Summary
Aseptic loosening due to wear debris is the most frequent modality of failure in total hip arthroplasty. Bisphosphonates, a class of molecules which inhibit bone resorption showed an inhibitory effects on particles-induced osteolysis in vitro and in animal models. We report the clinical, radiographic and densitometric outcome of four postmenopausal women with total hip arthroplasty affected by peri-prosthetic osteolysis treated with neridronate due to their unwillingness to be operated. After neridronate treatment, there was general improvement in pain and function: VAS decrease 13 points (15%), the Harris Hip Score increase 9 points (15%). An average number of 3.3 x-ray per patients with an average follow-up of 23 months (range 12–34) were collected and evaluated.
In all the patients except one, serial radiographs didn’t show any progression of radioluciencies lines or periprosthetic osteolysis. Bone density was evaluated by Dual energy X-ray absorptiometry after an average follow-up of 21 months (range 6–46 mo): periprosthetic BMD around the whole stem and the cup increased respectively 2.4% and 7.1%.
Treatment was well tolerated and no significant side effects were registered. This retrospective collection of a small group of patients suggest that bisphosphonates should be clinically useful in preventing periprosthetic wear debris mediated osteolysis and claim for dedicated clinical trials.
Keywords: aseptic loosening, total hip arthroplasty, bisphosphonates, osteolysis, bone mineral density
Introduction
Aseptic loosening to wear debris products which induce osteoclast-mediate bone resorption is the most frequent modality of failure in total hip arthroplasty.
Bisphosphonates (BPs) are a class of molecules which bind strongly to mineral crystals of bone and inhibit bone resorption acting predominantly on osteoclasts (1).
Several investigations have been published on the reduction of bone resorption by BPs in vitro and in animal models of particles-induced osteolysis suggesting that pharmacological inhibition of bone resorption might be used to control the osteolysis of aseptic loosening (2–6).
In a recent report, an aggressive periprosthetic osteolysis after total hip arthroplasty was treated with oral alendronate which halted the progression of osteolysis over a year before revision (7). These data from the literature suggest a potential role of bisphosphonates for the treatment of periprosthetic osteolysis. In this paper, we report the outcome of four patients with total hip arthoplasty affected by periprosthetic osteolysis treated with bisphosphonates.
Material and Methods
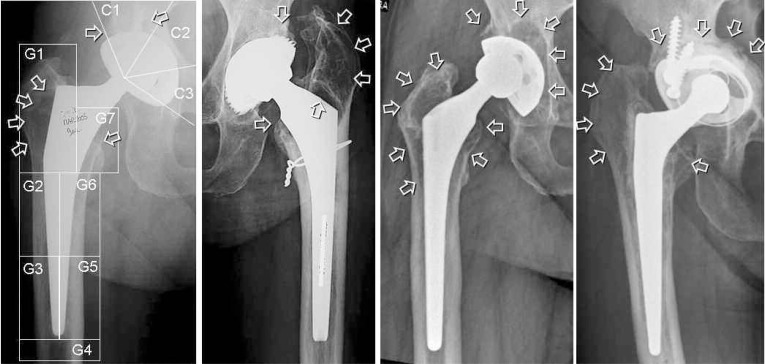
Four patients with a painful total hip arthroplasty and radiographic osteolysis for which an indication for a revision surgery was given, were treated with injective BPs to inhibit osteolysis progression (Figure 1). The main reason for BPs treatment was the unwillingness to be operated in the short term expressed by the patients.
Figure 1.
Patients radiographs showing sites of periprosthetic osteolysis (white arrows). In the first radiograph the Gruens Zones and Charnley Regions used for densitometric analysis of bone mineral density are shown.
All patients were postmenopausal women whose anamnestic and demographic data are shown on Table 1. They presented groin pain and a painful limp, radiological signs of periprosthetic osteolysis and a positive Tc-MDP bone scintigraphy showing a radionucleide homogeneous periprosthetic uptake. None of the patients show any clinical sign, symptom or laboratory tests suggestive of deep infection.
Table 1.
Demographic and pertinent clinical information on the patients.
| Age (yrs) | Bone Status L1–L4 T score | Type of prosthesis in the involved Hip | Time since OP (yrs) | Charnley class | Time from pain onset (months) | Indication for revision | Osteolysis location | |
|---|---|---|---|---|---|---|---|---|
| 1 TG | 69 | −2.4 | R Uncem. press fit stem and cup | 8 | B | 2 | Cup and stem | C1, C2, G1, G6, G7 |
| 2 SP | 66 | 0.4 | L Uncem. press fit stem and cup | 8 | BB | 7 | Cup | C1, G1, G7 |
| 3 BG | 69 | −1.1 | R Uncem. Press fit stem and cup | 9 | B | 3 | Cup and stem | C1, C2, G1, G2, G7 |
| 4 SM | 67 | −2,5 | R Cem. press fit stem and revision cup | 19 | BB | 15 | Cup and stem | C1, C2, C3, G7 |
R=right; L=left; Uncem=uncemented; Cem=cemented.
C=Charnley zones for cup; G=Gruen zones for stem.
The patients were treated with neridronate 25mg (Nerixia, Abiogen, Pisa - Italy) 1 intramuscular injection every 2 weeks for the first 3 months and then 1 injection per months for the whole time of follow-up. All the patients signed an informed consensus for the treatment.
Functional status of the patients before treatment and at follow-up was evaluated by means of Harris Hip Score (HHS). Pain assessment during activity was obtained with a VAS scale, activity level was estimated by means of the Mechanical Usage Score (MUS) developed by Rosenbaum et al. (8) and mobility level by Charnley classes modified according to Röder (9).
Serial standard radiographs were visually evaluated for location, size and progression of osteolysis or lines of radioluciencies. All patients underwent repeated assessment of periprosthetic bone mass and a basal evaluation of lumbar spine by means of dual energy x-ray absorptiometry (Hologic QDR2000, Hologic Inc., Waltham, MA, USA). Bone mineral density (BMD, g/cm2) have been calculated at L1–L4, in the seven Gruen zones around the stem and in the 3 Charnely regions for acetabulum (Figure 1).
Results
The four patients were treated with BPs for an average of 28 months (range 12–51). Functional status and pain at baseline are described in Table 2. After 1 year of neridronate treatment, there was an improvement in pain, function and activity: for HHS, the average increase was 15% (9 points) and 6,9% for MUS (1,8 points) and VAS decreased 15% (Table 2). After that time, the clinical situation worsened in the two patients (1-TG and 3-BG) due to a contralateral hip osteoarthritis and they were operated of total hip arthroplasty but they continue their BPs treatment.
Table 2.
Clinical results on pain, function and activity before and after 1 year of BPs treatment.
| Pain during activity (VAS) | Harris Hip Score | MUS Before | ||||
|---|---|---|---|---|---|---|
| Before BPs | 1 year | Before BPs | 1 year | BPs | 1year | |
| 1 TG | 65 | 44 | 58 | 66 | 23 | 31 |
| 2 SP | 62 | 48 | 41 | 55 | 25 | 25 |
| 3 BG | 48 | 25 | 57 | 62 | 21 | 25 |
| 4 SM | 27 | 29 | 82 | 91 | 25 | 34 |
VAS 0–100; Harris Hip Score 0–100; MUS=mechanical usage score (0–40).
An average number of 3.3 x-ray per patients with an average follow-up of 23 months (range 12–34) were collected and evaluated. Serial radiographs didn’t show any progression of periprosthetic osteolysis or radioluciencies lines (Figure 2) except for patients 2-SP where a small progression of osteolysis was observed around the cup after 20 months of treatment and the patient agreed to undergo a cup revision.
Figure 2.
Serial radiographs of patient 1-TG showing no evolution in osteolitic lesions in a 2 year period under bisphosphonates treatment.
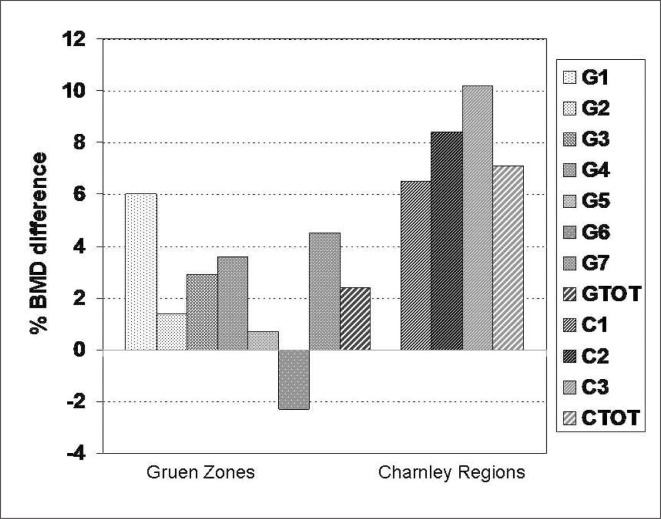
After an average follow-up of 21 months (range 6–46), periprosthetic BMD around the whole stem and the cup increased respectively 2.4% and 7.1% on the average.
In Gruen zones and Charnley regions including osteolysis, 7 out of 9 Gruen zones and 6 out of 7 Charnley regions had an increase in BMD with an average increase respectively of 5.7% (from −2.8% to 23.1%) and 5.3% (from −2.3% to 18.3%) (Figure 3). Treatment was well tolerated and no side effects were registered except for some discomfort in the site of injection.
Figure 3.
Bone mineral density percentage changes after bisphosphonates treatment from baseline in the four patients.
Discussion
In four postmenopausal women with a painful total hip arthroplasty for which revision was suggested, the parenteral administration of neridronate reduced pain, increase function and mobility, halted the radiographic progression of osteolysis and showed an increase of periprosthetic bone mineral density.
In our sample, pain was the main reason for referral in three out of four patients: a clinical significant variation of at least 20mm in a scale of 100 was achieved in 2 patients; in the third patient, the reduction was 16mm and in the fourth patient, the pain level remain low (below 30mm).
The function was measured with the Harris Hip Score: all the patients showed an improvement higher than 4 points suggesting a significant functional improvement after 1 year of treatment.
Progression of osteolysis under BPs treatment was monitored by x-rays and DEXA. In three of the four patients, osteolysis didn’t progress on standard radiographs. Accordingly, bone mineral density assessed by DEXA increased around the implants and also in the majority of regions where osteolysis was present. These data suggest an efficacy of BPs therapy to halt bone resorption and osteolysis.
The role of BPs in the prevention of periprosthetic bone loss soon after total hip arthroplasty has been demonstrated in several studies (10). Conversely, despite the evidence of an inhibitive effect of BPs on wear debris mediated bone resorption in vitro and in animal models, their potential role in human periprosthetic osteolysis has not been investigated. At our knowledge, there is only a case report in the literature which stated an inhibitory effect of alendronate on bone osteolysis due to polyethylene wear after hip prosthesis (7).
Therefore, even if this report is a retrospective collection of data from a small group of patients, it is the second only report in the literature concerning the potential role of BPs in preventing periprosthetic osteolysis in a clinical setting.
Our report suggest that BPs should halt or slow down wear debris mediated osteolysis, could be clinically useful particularly when the surgical option is not readily available or contraindicated and also claim for adequate dedicated clinical trials.
References
- 1.Rogers MJ, Gordon S, Benford HL, Coxon FP, Luckman SP, Monkkonen J, et al. Cellular and molecular mechanisms of action of bisphosphonates. Cancer. 2000;88((12) Suppl):2961–2978. doi: 10.1002/1097-0142(20000615)88:12+<2961::aid-cncr12>3.3.co;2-c. [DOI] [PubMed] [Google Scholar]
- 2.Pandey R, Quinn JM, Sabokbar A, Athanasou NA. Bisphosphonate inhibition of bone resorption induced by particulate biomaterial-associated macrophages. Acta Orthop Scand. 1996;67(3):221–8. doi: 10.3109/17453679608994677. [DOI] [PubMed] [Google Scholar]
- 3.Horowitz SM, Algan SA, Purdon MA. Pharmacologic inhibition of particulate-induced bone resorption. J Biomed Mater Res. 1996;31:91–96. doi: 10.1002/(SICI)1097-4636(199605)31:1<91::AID-JBM11>3.0.CO;2-P. [DOI] [PubMed] [Google Scholar]
- 4.Huk OL, Zukor DJ, Antoniou J, Petit A. Effect of pamidronate on the stimulation of macrophage TNF-alpha release by ultra-highmolecular-weight polyethylene particles: a role for apoptosis. J Orthop Res. 2003;21:81–87. doi: 10.1016/S0736-0266(02)00099-2. [DOI] [PubMed] [Google Scholar]
- 5.Yaffe A, Iztkovich M, Earon Y, et al. Local delivery of an amino bisphosphonate prevents the resorptive phase of alveolar bone following mucoperiosteal flap surgery in rats. J Periodontol. 1997;68:884–889. doi: 10.1902/jop.1997.68.9.884. [DOI] [PubMed] [Google Scholar]
- 6.Shanbhag AS, Hasselman CT, Rubash HE. Inhibition of wear debris mediated ostelysis in a canine total hip arthroplasty model. Clin Orthop. 1997;344:33–43. [PubMed] [Google Scholar]
- 7.O’Hara LJ, Nivbrant B, Rohrl S. Cross-linked polyethylene and bisphosphonate therapy for osteolysis in total hip arthroplasty: a case report. J Orthop Surg. 2004;12:114–21. doi: 10.1177/230949900401200121. [DOI] [PubMed] [Google Scholar]
- 8.Rosenbaum TG, Bloebaum RD, Ashrafi S, Lester DK. Ambulatory Activities Maintain Cortical Bone after Total Hip Arthroplasty. Clin Orthop. 2006;450:129–137. doi: 10.1097/01.blo.0000223981.21584.35. [DOI] [PubMed] [Google Scholar]
- 9.Röder C, Staub LP, Eichler P, Widmer M, Dietrich D, Eggli S, Müller U. Avoiding misclassification bias with the traditional Charnley classification: rationale for a fourth Charnley class BB. J Orthop Res. 2006;24:1803–8. doi: 10.1002/jor.20224. [DOI] [PubMed] [Google Scholar]
- 10.Bhandari M, Bajammal S, Guyatt GH, Griffith L, Busse JW, Schunemann H, Einhorn TA. Effect of bisphosphonates on periprosthetic bone mineral density after total joint arthroplasty. A meta-analysis. J Bone Joint Surg Am. 2005;87:293–301. doi: 10.2106/JBJS.D.01772. [DOI] [PubMed] [Google Scholar]