Abstract
OBJECTIVE
To estimate whether the timing of bladder emptying affects focal myometrial contraction development and image adequacy.
METHODS
Women at 14 0/7–32 0/7 weeks of gestation undergoing a transvaginal ultrasound examination from January 1, 2012, to September 1, 2012, were eligible for this blinded randomized controlled trial. Participants were randomly assigned to undergo transvaginal imaging immediately after urination (within 5 minutes) or to defer the imaging by at least 15 minutes. The primary outcome was focal myometrial contraction development as determined by two independent blinded reviews of the images. Secondary outcomes included image adequacy and the diagnosis of placenta previa. Relative risks (RRs) and 95% confidence intervals (CIs) were calculated using repeated-measures log binomial regression.
RESULTS
Two hundred twenty-one women provided 335 randomized encounters for analysis. Women in the deferred scan group were 30% less likely to experience a focal myometrial contraction (28.1% compared with 40.5%, RR 0.70, 95% CI 0.52–0.93) and 41% less likely to have inadequate images (18.6% compared with 31.5%, RR 0.59, 95% CI 0.40–0.86). The two groups were equally likely to be diagnosed with placenta previa (P=.13). However, participants in the deferred scan group were 76% less likely to have images demonstrating a placenta previa and focal myometrial contraction (3.0% compared with 12.5%, RR 0.24, 95% CI 0.09– 0.62) than participants in the immediate scan group. Eight women would need to defer imaging for 15 minutes from bladder voiding to prevent one focal myometrial contraction of the lower uterine segment or inadequate imaging.
CONCLUSIONS
A brief interval (at least 15 minutes) between voiding and transvaginal cervical evaluation is associated with decreased risk for focal myometrial contractions and improved imaging.
Transvaginal ultrasonography has revolutionized obstetric diagnosis as a result of its superior performance in cervical and placental assessment. Large prospective trials have demonstrated the use of transvaginal ultrasonography in determining preterm birth risk and cervical insufficiency.1–3 Previous studies also suggest that the ability to evaluate the internal cervical os and its relationship to the placental edge is improved with transvaginal imaging enabling more accurate diagnosis of placenta previa.4,5 These qualities have prompted clinicians and health care policymakers to recommend transvaginal cervical ultrasonography as a standard part of the second-trimester obstetric ultrasonographic examination.6–9 However, the visualization of the cervix and placenta can be impaired by the presence of localized muscular contractions of the lower uterine segment called focal myometrial contractions.10
Focal myometrial contractions have been labeled a common pitfall of obstetric ultrasonography. Despite numerous publications regarding cervical length measurement and preterm birth, relatively little has been published regarding the incidence of focal myometrial contractions and their clinical effect. It is hypothesized that they occur throughout gestation in association with maternal activity, bladder filling, and voiding.11 Our clinical experience suggests that focal myometrial contractions occur during ultrasonographic cervical assessments with a relatively high incidence and may be associated with the timing of bladder voiding. Biological support for this clinical observation is derived from studies demonstrating shared parasympathetic innervation between the uterus and bladder. Our objective was to estimate the affect of voiding on the incidence of lower uterine segment focal myometrial contractions and the ability to achieve accurate cervical length and placental location determinations.
PATIENTS AND METHODS
We performed this blinded randomized controlled trial at the Beth Israel Deaconess Medical Center from January 1, 2012, to September 1, 2012. Study participation was offered to women at 14 0/7 to 32 0/7 weeks of gestation presenting to our outpatient prenatal diagnosis center for indicated or routine transvaginal ultrasonographic cervical assessment, placental location determination, or both. Potential participants were approached by study staff on arrival and were provided a standard verbal explanation of the study. Before randomization, women were asked whether they would be willing to void in accordance with the required procedures of either arm. Women were excluded if they urgently needed to void and anticipated the inability to delay voiding comfortably until immediately before transvaginal imaging. Verbal consent was obtained from all participants.
Randomization was performed using a computergenerated block randomization scheme with block sizes of four, six, and eight. Arm allocation was concealed before enrollment in sequentially numbered opaque envelopes. Participants were randomized to undergo transvaginal imaging within 5 minutes of urination (immediate scan arm) or to defer the transvaginal imaging by at least 15 minutes after urination (deferred scan arm). Those in the immediate scan arm first underwent clinically indicated transabdominal imaging and then were asked to void completely and underwent transvaginal imaging within 5 minutes. Participants in the deferred scan arm were asked to void immediately after enrollment. Transabdominal imaging was then performed, and transvaginal imaging did not begin until at least 15 minutes had elapsed since voiding. Study personnel tracked voiding and imaging times. Positioning and image acquisition followed a standard protocol,1 and at least three transvaginal images were obtained from each participant. Imaging was performed by clinically trained ultrasonographers certified by the American Registry for Diagnostic Medical Sonography. Each received supplementary instruction on the study’s protocol and required technique. Images were captured, deidentified, and stored electronically by study identification number with no indication of assigned treatment arm. Randomization and image capture and storage were performed by a single coinvestigator. Demographic and obstetric data were collected from participants and review of the medical records during the encounters.
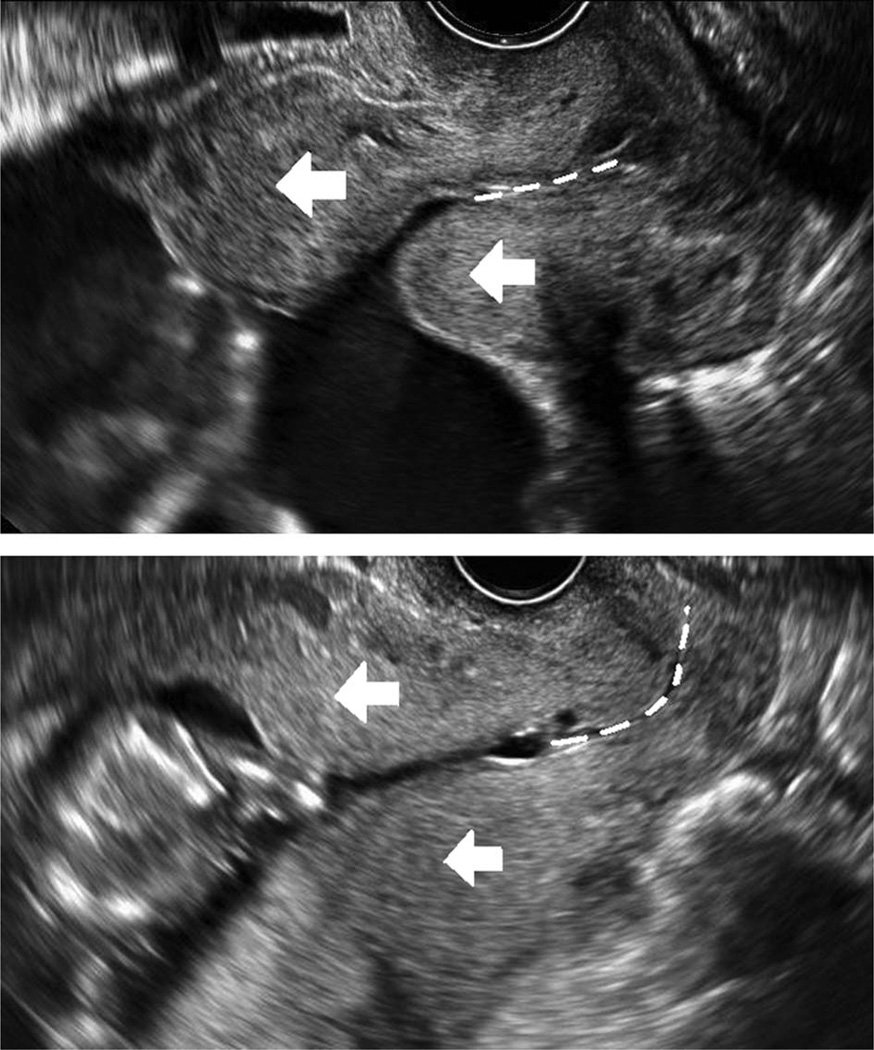
After all participants completed the study, two coinvestigators (W.T.S. and D.R.) blinded to the assigned arm assessed all of the images. A third coinvestigator (M.M.) independently adjudicated all cases in which there was disagreement in outcome determination. The prespecified primary outcome, presence of a focal myometrial contraction, was defined by two or more of the following transvaginal ultrasonography findings: a thickening of the myometrium visualized as two distinctly different areas of echogenicity; an unusually long-appearing cervix with an S-shaped endocervical canal and apparent internal os located appreciably cephalad to the inferior edge of the bladder reflection; asymmetric anterior and posterior lower uterine segment widths cephalad to the apparent internal os; or confirmation that the thickening was transient, present only for a portion of the total length of the examination (Fig. 1).2 Secondary outcomes included inadequate images (defined as the inability to definitively view the entire endocervical canal, external cervical os, internal cervical os, and caudal-most portion of the placenta), inadequate images with and without a focal myometrial contraction, the diagnosis of placenta previa, and placenta previa with and without a focal myometrial contraction.
Fig. 1.
Ultrasonographic appearance of focal myometrial contractions obscuring the internal cervical os and falsely elongating the endocervical canal. Arrows point to the focal myometrial contractions, and the dashed lines represent the endocervical canal.
Schnettler. Ultrasonographic Cervical Evaluation and Voiding. Obstet Gynecol 2013.
Based on previous studies, we estimated the incidence of lower uterine segment focal myometrial contractions in our population to be 30%.2,10 Given the voluntary nature of the study, participants were offered reenrollment at subsequent visits and were rerandomized at each reenrollment. We estimated an average of three enrollments per participant. We did not anticipate a substantial within-patient correlation for this exposure– outcome association given that no evidence suggests a physiologic predisposition among specific women for focal myometrial contractions after bladder voiding. Assuming a within-patient correlation of 0.1, a two-sided α=0.05, an allocation ratio of 1:1, and 80% power, we needed to enroll 101 women to contribute a total of 303 cervical assessments to detect a 50% reduction in focal myometrial contractions of the lower uterine segment from 30% to 15%. Assuming a 10% loss resulting from the need for women to void earlier than instructed or the inability to complete the assessment, we aimed to enroll 112 women.
All data were analyzed using SAS 9.3 software. All tests were two sided, and P values < 05 were considered statistically significant. Data are presented as proportions and medians (interquartile ranges). Proportions were compared using the χ2 or Fisher’s exact test, and medians were compared with the Wil-coxon rank-sum test. Relative risks (RRs) and 95% confidence intervals (CIs) were calculated using repeated-measures log binomial regression accounting for the repeated encounters for individual women.12 We received approval for this study from the institutional review board of the Beth Israel Deaconess Medical Center. All participants provided informed verbal consent.
RESULTS
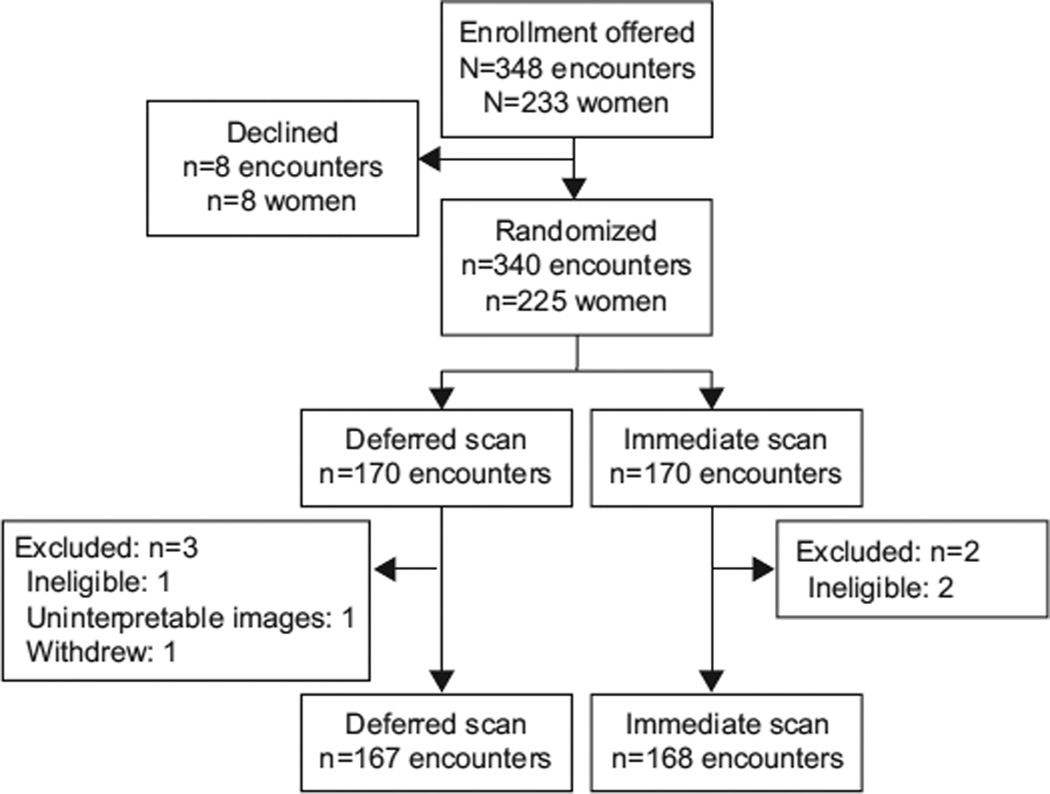
We approached 233 women; given that reenrollment was not an exclusion criterion, many women were approached more than once. Eight women declined leaving 340 randomized encounters (Fig. 2). Three encounters were excluded from the deferred scan arm: one failed to meet inclusion criteria, one set of images was noninterpretable as a result of technical issues, and one withdrew after randomization. Two encounters were excluded from the immediate scan arm as a result of failure to meet inclusion criteria. Thus, 221 women provided 335 randomized encounters for analysis: 167 in the deferred scan arm and 168 in the immediate scan arm. The number of initial encounters and reenrollments was similar between the groups (Table 1.)
Fig. 2.
Enrollment and allocation of participants into study groups.
Schnettler. Ultrasonographic Cervical Evaluation and Voiding. Obstet Gynecol 2013.
Table 1.
Baseline Characteristics of Participants
| Characteristic | Deferred Scan (n=167) | Immediate Scan (n=168) |
|---|---|---|
| Age (y) | 31.0 (27.0–34.0) | 31.0 (26.0–35.0) |
| Body mass index (kg/m2) | 23.4 (21.2–27.8) | 24.4 (21.5–27.3) |
| Race | ||
| White | 65 (38.9) | 63 (37.5) |
| African American | 50 (29.9) | 58 (34.5) |
| Hispanic | 30 (18.0) | 20 (11.9) |
| Asian or Pacific Islander | 17 (10.2) | 22 (13.1) |
| Other | 5 (3.0) | 5 (3.0) |
| Gravidity | 2.0 (1.0–4.0) | 2.0 (1.0–4.0) |
| Parity | 1.0 (0.0–1.0) | 1.0 (0.0–1.0) |
| Gestational age (wk) | 21.0 (18.3–25.9) | 19.4 (18.1–25.6) |
| Comorbidity | 42 (25.2) | 37 (22.0) |
| History of preterm birth | 37 (22.2) | 41 (24.4) |
| History of cervical insufficiency | 12 (7.2) | 15 (8.9) |
| Known leiomyomas | 9 (5.4) | 8 (4.8) |
| Indication for examination | ||
| Routine screen | 80 (29.9) | 64 (38.1) |
| Transabdominal cervical shortening | 2 (1.2) | 1 (0.6) |
| History of cervical insufficiency | 7 (4.2) | 9 (5.4) |
| History of preterm birth | 28 (16.8) | 29 (17.3) |
| Multiple gestation | 14 (8.4) | 13 (7.7) |
| Prior cervical shortening | 33 (19.8) | 23 (13.7) |
| Concern for placenta previa | 16 (9.6) | 18 (10.7) |
| Follow-up cervical cerclage | 17 (10.2) | 17 (10.1) |
| Other | 32 (19.2) | 25 (14.9) |
| Initial encounter | 105 (62.9) | 116 (69.0) |
| Reenrollments | 62 (37.1) | 52 (31.0) |
Data are median (interquartile range) or n (%).
Baseline demographic characteristics of participants were similar between groups (Table 1). Study participants in both groups were predominantly parous, nonobese, aged 25–35 years, and from various ethnicities. Nearly one-fourth had medical comorbidities such as diabetes mellitus, chronic hypertension, and thyroid disorders. A history of spontaneous preterm delivery was present in almost 25% of participants. The predominant indication for cervical evaluation was routine screening among participants.
Ultrasonography examination characteristics differed between groups. In the immediate scan group, women voided a median of 3.0 (interquartile range 3.0– 5.0, range 0.0–10.0) minutes before the scan; in the deferred scan group, women voided a median of 28.0 (interquartile range 21.0–38.0, range 15.0–188.0) minutes before the scan (P<.001). There were no differences between groups for the median time between participants’ study void and last recalled void (87.0 [56.5– 126.5] compared with 85.0 [57.0–121.0] minutes; P=.74) or the total duration of the transvaginal scan (2.0 [1.5–3.0] compared with 2.0 [1.0–3.0] minutes; P=.40).
A delay between bladder voiding and transvaginal ultrasonography was associated with a decreased incidence of focal myometrial contractions of the lower segment, an increased likelihood of obtaining adequate images, and a decreased incidence in the diagnosis of placenta previa together with a focal myometrial contraction. Participants in the deferred scan group were 30% less likely to experience focal myometrial contractions (RR 0.70, 95% CI 0.52–0.93) than participants in the immediate scan group (Table 2). Images were 41% less likely to be deemed inadequate among participants in the deferred scan group (RR 0.59, 95% CI 0.40–0.86). Focal myometrial contractions were present in more than 92% of inadequate images in each group, and the deferred scan group was 40% less likely to experience inadequate images together with a focal myometrial contraction (RR 0.60, 95% CI 0.40–0.89). Eight women would need to defer imaging for 15 minutes from bladder voiding to prevent one focal myometrial contraction of the lower uterine segment or inadequate imaging. The two groups were equally likely to be diagnosed with placenta previa (P=.13). However, participants were 76% less likely to be diagnosed with placenta previa together with a focal myometrial contraction (RR 0.24, 95% CI 0.09–0.62) than participants in the immediate scan group.
Table 2.
Primary and Secondary Outcomes Stratified by Randomization Groups
| Outcome | Deferred Scan (n=167) |
Immediate Scan (n=168) |
Risk Ratio (95% CI) |
P |
|---|---|---|---|---|
| Focal myometrial contraction | 47 (28.1) | 68 (40.5) | 0.70 (0.52–0.93) | .02 |
| Inadequate images | 31 (18.6) | 53 (31.5) | 0.59 (0.40–0.86) | .006 |
| Inadequate images without focal myometrial contraction | 2 (1.2) | 4 (2.4) | 0.50 (0.09–2.70) | .42 |
| Inadequate images and focal myometrial contraction | 29 (17.4) | 49 (29.2) | 0.60 (0.40–0.89) | .01 |
| Placenta previa | 22 (13.2) | 33 (19.6) | 0.67 (0.40–1.13) | .13 |
| Placenta previa without focal myometrial contraction | 17 (10.2) | 12 (7.1) | 1.4 (0.76–2.7) | .27 |
| Placenta previa and focal myometrial contraction | 5 (3.0) | 21 (12.5) | 0.24 (0.09–0.62) | .003 |
CI, confidence interval.
Data are n (%) unless otherwise specified.
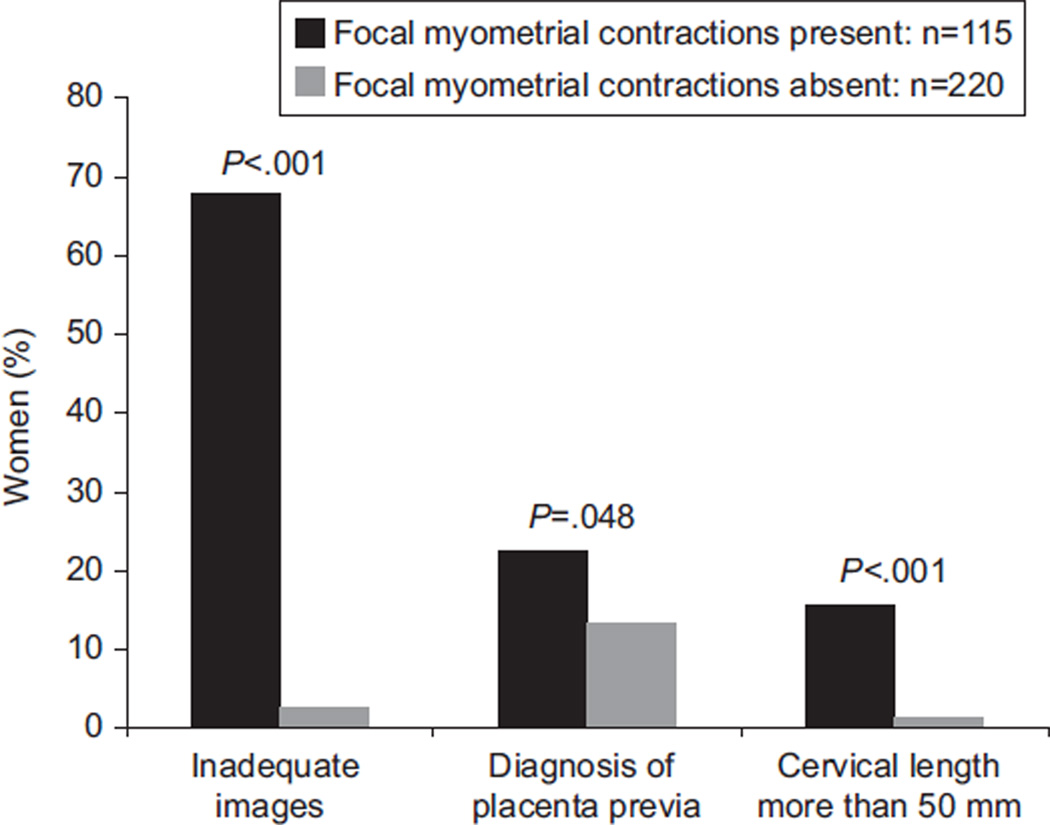
Although not the initial randomized exposure of interest, we investigated the clinical effects from focal myometrial contractions of the lower uterine segment. They were noted in 115 encounters and were absent in 220, yielding an overall incidence of 34.3% (95% CI 29.3–40.0). Focal myometrial contractions strongly affected imaging adequacy (Fig. 3). The incidence of inadequate images was 25.1% (95% CI 20.5–30.1) among all encounters, but images were considered inadequate in 67.8% of encounters in which a focal myometrial contraction was present compared with 2.7% of evaluations without a focal myometrial contraction (RR 24.2, 95% CI 11.0–53.5). The diagnosis of placenta previa was made in 16.4% (95% CI 12.6–20.8) of all encounters but was made in 22.6% of encounters with a focal myometrial contraction present compared with 13.2% of encounters without a focal myometrial contraction (RR 1.7, 95% CI 1.00–2.8). Cervical length measurement was significantly increased an average of 7 mm in the presence of a focal myometrial contraction (P<.001), and a measurement length greater than 50 mm was over 11 times more likely in the presence of a focal myometrial contraction (RR 11.5, 95% CI 3.4–38.4) (Fig. 3).
Fig. 3.
Imaging outcomes associated with focal myometrial contractions.
Schnettler. Ultrasonographic Cervical Evaluation and Voiding. Obstet Gynecol 2013.
The risk of focal myometrial contractions was associated with gestational age, body mass index (BMI, calculated as weight (kg)/[height (m)]2), and parity (Table 3). Women who were at an earlier gestational age (P<.001), had higher BMIs (P=.03), and were parous (P<.001) were more likely to develop focal myometrial contractions. The median gestational age among women who had a focal myometrial contraction was 18.9 (18.0– 21.3) weeks compared with 23.0 (18.4–27.2) weeks among those who did not. Focal myometrial contractions most commonly occurred in pairs lying along the anterior and posterior lower uterine segments (45.4%), whereas only 14.8% occurred solely along the anterior segment and 39.8% solely along the posterior segment. Those that were associated with imaging inadequacy lay immediately adjacent to the internal cervical os.
Table 3.
Demographic Factors Associated With Focal Myometrial Contraction Development
| Focal Myometrial Contraction Present (n=115) |
Focal Myometrial Contraction Absent (n=220) |
Risk Ratio (95% CI) |
P | |
|---|---|---|---|---|
| Gestational age (wk) | 18.9 (18.0–21.3) | 23.0 (18.4–27.2) | 0.90 (0.87–0.94) | <.001 |
| Body mass index (kg/m2) | 25.0 (21.4–29.0) | 23.5 (21.4–26.5) | 1.0 (1.0–1.1) | .03 |
| Parity | 1.0 (0.0–1.0) | 0.0 (0.0–1.0) | 1.3 (1.1–1.4) | <.001 |
CI, confidence interval.
Data are median (interquartile range) unless otherwise specified.
DISCUSSION
Our findings indicate that focal myometrial contractions of the lower uterine segment occur relatively frequently and impair transvaginal ultrasonographic evaluation of the cervix and placenta. A brief interval between voiding and transvaginal imaging was associated with a significant decrease in focal myometrial contractions of the lower uterine segment and improved image adequacy. Focal myometrial contractions of the lower uterine segment occurred in 34.3% of all transvaginal ultrasonograms, and they were significantly associated with an increased likelihood of obtaining inadequate images and ascribing a diagnosis of placenta previa. This provision for a brief interval between voiding and transvaginal imaging requires no additional examination time making it a logistically feasible means of potentially improving imaging quality and obstetric outcomes.
Shared parasympathetic innervation by the bladder and uterus provides biological support for the relationship between bladder emptying and myometrial contractions. The visceral surfaces of pelvic organs contain complex ganglionic plexi that share input from long efferent preganglionic axons of nerve cell bodies residing in the sacral spinal cord.13 The vesical neuronal plexus and paracervical ganglionic plexus are located within the same region.14 Autonomic activation of the bladder’s detrusor muscle for urination begins with signaling the vesical neuronal plexus but also may simultaneously activate the paracervical ganglionic plexus, which signals the myometrial muscarinic and cholinergic receptors triggering myometrial muscle contractions, specifically of the lower uterus.15,16
We found that earlier gestational age (approximately 4 weeks) was associated with focal myometrial contraction incidence. This finding is supported by an earlier study that demonstrated that 14 of 15 women imaged by magnetic resonance imaging between 5 and 16 weeks had “sustained uterine contractions.”11 Pregnancy-associated adaptive changes to the uterine autonomic innervation have been demonstrated by in vitro rat studies and may presumably confer some fetal protective benefit.15,17 Staining studies confirm a diminished presence of myometrial autonomic nerve fibers as gestation advances, and this may suggest an evolutionary process whereby the preterm uterine expulsion of the fetus is less likely as a result of the transient suppression of myometrial activation.15 Our findings support this theory.
Few studies have assessed the incidence of focal myometrial contractions. Previous clinical reports describe the presence of “anatomic factors” that resulted in cervical assessment inaccuracies in 10–30% of study populations.2,10 Owen and colleagues reported a 16% incidence of a transient poorly developed lower uterine segment when evaluating cervical length between 16 0/7 and 23 6/7 weeks of gestation. The phenomenon was described as transient and decreased with advancing gestation suggesting that they were, in fact, describing focal myometrial contractions. Yost and colleagues10 proposed the term focal myometrial contractions in their observational study of transvaginal ultrasonographic pitfalls. These authors found that anatomic factors hampered the ability to identify the essential landmarks (our definition of image inadequacy) among 27% of their cohort. These earlier studies report incidence data that are similar to our findings, but neither publication proposed an association with voiding.
Our study adds clinically important data to a topic that has undergone little rigorous investigation. We report the association of focal myometrial contractions with bladder voiding as well as their incidence and associated risk factors as specific outcomes. We have demonstrated that their incidence is associated with the timing of bladder voiding using a prospective and randomized approach. Furthermore, we have provided detailed criteria and shown the existence of risk factors such as gestational age, BMI, and parity. Potential limitations to our trial include the open treatment because blinding participants to arm allocation was not possible. However, the primary and secondary outcomes were objectively determined by reviewers blinded to assigned arm; thus, the potential effect from the lack of participant blinding was likely minimal. Definitions for the outcomes were determined before review, and an independent reviewer provided adjudication in cases of discrepancies between the two primary reviewers. A second limitation involves the potential for other image characteristics (such as bladder fullness) to cause inadvertent unblinding by the reviewers. Image reviewers were not asked to identify which group they thought the image came from to assess the degree of inadvertent unblinding. However, rereview of 50 images from each group confirmed that they could not be differentiated by the visual appearance of the bladder fullness.
Focal myometrial contractions of the lower uterine segment are common and affect image interpretation and quality. Cervical length measurements appear to be falsely lengthened, and the potential to falsely diagnose placenta previa is increased. An interval of at least 15 minutes between voiding and transvaginal imaging was associated with a significant decrease in focal myometrial contraction incidence, inadequate imaging, and diagnosis of placenta previa. Additionally, delaying the cervical evaluation to later gestational ages (21–23 weeks) may decrease focal myometrial contraction incidence. These simple changes to imaging protocols may lead to improved obstetric outcomes through enhanced preterm birth risk assessment and diagnosis of placenta previa.
Acknowledgments
Supported by Harvard Catalyst The Harvard Clinical and Translational Science Center (National Center for Research Resources and the National Center for Advancing Translational Sciences, National Institutes of Health Award 8UL1TR000170-05, and financial contributions from Harvard University and its affiliated academic health care centers).
Footnotes
The content is solely the responsibility of the authors and does not necessarily represent the official views of Harvard Catalyst, Harvard University and its affiliated academic health care centers, or the National Institutes of Health.
Financial Disclosure
The authors did not report any potential conflicts of interest.
REFERENCES
- 1.Iams JD, Goldenberg RL, Meis PJ, Mercer BM, Moawad A, Das A, et al. The length of the cervix and the risk of spontaneous premature delivery. N Engl J Med. 1996;334:567–572. doi: 10.1056/NEJM199602293340904. [DOI] [PubMed] [Google Scholar]
- 2.Owen J, Yost N, Berghella V, Thom E, Swain M, Dildy GA, 3rd, et al. Mid-trimester endovaginal sonography in women at high risk for spontaneous preterm birth. JAMA. 2001;286:1340–1348. doi: 10.1001/jama.286.11.1340. [DOI] [PubMed] [Google Scholar]
- 3.Berghella V, Tolosa JE, Kuhlman D, Weiner S, Bolognese RJ, Wapner RJ. Cervical ultrasonography compared with manual examination as a predictor of preterm delivery. Am J Obstet Gynecol. 1997;177:723–730. doi: 10.1016/s0002-9378(97)70259-x. [DOI] [PubMed] [Google Scholar]
- 4.Sherman SJ, Carlson DE, Platt LD, Medearis AL. Transvaginal ultrasound: does it help in the diagnosis of placenta previa? Ultrasound Obstet Gynecol. 1992;2:256–260. doi: 10.1046/j.1469-0705.1992.02040256.x. [DOI] [PubMed] [Google Scholar]
- 5.Taipale P, Hiilesmaa V, Ylöstalo P. Diagnosis of placenta previa by transvaginal sonographic screening at 12–16 weeks in a nonselected population. Obstet Gynecol. 1997;89:364–367. doi: 10.1016/S0029-7844(96)00503-0. [DOI] [PubMed] [Google Scholar]
- 6.Iams JD. Cervical ultrasonography. Ultrasound Obstet Gynecol. 1997;10:156–160. doi: 10.1046/j.1469-0705.1997.10030156.x. [DOI] [PubMed] [Google Scholar]
- 7.Ultrasonography in pregnancy. ACOG Practice Bulletin No. 101. American College of Obstetricians and Gynecologists. Obstet Gynecol. 2009;113:451–461. doi: 10.1097/AOG.0b013e31819930b0. [DOI] [PubMed] [Google Scholar]
- 8.Werner EF, Han CS, Pettker CM, Buhimschi CS, Copel JA, Funai EF, et al. Universal cervical-length screening to prevent preterm birth: a cost-effectiveness analysis. Ultrasound Obstet Gynecol. 2011;38:32–37. doi: 10.1002/uog.8911. [DOI] [PubMed] [Google Scholar]
- 9.Cahill AG, Odibo AO, Caughey AB, Stamilio DM, Hassan SS, Macones GA, et al. Universal cervical length screening and treatment with vaginal progesterone to prevent preterm birth: a decision and economic analysis. Am J Obstet Gynecol. 2010;202:548. doi: 10.1016/j.ajog.2009.12.005. e1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yost NB, Bloom SL, Twickler DM. Pitfalls in ultrasonic cervical length measurement for predicting preterm birth. Obstet Gynecol. 1999;93:510–516. doi: 10.1016/s0029-7844(98)00438-4. [DOI] [PubMed] [Google Scholar]
- 11.Togashi K, Kawakami S, Kimura I, Asato R, Takakura K, Mori T, et al. Sustained uterine contractions: a cause of hypointense myometrial bulging. Radiology. 1993;187:707–710. doi: 10.1148/radiology.187.3.8497617. [DOI] [PubMed] [Google Scholar]
- 12.Spiegelman D, Hertzmark E. Easy SAS calculations for risk or prevalence ratios and differences. Am J Epidemiol. 2005;162:199–200. doi: 10.1093/aje/kwi188. [DOI] [PubMed] [Google Scholar]
- 13.Moore. Essential clinical anatomy. 3rd ed. Philadelphia (PA): Lippincott Williams & Wilkins; 2007. [Google Scholar]
- 14.Yabuki Y, Asamoto A, Hoshiba T, Nishimoto H, Satou N. A new proposal for radical hysterectomy. Gynecol Oncol. 1996;62:370–378. doi: 10.1006/gyno.1996.0251. [DOI] [PubMed] [Google Scholar]
- 15.Papka RE, Traurig HH, Schemann M, Collins J, Copelin T, Wilson K. Cholinergic neurons of the pelvic autonomic ganglia and uterus of the female rat: distribution of axons and presence of muscarinic receptors. Cell Tissue Res. 1999;296:293–305. doi: 10.1007/s004410051290. [DOI] [PubMed] [Google Scholar]
- 16.Kitazawa T, Hirama R, Masunaga K, Nakamura T, Asakawa K, Cao J, et al. Muscarinic receptor subtypes involved in carbachol-induced contraction of mouse uterine smooth muscle. Naunyn-Schmiedeberg’s Arch Pharmacol. 2008;377:503–513. doi: 10.1007/s00210-007-0223-1. [DOI] [PubMed] [Google Scholar]
- 17.Chavez-Genero R, Lombide P, Anesetti G. A quantitative study of rat uterine sympathetic innervations during pregnancy and post partum. Reprod Fertil Dev. 2006;18:525–531. doi: 10.1071/rd05053. [DOI] [PubMed] [Google Scholar]