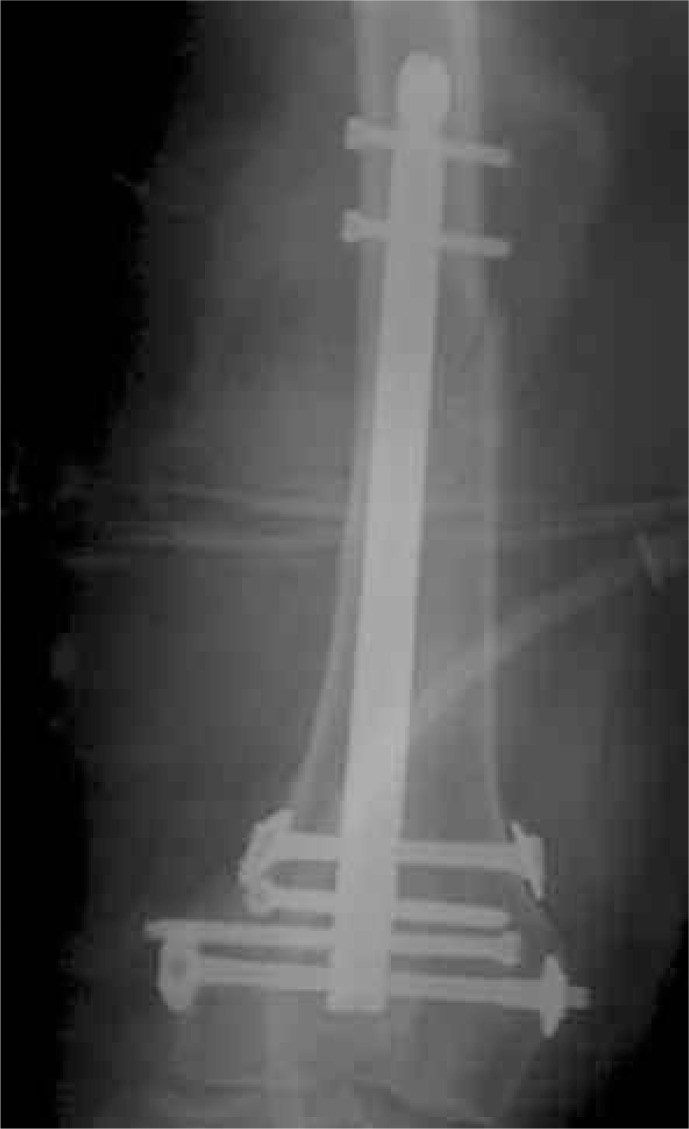
For this reason, the patient had a surgery reduction and synthesis of fracture with retrograde intramedullary nail (Figure 4). The choice of surgical technique was almost forced by patient’s general conditions, that required the least invasive and quickest surgical procedure, with the lower risk of blood loss.
Figure 4.
Post-operative X Ray after fracture fixation with a retrograde nail.
During last hospitalization the patient was submitted to first level blood tests to study bone metabolism, which showed a severe condition of hypovitaminosis D (vit D=4 ng/ml), therefore she was injected with 300,000 UI of Vitamin D.
At the moment of discharge the patient was suggested to abstain from any kind of loading for min 30 and was treated with antiosteoporotic therapy based on strontium ranelate (2 g/day), vit D (800 UI/day), calcium (1200mg/day) and magnetotherapy. About 1 month after surgery the patient complained functional inability of right lower limb. The X-ray showed the loss of fracture reduction with mobilization of the two proximal screws (Figure 5).
Figure 5.

Femoral refracture.
For this reason, the patient was referred back to surgical reduction and fixation of the fracture with plate and cerclage without removal of the nail and the prosthesis (Figure 6).
Figure 6.
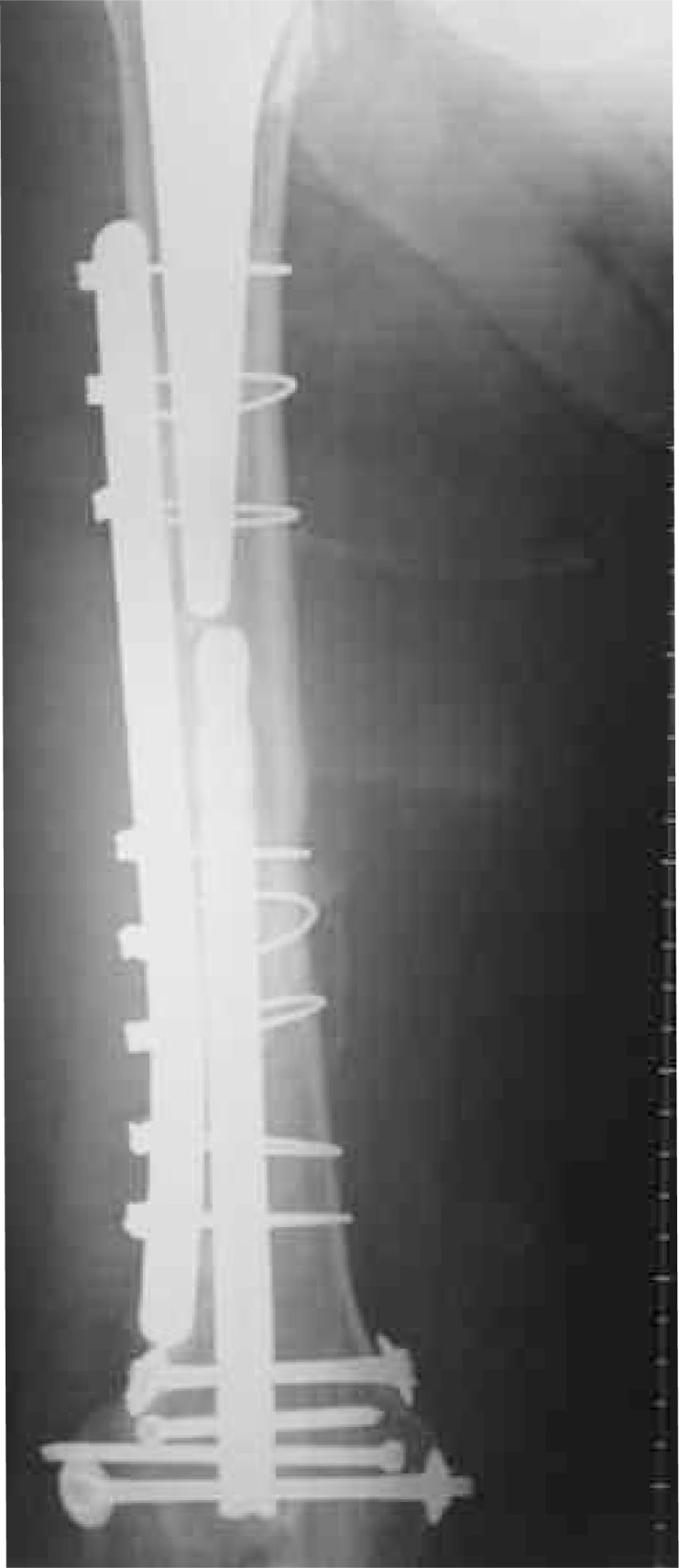
Fixation of the fracture with plate and cerclage without removal of the nail and the prosthesis.
In this case the choice was force to the plate, despite the general clinical condition of the patient and high perioperative risk.
After surgery a cast was packed to be kept for 30 days with complete abstention to any sort of loading.
The next 30 days x-ray control after surgery showed an initial formation of the bone callus.
The cast was removed and the patient was able to start an active and passive mobilisation, without loading, of the right lower limb; at this moment we recovery the medical therapy with strontium ranelate previously suspended for the immobilization period.
After 3 months x-ray showed fracture healing, with partial and progressing loading, up to total loading.
The radiographic check after 10 months from surgery showed that there was mobilization of a condylar screw that was removed.
After 15 months from surgery, at clinical and radiographic control, the patient was able to walk without crutches and had a range of motion of the lower right arm, with right knee flexion up to 100° and extension up to +10° (Figure 7).
Figure 7.
Current situation.
Discussion
Fractures are the most feared osteoporosis complications and often result in disability and loss of autonomy of patients, with socio-economic consequences.
Moreover, in Literature, many studies suggest a negative correlation between age and fracture healing (16) resulting in further difficulties in achieving clinical-radiographic healing of fractures in elderly patients.
The case described is a typical example of a serious osteoporotic pattern, complicated with 4 fractures occurred in 2 months.
In such cases the orthopaedic surgeon needs to formulate first a clinical osteoporotic pattern, than its treatment together with a surgery suitable choice, that has to take into consideration of the bone structural characteristics.
All this in order to optimize the resources available for the fragility fractures treatment: pharmacological resources (anti osteoporotic drugs and adequate calcium and Vit D supplementation), surgical resources (specific osteoporotic bone fixation) and physical resources (use of osteoinductive capacity of magnetic fields) (17, 18). In the case described one can note that fractures healing occurred thanks to both an improvement in surgical techniques and antiosteoporotic pharmacological support, in the specific case the Authors used strontium ranelate for its osteoinductive capacity. In fact there are many studies in Literature, that corroborate strontium ranelato osteoinductive capacity. In our opinion is crucial that the treatment used by orthopaedic surgeons is not related only to the “by-hand” treatment but take into consideration both the underlying disease and the possibility of positively affect bone healing with specific drug therapy.
References
- 1.Leali PT, Muresu F, Melis A, Ruggiu A, Zachos A, Doria C. Skeletal fragility definition. Clin Cases Miner Bone Metab. 2011 May;8(2):11–13. [PMC free article] [PubMed] [Google Scholar]
- 2.Della Carbonare L, Giannini S. Bone microarchitecture as an important determinant of bone strength. J Endocrinol Invest. 2004 Jan;27(1):99–105. doi: 10.1007/BF03350919. [DOI] [PubMed] [Google Scholar]
- 3.Piscitelli P, Brandi ML, Chitano G, Argentiero A, Neglia C, Distante A, Saturnino L, Tarantino U. Epidemiology of fragility fractures in Italy. Clin Cases Miner Bone Metab. 2011 May;8(2):29–34. [PMC free article] [PubMed] [Google Scholar]
- 4.Giannotti S, Bottai V, Dell’Osso G, Donati D, Bugelli G, De Paola G, Guido G. Indices of risk assessment of fracture of the proximal humerus. Clin Cases Miner Bone Metab. 2012 Jan;9(1):37–9. [PMC free article] [PubMed] [Google Scholar]
- 5.Barnett E, Nordin BEC. The radiological diagnosis of osteoporosis a new approach. Clin Radiol. 1960;11:166–9. doi: 10.1016/s0009-9260(60)80012-8. [DOI] [PubMed] [Google Scholar]
- 6.Piscitelli P, Tarantino U, Chitano G, Argentiero A, Neglia C, Agnello N, Saturnino L, Feola M, Celi M, Raho C, Distante A, Brandi ML. Updated incidence rates of fragility fractures in Italy: extension study 2002–2008. Clin Cases Miner Bone Metab. 2011 Sep;8(3):54–61. [PMC free article] [PubMed] [Google Scholar]
- 7.Giannotti S, Bottai V, Dell’Osso G, Donati D, Bugelli G, De Paola G, Guido G. Humeral bone fragility in patients with shoulder prosthesis: a case of humeral periprosthetic refracture. Clin Cases Miner Bone Metab. 2012 Jan;9(1):56–8. [PMC free article] [PubMed] [Google Scholar]
- 8.Rupprecht M, Sellenschloh K, et al. Biomechanical evaluation for mechanisms of periprosthetic femoral fractures. J Trauma. 2011 Apr;70(4):E62–6. doi: 10.1097/TA.0b013e3181e99ff1. [DOI] [PubMed] [Google Scholar]
- 9.Parvizi J, Vegari DN. Periprosthetic proximal femur fractures: current concepts. J Orthop Trauma. 2011 Jun;25(Suppl 2):S77–81. doi: 10.1097/BOT.0b013e31821b8c3b. [DOI] [PubMed] [Google Scholar]
- 10.Rocca GJ, Leung KS, Pape HC. Periprosthetic Fractures: Epidemiology and Future Projections. J Orthop Trauma. 2011 Jun;25(Number 6 Supplement 2):S66–S70. doi: 10.1097/BOT.0b013e31821b8c28. [DOI] [PubMed] [Google Scholar]
- 11.Guido G, Giannotti S, Bottai V, Ghilardi M, Bianchi MG, Ceglia MJ. Femoral fractures in the extremely elderly. Clin Cases Miner Bone Metab. 2011 May;8(2):35–37. [PMC free article] [PubMed] [Google Scholar]
- 12.Giannotti S, Bottai V, Ghilardi M, Dell’Osso G, Guido G. Shoulder resurfacing with Durom Cup: clinical and radiological re-assessment. J Orthop Sci. 2012 Sep;17(5):545–50. doi: 10.1007/s00776-012-0256-2. [DOI] [PubMed] [Google Scholar]
- 13.Zhan C, Kaczmarek R, Loyo-Berrios N, Sangl J, Bright RA. Incidence and short-term outcomes of primary and revision hip replacement in the United States. J Bone Joint Surg Am. 2007 Mar;89(3):526–33. doi: 10.2106/JBJS.F.00952. [DOI] [PubMed] [Google Scholar]
- 14.Garbuz DS, Masri BA, Duncan CP. Periprosthetic fractures of the femur: principles of prevention and management. Instr Course Lect. 1998;47:237–42. [PubMed] [Google Scholar]
- 15.Duncan CP, Masri BA. Fractures of the femur after hip replacement. In: Jackson DW, editor. Istructional Course Lectures. Rosemont, IL: A.A.O.S.; 1995. pp. 293–304. [PubMed] [Google Scholar]
- 16.Gruber R, Koch H, Doll BA, Tegtmeier F, Einhorn TA, Hollinger JO. Exp Gerontol. 2006 Nov;41(11:):1080–93. doi: 10.1016/j.exger.2006.09.008. Epub 2006 Nov 7. Review. [DOI] [PubMed] [Google Scholar]
- 17.Giannotti S, Bottai V, Dell’Osso G, De Paola G, Pini E, Guido G. Atrophic femoral nonunion successfully treated with teriparatide. Eur J Orthop Surg Traumatol. 2012 doi: 10.1007/s00590-012-1143-4.. [DOI] [PubMed] [Google Scholar]
- 18.Giannotti S, Bottai V, Ghilardi M, Dell’Osso G, Fazzi R, Trombi L, Petrini M, Guido G. Treatment of pseudoarthrosis of the upper limb using expanded mesenchymal stem cells: a pilot study. Eur Rev Med Pharmacol Sci. 2013 Jan;17(2):224–7. [PubMed] [Google Scholar]