Abstract
Objectives
Evidence from general population based studies and occupational cohorts has identified air pollution from mobile sources as a risk factor for cardiovascular disease. In a cohort of US trucking industry workers, with regular exposure to vehicle exhaust, we previously observed elevated standardized mortality ratios (SMRs) for ischemic heart disease compared to members of the general US population. Therefore, we examined the association of increasing years of work in jobs with vehicle exhaust exposure and ischemic heart disease mortality within the cohort.
Methods
We calculated years of work in eight job groups for 30,758 workers using work records from four nationwide companies. Proportional hazard regression was used to examine relationships between ischemic heart disease mortality 1985–2000 and employment duration in each job group.
Results
Hazard ratios for at least one year of work in each job were elevated for dockworkers, long-haul drivers, pick-up and delivery drivers, combination workers, hostlers, and shop workers. There was a suggestion of an increased risk of IHD mortality with increasing years of work as a long-haul driver, pick-up and delivery driver, combination worker, and dockworker.
Conclusions
These results suggest an elevated risk of ischemic heart disease mortality in workers with a previous history of regular exposure to vehicle exhaust.
Keywords: vehicle emissions, diesel exhaust, cardiovascular disease
Introduction
There is growing evidence from population-based studies that fine particulate air pollution is a risk factor for cardiovascular disease. [1–5] The specific constituents responsible are currently not known; however, attention has focused on the importance of particles from motor vehicles that fall mostly within the fine (less than 2.5 microns in diameter – PM2.5) range.[6] There is also suggestive evidence from occupational studies that professional drivers, a group with regular exposure to particulate matter (PM) from mobile sources, have an elevated risk of cardiovascular disease.[7–12] These occupational studies have mainly been conducted in Denmark and Sweden with exposure based on occupation reported in central registers or by self-report. Detailed occupational records in a large cohort of workers with regular exposure to traffic-related PM have not been available.
In a large US cohort of trucking industry workers we have previously identified elevated Standardized Mortality Ratios (SMR) for ischemic heart disease mortality (SMR=1.41; 95% Confidence Interval (CI): 1.33–1.49) compared to the general US population.[13] We also found that, independent of occupational exposures, ambient long-term exposures to PM10, NO2, and SO2 at the last known home address were associated with an increased risk of ischemic heart disease mortality in this cohort.[14] In this industry, job and specific exposure-related duties have remained stable over time and the dates of diesel and other equipment usage are known.[15] An industrial hygiene job review was conducted to identify specific jobs and job duties in the industry and the use of diesel and non-diesel vehicles, and we conducted a national exposure assessment to characterize occupational exposures by job title.[16–20] Each company has provided us with detailed monthly work records for each individual. Thus, we have the unique opportunity to examine the effects of years of work in specific job titles within the industry on ischemic heart disease mortality while controlling for ambient pollution exposures.
Methods
Population
Details of the cohort are provided elsewhere.[13, 21] Briefly, we obtained detailed computerized work records for unionized employees working in 1985 (54,319 men and 4,007 women) from four large national companies. We used National Death Index record axis data 1985–2000 that lists both underlying and contributing causes of death and identified all deaths with ischemic heart disease (ICD-9 410–414.9; ICD-10 I20-I25.9) listed. We also considered sensitivity analyses restricting to only those cases identified as the underlying cause of death. We limited analyses to men with at least one year of work in a trucking industry job (n= 52,836) who also had ambient pollution information available (n=52,345) at their home address. Job title and duties are the same across companies, and the work records included start date, retirement, and layoff dates. This allowed us to calculate years of work in each specific trucking industry job group for each employee. Study approval was obtained from the Institutional Review Boards of Brigham and Women's Hospital, Harvard School of Public Health, and VA Boston Healthcare System.
Exposure Assessment
We categorized exposure into eight job categories based on a review of job titles and duties from a 2001–2005 industrial hygiene exposure assessment,[16–18] and information on the historical use of diesel and other vehicles by workers in the cohort.[15] The number of workers in each job in 1985 is summarized in Table 1. Long-haul drivers deliver freight from one large trucking terminal to another, and are often away from home for up to three days. Pick-up and delivery drivers bring freight to and from customers in the surrounding area and the loading dock. Dockworkers move freight from one truck to another on the loading dock, primarily using propane-powered forklifts, while hostlers move trucks and trailers in the terminal yards. Combination workers perform the duties of a dockworker and of a P&D driver as needed on a daily basis. Shop workers perform maintenance on tractors and trailers. Office workers (mostly clerks, managers, and salespeople) spend the majority of their work time in an office environment. Each worker could potentially accumulate exposure in each job category throughout his career.
Table 1.
Characteristics of the study population (N=52,345).
| Characteristic | Mean ± SD |
|---|---|
| Age in 1985 | 42.3 ± 9.9 |
| Year of Hire | 1975 ± 7.9 |
| Average annual ambient pollution 1985–2000* | |
| PM10 (μg/m3) | 26.8 ± 5.9 |
| NO2 (ppb) | 14.1 ± 7.0 |
| SO2 (ppb) | 4.8 ± 2.9 |
| Job in 1985 | Number (%) |
| Long haul driver | 13,752 |
| Pick-up and delivery (P&D) driver | 8,930 |
| Dockworker | 12,652 |
| Combination worker | 8,022 |
| Hostler | 1,258 |
| Shop worker | 3,199 |
| Office worker | 2,284 |
| Other jobs | 2,204 |
| Census Region of Residence | |
| Northeast | 8,483 (16.2) |
| South | 18,755 (35.8) |
| Midwest | 16,833 (32.2) |
| West | 8,274 (15.8) |
| Race/Ehtnicity | |
| Asian | 69 (0.1) |
| African American | 4,831 (9.2) |
| Hispanic | 2,007 (3.8) |
| Native American | 387 (0.7) |
| White | 44,114 (84.3) |
| Other | 937 (1.8) |
Based on the last-known home address
Statistical Methods
Proportional hazard regression was used to examine relationships between ischemic heart disease mortality and employment duration in each trucking industry job category. All eight job-specific exposure variables were included in regression models to adjust for different jobs held throughout a worker's career. Penalized splines,[22] were used to test for nonlinearity in mortality risk with employment duration, and the change in hazard ratio (HR) and 95% confidence intervals (CI) associated with each year of work was calculated. To closely adjust for age and secular trends, risk sets were generated using attained age in one year increments as the time scale. As individuals starting work at one of the participating companies at different ages and different time periods may have different baseline risks of IHD and that these risks will change with calendar time, we created separate baseline hazards based on categories of age in 1985 (<40, 40–49, 50–59, 60–69, 70+), calendar year and decade of hire. Race, census region of residence (based on last home address), and company were considered as potential confounders in the regression models. To control for long-term ambient pollution exposures, we included the average (1985–2000) PM10, NO2, and SO2 pollution predicted at the last known address of each employee using national exposure models we previously developed based on data from EPA monitors.[23] Time-varying variables for years employed and years off work were used to adjust for a healthy worker survivor effect. All analyses were performed in UNIX SAS 9.2 or R 2.4.1.
Indirect Adjustment for Cigarette Smoking
Information on cigarette smoking is not available from the company personnel databases. However, to assess job-related variation in smoking habits, in 2003 a questionnaire was mailed to a sample of 11,986 active and recently retired workers from the same companies as the cohort members.[24] The response rate was 40.5%, and distributions of job titles, gender, region of residence, number of employees at the workplace, and urban or rural work location among responders and non-responders were similar. We have previously shown that in logistic regression models adjusted for age, region of the country, educational status, and size and location of the workplace, long haul drivers had higher odds of being ever smokers compared to other job groups and pick-up and delivery drivers were less likely to be current smokers. To indirectly adjust for smoking, proportions of current, former, and never smokers among male questionnaire respondents for each job group were used to weight cigarette smoking literature-based fatal ischemic heart disease relative risks for US males [current smoker RR=2.4; former smoker RR=1.1 [25]]. A job-specific smoking adjustment factor was calculated by dividing the weighted risk for workers employed in each job by the weighted risk for workers not employed in that job [26, 27] and 95% CIs were calculated by considering sampling error in calculating the adjustment factors.[28]
Results
Characteristics of the analysis cohort are presented in Table 1. The average age in 1985 was 42 years old, and most workers were hired after long-haul trucks changed from gasoline to diesel during the 1950's–1960's, but before or during the transition of pick-up and delivery trucks from gasoline to diesel during the 1970's–1980's. The workers were predominantly Caucasian and lived in the South or Midwest. The largest group of workers worked as long-haul drivers in 1985, followed by pick-up and delivery drivers, dockworkers, and combination workers. There were smaller numbers of hostlers, shop workers, office workers, and people in other jobs (managers, trainees, etc.)
There were 1,357 deaths from ischemic heart disease (IHD) (1,094 as the underlying cause of death) during the follow-up period (1985–2000). Hazard ratios for IHD mortality associated with at least one year of work in each specific job category are presented in Table 2. There was little difference between the basic, healthy worker survivor effect (HWSE) adjusted, and multivariate models. Hazard ratios were statistically significantly elevated for dockworkers and long-haul drivers and were elevated for pick-up and delivery drivers, combination workers, hostlers, and shop workers. The multivariate hazard ratio for clerks was 0.63.
Table 2.
Ischemic heart disease mortality hazard ratios and 95% confidence intervals associated with any work in each major job title, follow-up 1985–2000
| Job title | Person years | Ischemic heart disease deaths | Basic Hazard Ratio (95%CI)* | HWSE Adjusted Hazard Ratio (95%CI)** | Multivariate Hazard Ratio (95%CI)*** |
|---|---|---|---|---|---|
| Long haul | 216,019 | 626 | 1.39 (1.18–1.64) | 1.41 (1.19–1.66) | 1.44 (1.22–1.70) |
| P&D | 228,961 | 369 | 1.11 (0.96–1.28) | 1.09 (0.95–1.26) | 1.11 (0.96–1.28) |
| Dockworker | 295,369 | 352 | 1.31 (1.13–1.52) | 1.30 (1.12–1.51) | 1.30 (1.12–1.51) |
| Combination | 165,151 | 201 | 1.07 (0.90–1.28) | 1.11 (0.93–1.33) | 1.11 (0.93–1.32) |
| Mechanic | 46,524 | 76 | 1.05 (0.80–1.38) | 1.07 (0.82–1.41) | 1.10 (0.84–1.44) |
| Hostler | 58,833 | 56 | 1.01 (0.77–1.33) | 1.06 (0.80–1.39) | 1.04 (0.79–1.37) |
| Clerk | 78,531 | 31 | 0.60 (0.41–0.87) | 0.61 (0.42–0.89) | 0.63 (0.43–0.91) |
Basic hazard ratios using regression coefficients from Cox proportional hazards regression models stratified on age in 1985, decade of hire, and calendar time, with risk sets by attained age, and adjusted for race.
HWSE hazard ratios additionally adjusted for the healthy worker survivor effect (total years on work, years off of work).
Multivariate hazard ratios additionally adjusted for Census region and the 1985–2000 average ambient PM10, NO2, and SO2 values at the last known residential address.
Note: Each worker could potentially accumulate exposure in multiple job categories throughout his career.
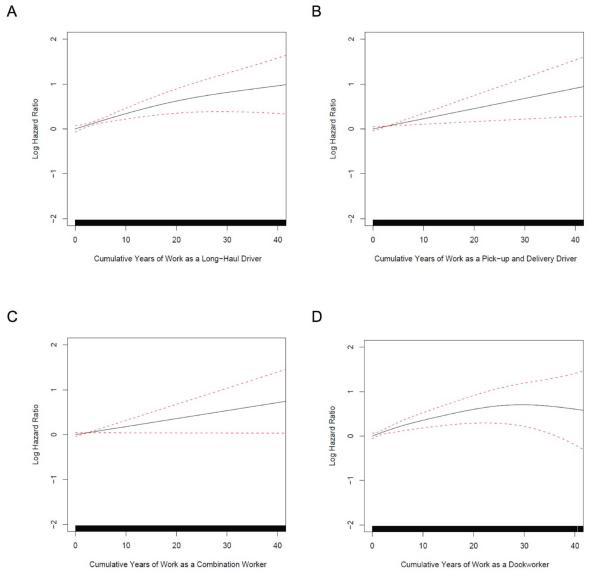
Percent change in the hazard ratio per additional year of work was calculated for long-haul drivers, pick-up and delivery drivers, dockworkers, and combination workers, the four job titles with the largest number of cases (Table 3). Based on the penalized splines (Figure 1), the association of IHD with increasing years of exposure was not statistically significantly different from linear in any of these job categories. In linear models, there was a suggestive positive association between increasing years of work in each of these four jobs and an increased risk of IHD mortality. Results were similar for models restricted to those IHD cases listed only as the underlying cause of death.
Table 3.
Ischemic heart disease hazard ratios and 95% confidence intervals associated with cumulative years of work in each major job title
| Hazard Ratio for 20 yrs of work | ||||||
|---|---|---|---|---|---|---|
| Job title | Person years | Ischemic heart disease deaths | % change in relative risk per year of work | Smoking adjustment factor* | Multivariate† | Smoking Adjusted‡ |
| Long haul | 216,019 | 626 | 4.2 (−0.9, 9.8) | 1.04 | 2.32 (0.84–6.44) | 2.23 (0.80–6.18) |
| P&D | 228,961 | 369 | 3.7 (−1.4, 9.2) | 0.92 | 2.09 (0.75–5.82) | 2.27 (0.81–6.32) |
| Dockworker | 295,369 | 352 | 3.9 (−1.2, 9.5) | 1.04 | 2.20 (0.79–6.13) | 2.11 (0.76–5.89) |
| Combination | 165,151 | 201 | 3.2 (−2.0, 8.7) | 0.98 | 1.89 (0.67–5.30) | 1.93 (0.68–5.42) |
Job-specific smoking adjustment factors were calculated by dividing the smoking weighted risk for each job by the smoking weighted risk for workers not employed in that job.
Multivariate hazard ratios using regression coefficients from Cox proportional hazards regression models stratified on age in 1985, decade of hire, and calendar time, with risk sets by attained age, adjusted for the healthy worker survivor effect (total years on work, years off of work) race, Census region of residence and the 1985–2000 average ambient PM10, NO2, and SO2 values at the last known residential address.
Smoking adjusted hazard ratios are calculated by dividing the multivariate hazard ratio by the appropriate smoking adjustment factor. The 95% CI were calculated by considering the sampling error in calculating each job-specific correction factor.
Note: Each worker could potentially accumulate exposure in multiple job categories throughout his career.
Figure 1.
Natural log of the hazard ratio and 95% confidence intervals for ischemic heart disease mortality risk for cumulative years of work as a (A) long-haul driver, (B) pick-up and delivery driver, (C) dockworker, and (D) combination worker. The solid lines indicate the natural log of the hazard ratio, and the dotted lines are the 95% confidence intervals. A histogram of the distribution of years of work is at the bottom of each graph.
The job-specific coefficients from the regression models in Table 3 were used to estimate hazard ratios for 20 years of work. The job-specific smoking adjustment factors were used to estimate smoking-adjusted risks by dividing each job-specific regression coefficient by the appropriate adjustment factor. After the indirect smoking adjustment, the hazard ratios did not appreciably change in any of the job groups.
Discussion
Within this population of U.S. trucking industry employees, jobs associated with exposures to vehicle exhaust were associated with increases in ischemic heart disease mortality. Increasing years of work was associated with increases in ischemic heart disease mortality, although these increases were not statistically significant. These exposures were robust to adjustment for residential ambient average PM10, NO2, and SO2 pollution and indirect adjustments for cigarette smoking. Clerks, who did not work in a job with regular exposure to vehicle exhaust, had a decreased risk of dying of IHD. Our findings of elevated risks in the specific job titles are consistent with our earlier SMR analysis comparing this population to members of the general US population (SMRs: ever driver = 1.49 (95% CI, 1.40–1.59), ever dockworker = 1.32 (95% CI, 1.15–1.52, ever mechanic = 1.34 (95% CI, 1.05–1.72)).
Other studies have reported elevated risks of cardiovascular disease in professional drivers, an occupational group with regular exposure to PM from mobile sources, although not all studies have reported elevated risks [7–11]. In Danish bus, taxi, and truck drivers, rates of hospital admissions for ischemic heart disease were consistently elevated in successive 5-year cohorts of 20–59 year old men studied between 1981 and 1997. Compared to rates in other employed Danish men, the risk was significantly increased 20 to 80% [11]. Gustavsson et al [29] found a significantly elevated risk of myocardial infarction among 691 long distance truck drivers in five counties in Sweden (Relative Risk=1.31). The risk was not elevated among short distance truck drivers, but relatively few (only 169) were included in the study. In a later case-control study assessing cardiovascular risk factors in survivors of first time myocardial infarction ages 45–70 in Stockholm County between 1992–1994, Gustavsson et al. [30] used a job-exposure matrix to estimate vehicle exhaust exposure intensity and duration. Adjusting for gender, smoking, diabetes, and body mass index, the risk associated with greater exposure levels was 1.2 to 1.3. In a similar analysis in the same cohort, but based on job title, male bus and taxi drivers who worked for more than 1 year had a non-statistically significantly elevated risk (RR=1.49; 95% CI 0.90–2.45 and RR=1.34; 95% CI 0.82–2.19, respectively). The risk among truck drivers was 1.10; 95% CI 0.79–1.53 [31].
Current research efforts suggest that exposure to PM from mobile sources is responsible for adverse cardiovascular events in the general population as well. A prospective study of 4,466 participants followed for eight years in the Netherlands concluded that long-term exposure to traffic-related particulate air pollution measured by ambient Black Smoke measurements, an indicator of elemental carbon (EC), presumably from gasoline and diesel-powered vehicles, was associated with increased all cause mortality (RR=1.32, 95%CI=0.98–1.78) and specifically cardiopulmonary mortality (RR=1.71; 95%CI=1.10–2.67) for each 10 μg/m3 increase in Black Smoke [32]. An analysis based on specific elements from particles in 6 US Cities found greater effects on daily mortality rates (particularly for cardiovascular deaths) attributable to particles from mobile sources than to particles from other sources [33]. Death from cardiovascular disease in Western European cities has been associated with daily ambient concentrations of Black Smoke [34].
PM from mobile sources has also been associated with non-fatal cardiovascular disease and systemic markers associated with a greater disease risk. The increased risk of cardiovascular hospitalization associated with a fixed increment in recent exposure to ambient particles has been shown to increase with the percent of the particles emitted from traffic sources [35]. In a US Medicare cohort examining the constituents of PM2.5, one of the strongest associations was observed between EC and cardiovascular admissions [36]. Findings from Peters et al. also supported a more specific role for traffic related particles in cardiovascular damage [37]. In a Boston-based cohort of subjects wearing implantable defibrillators EC and nitrogen dioxide (NO2) (markers of traffic exposure), were stronger predictors of defibrillator discharge than PM2.5. Similarly, in a London study, Black Smoke and NO2 showed stronger associations with plasma fibrinogen – an intermediate marker of cardiovascular disease risk– than particulate matter less than 10 microns in diameter (PM10) [38]]. Peters and coworkers found that exposure to traffic was associated with the time of onset of myocardial infarction [39]. In a study of state police troopers riding in their patrol cars, in-vehicle PM (presumably from traffic sources) was associated with elevations in C-reactive protein and changes in heart-rate variability [40]. In a design similar to our current study, but based in the general population, residents living closer to traffic had a greater risk of incident coronary heart disease, adjusting for residential background air pollution [41]. These observations indicate that exposure to fine particles from traffic can influence the occurrence of clinical IHD and in some studies, systemic markers of inflammation.
Recent studies have assessed the mechanism responsible for the association of cardiovascular disease mortality with traffic-related exposures. Traffic-exposures may specifically adversely affect future IHD by accelerating systemic atherosclerosis (and presumably coronary atherosclerosis) assessed based on quantity of aortic calcification [42], increase in pulse-wave velocity [43], and carotid intima-media thickness [44, 45]. Findings in experimental animal models also support the potential for fine particulate air pollution and specifically traffic-related particles to contribute to the progression of atherosclerosis [46–48].
A limitation of this analysis is the lack of personal information on potential risk factors for ischemic heart disease. Although cigarette smoking is an important risk factor, the degree that it is a confounder in this study depends on differences in smoking behavior associated with job title within the cohort. To minimize the possible effect of uncontrolled confounding by smoking, we have studied workers of similar socioeconomic class, a known correlate of smoking habits [49, 50]. Although we were unable to directly survey workers in this cohort, using a representative sample of active and retired workers in the industry [24], we found that variation in ischemic heart disease risk among exposed workers did not reflect differences in smoking rates, and adjustment did not significantly influence the observed results. As expected [51] we found that smoking rates in the survey varied by age and birth cohort [13]. Although a limitation of this indirect adjustment is that smoking patterns between jobs may have been different historically, we found that birth-cohort specific smoking rates were similar among drivers and non-drivers [13], suggesting that smoking rates did not vary substantially between jobs. In addition, all analyses are tightly controlled for age and calendar year. However, it is still possible that residual confounding by smoking exists. In addition, we do not have information on other important potential confounders, such as physical activity, diet, alcohol consumption, family history, medication use, etc, which, if also related to job title could partially explain our results. Other job related factors, such as stress, noise, personal work practices, in addition to or instead of traffic pollution exposures may also explain our results. Without direct information on each of these factors, we are unable to definitely determine the precise factors of these job titles responsible for the elevated risk of IHD.
To conclude, our results suggest that ischemic heart disease mortality in workers with a previous history of regular exposures to vehicle exhaust is elevated and that this risk may increase with increasing exposure duration.
What this paper adds
Occupational studies of professional drivers, conducted mainly in Denmark and Sweden, have identified elevations in ischemic heart disease in this occupational group. The results of this study suggest that workers in the US trucking industry with a variety of patterns of exposure to vehicle exhaust are at an increased risk of mortality from ischemic heart disease, and that this risk may increase with increasing years of work.
Acknowledgements
The authors thank Marina Jacobson Canner for programming assistance, the Teamster Safety and Health Dept. (LaMont Byrd); the Central States Pension Fund (Bill Schaefer), and the participating companies.
Footnotes
Sources of financial support: NIH/NCI R01 CA90792; NIEHS ES00002
References
- 1.Health Effects Institute . Particulate air pollution and daily mortality: Replication and validation of selected studies. Health Effects Institute; Andover, MA: Aug, 1995. 1995 Contract No.: Document Number|. [Google Scholar]
- 2.Samet JM, Dominici F, Curriero FC, et al. Fine particulate air pollution and mortality in 20 U.S. cities, 1987–1994. N Engl J Med. 2000 Dec 14;343(24):1742–9. doi: 10.1056/NEJM200012143432401. [DOI] [PubMed] [Google Scholar]
- 3.Pope CA, 3rd, Burnett RT, Thun MJ, et al. Lung cancer, cardiopulmonary mortality, and long-term exposure to fine particulate air pollution. Jama. 2002;287(9):1132–41. doi: 10.1001/jama.287.9.1132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pope CA, 3rd, Burnett RT, Thurston GD, et al. Cardiovascular mortality and long-term exposure to particulate air pollution: epidemiological evidence of general pathophysiological pathways of disease. Circulation. 2004 Jan 6;109(1):71–7. doi: 10.1161/01.CIR.0000108927.80044.7F. [DOI] [PubMed] [Google Scholar]
- 5.Dockery DW, Pope ACd, Xu X, et al. An association between air pollution and mortality in six U.S. cities. N Engl J Med. 1993;329(24):1753–9. doi: 10.1056/NEJM199312093292401. [DOI] [PubMed] [Google Scholar]
- 6.Bagley ST, Baumgard KJ, Gratz LD, et al. Health Effects Institute; Cambridge, MA: 1986. Characterization of fuel and after treatment device effects on diesel emissions. Contract No.: Document Number|. [PubMed] [Google Scholar]
- 7.Holme I, Helgeland A, Hjermann I, et al. Coronary risk factors in various occupational groups: the Oslo study. Br J Prev Soc Med. 1977 Jun;31(2):96–100. doi: 10.1136/jech.31.2.96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rosengren A, Anderson K, Wilhelmsen L. Risk of coronary heart disease in middle-aged male bus and tram drivers compared to men in other occupations: a prospective study. Int J Epidemiol. 1991 Mar;20(1):82–7. doi: 10.1093/ije/20.1.82. [DOI] [PubMed] [Google Scholar]
- 9.Hammar N, Alfredsson L, Smedberg M, et al. Differences in the incidence of myocardial infarction among occupational groups. Scand J Work Environ Health. 1992 Jun;18(3):178–85. doi: 10.5271/sjweh.1590. [DOI] [PubMed] [Google Scholar]
- 10.Tuchsen F, Bach E, Marmot M. Occupation and hospitalization with ischaemic heart diseases: a new nationwide surveillance system based on hospital admissions. Int J Epidemiol. 1992 Jun;21(3):450–9. doi: 10.1093/ije/21.3.450. [DOI] [PubMed] [Google Scholar]
- 11.Hannerz H, Tuchsen F. Hospital admissions among male drivers in Denmark. Occup Environ Med. 2001 Apr;58(4):253–60. doi: 10.1136/oem.58.4.253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fang SC, Cassidy A, Christiani DC. A systematic review of occupational exposure to particulate matter and cardiovascular disease. Int J Environ Res Public Health. 2010 Apr;7(4):1773–806. doi: 10.3390/ijerph7041773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Laden F, Hart JE, Smith TJ, et al. Cause specific mortality in the unionized U.S. trucking industry. Environ Health Perspect. 2007;115(8):1192–6. doi: 10.1289/ehp.10027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hart JE, Garshick E, Dockery DW, et al. Long-term ambient multipollutant exposures and mortality. American Journal of Respiratory and Critical Care Medicine. doi: 10.1164/rccm.200912-1903OC. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Garshick E, Smith TJ, Laden F. Quantitative Assessment of Lung Cancer Risk from Diesel Exhaust Exposure in the US Trucking Industry: A Feasibility Study. In: Diesel Epidemiology Working Group, editor. Research Directions for Improve Estimates of Human Exposure and Risk from Diesel Exhaust. Health Effects Institute; Boston, MA: 2002. [Google Scholar]
- 16.Smith TJ, Davis ME, Reaser P, et al. Overview of particulate exposures in the US trucking industry. J Environ Monit. 2006 Jul;8(7):711–20. doi: 10.1039/b601809b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Davis ME, Smith TJ, Laden F, et al. Driver exposure to combustion particles in the US trucking industry. Journal of Occupational and Environmental Hygiene. 2007;4(11):848–54. doi: 10.1080/15459620701643347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Davis ME, Smith TJ, Laden F, et al. Modeling Particle Exposure in US Trucking Terminals Environmental Science and Technology. 2006;40(13):4226–32. doi: 10.1021/es052477m. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sheesley RJ, Schauer JJ, Garshick E, et al. Tracking personal exposure to particulate diesel exhaust in a diesel freight terminal using organic tracer analysis. J Expo Sci Environ Epidemiol. 2008 Mar 5; doi: 10.1038/jes.2008.11. doi:10.1038/jes.2008.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sheesley RJ, Schauer JJ, Smith TJ, et al. Assessment of diesel particulate matter exposure in the workplace: freight terminals. J Environ Monit. 2008 Mar;10(3):305–14. doi: 10.1039/b715429a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Garshick E, Laden F, Hart JE, et al. Lung Cancer and Vehicle Exhaust in Trucking Industry Workers. Environmental Health Perspectives. 2008 May 30;116(10):1327–32. doi: 10.1289/ehp.11293. 2008 Epub. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Thurston SW, Eisen EA, Schwartz J. Smoothing in survival models: an application to workers exposed to metalworking fluids. Epidemiology. 2002 Nov;13(6):685–92. doi: 10.1097/00001648-200211000-00013. [DOI] [PubMed] [Google Scholar]
- 23.Hart JE, Yanosky JD, Puett RC, et al. Spatial Modeling of PM10 and NO2 1985–2000 in the Continental US. Environmental Health Perspectives. 2009;117(11):1690–6. doi: 10.1289/ehp.0900840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jain N, Hart JE, Smith TJ, et al. Smoking behavior in trucking industry workers. American Journal of Industrial Medicine. 2006 Dec;49(12):1013–20. doi: 10.1002/ajim.20399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Doyle JT, Dawber TR, Kannel WB, et al. The Relationship of Cigarette Smoking toCoronary Heart Disease: The Second Report of the Combined Experience of the Albany, NY, and Framingham, Mass, Studies. Journal of the American Medical Association. 1964;190(10):108–12. [PubMed] [Google Scholar]
- 26.Schlesselman JJ. Assessing effects of confounding variables. Am J Epidemiol. 1978;108(1):3–8. [PubMed] [Google Scholar]
- 27.Axelson O. Aspects of confounding and effect modification in the assessment of occupational cancer risk. J Toxicol Environ Health. 1980;6(5–6):1127–31. doi: 10.1080/15287398009529933. [DOI] [PubMed] [Google Scholar]
- 28.Larkin EK, Smith TJ, Stayner L, et al. Diesel exhaust and lung cancer: Adjustment for the effects of smoking in a retrospective cohort study. Am J Ind Med. 2000;38(4):399–409. doi: 10.1002/1097-0274(200010)38:4<399::aid-ajim5>3.0.co;2-d. [DOI] [PubMed] [Google Scholar]
- 29.Gustavsson P, Alfredsson L, Brunnberg H, et al. Myocardial infarction among male bus, taxi, and lorry drivers in middle Sweden. Occup Environ Med. 1996 Apr;53(4):235–40. doi: 10.1136/oem.53.4.235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gustavsson P, Plato N, Hallqvist J, et al. A population-based case-referent study of myocardial infarction and occupational exposure to motor exhaust, other combustion products, organic solvents, lead, and dynamite. Stockholm Heart Epidemiology Program (SHEEP) Study Group. Epidemiology. 2001;12(2):222–8. doi: 10.1097/00001648-200103000-00015. [DOI] [PubMed] [Google Scholar]
- 31.Bigert C, Gustavsson P, Hallqvist J, et al. Myocardial infarction among professional drivers. Epidemiology. 2003 May;14(3):333–9. [PubMed] [Google Scholar]
- 32.Hoek G, Brunekreef B, Goldbohm S, et al. Association between mortality and indicators of traffic-related air pollution in the Netherlands: a cohort study. Lancet. 2002;360(9341):1203–9. doi: 10.1016/S0140-6736(02)11280-3. [DOI] [PubMed] [Google Scholar]
- 33.Laden F, Neas LM, Dockery DW, et al. Association of fine particulate matter from different sources with daily mortality in six U.S. cities. Environ Health Perspect. 2000;108(10):941–7. doi: 10.1289/ehp.00108941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zmirou D, Schwartz J, Saez M, et al. Time-series analysis of air pollution and cause-specific mortality. Epidemiology. 1998 Sep;9(5):495–503. [PubMed] [Google Scholar]
- 35.Janssen NA, Schwartz J, Zanobetti A, et al. Air conditioning and source-specific particles as modifiers of the effect of PM(10) on hospital admissions for heart and lung disease. Environ Health Perspect. 2002;110(1):43–9. doi: 10.1289/ehp.0211043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bell ML, Ebisu K, Peng RD, et al. Hospital admissions and chemical composition of fine particle air pollution. Am J Respir Crit Care Med. 2009 Jun 15;179(12):1115–20. doi: 10.1164/rccm.200808-1240OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Peters A, Liu E, Verrier RL, et al. Air pollution and incidence of cardiac arrhythmia. Epidemiology. 2000;11(1):11–7. doi: 10.1097/00001648-200001000-00005. [DOI] [PubMed] [Google Scholar]
- 38.Pekkanen J, Brunner EJ, Anderson HR, et al. Daily concentrations of air pollution and plasma fibrinogen in London. Occup Environ Med. 2000 Dec;57(12):818–22. doi: 10.1136/oem.57.12.818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Peters A, von Klot S, Heier M, et al. Exposure to traffic and the onset of myocardial infarction. N Engl J Med. 2004 Oct 21;351(17):1721–30. doi: 10.1056/NEJMoa040203. [DOI] [PubMed] [Google Scholar]
- 40.Riediker M, Cascio WE, Griggs TR, et al. Particulate matter exposure in cars is associated with cardiovascular effects in healthy young men. Am J Respir Crit Care Med. 2004 May 15;169(8):934–40. doi: 10.1164/rccm.200310-1463OC. [DOI] [PubMed] [Google Scholar]
- 41.Kan H, Heiss G, Rose KM, et al. Prospective analysis of traffic exposure as a risk factor for incident coronary heart disease: the Atherosclerosis Risk in Communities (ARIC) study. Environ Health Perspect. 2008 Nov;116(11):1463–8. doi: 10.1289/ehp.11290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Allen RW, Criqui MH, Diez Roux AV, et al. Fine particulate matter air pollution, proximity to traffic, and aortic atherosclerosis. Epidemiology. 2009 Mar;20(2):254–64. doi: 10.1097/EDE.0b013e31819644cc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lenters V, Uiterwaal CS, Beelen R, et al. Long-term exposure to air pollution and vascular damage in young adults. Epidemiology. Jul;21(4):512–20. doi: 10.1097/EDE.0b013e3181dec3a7. [DOI] [PubMed] [Google Scholar]
- 44.Kunzli N, Jerrett M, Garcia-Esteban R, et al. Ambient air pollution and the progression of atherosclerosis in adults. PLoS One. 5(2):e9096. doi: 10.1371/journal.pone.0009096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kunzli N, Jerrett M, Mack WJ, et al. Ambient air pollution and atherosclerosis in Los Angeles. Environ Health Perspect. 2005 Feb;113(2):201–6. doi: 10.1289/ehp.7523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lund AK, Lucero J, Lucas S, et al. Vehicular emissions induce vascular MMP-9 expression and activity associated with endothelin-1-mediated pathways. Arterioscler Thromb Vasc Biol. 2009 Apr;29(4):511–7. doi: 10.1161/ATVBAHA.108.176107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Floyd HS, Chen LC, Vallanat B, et al. Fine ambient air particulate matter exposure induces molecular alterations associated with vascular disease progression within plaques of atherosclerotic susceptible mice. Inhal Toxicol. 2009 Apr;21(5):394–403. doi: 10.1080/08958370802317745. [DOI] [PubMed] [Google Scholar]
- 48.Campen MJ, Lund AK, Knuckles TL, et al. Inhaled diesel emissions alter atherosclerotic plaque composition in ApoE(−/−) mice. Toxicol Appl Pharmacol. Feb 1;242(3):310–7. doi: 10.1016/j.taap.2009.10.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Brackbill R, Frazier T, Shilling S. Smoking characteristics of US workers, 1978–1980. Am J Ind Med. 1988;13(1):5–41. doi: 10.1002/ajim.4700130103. [DOI] [PubMed] [Google Scholar]
- 50.Stellman SD, Boffetta P, Garfinkel L. Smoking habits of 800,000 American men and women in relation to their occupations. Am J Ind Med. 1988;13(1):43–58. doi: 10.1002/ajim.4700130104. [DOI] [PubMed] [Google Scholar]
- 51.Burns D, Shanks T, Choi E, et al. Burns D, Garfinkel L, Samet J, editors. The American Cancer Society cancer prevention study I: 12-year followup of 1 million men and women. Changes in cigarette-relate disease risks and their inplication for prevention and control 113–304. National Institutes of Health. 1997 [Google Scholar]