Abstract
Objective
To investigate family physicians’ knowledge of, attitudes toward, and understanding of urinary incontinence (UI), as well as their perceptions of barriers to continence care, as a foundation for designing interventions to improve service provision for those in northern Alberta who suffer from UI.
Design
Descriptive survey using a standardized instrument. The survey instrument was completed either by telephone interview or on paper copy faxed back to the researchers, depending on participant preference.
Setting
Northern Alberta.
Participants
Random sample of family physicians (N = 158).
Main outcome measures
Physician knowledge of and attitudes toward UI, UI management practices, and barriers to providing UI care.
Results
Survey response rate was 10.6% (158 of 1488); 84.2% (133 of 158) of respondents practised in urban settings, 44.9% (71 of 158) had been in practice for fewer than 15 years, 24.1% (38 of 158) reported having no training in UI management since graduation, and 53.8% (85 of 158) reported that they proactively discussed UI with their patients. Overall, 70.0% of respondents felt fairly confident in managing UI. Most family physicians referred patients for specialist care, with few referrals to community services. Respondents thought that continence services were scarce, with long waiting times, and that such services were generally overstretched; they believed that although high-quality continence care was a personal priority, it was not a priority focus for their practice partnerships or networks. In terms of the highest ranked areas for improvement in UI management, increased awareness and understanding among physicians (ranked first by 28.5% of respondents), followed by dedicated incontinence clinics or nurses for referral (17.7%) and improving patient awareness and understanding (12.0%).
Conclusion
There continues to be considerable variation in knowledge about UI management and a relative overreliance on specialist care, despite well recognized difficulties in gaining access to services. Respondents believed that increased awareness among patients and health care providers coupled with greater access to continence services were key factors in improving care delivery.
Résumé
Objectif
Déterminer les connaissances des médecins de famille sur l’incontinence urinaire (IU), leur attitude et leur compréhension à l’égard de ce problème, de même que leur perception des obstacles au traitement de l’incontinence, comme première étape menant à l’instauration d’interventions pour améliorer les services aux personnes du nord de l’Alberta qui souffrent d’IU.
Type d’étude
Enquête descriptive à l’aide d’un document standardisé. Le document d’enquête a été complété soit par interview téléphonique ou par copie papier devant être retourné aux chercheurs par télécopieur, selon le choix des participants.
Contexte
Le nord de l’Alberta.
Participants
Un échantillon aléatoire de médecins de famille (N = 158).
Principaux paramètres à l’étude
Connaissances et attitudes des médecins au sujet de l’IU, leur façon de traiter ce problème et les obstacles à son traitement.
Résultats
Le taux de réponse à l’enquête était de 10,6 % (158 sur 1488); 133 répondants (84,2 %) pratiquaient en milieu urbain, 71 (44,9 %) étaient en pratique depuis moins de 15 ans, 38 (24,1 %) déclaraient n’avoir eu aucune formation sur le traitement de l’IU depuis leur diplomation et 85 (53,8 %) mentionnaient qu’ils discutaient de l’UI de façon proactive avec leurs patients. Globalement, 70,0 % des répondants se disaient plutôt à l’aise pour traiter l’IU. La plupart des médecins de famille confiaient leurs patients à des spécialistes pour le traitement, quelques-uns les dirigeant vers des services communautaires. Les répondants croyaient que les services de continence étaient rares et avaient de longs temps d’attente, et que ce type de service était généralement surchargé; ils croyaient que bien que les soins de continence de grande qualité soient une priorité personnelle, ce n’était pas une question prioritaire pour leurs réseaux et partenaires de pratique. Quant aux aspects du traitement de l’IU à améliorer les plus souvent mentionnés étaient les connaissances et la compréhension des médecins (classés premiers par 28,5 % des répondants), suivis des cliniques ou des infirmiers spécialisés en incontinence (17,7 %) et de l’amélioration des connaissances et de la compréhension des patients (12 %).
Conclusion
Il continue d’y avoir des variations considérables dans la connaissance du traitement de l’IU ainsi qu’une certaine tendance à trop compter sur les spécialistes pour le traitement, même si la difficulté d’accès à ces services est bien connue. Les répondants étaient d’avis qu’une amélioration des connaissances des patients et des soignants jumelée à un accès plus facile à des services de continence constituait un facteur clé pour améliorer la prestation des services.
Urinary incontinence (UI) and lower urinary tract symptoms (LUTS) are common and are a great cause of distress for many women and men of all ages.1 According to the 2006 EPIC (European Prospective Investigation into Cancer and Nutrition) study, conducted in 5 different countries including Canada, LUTS are highly prevalent in men (62.5%) and women (66.6%) aged 40 years and older.2 These conditions are associated with adverse effects on quality of life and work productivity.3 Incontinence in later life is further associated with substantial morbidity, an increased likelihood of institutionalization, and in some cases mortality.4–6 Despite this, those who suffer from UI and LUTS often fail to properly communicate their symptoms and concerns to their family physicians, who are the first point of contact for most patients.7 Many are reluctant to discuss such a stigmatizing condition with their physicians out of embarrassment, but also because they lack knowledge about the condition and its available treatments.8,9 Older people also delay seeking health care for these reasons.10
Lagace and colleagues found that 72.0% of those currently afflicted with UI had not spoken to physicians about the problem, while 37.0% indicated that they would have sought care if they had been aware of the available tests and effective treatments.11 Men and women seeking incontinence help often exhibit similar attitudes toward their symptoms, although Irwin and colleagues2 found that men aged 50 years and older with overactive bladder conditions were more likely than women with such conditions (82.7% vs 64.8%) to seek health care. Women in particular often believe that incontinence is an inevitable consequence of childbirth and aging, as only 9% of incontinent women ever consult health professionals about the problem.12
Although the reluctance of patients to openly discuss their urinary symptoms serves as a barrier to providing treatment, UI often remains unaddressed because of a lack of awareness among health care professionals and care providers.12 It is expected that family physicians should be able to diagnose and manage most problems with UI, but many Canadian family physicians believe they are unprepared to deal with UI. Indeed, in a 2002 national survey, differentiating types of incontinence was reported as difficult by almost two-thirds of family physicians, and managing incontinence was considered by 60.0% of respondents to be a difficult task.12 There remain limited data concerning the attitudes and practices of family physicians around UI in Canada. In the 2002 survey, less than half of family physicians indicated that they clearly understood incontinence, and just 37.9% identified having an organized plan for continence issues. Because of the nature of the problem, the changing demographic characteristics of the Canadian population in terms of aging, and the expected increasing demands from the baby boomers for services and care,13 there is a need to establish the current level of knowledge and awareness of, practice patterns for, and attitudes toward incontinence and LUTS among family physicians. The purpose of this study was to assess family physicians’ attitudes toward and knowledge and management patterns of UI, with the eventual aim of designing interventions to improve service provision for those suffering with UI in northern Alberta.
METHODS
Design
A cross-sectional survey, using a randomly selected sample of family physicians practising in Edmonton, Alta, was designed. Family physicians were selected from the publicly available directory published by the College of Physicians and Surgeons of Alberta using a computer-generated random-number list. We used a standardized survey developed for physicians that had been used to assess the same topic across 4 European countries,14 adapted for language and terms familiar to Canadian physicians. The survey has been validated for content only. Ethical committee approval was gained from the Health Research Ethics Board of the University of Alberta.
Data collection and analysis
The survey was designed for telephone administration, and potential participants were contacted between July and November 2011. Owing to low initial rates of participation, physicians who had given their consent to participate were sent the survey by fax, and the list of physicians to be contacted was expanded to include those located in the entire northern Alberta region. An honorarium of $50 was offered for completion and return of the survey. No identifying information was retained following payment of the incentive. Recruitment continued until the desired sample size of 150 family physicians was reached.
RESULTS
Demographic data and key results are shown in Table 1. Of 1488 family practitioners contacted, only 10.6% (158 of 1488) participated in the survey. Of these, 9 completed the questionnaire via telephone and 149 completed it via fax. Quality of the data was high, with only 1.5% of total data items missing. No nonrespondent analysis was performed. On average, respondents estimated that a median 11.2% (range 0% to 90%) of the patients they had seen in the past 3 months experienced problems with UI. Only 18.4% (29 of 158) indicated that they had last received formal training or instruction in the assessment or management of people with UI within the past year; 43.0% (68 of 158) had last received training more than 5 years ago; and 24.1% (38 of 158) had had no training or instruction since medical school. Physicians were asked about the extent to which they believed specified conditions (Table 2) had an effect on quality of life. Urinary incontinence was thought to affect quality of life to some extent or a great extent by 85.5% of physicians, ranking behind depression, arthritis, and chronic pain.
Table 1.
Demographic characteristics and key responses of respondents: N = 158.
| CHARACTERISTIC | VALUE |
|---|---|
| Male sex, n (%) | 81 (51.3) |
| Urban practice location, n (%) | 133 (84.2) |
| Mean (SD) time in practice, y | 11.0 (17.4) |
| Fewer than 15 y in practice, n (%) | 71 (44.9) |
| Median estimated patients seen in previous 3 mo (95% CI) | 1458 (524–2392) |
| Use of integrated care pathway, n (%) | 41 (25.9) |
| Confidence in management of UI, n (%) | |
| • Very confident | 10 (6.3) |
| • Fairly confident | 109 (69.0) |
| • Not at all confident | 39 (24.7) |
| Management of continence in past 2 y, n (%) | |
| • Improved | 59 (37.3) |
| • Same | 95 (60.1) |
| • Worse | 2 (1.3) |
UI—urinary incontinence.
Table 2.
The extent to which family physicians thought different conditions affected their patients’ quality of life: N = 158.
| PATIENT CONDITION |
PHYSICIAN RESPONSE, N (%)
|
||||
|---|---|---|---|---|---|
| TO A GREAT EXTENT | TO SOME EXTENT | HARDLY AT ALL | NOT AT ALL | DON’T KNOW | |
| Arthritis | 114 (72.2) | 27 (17.1) | 4 (2.5) | 13 (8.2) | 0 (0.0) |
| Chronic pain | 115 (72.8) | 23 (14.6) | 7 (4.4) | 13 (8.2) | 0 (0.0) |
| Dermatitis | 9 (5.7) | 105 (66.5) | 37 (23.4) | 6 (3.8) | 1 (0.6) |
| Incontinence | 68 (43.0) | 67 (42.4) | 11 (7.0) | 12 (7.6) | 0 (0.0) |
| Menopause | 26 (16.5) | 106 (67.1) | 21 (13.3) | 5 (3.2) | 0 (0.0) |
| Depression | 110 (69.6) | 32 (20.3) | 2 (1.3) | 13 (8.2) | 0 (0.0) |
| Erectile dysfunction | 28 (17.7) | 97 (61.4) | 22 (13.9) | 7 (4.4) | 4 (2.5) |
When asked to identify and rank factors that placed people at risk of UI, respondents ranked age, and pregnancy, parity, and parturition disorders as being the most important (Figure 1). Among the 158 participants, 53.8% (85 of 158) indicated that they proactively discussed incontinence with most or all of the patients they suspected had incontinence problems; 29.7% (47 of 158) indicated that they proactively discussed incontinence with some of their patients, and 15.2% (24 of 158) indicated that they did not discuss incontinence with anyone unless the patients raised the issue themselves. After initial management, such as providing lifestyle advice, prescribing medication, recommending incontinence products, or providing referral to specialists, 78.5% (124 of 158) of physicians sometimes, if not always, arranged follow-up appointments specifically to deal with the incontinence; 21.5% (34 of 158) rarely if ever arranged follow-up. Reasons for lack of confidence in management included concerns about the level of training, drug side effects, a lack of support services in the area, and the general embarrassment around UI.
Figure 1.
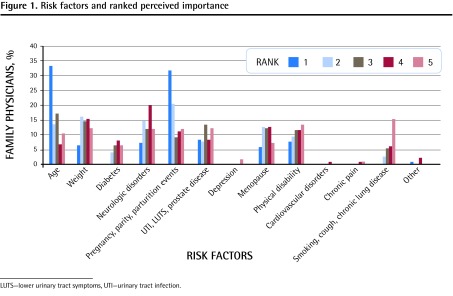
Risk factors and ranked perceived importance
LUTS—lower urinary tract symptoms, UTI—urinary tract infection.
Figure 2 shows the distribution and variety of allied health professionals, if any, that respondents referred their patients to for the management of incontinence. When asked about the extent to which they agreed with the statement that “support and care services for UI were easy to access,” 15.8% (25 of 158) strongly disagreed, 26.6% (42 of 158) disagreed, 23.4% (37 of 158) either agreed or strongly agreed, and 29.7% (47 of 158) had no opinion. Sixty-nine (43.7%) family physicians either strongly disagreed or disagreed that the current range of continence care and support services was adequate for their patients needs; only 22.8% (36 of 158) were in agreement, and 62.7% (99 of 158) of respondents thought that the currently available services were overloaded. When asked to what extent they believed their patients were satisfied with the management options currently available for incontinence, 46.2% (73 of 158) indicated that their patients were very to fairly satisfied with the options; 41.1% (65 of 158) reported that their patients were not very or not at all satisfied with the offered resources, and 5.1% had not asked their patients.
Figure 2.
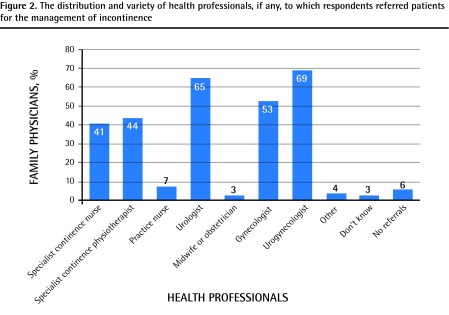
The distribution and variety of health professionals, if any, to which respondents referred patients for the management of incontinence
In total, 70.9% (112 of 158) of family physicians reported that improving the treatment and management of patients with incontinence was a fairly high if not a high priority to them personally, with 25.9% (41 of 158) reporting it to be either a fairly low or a low priority. When asked about the priority of improving continence care within the context of their office or institutional practice, 62.7% (99 of 158) believed that it was a very high to fairly high priority, while 32.9% (52 of 158) reported continence to be a low or very low priority.
The top ranked factors that respondents thought would contribute to improved management of continence problems included increasing awareness and understanding of incontinence among physicians (ranked first by 28.5% of respondents) and patients (12.0%), and ensuring dedicated referral resources (incontinence clinics or nurses) were available (17.7%). Barriers to the management of UI are shown in Figure 3. Respondents identified lack of awareness among patients and care providers along with inadequate services to which their patients could be referred as important barriers. In terms of physicians’ expectations of advancements in the treatment of incontinence within the next 2 years, 45.6% (72 of 158) expected to see some improvements, 27.2% (43 of 158) believed that there would hardly be any change, and 7.6% (12 of 158) expected great advancement.
Figure 3.
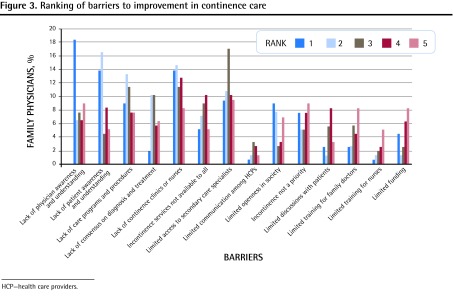
Ranking of barriers to improvement in continence care
HCP—health care providers.
DISCUSSION
Urinary incontinence is a common condition, with a demonstrable effect on everyday life. Despite the high prevalence of UI, many respondents in this study estimated the frequency to be low. In total, 67.1% of responding physicians had received no training on UI and its management within 5 years, and approximately a third of these had received none since medical school. Although most respondents did not think it was a main cause of impairment of quality of life or associated morbidity, they did recognize that UI did certainly have an effect on patients’ lives. In our study, family physicians were able to identify some of the common risk factors associated with the development of UI, but important factors such as depression and diabetes were not identified as risk factors for UI, similar to the findings of other published studies.15–20 These common risk factors are shown in Box 1. Most respondents reported that they proactively asked their patients about incontinence; a case-finding question is certainly recommended in international guidelines, owing to the prevalence of the condition.21,22 Data from a national audit of continence care in the United Kingdom show a high level of adherence with this recommendation, although patients do not always recall being asked.23,24 There are validated case-finding tools available for patients to complete that can be of use in primary care settings,25,26 and there is evidence that management of UI in primary care by family physicians is effective.27 Additionally, initial management in primary care is in accordance with many national and international guidelines on the subject.28
Box 1. Common risk factors for the development of urinary incontinence.
The following are common risk factors for the development of urinary incontinence:
Age
Parity/no. of pregnancies > 20/40
Parturition injury
Being obese or overweight
Race
Heredity (stress incontinence)
Chronic constipation
Smoking (cough, chronic lung disease), although there is conflicting evidence
Neurologic conditions (eg, multiple sclerosis, stroke, Parkinson disease, multisystem atrophy)
Post-prostatectomy
Drugs (eg, α-blockers, diuretics, cholinesterase inhibitors, systemic hormone replacement therapy)
Diabetes mellitus
Urinary tract infection
Cognitive impairment
Low physical function
Diet and lifestyle factors (eg, high glycemic index, low fibre intake, low vegetable intake)
High caffeine intake
Most of our respondents sometimes offered follow-up appointments for their patients with UI, and most also felt confident in their management of incontinence. Many offered lifestyle and behavioural advice to manage incontinence, but there was little evidence that structured, supervised programs of treatment were used, such as pelvic floor muscle therapy for which evidence of efficacy exists.29 Medication also appeared to be used rarely by our family physician respondents, despite plentiful evidence of benefit from antimuscarinic drugs in the pharmacologic treatment of overactive bladder.30 The coverage for these drugs in Alberta requires an initial prescription for immediate-release oxybutynin, which, owing to side effect concerns, might lead to a relative undertreatment of this condition.31
Despite professed confidence in the management of continence, there were considerable referrals to specialist services. The pattern of referrals included other specialist physicians, physiotherapists, and nurses. Wait-list times to see specialist community practitioners after referral are not known, but there was a relative paucity of referrals to specialist community practitioners, perhaps reflecting the extent of coverage and availability of these services in the region. Certainly our respondents thought that the services available to people with UI were stable or had improved, with only a small number believing that there had been deterioration. Overall, 42.4% of family physicians agreed or strongly agreed that services for UI were difficult to access, and only 23.4% thought that this was not the case. To what extent this is similar for other common conditions within Alberta is not known, but this might reflect the relative paucity of services in the community specifically for continence care.
Despite the views of the family physicians about the limited support from and difficulty in gaining access to continence services, approximately half of them thought that their patients were largely satisfied with their treatment. There are no patient outcome or satisfaction data with which to qualify this opinion, and physicians might overestimate outcomes with regard to UI treatment,32 so this might truly overestimate the level of satisfaction. Our respondents showed a clear desire to improve the care they offered to patients with incontinence; this was seen as less of a priority to the practice partnerships or networks that they worked within.
Respondents identified raising both patient and health care provider awareness as a key step forward in improving the care of people with UI, and there was a reasonable level of optimism among the physicians, with 45.6% considering it likely that there would be some advances in care during the next 2 years.
Limitations
The response rate from family physicians was low and our findings might not be generalizable. Response rates to surveys such as ours appear to be in decline, either owing to “survey fatigue”33 or to suspicion of the underlying motive of the survey. Likewise, there might be bias in the obtained results because of unidentified motivation to participate, such as either a markedly positive or negative outlook on the subject of inquiry. Some of the more positive results might reflect this. We did not consider the $50 incentive to be excessive or likely to potentially skew results. Similar studies in other areas would be expected to achieve a 50% response rate,34 although it is well recognized that participation rates have been falling consistently over the past 2 decades.35 Published evidence suggests that a combination of Web surveys and mailed self-completion questionnaires might achieve a slight increase in response rate compared with a single-pronged approach.36 We assumed that physicians would be more likely to respond to a telephone questionnaire, but we were clearly wrong. Family physicians, when they could be engaged and were interested, preferred to complete a faxed questionnaire. Data quality using this method was high, with only 1.5% of data items missing, in contrast to a previous study that reported a much higher rate of incomplete responses.37 However, regardless of the low response rate, there are some general and common themes that arose from this study that should inform health service provision and appear to reveal that, as was similarly suggested by the findings of Swanson et al in 2002,12 there is a continuing need to pay more attention to continence and its management in the community.
Conclusion
Participating physicians identified increased awareness and understanding of incontinence as well as availability of referral resources as key issues in improving the management of UI.
Physicians in our survey reported that the initial treatment of UI in primary care was satisfactory. Further research with patients is needed to corroborate this finding. A survey of available referral resources (community-based continence clinics, specialist nurses, urologists, and urogynecologists) to determine wait-list time and variation between urban and rural access would also be helpful to policy makers in planning to meet the needs of the population.
Acknowledgments
We thank Mandy Kravic and Jesse Luyenduyk for assistance with data collection.
EDITOR’S KEY POINTS
Urinary incontinence (UI) is a common and distressing condition associated with adverse effects on quality of life and work productivity, but many of those affected by UI do not discuss it with their doctors.
In total, 53.8% of the physician respondents to this survey reported that they proactively discussed UI with most or all of the patients they suspected had incontinence problems; 29.7% indicated that they proactively discussed UI with some of their patients, and 15.2% indicated that they did not discuss UI with anyone unless the patients raised the issue themselves. But despite the high prevalence of UI, many respondents in this study estimated the frequency to be low.
This study was limited by its low response rate.
POINTS DE REPÈRE DU RÉDACTEUR
L’incontinence urinaire est un problème fréquent et embarrassant qui a des effets pervers sur la qualité de vie et sur la productivité au travail, mais plusieurs de ceux qui en souffrent évitent d’en discuter avec leur médecin.
Dans l’ensemble, 53,8 % des médecins ayant répondu à cette enquête disaient discuter de façon proactive de l’IU avec la majorité ou tous les patients chez qui ils soupçonnaient un problème d’incontinence; 29,7 % déclaraient en discuter de façon proactive avec certains de leurs patients; et 15,2 %, ne jamais en discuter, à moins que le patient lui-même aborde ce problème. Toutefois, malgré la prévalence élevée de l’IU, plusieurs répondants à cette enquête estimaient que ce problème était peu fréquent.
À cause d’un faible taux de réponse, cette étude demeure donc limitée.
Footnotes
This article has been peer reviewed.
Cet article a fait l’objet d’une révision par des pairs.
Contributors
Drs Hunter and Wagg contributed to the concept and design of the study.
Dr Nguyen collected data. All authors participated in data analysis and manuscript preparation and revision.
Competing interests
This study was supported by an investigator grant from Pfizer Canada. The sponsor had no role in the design, data collection, analysis, or reporting of the findings of the study. The sponsor did receive a copy of the study report. Dr Wagg has received financial support from Astellas Pharma, Pfizer, SCA Pharmaceuticals, and Watson Pharma for research, speaker fees, and consulting. Dr Hunter has received financial support from Astellas Pharma and Pfizer for research.
References
- 1.Herschorn S, Gajewski J, Schulz J, Corcos J. A population-based study of urinary symptoms and incontinence: the Canadian Urinary Bladder Survey. BJU Int. 2008;101(1):52–8. doi: 10.1111/j.1464-410X.2007.07198.x. [DOI] [PubMed] [Google Scholar]
- 2.Irwin DE, Milsom I, Hunskaar S, Reilly K, Herschorn S, Coyne K, et al. Population-based survey of urinary incontinence, overactive bladder, and other lower urinary tract symptoms in five countries: results of the EPIC study. Eur Urol. 2006;50(6):1306–14. doi: 10.1016/j.eururo.2006.09.019. discussion 1314–5. [DOI] [PubMed] [Google Scholar]
- 3.Coyne KS, Sexton CC, Irwin DE, Kopp ZS, Kelleher CJ, Milsom I. The impact of overactive bladder, incontinence and other lower urinary tract symptoms on quality of life, work productivity, sexuality and emotional well-being in men and women: results from the EPIC study. BJU Int. 2008;101(11):1388–95. doi: 10.1111/j.1464-410X.2008.07601.x. [DOI] [PubMed] [Google Scholar]
- 4.Thom DH, Haan MN, Van Den Eeden SK. Medically recognized urinary incontinence and risks of hospitalization, nursing home admission and mortality. Age Ageing. 1997;26(5):367–74. doi: 10.1093/ageing/26.5.367. [DOI] [PubMed] [Google Scholar]
- 5.Nakagawa H, Niu K, Hozawa A, Ikeda Y, Kaiho Y, Ohmori-Matsuda K, et al. Impact of nocturia on bone fracture and mortality in older individuals: a Japanese longitudinal cohort study. J Urol. 2010;184(4):1413–8. doi: 10.1016/j.juro.2010.05.093. [DOI] [PubMed] [Google Scholar]
- 6.Wagg A. Treating overactive bladder in the elderly. Can Urol Assoc J. 2011;5(5 Suppl 2):S149–51. doi: 10.5489/cuaj.11188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shaw C, Tansey R, Jackson C, Hyde C, Allan R. Barriers to help seeking in people with urinary symptoms. Fam Pract. 2001;18(1):48–52. doi: 10.1093/fampra/18.1.48. [DOI] [PubMed] [Google Scholar]
- 8.Shaw C, Gupta RD, Bushnell DM, Assassa RP, Abrams P, Wagg A, et al. The extent and severity of urinary incontinence amongst women in UK GP waiting rooms. Fam Pract. 2006;23(5):497–506. doi: 10.1093/fampra/cml033. [DOI] [PubMed] [Google Scholar]
- 9.Shaw C, Atwell C, Wood F, Brittain K, Williams K. A qualitative study of the assessment and treatment of incontinence in primary care. Fam Pract. 2007;24(5):461–7. doi: 10.1093/fampra/cmm041. [DOI] [PubMed] [Google Scholar]
- 10.Horrocks S, Somerset M, Stoddart H, Peters TJ. What prevents older people from seeking treatment for urinary incontinence? A qualitative exploration of barriers to the use of community continence services. Fam Pract. 2004;21(6):689–96. doi: 10.1093/fampra/cmh622. [DOI] [PubMed] [Google Scholar]
- 11.Lagace EA, Hansen W, Hickner JM. Prevalence and severity of urinary incontinence in ambulatory adults: an UPRNet study. J Fam Pract. 1993;36(6):610–4. [PubMed] [Google Scholar]
- 12.Swanson JG, Skelly J, Hutchison B, Kaczorowski J. Urinary incontinence in Canada. National survey of family physicians’ knowledge, attitudes, and practices. Can Fam Physician. 2002;48:86–92. [PMC free article] [PubMed] [Google Scholar]
- 13.Bowling A, Mariotto A, Evans O. Are older people willing to give up their place in the queue for cardiac surgery to a younger person? Age Ageing. 2002;31(3):187–92. doi: 10.1093/ageing/31.3.187. [DOI] [PubMed] [Google Scholar]
- 14.Proceedings of 3rd Global Forum for Incontinence, Prague 2010. Plymouth, UK: Health Publications; 2010. [Google Scholar]
- 15.Zorn BH, Montgomery H, Pieper K, Gray M, Steers WD. Urinary incontinence and depression. J Urol. 1999;162(1):82–4. doi: 10.1097/00005392-199907000-00020. [DOI] [PubMed] [Google Scholar]
- 16.Asplund R, Henriksson S, Johansson S, Isacsson G. Nocturia and depression. BJU Int. 2004;93(9):1253–6. doi: 10.1111/j.1464-410X.2004.04835.x. [DOI] [PubMed] [Google Scholar]
- 17.Dugan E, Cohen SJ, Bland DR, Preisser JS, Davis CC, Suggs PK, et al. The association of depressive symptoms and urinary incontinence among older adults. J Am Geriatr Soc. 2000;48(4):413–6. doi: 10.1111/j.1532-5415.2000.tb04699.x. [DOI] [PubMed] [Google Scholar]
- 18.Coyne KS, Kvasz M, Ireland AM, Milsom I, Kopp ZS, Chapple CR. Urinary incontinence and its relationship to mental health and health-related quality of life in men and women in Sweden, the United Kingdom, and the United States. Eur Urol. 2012;61(1):88–95. doi: 10.1016/j.eururo.2011.07.049. [DOI] [PubMed] [Google Scholar]
- 19.Brown JS. Urinary incontinence: an important and underrecognized complication of type 2 diabetes mellitus. J Am Geriatr Soc. 2005;53(11):2028–9. doi: 10.1111/j.1532-5415.2005.53570.x. [DOI] [PubMed] [Google Scholar]
- 20.Felde G, Bjelland I, Hunskaar S. Anxiety and depression associated with incontinence in middle-aged women: a large Norwegian cross-sectional study. Int Urogynecol J. 2012;23(3):299–306. doi: 10.1007/s00192-011-1564-3. [DOI] [PubMed] [Google Scholar]
- 21.DuBeau CE, Kuchel GA, Johnson T, 2nd, Palmer MH, Wagg A. Incontinence in the frail elderly: report from the 4th International Consultation on Incontinence. Neurourol Urodyn. 2010;29(1):165–78. doi: 10.1002/nau.20842. [DOI] [PubMed] [Google Scholar]
- 22.Van Pinxteren B, Lagro-Janssen AL, Wiersma T, Goudswaard AN. Summary of the practice guideline ‘urinary incontinence’ (first revision) from the Dutch College of General Practitioners [article in Dutch] Ned Tijdschr Geneeskd. 2008;152(47):2559–63. [PubMed] [Google Scholar]
- 23.Wagg A, Duckett J, McClurg D, Harari D, Lowe D. To what extent are national guidelines for the management of urinary incontinence in women adhered? Data from a national audit. BJOG. 2011;118(13):1592–600. doi: 10.1111/j.1471-0528.2011.03100.x. [DOI] [PubMed] [Google Scholar]
- 24.Albers-Heitner P, Berghmans B, Nieman F, Lagro-Janssen T, Winkens R. Adherence to professional guidelines for patients with urinary incontinence by general practitioners: a cross-sectional study. J Eval Clin Pract. 2008;14(5):807–11. doi: 10.1111/j.1365-2753.2007.00925.x. [DOI] [PubMed] [Google Scholar]
- 25.Basra R, Artibani W, Cardozo L, Castro-Diaz D, Chapple C, Cortes E, et al. Design and validation of a new screening instrument for lower urinary tract dysfunction: the bladder control self-assessment questionnaire (B-SAQ) Eur Urol. 2007;52(1):230–7. doi: 10.1016/j.eururo.2006.11.015. [DOI] [PubMed] [Google Scholar]
- 26.Coyne KS, Zyczynski T, Margolis MK, Elinoff V, Roberts RG. Validation of an overactive bladder awareness tool for use in primary care settings. Adv Ther. 2005;22(4):381–94. doi: 10.1007/BF02850085. [DOI] [PubMed] [Google Scholar]
- 27.Moore KN, Saltmarche B, Query A. Urinary incontinence. Non-surgical management by family physicians. Can Fam Physician. 2003;49:602–10. [PMC free article] [PubMed] [Google Scholar]
- 28.Kirby M, Artibani W, Cardozo L, Chapple C, Diaz DC, De Ridder D, et al. Overactive bladder: the importance of new guidance. Int J Clin Pract. 2006;60(10):1263–71. doi: 10.1111/j.1742-1241.2006.01127.x. [DOI] [PubMed] [Google Scholar]
- 29.Dumoulin C, Hay-Smith J. Pelvic floor muscle training versus no treatment for urinary incontinence in women. A Cochrane systematic review. Eur J Phys Rehabil Med. 2008;44(1):22. [PubMed] [Google Scholar]
- 30.Novara G, Galfano A, Secco S, D’Elia C, Cavalleri S, Ficarra V, et al. A systematic review and meta-analysis of randomized controlled trials with anti-muscarinic drugs for overactive bladder. Eur Urol. 2008;54(4):740–63. doi: 10.1016/j.eururo.2008.06.080. [DOI] [PubMed] [Google Scholar]
- 31.Kessler TM, Bachmann LM, Minder C, Löhrer D, Umbehr M, Schünemann HJ, et al. Adverse event assessment of antimuscarinics for treating overactive bladder: a network meta-analytic approach. PLoS ONE. 2011;6(2):e16718. doi: 10.1371/journal.pone.0016718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tannenbaum C, Brouillette J, Corcos J. Rating improvements in urinary incontinence: do patients and their physicians agree? Age Ageing. 2008;37(4):379–83. doi: 10.1093/ageing/afn108. [DOI] [PubMed] [Google Scholar]
- 33.Weibe ER, Kaczorowski J, MacKay J. Why are response rates in clinician surveys declining? Can Fam Physician. 2012;58:e225–8. Available from: www.cfp.ca/content/58/4/e225.full. Accessed 2013 Jun 18. [PMC free article] [PubMed] [Google Scholar]
- 34.Eaker S, Bergstrom R, Bergstrom A, Adami HO, Nyren O. Response rate to mailed epidemiologic questionnaires: a population-based randomized trial of variations in design and mailing routines. Am J Epidemiol. 1998;147(1):74–82. doi: 10.1093/oxfordjournals.aje.a009370. [DOI] [PubMed] [Google Scholar]
- 35.Galea S, Tracy M. Participation rates in epidemiologic studies. Ann Epidemiol. 2007;17(9):643–53. doi: 10.1016/j.annepidem.2007.03.013. [DOI] [PubMed] [Google Scholar]
- 36.Beebe TJ, Locke GR, 3rd, Barnes SA, Davern ME, Anderson KJ. Mixing web and mail methods in a survey of physicians. Health Serv Res. 2007;42(3 Pt 1):1219–34. doi: 10.1111/j.1475-6773.2006.00652.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.McMahon SR, Iwamoto M, Massoudi MS, Yusuf HR, Stevenson JM, David F, et al. Comparison of e-mail, fax, and postal surveys of pediatricians. Pediatrics. 2003;111(4 Pt 1):e299–303. doi: 10.1542/peds.111.4.e299. [DOI] [PubMed] [Google Scholar]


