Abstract
Background
Changes in body composition during weight loss among obese adolescents are poorly understood. This study characterized the composition of weight loss, and its association with changes in waist circumference (WC) in obese adolescents.
Methods
Total (Tot), trunk (Tr) and appendicular (Ap) fat mass (FM) and lean mass (LM) were measured by dual-energy X-ray absorptiometry (DXA) in 61 obese adolescents (40 girls) who participated in a randomized-controlled weight-loss trial. Changes in body composition were assessed at 0, 6, and 12 months using mixed-effects regression models. Correlation analysis of change in WC and total and regional compartments of FM and LM were also assessed.
Results
Weight-loss for adolescents was 90.3% FM and 15.9% LM at 0–6mo, and 98.2% FM and 7% LM at 0–12 mo. At 12mo, girls lost 2.67 kg more TotFM than boys in models adjusted for height, age, race, and baseline weight. Boys gained LM in all compartments in all models. At 12mo, girls lost TotLM (2.23 ±0.74, p<0.004) and ApLM (0.69 ±0.31, p=0.03), and gained TrLM (0.37±0.35, p=0.29). The percentage LM, increased for boys and girls in all models. TotFM was correlated with BMI change with TotFM (R=0.70–0.91, p=0.001) and WC change (R=0.53–0.55, p<0.001).
Conclusions
Weight loss in obese adolescents during a weight-loss trial using lifestyle management and sibutramine was primarily from trunk fat mass. Although absolute LM increased in boys and decreased in girls, the percentage of weight that is LM increased for both boys and girls. Changes in BMI were more reflective of changes in FM than changes in WC.
Keywords: body mass index, body composition, weight loss, childhood obesity, waist circumference
INTRODUCTION
Obesity in adolescents has reached epidemic proportions at 16.9% in the US and is associated with many co-morbidities (1). The distribution of adipose tissue is an independent risk factor for cardio-metabolic complications of obesity (2–4). Having a preferential loss of trunk fat mass (central adiposity) over appendicular mass (arms and legs) is metabolically more favorable (5). The goal of weight reduction is not only to lose overall body mass and fat mass (FM), but to also lose central adiposity and to preserve or increase lean mass (LM). Changes in body mass index (BMI) or BMI-z score which are used to categorize obesity risk do not describe which tissue compartment is changing. The changes in tissue compartments (lean vs. fat) and their distribution (trunk vs. arms and legs) during the acute (0–6 months) and maintenance phases of weight loss (12 months) in adolescents has not been studied.
Adolescence is an important time of physical development due to hormonal changes, sexual maturation and linear growth, all of which may potentially affect body composition (6). Although prior work has shown that bone mineral content is preserved (7), the effects of weight loss on fat mass and lean mass in obese adolescents are not well understood. The effect of baseline weight on changes in body composition in adolescents is also an area in need of further study.
Waist circumference is used as an indicator of central adiposity and increased cardiovascular risk (8). The determination of the correlation of changes of these simple anthropometric measurements to changes in lean and fat tissue compartments adds to the clinical relevance of these measurements.
The primary objectives of this study were to assess the changes in total and regional body composition after a 12 month outpatient multidisciplinary weight loss program in obese adolescents, and to examine the correlation of change in waist circumference with BMI, BMI z-score, weight, total FM, total LM,trunk FM, trunk LM, appendicular FM, and appendicular LM.
METHODS AND PROCEDURES
This is an observational study of body-composition in obese adolescents taking part in a randomized controlled trial of weight loss (9). A detailed description of the trial methods and results has been provided elsewhere (9). Briefly, boys and post-menarcheal girls aged 13–17 years were eligible if their BMI (kg/m2) was between 32 and 44, and if they had no significant medical or psychiatric condition. The study tested the effectiveness of sibutramine in conjunction with a comprehensive, family-based, behavioral weight control program in a placebo controlled, randomized clinical trial. All subjects were included in a comprehensive weight loss program that included 13-weekly sessions, followed by 9 bi-weekly group sessions, and 3-monthly group sessions, for a total of 25 group sessions over 12 months. The subjects were instructed to consume a 1,200–1,500 kcal/day balanced diet and prescribed an eventual goal of walking (or engaging in similar aerobic activities) for 120 min or more per week. Participants kept daily eating and activity logs that they submitted at each session. During the first 6 month period, half of the participants were randomized to escalating doses of sibutramine up to 15 mg/day and the other half to a matching placebo. Dosage was decreased or medication interrupted if significant increases in blood pressure occurred. For the second 6-month period, all subjects received the active drug in an open-label trial in combination with a weight loss program.
Because we were only interested in study subjects who lost weight, longitudinal analyses were restricted to study subjects who completed the 12-month assessment. Subjects who do not complete weight loss trials are often those subjects who are not successful in their weight loss (10). While this could potentially bias the randomized trial which compared two treatment groups, it is not relevant to this examination of the composition of weight loss. Therefore, restriction to completers was a justifiable approach in this case, and data from the baseline, 6 months, and 12 months visits were analyzed.
Body weight was measured to the nearest 0.1kg using a digital electronic scale (Seca, Munich, Germany), and stature to the nearest 0.1cm using a stadiometer (Holtain, Crymych, UK), and BMI was calculated. Weight, height, and BMI were converted to age- and sex-specific z-scores based on the Centers of Disease Control and Prevention reference growth charts (11). Waist circumference (0.1cm) at the level of the umbilicus was measured using a flexible measuring tape (12).
Outcome measures
Fat mass (FM) (kg) and lean mass (LM) (kg), were estimated from whole body dual energy x-ray absorptiometry (DXA) (QDR2000, Hologic, Bedford, MA) with a fan beam densitometer. Body regions (arms, legs, trunk, and head) were delineated in the scan images analysis by the DXA operator according to manufacturer guidelines. All subjects were measured on the same machine using standard positioning techniques. Quality control scans were performed daily using a simulated L1–L4 spine of hydroxyapatite encased in resin. There was no significant change or drift in phantom scan results, and the coefficient of variation (%CV) was less than 1% (0.45%). A step phantom was scanned with each whole body scan, but a whole body phantom for longitudinal quality control was not available at that time.
The primary outcome measures were the change in total FM (TotFM), trunk FM (TrFM), and appendicular (arms and legs) FM (ApFM) (kg), total LM (TotLM), trunk LM (TrLM), and appendicular LM (ApLM) (kg) at 0–6 months, 6–12 months, and 0–12 months. The LM measures did not include bone mass. Change in waist circumference (cm) was a secondary outcome measure. Measurements were obtained between May 1999 and July 2002 at baseline, 6 months, and 12 months. The study was approved by the Institutional Review Boards of the Perelman School of Medicine at the University of Pennsylvania and The Children’s Hospital of Philadelphia.
African-Americans have more LM and bone mineral content (BMC) than Caucasians (13), thus the sample was divided into African-American versus non-African-American participants. There are differences in the rate of growth and the distribution of LM and FM by age, pubertal status and sex (14). Therefore, interactions of sex, age, height, and African ancestry with time were tested and only significant interactions were included in the final model. Analyses were also adjusted for age, sex, height and the interaction of sex with time to account for different patterns of change in males vs. females. All children in this analysis were Tanner IV or above. Tanner staging was assessed using a validated adolescent self-assessment tool (15).
Statistical Analyses
Descriptive analyses were conducted, including graphical displays of data, as appropriate. Normality of the distribution was assessed graphically and by the Kolmogorov-Smirnov test. Baseline characteristics of subjects who completed the study compared to subjects who did not complete the study are described elsewhere (9). To assess changes in total, trunk, and appendicular FM and LM, mixed effects longitudinal regression analysis was used. In these models, sex was the between-subject factor, and time and changes at 6 months and 12 months were the within-subject factors. Mixed-model analyses allows for the incorporation of proper time trends (e.g. nonlinear) and of a variance-covariance structure that accounts for the correlation between repeated measures. The mixed-model results are summarized with mean and s.e. by sex and time. A significant sex-by-time interaction indicates that, for the given outcome measure, changes from baseline differ significantly between the two sexes. In addition to the sex-by-time interaction, the age, height, baseline weight and African ancestry were entered into the model as covariates.
The unadjusted analyses characterized changes from 0 to 6 months, 6–12 months, and 0–12 months in each of the following variables: TotFM, TrFM, ApFM, TotLM, TrLM, ApLM, percent LM, percent FM, waist circumference with visit, and the interaction of sex-by time. The above model was adjusted for the following covariates: age, height, African Ancestry, and baseline weight. Spearman correlations were computed to assess associations among changes in waist circumference with TotFM, TrFM, ApFM, TotLM, TrLM, and ApLM.
Mixed-model analyses were conducted utilizing SAS statistical software (version 9.1; SAS Institute, Cary, NC). Spearman correlations were conducted utilizing STATA version 11.0 (StataCorp, College Station, TX). For all analyses, an α level of 0.05 was considered statistically significant.
RESULTS
Among the 89 adolescents enrolled and measured at baseline, 82 were randomized in the weight loss trial, and 61 completed the assessment. As reported previously (9), the characteristics of the subjects who completed the study did not differ at baseline from the characteristics of the subjects who did not complete the study. The baseline characteristics for those who completed the study are described in Table 1. The BMI-z-score for boys was significantly higher than for girls at baseline. Although there were more girls than boys, there was a higher percentage of boys of African ancestry than girls of African ancestry. There were no significant differences in body composition between sexes at baseline. There was no difference in change in LM or FM in adolescent subjects that received the drug or placebo. That is, drug X sex X visit was not a significant interaction factor in the association of change in FM and LM with change in weight; TotFM (p=0.59), pctTotFM (p=0.82), TotLM (p=0.38), pctTotLM (p=0.83), TrLM (p=0.26), TrFM (0.95), ApFM (p=0.16, ApLM (0.47). There was a significant difference in weight loss at baseline and 6 months in adolescents who received sibutramine or placebo, but there were no significant differences in body composition.
Table 1.
Baseline characteristics in adolescents (n=61)
| Boys (n=21) | Girls (n=40) | p value | |
|---|---|---|---|
|
| |||
| Percent or mean ± SD | |||
| Age (years) | 14.1±1.6 | 14.6±1.0 | 0.13 |
| Non-black, % | 53 | 81 | 0.03* |
| Weight (kg) | 96.3±17.8 | 101.25±14.90 | 0.25 |
| Height (cm) | 164.0±11.1 | 164.3±6.9 | 0.87 |
| BMI(kg/m2) | 35.5±3.1 | 37.4±4.0 | 0.07 |
| BMI z score | 2.47±0.17 | 2.36±0.19 | 0.03* |
| TotFMa (kg) | 47.7±11.6 | 51.3±10.9 | 0.23 |
| TotFM%b | 49.6±6.6 | 50.6±5.4 | 0.53 |
| TotLMc (kg) | 46.0±10.1 | 47.2±7.4 | 0.61 |
| TotLM%d | 48.2±6.6 | 46.9±5.7 | 0.44 |
| TrFMe (kg) | 21.8±6.4 | 24.3±5.3 | 0.11 |
| TrFM%f | 49.0±7.3 | 51.6±5.9 | 0.13 |
| TrLMg(kg) | 21.8±5.2 | 21.8±3.5 | 0.99 |
| TrLM%h | 49.8±7.1 | 46.9±5.8 | 0.09 |
| Waist circumference (cm) | 93.9±44.0 | 101.2±28.3 | 0.43 |
| ApFMi (kg) | 24.8±5.9 | 25.9±6.4 | 0.52 |
| ApFM%j | 53.1±7.6 | 52.7±6.2 | 0.83 |
| ApLMk (kg) | 20.6±4.8 | 21.6±4.0 | 0.36 |
| ApLM%l | 44.2±7.2 | 44.5±6.0 | 0.86 |
| Ratio TrLM/ApLM (kg) | 1.06±0.10 | 1.06±0.00 | 0.17 |
| Ratio TrFM/ApFM (kg) | 0.88±0.2 | 0.96±0.18 | 0.11 |
| Ratio TrLM/TotLM (kg) | 0.47±0.0 | 0.46±0.0 | 0.17 |
| Ratio TrFM/TotFM (kg) | 0.45±0.0 | 0.47±0.0 | 0.07 |
| Drug | 1.48±0.51 | 1.53±0.51 | 0.72 |
TotFM=total fat mass,
TotFM%=percentage total mass that is fat,
TotLM= total lean mass,
TotLM%= percentage total mass that is lean
TrFM=trunk fat mass,
TrFM%=percentage trunk mass that is fat
TrLM=trunk lean mass,
TrLM%=percentage trunk mass that is lean,
ApLM=appendicular (leg + arm) lean mass.
ApLM%=percentage appendicular mass that is lean,
ApFM= appendicular fat mass,
ApFM%=percentage appendicular mass that is fat
Body Composition
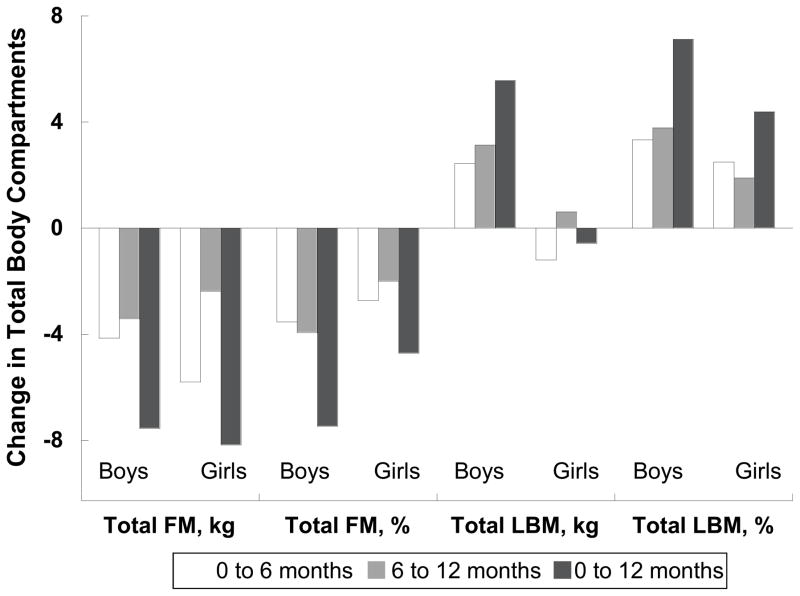
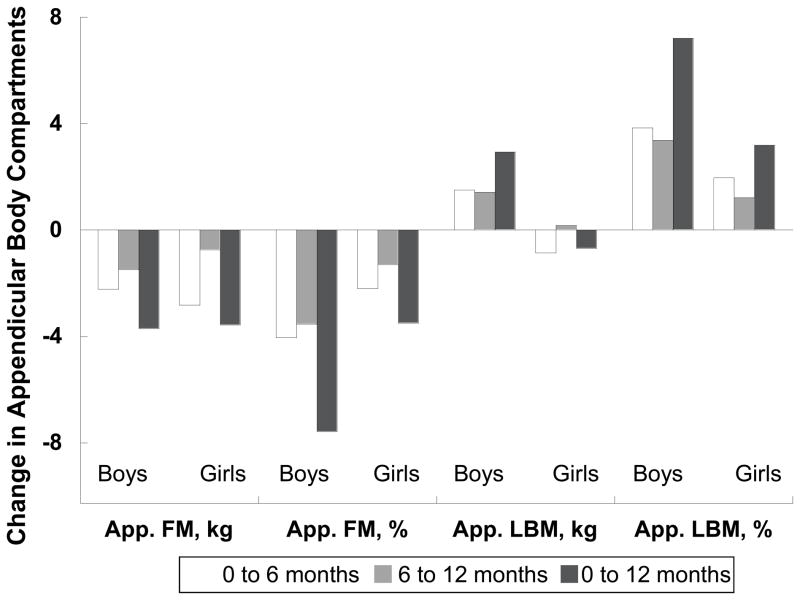
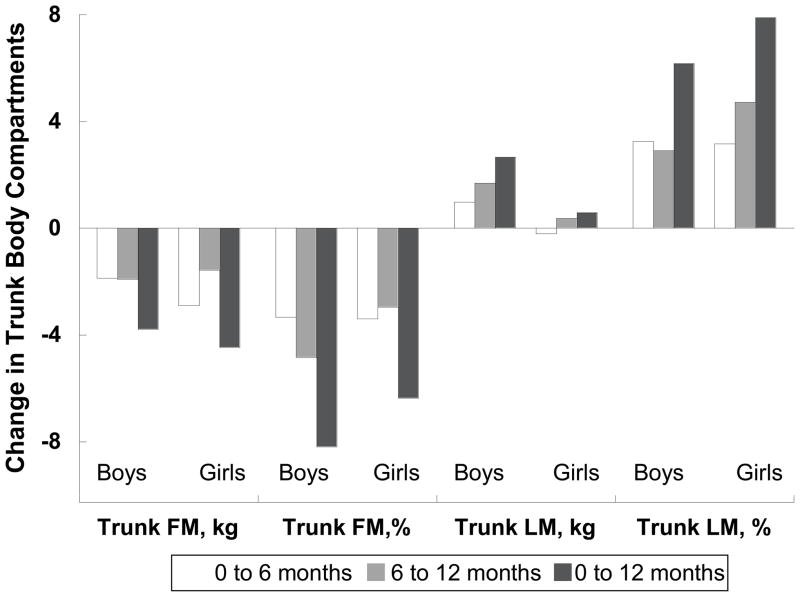
Adolescents reduced their BMI (3.22±.028 kg/m2), BMI-z-score (0.33±0.02 s.d.), weight (5.9±0.83 kg), and FM (−8.0±0.68 kg) over 12 months (p<0.001) in the unadjusted analysis and after adjusting for important growth related covariates. Figure 1 depicts the unadjusted change in total, trunk, and ApFM and LM in boys and girls at 0–6 months, 6–12 months, and 0–12 months. Table 2 depicts the changes in FM and LM and change in percent FM and percent LM in all of the compartments in the unadjusted models and the adjusted model for age, height, and African ancestry, and baseline weight.
Figure 1.
Table 2.
Total ®ional changes in body composition in 61 adolescents who completed a 12-month comprehensive weight loss program
| Boys n=21 | Girls n=40 | |||||
|---|---|---|---|---|---|---|
|
| ||||||
| Δ0–6 months | Δ6–12 months | Δ0–12months | Δ0–6 months | Δ6–12months | Δ0–12 months | |
| Weight (kg) | ||||||
| Unadjusted | −1.22 (11.80) | −0.43 (5.88) | −1.65 (13.60) | −6.29 (7.27) | −1.99 (5.52) | −8.30 (9.99) |
| aTotFM (kg) | ||||||
| Unadjusted | −4.14 (1.60) | −3.42 (1.04) | −7.56 (2.09) | −5.79 (1.17) | −2.38 (0.75) | −8.17 (1.50) |
| Adjusted | −1.97 (1.84) | −1.84 (1.11) | −3.81 (2.39) | −5.02 (1.31) | −1.47 (0.81) | −6.48 (1.71) |
| TotFM % | ||||||
| Unadjusted | −3.54 (0.86) | −3.94 (0.76) | 7.47 (1.34)* | −2.72 (0.62) | −2.00 (0.55) | −4.72 (0.97) |
| Adjusted | −1.79 (1.05) | −4.45 (1.59) | −2.66 (0.83) | −2.11 (0.74) | −2.66 (0.82) | −3.39 (1.14) |
| TotLM (kg) | ||||||
| Unadjusted | +2.44 (0.62) | +3.13 (0.61) | +5.56 (0.87) | −1.20 (0.45) | +0.62 (0.44) | −0.58 (0.62) |
| Adjusted | −0.09 (0.63) | +1.31(0.67)* | +1.22 (0.99) | −1.94 (0.45) | −0.30 (0.51)* | −2.23 (0.74) |
| TotLM % | ||||||
| Unadjusted | +3.33 (0.83) | +3.78 (0.74) | +7.12 (1.29) | +2.49 (0.60) | +1.90 (0.54) | +4.39 (0.93) |
| Adjusted | +1.76 (1.00) | +2.64 (0.81) | +4.40 (1.53) | +1.95 (0.71) | +1.26 (0.60) | +3.21 (1.10) |
| TrFM (kg) | ||||||
| Unadjusted | −1.87 (0.87) | −1.92 (0.57) | −3.79 (1.12) | −2.90 (0.63) | −1.57 (0.42) | −4.47 (0.80) |
| Adjusted | −1.22 (0.94)* | −1.44 (0.60) | −2.66 (1.24)* | −2.62 (0.68)* | −1.24 (0.44) | −3.86 (0.89)* |
| TrFM % | ||||||
| Unadjusted | −3.33 (1.16) | −4.84 (1.03) | −8.20 (1.70) | −3.40 (0.84) | −2.96 (0.75) | −6.37 (1.24) |
| Adjusted | −1.39 (1.35) | −3.45 (1.09) | −4.85 (1.96) | −2.86 (0.96) | −2.28 (0.80) | −5.15 (1.40) |
| TrLM (kg) | ||||||
| Unadjusted | +0.97 (0.30) | +1.69 (0.39)* | +2.66 (0.48) | −0.21 (0.22) | +0.58 (0.28) | +0.37 (0.35) |
| Adjusted | −0.29 (0.33) | +0.79 (0.41) | +0.50 (0.55) | −0.46 (0.24) | +0.22 (0.31) | −0.23 (0.41) |
| TrLM% | ||||||
| Unadjusted | +3.25 (0.83) | +2.91 (0.74) | +6.17 (1.21) | +3.16 (1.14) | +4.72 (1.02) | +7.88 (1.68) |
| Adjusted | +2.76 (0.94) | +2.29 (0.79) | +5.05 (1.38) | +1.33 (1.33) | +3.41 (1.08) | +4.74 (1.93) |
| Waist circumference (cm) | ||||||
| Unadjusted | −2.83 (2.19) | −1.09 (1.47) | −3.91 (2.53) | −5.62 (1.48) | −1.89 (1.05) | −7.52 (1.75) |
| Adjusted | +7.52 (9.90) | −3.80 (7.76) | +3.73 (7.75 | −2.43 (7.13) | −13.10 (5.64) | −15.53 (9.23) |
| ApFM (kg) | ||||||
| Unadjusted | −2.22 (0.77) | −1.49 (0.51) | −3.71 (−1.00) | −2.82 (0.56) | −0.74 (0.37) | −3.56 (0.72)* |
| Adjusted | −1.20 (0.91)* | −0.74 (0.57)* | −1.94 (1.22)* | −2.48 (0.64)* | −0.34 (0.43)* | −2.83 (0.88)* |
| ApFM% | ||||||
| Unadjusted | −4.05 (0.73) | −3.53 (0.69) | −7.58 (1.17) | −2.20 (0.53) | −1.31 (0.50) | −3.51 (0.85) |
| Adjusted | −2.55 (0.92) | −2.42 (0.77) | −4.97 (1.45) | −1.56 (0.65) | −0.58 (0.58) | −2.14 (1.07) |
| ApLM (kg) | ||||||
| Unadjusted | +1.51 (0.36) | +1.43 (0.29) | +2.94 ( 0.43) | −0.86 (0.26) | +0.17 (0.21) | −0.69 (0.31) |
| Adjusted | +0.32 (0.36) | +0.57 (0.33)* | +0.89 (0.50)* | −1.25 (0.26) | −0.30 (0.25)* | −1.55 (0.38)* |
| ApLM% | ||||||
| Unadjusted | +3.85 (0.70) | +3.37 (0.67) | +7.22 (1.12) | +1.97 (0.51) | +1.22 (0.48) | +3.19 (0.81) |
| Adjusted | +2.53 (0.88) | +2.39 (0.75) | +4.91 (1.40) | +1.38 (0.62) | +0.56 (0.57) | +1.95 (1.03) |
Unadjusted
Adjusted for height, age, race and baseline weight
=significant difference between sexes, bold= significant difference between visits within a sex
TotFM=total fat mass,
TotFM%=percentage total mass that is fat,
TotLM= total lean mass,
TotLM%= percentage total mass that is lean
TrFM=trunk fat mass,
TrFM%=percentage trunk mass that is fat
TrLM=trunk lean mass,
TrLM%=percentage trunk mass that is lean,
ApLM=appendicular (leg + arm) lean mass.
ApLM%=percentage appendicular mass that is lean,
ApFM= appendicular fat mass,
ApFM%=percentage appendicular mass that is fat
Total Body Composition Change
Weight loss was predominantly accounted for by change in fat mass for boys and girls even when adjusting for height, age and race (p<0.001) (Table 2). In the unadjusted model the percent of weight-loss due to fat mass for girls was 51% at 6 months, and 79.5% at 12 months. For boys, the percent of weight loss due to fat mass was 80.7% at 6 months, and 100% at 12 months. (Fig. 1) Boys lost more TotFM and TotFM% in the unadjusted model. (Fig. 1) However, when further adjusted for height, age, African ancestry, and baseline weight girls lost more TotFM and TotFM% (p< 0.001) than boys. (Table 2)
Overall, boys gained TotLM (Model 1, p=0.17), but the gain was not statistically significant in the adjusted models 2 (p=0.32) and 3 (p =0.06). Conversely, girls lost TotLM between visits, and although this was not significant in the unadjusted analyses (p=0.07), the TotLM loss became significant in the adjusted model (p=0.004) (Table 2). The TotLM% increased equally for boys and girls in all models.
Regional Body Composition Change
The change in percent TrFM accounts for 54.7% [95%CI(0.48–0.62)] while the change in percent ApFM accounts for 45.0% [95% CI (0.38–0.51)] of total change in FM (p<0.001). There was a significant decrease in TrFM and TrFM% for boys and girls in all models (Fig. 1). The change in TrFM and TrFM% was significantly greater for girls (p=0.003) in the adjusted model (Table 2). Similar to TotLM, boys gained TrLM in all models and girls lost TrLM, however there was no statistical difference between sexes. TrLM percent increased in both sexes in all models.
Boys and girls lost appendicular FM (ApFM). There was no difference of ApFM% between boys and girls in either model. Boys gained ApLM but this was only statistically significant in the unadjusted Model 1 (p<0.001). (Fig. 1) Although girls lost ApLM at each time point, there was no statistical difference between boys and girls (p>0.1). Both boys and girls gained ApLM% in the unadjusted analysis, but only boys had a significant gain in ApLM percent (p=0.001) in the adjusted model.
Waist circumference was reduced in all models for boys and girls, although this was not statistically significant. There was no difference between boys and girls in the change in waist circumference. (Table 2)
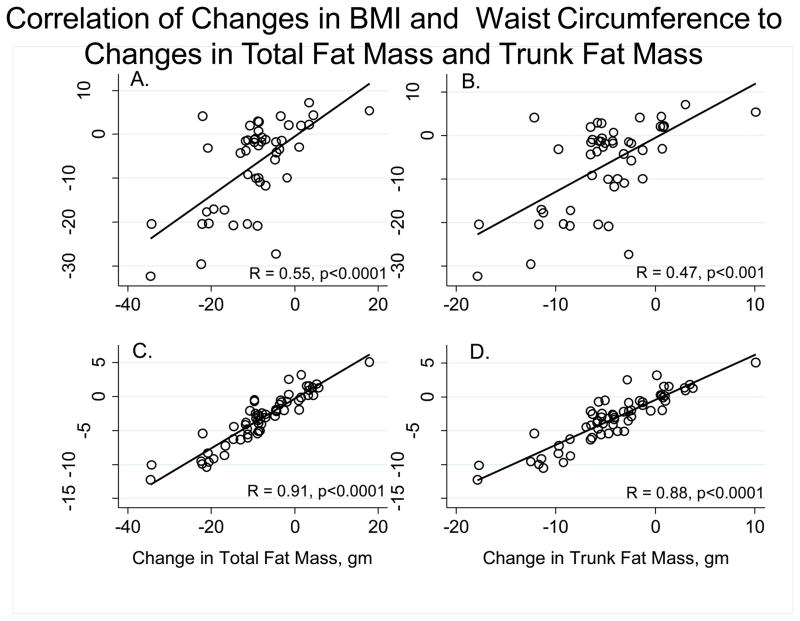
Correlation Analyses
Changes in weight were highly correlated with changes in TotFM (0.80–0.90), TrFM (0.72–0.87), and ApFM (0.78–0.89). Changes in BMI were moderate-highly correlated with changes in TotFM (0.78–0.89), TrFM (0.70–0.88), and ApFM (0.80–0.93). Changes in WC were moderately correlated with changes in TotFM (0.53–0.55), TrFM (0.47–0.51), and ApFM (0.53–0.58). Changes in weight were moderately correlated with changes in TotLM (0.45–0.57), TrLM (0.27–0.44), and ApLM (0.51–0.61). Changes in BMI had a low-moderate correlation with changes in TotLM (0.35–0.41), TrLM (0.19–0.28), and ApLM (0.41–0.45). Changes in WC had a low correlation with changes in TotLM (0.18–0.33), TrLM (−0.02–0.22), ApLM (0.30–0.42).
DISCUSSION
The body composition of weight-loss in adolescents is complex and is varied between boys and girls. The objective of this study was to determine the body composition of weight-loss using DXA during the acute (0–6 months) and maintenance phase (12 months) of weight loss in adolescents enrolled in an outpatient weight loss intervention study lasting 12 months. Weight loss in adolescents was found to be primarily from FM and mostly from trunk FM at 6 months (an acute weight-loss) and 12 months (a maintenance phase). Unlike girls, the change in kg of total FM is greater than change in kg weight (or total mass) in boys. (Table 2) Although at a single time point body compartments add up to total mass or weight. The absolute change in fat mass for boys exceeded the change in weight at 6 months and 12 months. This was true for both weight on the scale and total mass calculated with DXA. Boys gained LM, although this was not significant after adjusting for important growth parameters and baseline weight. In addition, we found that changes in BMI and waist circumference were not more strongly related to changes in TotFM or TrunkFM than change in BMI. Even after adjusting for height, age, race, and baseline weight in Tanner IV and above, girls lost LM from all regional compartments.
Prior studies have either observed body composition in the inpatient setting, had very homogeneous samples, used suboptimal methods of body composition (BIA), or were of limited duration (16, 17). This study adds to the literature through the use of longitudinal data with measurements from baseline to 6 and 12 months of treatment in an outpatient setting, and included traditional uses of multidisciplinary behavioral therapy and pharmacotherapy to induce weight loss in adolescents. Additionally, previous studies of body composition of weight loss have not included baseline weight in the analysis. This study demonstrates that changes in differences in body composition by gender are masked when baseline weight is not included in the analyses.
The effect of weight loss trials on LM in adolescents has been variable (17, 18). Earlier studies using very low calorie diets and moderate vigorous physical activity resulted in loss of LM in adults (19) and children (16). Subsequent intensive inpatient studies demonstrated maintenance of LM (16, 20). In this study which used a moderate calorie restriction, LM was preserved in boys and that although the absolute LM decreases in girls, the percentage of weight that is LM continues to increase.
Another goal of this study was to determine whether waist circumference provided important information about the composition of weight lost and its distribution. Our findings indicated that waist circumference did not improve upon BMI in providing information related to total and regional compartments of body fat. However this does not reduce the clinical utility of waist circumference as it is a predictor of cardiovascular disease and has been linked with metabolic syndrome in adults (21, 22), children and adolescents (23, 24). In other studies, baseline and final waist circumference was highly correlated with total and trunk FM (16), however change in waist circumference was only moderately correlated with change in both total trunk FM and total FM. For purposes of monitoring the composition and distribution of weight loss, our findings do not support the use of change in waist circumference over BMI to estimate change in FM in obese adolescents. Currently, waist circumference in combination with BMI is used to screen for cardiovascular and metabolic disease. Future studies examining the relationship of change in arm circumference, waist circumference, and BMI in adolescents with cardiovascular disease risk factors need to be performed.
This study has several limitations. The main limitation is the use of DXA to assess compartmental differences in FM and LM among obese adolescents. Analysis of DXA scan images requires placement of lines separating limbs from the trunk regions. For obese individuals, these lines of separation usually do not completely separate appendages from the trunk and there may be some overlap of fat between trunk and appendicular compartments. In addition, sexual maturity is an important factor influencing changes in body composition. In this sample all subjects were Tanner IV or greater; therefore, it is necessary to test these effects in a group of adolescents at earlier stages of pubertal development to further estimate the relationships in younger children. The use of a self-assessment tool for Tanner staging in obese adolescents has been found to be inaccurate, particularly for early stages, because it underestimates adolescents’ sexual maturation (25). However, adolescents in this study rated themselves as Tanner IV or greater, making this type of error much less likely (25).
Furthermore, to account for differences in physiological growth between boys and girls, we adjusted for height in our analysis. An alternative approach is to use lean mass/height2, available from recent reference data (26). We are unable to use this reference data, however as (1) bone was included in the lean mass calculations, and we excluded bone as our tissue of interest was muscle; (2) the reference data is provided in 2 year age increments, and does not have the refinement required for this 12 month study; and (3) we used a different DXA hardware and software system so our LM measurements are not comparable to the reference data. Given the rapid growth of adolescents and these other limitations, we opted to simply adjust for height in regression models so that changes in LM adjusted for height would be represented (26). Furthermore, our findings do not address the composition of lean body mass. The hydration of fat free mass (lean mass) is greater in obese adolescents (27). This hydration difference and a lack of a model that addresses measured protein in adolescent does not distinguish how much of the change in LM reflects protein versus water as assessed by DXA.
This study has unique strengths. The data were adjusted for important factors for growth in adolescents: height, age, African ancestry, and sex. The effect of baseline weight on changes in body composition was included in this study. The impact of initial weight on body composition has not been previously assessed. As the goal was to study the body composition of weight loss, only adolescents that lost weight were included in this study as we were interested in the composition of weight loss, whereas other studies have also included those who did not lose weight. Additionally, in contrast to previous studies which have primarily examined the effects of weight loss on body composition in inpatient or residential settings, this study examined the effects of weight loss in adolescents from an outpatient weight loss trial which is closer to real life conditions.
CONCLUSIONS
Adolescence is a developmental period when sex-specific changes in stature and body composition are expected to occur. This evaluation of the composition of weight loss in obese adolescents examined the pattern of change in boys and girls, and also examined the effects of growth on these outcomes. Our findings showed that in the setting of a 12 month weight loss intervention in adolescents receiving multidisciplinary behavioral therapy and pharmacotherapy, weight loss was primarily from FM in both boys and girls, and was sustained over 12 months. In addition, boys gained and girls lost LM. However, in relative terms, LM percentage increased for both males and females. While waist circumference may be a good screening measure for cardio-metabolic complications of obesity, it does not improve upon BMI as a measure to monitor changes in body composition over time.
Figure 2.
Acknowledgments
The authors would like to thank the subjects and their families for participating in the study, the staff of The Children’s Hospital of Philadelphia Nutrition and Growth Laboratory and the Center for Clinical and Translational Research. This work was supported by the National Institute of Health (R01-DK054713 to RIB), the Center for Translational Research of The Children’s Hospital of Philadelphia (M01-RR00240), and Knoll Pharmaceutical and Abbott Laboratories. EP is supported by the NIH grant 3R01HD049701-02S1. The authors would also like to acknowledge Thomas A. Wadden and Joanna L. Cronquist for their contribution.
Abbreviations
- ApFM
appendicular fat mass
- ApLM
appendicular lean mass
- BMI
body mass index
- BMC
bone mineral content
- DXA
dual-energy X-ray absorptiometry
- TotLM
total lean mass
- TotFM
total fat mass
- TrLM
trunk lean mass
- TrFM
trunk fat mass
- WC
waist circumference
Footnotes
The authors declare no conflicts of interest.
References
- 1.Ogden CL, Carroll MD, Kit BK, et al. Prevalence of obesity and trends in body mass index among US children and adolescents, 1999–2010. JAMA. 2012;307:483–490. doi: 10.1001/jama.2012.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rodriguez G, Moreno LA, Blay MG, et al. Body composition in adolescents: measurements and metabolic aspects. Int J Obes Relat Metab Disord. 2004;28 (Suppl 3):S54–8. doi: 10.1038/sj.ijo.0802805. [DOI] [PubMed] [Google Scholar]
- 3.Semiz S, Ozgoren E, Sabir N, et al. Body fat distribution in childhood obesity: association with metabolic risk factors. Indian Pediatr. 2008;45:457–462. [PubMed] [Google Scholar]
- 4.Botton J, Heude B, Kettaneh A, et al. Cardiovascular risk factor levels and their relationships with overweight and fat distribution in children: the Fleurbaix Laventie Ville Sante II study. Metabolism. 2007;56:614–622. doi: 10.1016/j.metabol.2006.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lawlor DA, Benfield L, Logue J, et al. Association between general and central adiposity in childhood, and change in these, with cardiovascular risk factors in adolescence: prospective cohort study. BMJ. 2010;341:c6224. doi: 10.1136/bmj.c6224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hills AP, Byrne NM. An overview of physical growth and maturation. Med Sport Sci. 2010;55:1–13. doi: 10.1159/000321968. [DOI] [PubMed] [Google Scholar]
- 7.Stettler N, Berkowtiz RI, Cronquist JL, et al. Observational study of bone accretion during successful weight loss in obese adolescents. Obesity (Silver Spring) 2008;16:96–101. doi: 10.1038/oby.2007.17. [DOI] [PubMed] [Google Scholar]
- 8.Taylor RW, Jones IE, Williams SM, Goulding A. Evaluation of waist circumference, waist-to-hip ratio, and the conicity index as screening tools for high trunk fat mass, as measured by dual-energy X-ray absorptiometry, in children aged 3–19 y. Am J Clin Nutr. 2000;72:490–495. doi: 10.1093/ajcn/72.2.490. [DOI] [PubMed] [Google Scholar]
- 9.Berkowitz RI, Wadden TA, Tershakovec AM, Cronquist JL. Behavior therapy and sibutramine for the treatment of adolescent obesity: a randomized controlled trial. JAMA. 2003;289:1805–1812. doi: 10.1001/jama.289.14.1805. [DOI] [PubMed] [Google Scholar]
- 10.Ware JH. Interpreting incomplete data in studies of diet and weight loss. N Engl J Med. 2003;348:2136–2137. doi: 10.1056/NEJMe030054. [DOI] [PubMed] [Google Scholar]
- 11.Kuczmarski RJ, Ogden CL, Guo SS, et al. 2000 CDC Growth Charts for the United States: methods and development. Vital Health Stat. 2002;11(246):1–190. [PubMed] [Google Scholar]
- 12.Calloway C, Chumlea W, Bouchard C. Circumferences. In: Lohman T, Roche A, Martorell R, editors. Anthropometric Standardization Manual. Vol. 39. Human Kinetics Publishers; Champaign, IL: 1988. pp. 39–64. [Google Scholar]
- 13.Nelson DA, Barondess DA. Whole body bone, fat and lean mass in children: comparison of three ethnic groups. Am J Phys Anthropol. 1997;103:157–162. doi: 10.1002/(SICI)1096-8644(199706)103:2<157::AID-AJPA2>3.0.CO;2-R. [DOI] [PubMed] [Google Scholar]
- 14.Wang J, Horlick M, Thornton JC, Levine LS, Heymsfield SB, Pierson RN., Jr Correlations between skeletal muscle mass and bone mass in children 6–18 years: influences of sex, ethnicity, and pubertal status. Growth Dev Aging. 1999;63:99–109. [PubMed] [Google Scholar]
- 15.Duke PM, Litt IF, Gross RT. Adolescents' self-assessment of sexual maturation. Pediatrics. 1980;66:918–920. [PubMed] [Google Scholar]
- 16.Dao HH, Frelut ML, Oberlin F, Peres G, Bourgeois P, Navarro J. Effects of a multidisciplinary weight loss intervention on body composition in obese adolescents. Int J Obes Relat Metab Disord. 2004;28:290–299. doi: 10.1038/sj.ijo.0802542. [DOI] [PubMed] [Google Scholar]
- 17.Knopfli BH, Radtke T, Lehmann M, et al. Effects of a multidisciplinary inpatient intervention on body composition, aerobic fitness, and quality of life in severely obese girls and boys. J Adolesc Health. 2008;42:119–127. doi: 10.1016/j.jadohealth.2007.08.015. [DOI] [PubMed] [Google Scholar]
- 18.Schwingshandl J, Borkenstein M. Changes in lean body mass in obese children during a weight reduction program: effect on short term and long term outcome. Int J Obes Relat Metab Disord. 1995;19:752–755. [PubMed] [Google Scholar]
- 19.Hoie LH, Bruusgaard D, Thom E. Reduction of body mass and change in body composition on a very low calorie diet. Int J Obes Relat Metab Disord. 1993;17:17–20. [PubMed] [Google Scholar]
- 20.Prado WL, Siegfried A, Damaso AR, Carnier J, Piano A, Siegfried W. Effects of long-term multidisciplinary inpatient therapy on body composition of severely obese adolescents. J Pediatr (Rio J) 2009;85:243–248. doi: 10.2223/JPED.1889. [DOI] [PubMed] [Google Scholar]
- 21.Despres JP, Moorjani S, Lupien PJ, Tremblay A, Nadeau A, Bouchard C. Regional distribution of body fat, plasma lipoproteins, and cardiovascular disease. Arteriosclerosis. 1990;10:497–511. doi: 10.1161/01.atv.10.4.497. [DOI] [PubMed] [Google Scholar]
- 22.Shen W, Punyanitya M, Chen J, et al. Waist circumference correlates with metabolic syndrome indicators better than percentage fat. Obesity (Silver Spring) 2006;14:727–736. doi: 10.1038/oby.2006.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Li C, Ford ES, Mokdad AH, Cook S. Recent trends in waist circumference and waist-height ratio among US children and adolescents. Pediatrics. 2006;118:e1390–8. doi: 10.1542/peds.2006-1062. [DOI] [PubMed] [Google Scholar]
- 24.Messiah SE, Arheart KL, Lipshultz SE, Miller TL. Body mass index, waist circumference, and cardiovascular risk factors in adolescents. J Pediatr. 2008;153:845–850. doi: 10.1016/j.jpeds.2008.06.013. [DOI] [PubMed] [Google Scholar]
- 25.Lee K, Valeria B, Kochman C, Lenders CM. Self-assessment of height, weight, and sexual maturation: validity in overweight children and adolescents. J Adolesc Health. 2006;39:346–352. doi: 10.1016/j.jadohealth.2005.12.016. [DOI] [PubMed] [Google Scholar]
- 26.Kelly TL, Wilson KE, Heymsfield SB. Dual energy X-Ray absorptiometry body composition reference values from NHANES. PLoS One. 2009;4:e7038. doi: 10.1371/journal.pone.0007038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wells JC, Williams JE, Chomtho S, et al. Pediatric reference data for lean tissue properties: density and hydration from age 5 to 20 y. Am J Clin Nutr. 2010;91:610–618. doi: 10.3945/ajcn.2009.28428. [DOI] [PubMed] [Google Scholar]