Abstract
Objective
To identify the factors that can predict physicians’ use of electronic prescribing.
Design
All primary care physicians who practised in a single geographic region in Quebec were invited to use a free, advanced, research-based electronic prescribing and drug management system. This natural experiment was studied with an expansion of the Technology Acceptance Model (TAM), which was used to explain early adopters’ use of this electronic prescribing technology.
Setting
Quebec city region.
Participants
A total of 61 primary care physicians who practised in a single geographic region where there was no electronic prescribing.
Main outcome measures
Actual use of electronic prescribing; physicians’ perceptions of and intentions to use electronic prescribing; physician and practice characteristics.
Results
During the 9-month study period, 61 primary care physicians located in 26 practice sites used electronic prescribing to write 15 160 electronic prescriptions for 18 604 patients. Physician electronic prescribing rates varied considerably, from a low of 0 to a high of 75 per 100 patient visits, with a mean utilization rate of 30 per 100 patient visits. Overall, 34% of the variance in the use of electronic prescribing was explained by the expanded TAM. Computer experience (P = .001), physicians’ information-acquisition style (P = .01), and mean medication use in the practice (P = .02) were significant predictors. Other TAM factors that generally predict new technology adoption (eg, intention to use, perceived ease of use, and perceived usefulness) were not predictive in this study.
Conclusion
The adoption of electronic prescribing was a highly challenging task, even among early adopters. The insight that this pilot study provides into the determinants of the adoption of electronic prescribing suggests that novel physician-related factors (eg, information-acquisition style) and practice-related variables (eg, prevalence of medication use) influence the adoption of electronic prescribing.
Résumé
Objectif
Identifier les facteurs qui permettent de prévoir l’utilisation de la prescription électronique par les médecins.
Type d’étude
Tous les médecins de première ligne pratiquant dans une région géographique donnée du Québec ont été invités à utiliser gratuitement un système avancé de prescription électronique et de gestion des médicaments, fondé sur la recherche. Les résultats de cette expérience naturelle ont été analysés à l’aide d’une expansion du Technology Acceptance Model (TAM), lequel a servi à expliquer les raisons de l’utilisation de la technologie de la prescription électronique chez ceux qui l’avaient adoptée récemment.
Contexte
La ville de Québec et ses environs.
Participants
Un total de 61 médecins de première ligne qui pratiquaient dans une région donnée où il n’y avait pas de prescription électronique.
Principaux paramètres à l’étude
L’utilisation actuelle de la prescription électronique; la perception des médecins et leur intention de l’utiliser; les caractéristiques des médecins et des sites de pratique.
Résultats
Durant les 9 mois de l’étude, 61 médecins de première ligne situés dans 26 lieux de pratique ont utilisé la prescription électronique pour rédiger 15 160 prescriptions électroniques à l’intention de 18 604 patients. Les taux de prescription électronique variaient considérablement, entre un minimum de 0 et un maximum de 75 % visites de patients, la moyenne étant de 30 pour 100 visites. Globalement, 34 % de la variance pour l’utilisation de la prescription électronique était explicable par le TAM étendu. Une bonne expérience de l’ordinateur (P = ,001), un type de médecin favorable à l’acquisition d’information et le nombre moyen de médicaments utilisés dans la pratique (P = ,02) étaient des indices significatifs. Les autres facteurs TAM qui permettent généralement de prédire l’adoption des nouvelles technologies (c.-à-d. l’intention de s’en servir, l’impression de facilité d’utilisation et l’idée que c’est utile) n’étaient pas des indices dans cette étude.
Conclusion
L’adoption de la prescription électronique était une tâche particulièrement exigeante, même pour ceux qui venaient de l’adopter. Cette étude pilote permet de mieux comprendre les facteurs qui déterminent l’adoption de la prescription électronique et suggère que des facteurs nouveaux liés aux médecins (p. ex. un style favorable à l’acquisition d’information) ainsi que des variables liées à la pratique (p. ex. le nombre de médicaments utilisés) influencent l’adoption de la prescription électronique.
Large investments are made in information technology for health care based on the assumption that users will incorporate the technology into their daily work for improving patient safety, quality of care, and health care efficiency. In the United States (US), the American Recovery and Reinvestment Act of 2009 included funding of an estimated $36.5 billion to achieve the goal of giving all US patients access to electronic health records by 2014. Even if this act should result in an increase in new information technology projects, physicians’ adoption of the technology remains an important challenge. Widespread adoption of electronic health information technology (HIT) is largely lagging in North America.1,2 Various surveys on the adoption of HIT in different countries have established that primary care in the US and Canada are substantially behind in comparison with other leading countries such as the Netherlands and Australia.3–5
The situation is similar for electronic prescribing, which is one of the areas in which considerable gains in the quality and safety of patient care are expected.6,7 Prescribing and dispensing errors are among the most common types of preventable medication errors in general practice.8 Electronic prescribing can not only eliminate illegible prescriptions, but it can also enhance professional communication throughout the prescribing chain and increase access to patient information, evidence-based recommendations, and other decision-support modules.6,7 Yet, in 2006, only 11% of general practitioners in Canada and 20% in the US routinely used electronic prescribing.3 In 2009, these figures increased to 27% in Canada and 40% in the US, but both countries still occupied the lowest ranks when compared with a group of 11 countries.5
Roger’s theory of innovation diffusion9 identified that the success of new technologies is determined to a great extent by the acceptance by early adopters. These adopters are important because they act as opinion leaders and champions, and their enthusiasm about new technologies is critical to successful implementation.10 The expected proportion of early adopters of new technology according to Roger’s theory of innovation is estimated at 13.5%.9 However, it is very difficult to study the adoption process and the characteristics of early adopters in health care, as the population “exposed” to the uptake of new technology is difficult to define, and information on that population’s use is rarely accessible. We had the opportunity to perform a natural experiment in the introduction of electronic prescribing to a geographically defined population of primary care physicians, who had no previous experience with any form of HIT in their practices, to study the experience of early adopters and to identify the factors that influenced the physicians’ use of the technology.
To understand the factors that can predict early adopters’ use of electronic prescribing in primary care, we used an expansion of the Technology Acceptance Model (TAM),11,12 an analytical framework that is commonly used to explain adoption of information technology.13,14 The TAM is the most widely recognized model of behavioural intention in the information systems literature.13 It was derived from the theory of reasoned action. The theory of reasoned action is a very general model of behaviour that suggests beliefs influence attitudes, which determine intentions, and that intentions dictate behaviour.13 However, the TAM has not been extensively adapted to incorporate particular elements of medical practice, such as practice volume, continuity of care, and physicians’ attitudes toward use of information in decision making, that might influence the adoption of electronic prescribing. Therefore, to increase the potential explanatory power of the TAM, we expanded the model to incorporate these attributes. Further, we measured the actual use of electronic prescribing rather than self-reported use to minimize reporting bias.15
METHODS
Study context
In 2005, the Quebec Ministry of Health supported a pilot implementation of an advanced, research-based electronic prescribing and drug management system for the geographic region of Quebec city, Que. For this natural experiment, all primary care physicians in this area were given the opportunity to have access to free electronic prescribing hardware and software, as well as training and service support. These physicians had no previous HIT experience in their practices. The government’s plan was to introduce electronic prescribing and drug management as the first technology because it was expected that this technology would provide the greatest value to the first step in computerizing physicians’ practices. The medical office of the 21st century (MOXXI) system was selected, as it had the most advanced features to maximize clinical value and efficiency.16
With the MOXXI system, physicians are able to write prescriptions electronically and retrieve information on dispensed prescriptions and medical visits from the provincial and private health insurance programs.16 Data regarding dispensed medications are displayed in an electronic medication history that provides a graphic representation of the list of medications based on start and end dates of prescriptions, colour-coded by prescribing physician. It also provides information on emergency department visits and hospitalizations based on medical visit information from the health insurance program. There are also automated alerts that provide decision support in drug prescribing, as they flag dosing and duplication errors, potentially toxic drug-drug interactions and duplications, and possible drug-disease contraindications and allergic reactions.
Study population
The geographically defined population of 370 primary care physicians who were offered free technology by the government were identified by the public list of licensed physicians from the provincial medical regulatory authority. A letter of invitation was sent to all physicians briefly outlining the project and inviting them to attend an information session. Follow-ups with physicians were conducted to ascertain their interest in joining the project. After the information sessions, physicians who were interested in participating consented to provide usage, personal, and practice data for evaluation in the project. Extensive training and field support for the new electronic prescribing system was provided. Participating physicians represented the early adopters in a whole geographically defined population, as they were the first to volunteer to experiment with a technological innovation that was being introduced to all primary care physicians in the area. The use of electronic prescribing by these early-adopter physicians was studied during a 9-month study period (October 2005 to July 2006). The study was approved by the McGill University ethics committee.
Data sources
Three databases were used to measure physicians’ perceptions and intentions (the TAM main variables), identify physician characteristics and practice settings, and determine the use of electronic prescribing: the Régie de l’assurance maladie du Québec database of provincial health insurance beneficiaries and medical and pharmaceutical services (a population-based and single-payer information system that is thus highly comprehensive); the MOXXI application database; and the physician training and baseline questionnaire database. Using the provincial health insurance identifiers, data were reliably linked by unique identifiers for both patients and physicians.
Potential predictors
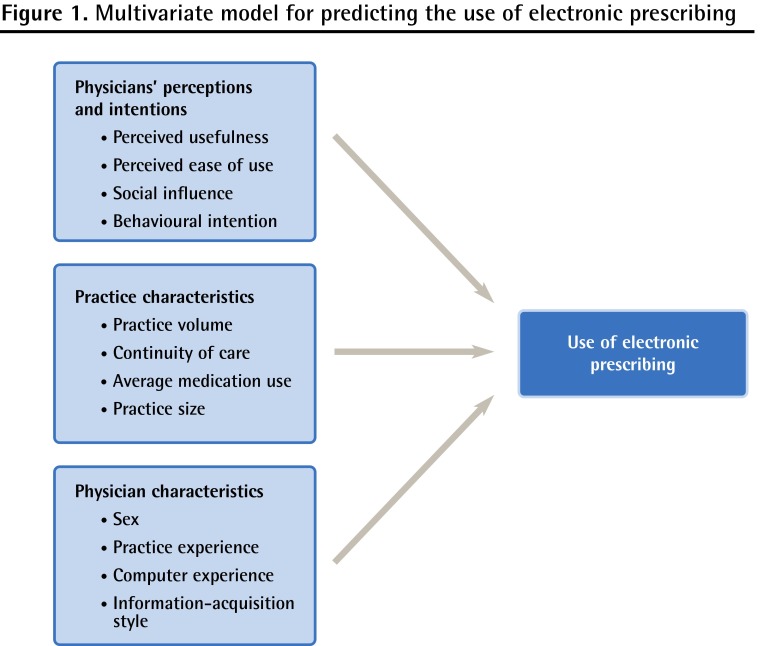
Three groups of variables were defined as having a potential effect on the use of electronic prescribing (Figure 1): physicians’ perceptions of and intentions to use the new information system, physician characteristics, and practice setting characteristics.
Figure 1.
Multivariate model for predicting the use of electronic prescribing
Physicians’ perceptions of and intention to use electronic prescribing
Previous research has reported substantial correlations between use of a new technology and the ease of use, perceived usefulness, social influence, and intention to use that new technology.13,14 Each physician completed a standard TAM questionnaire following the completion of training on the MOXXI system.16 Four variables were then created from physician responses: perceived usefulness (9 items), perceived ease of use (1 item), social influence (1 item), and intention to use electronic prescribing (1 item). All measures used a 5-point Likert scale with anchors ranging from “strongly disagree” to “strongly agree.” For perceived usefulness, the mean of all item responses was used to predict adoption.
Physician characteristics
Based on previous evidence that computer skills and youth were positively associated with technology adoption,15 we hypothesized that younger physicians would have stronger computer skills and would be more likely to adopt electronic prescribing tools. Physician sex, practice experience (defined as the number of years since the date of graduation from medical school), and computer experience (defined as self-reported hours per week of computer use) were measured by questionnaire. Also, we expected that a physician’s information-acquisition style might be a factor that could influence technology adoption.17 Previous research has suggested that physicians’ response styles to decision-support information about effective clinical strategies will likely differ as a function of what is considered to be a credible information source, the practicality of altering practice, and the level of comfort with practising in a manner that might be divergent from their peers.17 The information-acquisition style of physicians was assessed with a 17-item psychometric instrument (using a 5-point Likert scale) developed by Green et al.17 This instrument allowed us to classify physicians into 4 mutually exclusive categories: seeker, receptive, traditionalist, and pragmatist. Seekers and receptives are the most evidence-oriented profiles. The seekers collect, analyze, and respond to evidence-based information, while receptives rely on the judgment of respected others and might only translate evidence-based information into practice if it is sufficiently compelling. Traditionalists and pragmatists are less prone to the use of evidence-based information. Traditionalists tend to rely on clinical experience to guide their practice behaviour, while pragmatists view both experience and evidence as valid sources to guide practice in focusing on efficiency. We hypothesized that seekers and receptives would be intensive electronic prescribing users.
Practice characteristics
Four aspects of practice were hypothesized to predict the adoption of electronic prescribing.18 First, we expected that physicians with high-volume practices would have greater difficulty in adopting new technology, as available time for change would be at a premium. In contrast, we expected that physicians who had higher continuity of care and greater medication use in their practices would experience greater efficiencies by adopting electronic prescribing technology, as refills for patients on a greater number of medications would be more efficient—a factor that was important in determining adoption in the United Kingdom.19 Practice volume was measured as the mean daily number of patients seen based on the number of patient visits during the 18-month period before the study period, divided by the number of days worked during that same period. Practice size was also measured, defined as the sum of unique patients that visited the study physician during the 18-month period before study enrolment. Medication use in the practice population was measured as the mean medication use per patient. The number of different medications was counted for each patient, and the mean was calculated for all patients in the practice. Continuity of care was measured as the proportion of visits made to the study physician for each patient in the practice in the 18 months before the beginning of the study. The mean value was calculated for all patients in the practice. These 4 practice characteristics were measured using billing and prescribing data from each physician’s practice.
Physician adoption
To measure adoption, we used the rate of electronic prescriptions per 100 patient visits. Although not all patient visits led to a prescription, the electronic prescribing rate allowed us to derive a standard measure to compare physicians with different practice volumes. The denominator was defined as the number of visits made by patients during follow-up. The numerator was defined as the number of visits in which an electronic prescription was written for these patients. We thus used an actual rather than self-reported rate of usage.
Data analysis
Descriptive statistics were used to characterize potential predictors of usage. The relationship among potential predictors and the dependent variable was assessed using correlation analysis. Owing to the small sample size of participating physicians, we conducted 3 multivariate generalized linear models to estimate the R2 and F statistic for each of our 3 groups of potential predictor variables (ie, physicians’ perceptions and intention, physician characteristics, and practice setting characteristics) in relationship to usage. In conducting 3 separate multivariate analyses, the number of independent variables was kept sufficiently low to produce statistically valid analyses. This strategy allowed us to compare and appreciate the relative performance of each group of independent variables in explaining the variance in the use of electronic prescribing. To be able to correctly compare the respective explanatory power of each group of predictor variables, we used the adjusted R2. Finally, we attempted an exploratory multivariate analysis including all the independent variables in one sole model. The selection of the significant variables was then based on a stepwise procedure to adequately take into account the large number of independent variables. This last analysis was exploratory, aiming to provide an indication of potentially important predictors of the use of electronic prescribing for subsequent research. All data analyses were performed using SAS, version 9.1.
RESULTS
Of the 370 primary care physicians to whom the technology was offered, 61 (16%) of them volunteered to use the electronic prescribing technology in their practices. This proportion of physicians is very similar to the proportion of the group of early adopters of new technology (13.5%) predicted by Roger’s theory of innovation diffusion.9 Overall, 54% of study physicians were men, 49% had been in practice for 25 years or more, and 53% used a computer less than 5 hours per week (Table 1). Most physicians were classified as having a pragmatist approach (64%) in their information-acquisition style, followed by those who had a receptive approach (16%), seeker approach (15%), and traditional approach (5%). Practice sizes ranged from 19 to 3880 patients, with a mean practice size of 1840 patients. Overall, an average of 21 visits were made to the study physicians per working day. Mean practice medication use was 2.8 medications dispensed per patient. The mean baseline continuity of care index was 0.57, representing the proportion of visits to the study physician. At the beginning of the project, 54% of physicians strongly agreed that they intended to use the new electronic prescribing application for most of their patients, and approximately 50% of participating physicians strongly agreed that the new electronic prescribing application would be useful.
Table 1.
Descriptive statistics and linear regression model for predicting use of electronic prescribing
| PREDICTORS | DESCRIPTIVE STATISTICS AND CORRELATIONS | LINEAR REGRESSION MODEL TO PREDICT USAGE | |||||
|---|---|---|---|---|---|---|---|
|
|
|
||||||
| MEAN (SD) | MINIMUM | MAXIMUM | CORRELATION WITH USAGE | ESTIMATE | 95% CI | P VALUE | |
| Physicians’ perceptions and intentions | |||||||
| Perceived usefulness* | |||||||
| • Average score of usefulness† | 4.26 (0.51) | 3 | 5 | 0.08 | 0.03 | −0.06 to 0.12 | .57 |
| Perceived ease of use | |||||||
| • MOXXI will be easy to use | 4.13 (0.69) | 2 | 5 | 0.19 | 0.05 | −0.02 to 0.12 | .14 |
| Social influence | |||||||
| • Colleagues’ attitudes will be positive toward my use of MOXXI | 4.08 (0.61) | 3 | 5 | 0.11 | 0.03 | −0.04 to 0.11 | .40 |
| Intention to use | |||||||
| • I will use MOXXI with most of my patients | 4.49 (0.62) | 2 | 5 | −0.02 | 0.00 | −0.08 to 0.07 | .90 |
| Physician characteristics | |||||||
| Male sex‡ | NA | NA | NA | 0.19 | 0.07 | −0.02 to 0.16 | .15 |
| Practice experience | |||||||
| • Graduation year | 1982 (7.55) | 1965 | 1999 | −0.17 | −0.004 | −0.010 to 0.002 | .18 |
| Physician typology§ | |||||||
| • Pragmatist | NA | NA | NA | 0.18 | 0.07 | −0.03 to 0.16 | .17 |
| • Receptive | NA | NA | NA | 0.10 | −0.07 | −0.20 to 0.06 | .26 |
| • Seeker | NA | NA | NA | −0.15 | 0.05 | −0.08 to 0.17 | .44 |
| Previous computer experience | |||||||
| • No. of hours per week of computer use | 5.67 (6.37) | 0 | 30 | 0.45 | 0.01 | 0.01 to 0.02 | < .001 |
| Practice characteristics | |||||||
| Continuity of care|| | 0.57 (0.09) | 0 | 1 | −0.08 | −0.17 | −0.69 to 0.35 | .52 |
| Average medication use¶ | 2.84 (0.83) | 1 | 5 | 0.30 | 0.07 | 0.01 to 0.12 | .02 |
| Practice size | 1840 (877) | 19 | 3880 | −0.17 | 0.00 | 0.00 to 0.00 | .20 |
| Practice volume# | 20.74 (7.26) | 2 | 42 | −0.17 | 0.00 | −0.01 to 0.00 | .19 |
MOXXI—medical office of the 21st century, NA—not applicable.
Cronbach α = .90.
Average score of usefulness is average of scores of 9 questions coming from perceived usefulness: 1) electronic prescribing will be useful; 2) electronic prescribing will make work easier; 3) electronic prescribing will have a beneficial effect on quality of patient care; 4) electronic prescribing will increase my professional satisfaction; 5) electronic prescribing will have a beneficial communication with other health care professionals; 6) electronic prescribing will improve continuity of care; 7) electronic prescribing will increase my professional autonomy; 8) electronic prescribing will increase patients’ satisfaction; and 9) electronic prescribing will have a minimal effect on depersonalizing patient care.
Female sex was used as reference category.
Traditionalist was used as reference category.
Proportion of visits made to study physician for each patient in the practice in the 18 months before the study.
No. of medications was counted for each patient in the 18 months before the study.
Daily no. of patients seen based on the no. of patient visits during the 18 months before the study divided by the no. of days worked during that same period.
During the 9-month study period (October 2005 to July 2006), 15 160 electronic prescriptions were written for 18 604 consenting patients. Physician electronic prescribing rates varied considerably, from a low of 0, to a high of 75 per 100 patient visits, with a mean (SD) utilization rate of 30 (8.1) per 100 patient visits. In relation to physician characteristics, the highest utilization rates were for male physicians (0.33); physicians with more than 34 years of practice experience (0.44); receptives (0.34) and pragmatists (0.33); physicians with more than 10 hours of computer use per week (0.41); physicians with mean practice sizes of less than 1500 patients (0.35); and physicians with patients with an average of 3 or more medications (0.36). Higher utilization rates were seen for physicians who strongly believed electronic prescribing would improve continuity of care (0.33), provide professional autonomy (0.36), be useful (0.34), be easy to use (0.40), make work easier (0.36), and be viewed positively by colleagues (0.36).
Two multivariate models had weak explanatory power (Table 2). Indeed, physicians’ perceptions and intentions and their practice settings only explained 5% and 12% (unadjusted R2), respectively, of the variance in the use of electronic prescribing. Only the mean medication use was significant (P = .02). The third model, physician characteristics, was far more successful in explaining 34% of the variance. Computer experience (P = .001) and information-acquisition style (P = .01) were the 2 significant variables.
Table 2.
Three multivariate models to predict use of electronic prescribing: A) Parameters of physicians’ perceptions and intentions; B) Parameters of practice characteristics; C) Parameters of physician characteristics.
| A) PHYSICIANS’ PERCEPTIONS AND INTENTIONS* |
PERCEIVED USEFULNESS + PERCEIVED EASE OF USE + SOCIAL INFLUENCE + BEHAVIOURAL INTENTION
|
||
| ESTIMATE | 95% CI | P VALUE | |
|
| |||
| Intercept | 0.22 | −0.26 to 0.70 | .36 |
| Perceived usefulness | |||
| • Average score of usefulness | −0.02 | −0.14 to 0.09 | .72 |
| Perceived ease of use | |||
| • MOXXI will be easy to use | 0.06 | −0.03 to 0.16 | .19 |
| Social influence | |||
| • Colleagues’ attitudes will be positive toward my use of MOXXI | 0.01 | −0.09 to 0.10 | .85 |
| Behavioural intention | |||
| • I will use MOXXI with most of my patients | −0.03 | −0.11 to 0.05 | .50 |
| B) PRACTICE CHARACTERISTICS† |
PRACTICE VOLUME + CONTINUITY OF CARE + MEDICATION USE + PRACTICE SIZE
|
||
| ESTIMATE | 95% CI | P VALUE | |
|
| |||
| Intercept | 0.20 | −0.17 to 0.57 | .28 |
| Practice volume‡ | 0.00 | −0.01 to 0.01 | .34 |
| Continuity of care§ | −0.12 | −0.72 to 0.48 | .68 |
| Average medication use|| | 0.08 | 0.01 to 0.14 | .02 |
| Practice size¶ | 0.00 | 0.00 to 0.00 | .52 |
| C) PHYSICIAN CHARACTERISTICS# |
AGE + SEX + INFORMATION-ACQUISITION STYLE + COMPUTER EXPERIENCE
|
||
| ESTIMATE | 95% CI | P VALUE | |
|
| |||
| Intercept | 0.07 | −0.55 to 0.68 | .83 |
| Practice experience | |||
| • Graduation year | −0.001 | −0.01 to 0.01 | .77 |
| Sex** | |||
| • Male | 0.03 | −0.07 to 0.14 | .53 |
| Physician typology†† | |||
| • Pragmatist | 0.26 | 0.08 to 0.45 | .01 |
| • Seeker | 0.16 | −0.05 to 0.36 | .13 |
| • Receptive | 0.26 | 0.06 to 0.47 | .01 |
| Computer experience | |||
| • Hours per week of computer use | 0.01 | 0.005 to 0.02 | .001 |
MOXXI—medical office of the 21st century.
R2 = 0.05; adjusted R2 = 0.02.
R2 = 0.12; adjusted R2 = 0.06.
Daily no. of patients seen based on the no. of patient visits during the 18 months before the study.
Proportion of visits made to study physician for each patient in the practice in the 18 months before the study.
No. of medications was counted for each patient in the 18 months before the study.
Unique patients that visited the study physician during the 18 months before study enrolment.
R2 = 0.34; adjusted R2 = 0.27.
Female sex was reference category.
Traditionalist was reference category.
These results were confirmed by the exploratory multivariate analysis (Table 3). The explanatory power of the model reached 37% with 3 significant variables: computer experience (P = .001), information-acquisition style (P = .001, P = .003, P = .06), and mean medication use (P = .01).
Table 3.
Exploratory multivariate model with all variables: Variables selected by stepwise procedure; R2 = 0.42; adjusted R2 = 0.37.
| VARIABLES |
MULTIPLE REGRESSION, WITH VARIABLES DETERMINED BY STEPWISE SELECTION PROCEDURE
|
||
|---|---|---|---|
| ESTIMATE | 95% CI | P VALUE | |
| Intercept | −0.22 | −0.44 to 0.01 | .06 |
| Hours per week of computer use | 0.01 | 0.005 to 0.02 | .001 |
| Medication use | 0.07 | 0.02 to 0.11 | .01 |
| Pragmatist versus others | 0.30 | 0.12 to 0.47 | .001 |
| Receptive versus others | 0.30 | 0.11 to 0.49 | .003 |
| Seeker versus others | 0.18 | −0.01 to 0.38 | .06 |
DISCUSSION
The goal of this research was to understand the factors that can predict early adopters’ use of electronic prescribing technology in primary care. There were 4 main findings. First, utilization rates of electronic prescribing were highly variable. This finding suggests that, even among early adopters, adoption is not an easy task. It seems that early adopters are not as homogeneous of a group as one might have thought. Such variability means that adoption of electronic prescribing is a real challenge, even among early adopters who are usually the most motivated to adopt new technology. Because of the crucial role of early adopters in technology diffusion, thoughtful strategies are needed to ensure adoption and use of electronic prescribing among this crucial group of users.
The second finding was the lack of importance of the usual TAM factors (ie, perceived usefulness, perceived ease of use, and behavioural intention) that generally predict new technology use, including among physicians.13,14 Two reasons might explain such discrepancy. First, it is possible that, among early adopters, the usual TAM factors score high, as we observed, and remain useless to discriminate and predict utilization rates. Second, it is also possible that our results are different because we studied actual use of the technology, while most of the TAM studies look at physician behavioural intention.17 However, it is important to emphasize that we were still able to reach an explanatory power similar to that of what is usually observed in TAM studies (30% to 40%).14
Another important finding was that information-acquisition style was able to predict use of electronic prescribing. The information-acquisition style provides new insight into the determinants of the adoption of electronic prescribing. This result suggests that knowledge of physicians’ information-acquisition style provides a means of predicting which individuals are more likely to be successful in adopting electronic prescribing. This finding suggests that the successful integration of electronic prescribing into the day-to-day practice of physicians will require a better understanding of how to present new information in electronic modes to enhance adoption and change physician practice patterns. From the same perspective, the finding that previous computer experience had a positive influence on usage is consistent with published research,15 and can be helpful in building more successful implementation strategies. It underlines the importance of carefully choosing users who have previous computer experience. Thus, the selection of physicians who are more likely to adopt a new technology is vital if early adopters are to successfully blaze the trail for HIT diffusion.
The last important finding showed that the intensity of medication use predicted the use of electronic prescribing. The hypothesis that electronic prescribing would be of greater interest to physicians who had patients with higher rates of medication use was confirmed by our results.18 To further physicians’ acceptance, electronic prescribing applications should emphasize the value-added benefits, such as prescription refills and access to the current list of dispensed medications, that should improve both practice efficiency and patient safety.
Limitations
This pilot study has limitations that need to be considered in the interpretation of results. First, 61 physicians participated in the experiment. Even if 16% of the population corresponded to the usual proportion of early adopters among a population of users according to the diffusion theory,9 the small sample size meant there were some constraints on conducting the statistical analysis that were overcome by testing 3 separate multivariate models. Future research should be conducted with larger samples in order to validate the findings derived from the present sample. Second, this pilot study was conducted in a single jurisdiction. Further investigation should explore other jurisdictions. Third, the participating physicians were spread among a large number of practice settings and were thus rather isolated. It is possible that their use of electronic prescribing would have been higher with more support from colleagues and their respective organizations.
Conclusion
Electronic prescribing applications are seen as a potential way to provide valuable benefits in terms of overall efficiency, patient safety, quality of care, and productivity in primary care. While enthusiasm has been expressed over the ability of electronic prescribing to achieve such goals, its successful deployment remains a highly challenging task, even among early adopters as this pilot study has revealed. We hope that the new theoretical and practical insights provided herein will shed light on the management of implementation projects for electronic prescribing, and will lead to further research on the implications of electronic prescribing that will overcome some of the limitations in this study.
EDITOR’S KEY POINTS
Although electronic prescribing can improve the quality and safety of patient care, its widespread adoption is largely lagging in North America.
Three groups of variables were defined as having a potential effect on the use of electronic prescribing: physicians’ perceptions of and intentions to use the new information system, physician characteristics, and practice setting characteristics. Within those variables, significant predictors of early adopters’ use of electronic prescribing were computer experience (P = .001), information-acquisition style (P = .01), and mean medication use in the practice (P = .02).
Knowledge of physicians’ information-acquisition styles (ie, pragmatist, receptive, seeker, or traditionalist approaches) is important, as the successful integration of electronic prescribing into the day-to-day practice of physicians will require a better understanding of how to present new information in electronic modes to enhance adoption and change physician practice patterns.
POINTS DE REPÈRE DU RÉDACTEUR
Même si l’utilisation de la prescription électronique peut améliorer la qualité et la sécurité des soins, son adoption tarde de façon importante en Amérique du Nord.
On a identifié trois groupes de variables susceptibles d’influencer l’utilisation de la prescription électronique : l’opinion du médecin sur les nouveaux systèmes d’information et son intention de les utiliser, les caractéristiques du médecin et celles du contexte de pratique. Parmi ces variables, les indices significatifs de l’utilisation de la prescription électronique par ceux qui l’avaient adoptée récemment étaient : une bonne expérience de l’ordinateur (P = ,001), un style favorable à l’acquisition d’information (P = ,01) et le nombre moyen de médicaments utilisés dans la pratique (P = ,02).
Les connaissances sur les types d’acquisition de l’information par les médecins (c.-à-d. des démarches pragmatiques, réceptives, de chercheur ou traditionnelles) sont importantes, puisque l’intégration réussie de la prescription électronique dans la pratique quotidienne des médecins demandera une meilleure compréhension de la façon de présenter la nouvelle information sous des formes électroniques afin d’en accroître l’adoption et de modifier les modèles de pratique des médecins.
Footnotes
This article has been peer reviewed.
Cet article a fait l’objet d’une révision par des pairs.
Contributors
All authors contributed to the concept and design of the study; data gathering, analysis, and interpretation; and preparing the manuscript for submission.
Competing interests
None declared
References
- 1.Jha AK, DesRoches CM, Campbell EG, Donelan K, Rao SR, Ferris TG, et al. Use of electronic health records in U.S. hospitals. N Engl J Med. 2009;360(16):1628–38. doi: 10.1056/NEJMsa0900592. [DOI] [PubMed] [Google Scholar]
- 2.DesRoches CM, Campbell EG, Rao SR, Donelan K, Ferris TG, Jha AK, et al. Electronic health records in ambulatory care—a national survey of physicians. N Engl J Med. 2008;359(1):50–60. doi: 10.1056/NEJMsa0802005. Epub 2008 Jun 18. [DOI] [PubMed] [Google Scholar]
- 3.Schoen C, Osborn R, Huynh PT, Doty M, Peugh J, Zapert K. On the front lines of care: primary care doctors’ office systems, experiences, and views in seven countries. Health Aff (Millwood) 2006;25(6):w555–71. doi: 10.1377/hlthaff.25.w555. Epub 2006 Nov 2. [DOI] [PubMed] [Google Scholar]
- 4.Jha AK, Doolan D, Grandt D, Scott T, Bates DW. The use of health information technology in seven countries. Int J Med Inform. 2008;77(12):848–54. doi: 10.1016/j.ijmedinf.2008.06.007. Epub 2008 Jul 25. [DOI] [PubMed] [Google Scholar]
- 5.Schoen C, Osborn R, Doty MM, Squires D, Peugh J, Applebaum S. A survey of primary care physicians in eleven countries, 2009: perspectives on care, costs, and experiences. Health Aff (Millwood) 2009;28(6):w1171–83. doi: 10.1377/hlthaff.28.6.w1171. Epub 2009 Nov 2. [DOI] [PubMed] [Google Scholar]
- 6.Schade CP, Sullivan FM, de Lusignan S, Madeley J. E-prescribing, efficiency, quality: lessons from the computerization of UK family practice. J Am Med Inform Assoc. 2006;13(5):470–5. doi: 10.1197/jamia.M2041. Epub 2006 Jun 23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Garg AX, Adhikari NK, McDonald H, Rosas-Arellano MP, Devereaux PJ, Beyene J, et al. Effects of computerized clinical decision support systems on practitioner performance and patient outcomes: a systematic review. JAMA. 2005;293(10):1223–38. doi: 10.1001/jama.293.10.1223. [DOI] [PubMed] [Google Scholar]
- 8.Dovey SM, Phillips RL, Green LA, Fryer GE. Types of medical errors commonly reported by family physicians. Am Fam Physician. 2003;67(4):697. [PubMed] [Google Scholar]
- 9.Rogers EM. Diffusion of innovations. 5th ed. New York, NY: Free Press; 2005. [Google Scholar]
- 10.Ash JS, Stavri PZ, Dykstra R, Fournier L. Implementing computerized physician order entry: the importance of special people. Int J Med Inform. 2003;69(2–3):235–50. doi: 10.1016/s1386-5056(02)00107-7. [DOI] [PubMed] [Google Scholar]
- 11.Davis FD. Perceived usefulness, perceived ease of use, and user acceptance of information technology. Manage Inf Syst Q. 1989;13(3):319–40. [Google Scholar]
- 12.Venkatesh V, Morris MG, Davis GB, Davis FD. User acceptance of information technology: toward a unified view. Manage Inf Syst Q. 2003;27(3):425–78. [Google Scholar]
- 13.Yarbrough AK, Smith TB. Technology acceptance among physicians: a new take on TAM. Med Care Res Rev. 2007;64(6):650–72. doi: 10.1177/1077558707305942. Epub 2007 Aug 23. [DOI] [PubMed] [Google Scholar]
- 14.Holden RJ, Karsh BT. The technology acceptance model: its past and its future in health care. J Biomed Inform. 2010;43(1):159–72. doi: 10.1016/j.jbi.2009.07.002. Epub 2009 Jul 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Taylor S, Todd P. Assessing IT usage: the role of prior experience. Manage Inf Syst Q. 1995;19(4):561–670. [Google Scholar]
- 16.Tamblyn R, Huang A, Kawasumi Y, Bartlett G, Grad R, Jacques A, et al. The development and evaluation of an integrated electronic prescribing and drug management system for primary care. J Am Med Inform Assoc. 2006;13(2):148–59. doi: 10.1197/jamia.M1887. Epub 2005 Dec 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Green LA, Gorenflo DW, Wyszewianski L. Validating an instrument for selecting interventions to change physician practice patterns: a Michigan Consortium for Family Practice Research study. J Fam Pract. 2002;51(11):938–42. [PubMed] [Google Scholar]
- 18.Simon SR, Kaushal R, Cleary PD, Jenter CA, Volk LA, Poon EG, et al. Correlates of electronic health record adoption in office practices: a statewide survey. J Am Med Inform Assoc. 2007;14(1):110–7. doi: 10.1197/jamia.M2187. Epub 2006 Oct 26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Protti D, Wright G, Treweek S, Johansen I. Primary care computing in England and Scotland: a comparison with Denmark. Inform Prim Care. 2006;14(2):93–9. doi: 10.14236/jhi.v14i2.619. [DOI] [PubMed] [Google Scholar]