Abstract
Background
The quality of the continuity clinic experience for internal medicine (IM) residents may influence their choice to enter general internal medicine (GIM), yet few data exist to support this hypothesis.
Objective
To assess the relationship between IM residents’ satisfaction with continuity clinic and interest in GIM careers.
Design
Cross-sectional survey assessing satisfaction with elements of continuity clinic and residents' likelihood of career choice in GIM.
Participants
IM residents at three urban medical centers.
Main Measures
Bivariate and multivariate associations between satisfaction with 32 elements of outpatient clinic in 6 domains (clinical preceptors, educational environment, ancillary staff, time management, administrative, personal experience) and likelihood of considering a GIM career.
Key Results
Of the 225 (90 %) residents who completed surveys, 48 % planned to enter GIM before beginning their continuity clinic, whereas only 38 % did as a result of continuity clinic. Comparing residents’ likelihood to enter GIM as a result of clinic to likelihood to enter a career in GIM before clinic showed that 59 % of residents had no difference in likelihood, 28 % reported a lower likelihood as a result of clinic, and 11 % reported higher likelihood as a result of clinic. Most residents were very satisfied or satisfied with all clinic elements. Significantly more residents (p ≤ 0.002) were likely vs. unlikely to enter GIM if they were very satisfied with faculty mentorship (76 % vs. 53 %), time for appointments (28 % vs. 11 %), number of patients seen (33 % vs. 15 %), personal reward from work (51 % vs. 23 %), relationship with patients (64 % vs. 42 %), and continuity with patients (57 % vs. 33 %). In the multivariate analysis, being likely to enter GIM before clinic (OR 29.0, 95 % CI 24.0–34.8) and being very satisfied with the continuity of relationships with patients (OR 4.08, 95 % CI 2.50–6.64) were the strongest independent predictors of likelihood to enter GIM as a result of clinic.
Conclusions
Resident satisfaction with most aspects of continuity clinic was high; yet, continuity clinic had an overall negative influence on residents’ attitudes toward GIM careers. Targeting resources toward improving ambulatory patient continuity, workflow efficiency and increasing pre-residency interest in primary care may help build the primary care workforce.
Key Words: medical education—career choice, medical education—graduate, primary care, ambulatory medicine
Introduction
The US faces a critical shortage in the primary care workforce, which will soon be inadequate to meet the needs of the aging US population.1,2 Trends in medical student and resident career choices over the last decade offer little optimism that this shortage can be avoided.2–6 From 1997 to 2006, the number of US medical school graduates likely to pursue primary care residencies (family medicine, general medicine, general pediatrics) declined from 43.5 % to 20.2%,5 and from 2002 to 2007 the number of US resident physicians intending to practice primary care decreased from 28.1 % to 23.8 %.3 Internal medicine (IM) residency programs train one-fourth of all residents7 but are producing fewer graduates pursuing primary care careers. From 1998 to 2006, the number of US medical school graduates intending to pursue general internal medicine (GIM) decreased from 15.7 % to 6.7 %,5 and from 1998 to 2003 the proportion of IM residents planning to enter GIM declined from 54 % to 27 %.4
Many believe that dissatisfaction with the continuity clinic experience may discourage trainees from selecting primary care careers.8–11 The challenges residents face during their continuity clinics include lack of continuity with patients, burdensome administrative duties, lack of support for coordination of care and disease management, staffing shortages, distraction from inpatient duties, and dissatisfied primary care role models, all against the backdrop of managing patient panels full of medically and socially complex patients.8–11 In an effort to improve the ambulatory continuity experience, several important stakeholders in IM have called for reform.7,12–14 Specifically, in 2009, the ACGME IM Residency Review Committee required IM residents to have 130 ambulatory half–day sessions over 3 years, up from 108 in 2004, and mandated decreased conflict between ambulatory and inpatient experiences and improved coordination of care and mentorship in clinic.7,9 While these efforts were, in part, motivated by the primary care workforce crisis, it is not clear whether changes to the ambulatory care experience will actually impact career choices of IM residents.
The goals of this study were to assess resident satisfaction with continuity clinic and the association of the resident clinic experience with resident attitudes toward careers in GIM. We hypothesized that IM residents’ satisfaction with many elements of continuity clinic would be low, that the continuity clinic experience would influence residents away from GIM careers, and that high resident satisfaction with continuity clinic would be associated with a higher self-reported likelihood of pursuing a GIM career.
Methods
Study Design and Setting
We administered a survey at two tertiary care hospital centers, Mount Sinai School of Medicine (MSSM) in New York City, NY, and Temple University School of Medicine (TUSM) in Philadelphia, PA, between April and July 2010, and at one community hospital, Johns Hopkins Bayview Medical Center (JHBMC) in Baltimore, MD, between May and July 2011. The programs were selected as a result of collaboration at a regional SGIM meeting. The IM residency programs at these institutions had similar team-based, ambulatory clinic structures and all programs had primary care programs within their categorical program. The study was approved by the Institutional Review Boards at all three institutions.
Participants
All IM residents at the three institutions who had continuity clinic were eligible to participate in the study (e.g., categorical and primary care residents were included, preliminary year interns were not). At MSSM and JHBMC, residents were recruited in person at conferences and completed paper surveys. At TUSM, residents were recruited via email and completed Internet-based surveys (SurveyMonkey). The survey took approximately 10 min to complete. All data were de-identified and aggregated.
Survey Design and Domain Structure
The survey was adapted from the Veterans Affairs (VA) Learner’s Perception Survey (LPS), which had been previously modified for the continuity clinic experience15,16 and has been used in other studies, including the Accreditation Council for Graduate Medical Education (ACGME)-sponsored Educational Innovations Project.17,18 The Continuity Clinic LPS asks residents to use a five-item Likert scale to rate their satisfaction with 35 elements of clinic in five domains: (1) clinical preceptors; (2) learning environment; (3) working environment; (4) clinical environment; (5) personal environment.15,16 We conducted principle components analysis on a subset of the data, which resulted in dropping 3 items because of redundancy and adding an additional domain, making a 32-item survey with 6 domains (Table 3), which demonstrated content validity based on the available literature.15,16,19–24 The final domains and their Cronbach alpha scores are (1) clinical preceptors (0.866), (2) educational environment (0.763), (3) ancillary staff (0.600), (4) time management (0.878), (5) administrative: records/space (0.708), and (6) personal experience (0.853). Although ancillary staff had a lower than typically acceptable Cronbach’s alpha, we kept this domain because the grouping intuitively made sense (front desk, nursing and medical assistant staff) and because we did not use the domains to create scores.
Table 3.
Percentage of Residents Very Satisfied with Clinic Element by Self-reported Likelihood of Entering GIM AS A RESULT of Clinic
| Percent of residents very satisfied | |||
|---|---|---|---|
| Clinic domains and elements (n = 225) | Likely to Enter GIM | Unlikely to Enter GIM | p value |
| n = 86 | n = 139 | ||
| n (%) | n (%) | ||
| Clinical preceptors | |||
| Teaching ability | 70 (82) | 104 (75) | 0.22 |
| Timeliness of feedback | 54 (66) | 78 (57) | 0.21 |
| Fairness in evaluation | 60 (77) | 87 (67) | 0.14 |
| Being role models | 73 (87) | 96 (70) | 0.004 |
| Evidence-based clinical practice | 66 (78) | 86 (62) | 0.01 |
| Mentorship from faculty | 64 (76) | 72 (53) | 0.001* |
| Educational environment | |||
| Degree of supervision | 59 (69) | 96 (69) | 0.96 |
| Preparation for clinical practice | 46 (54) | 61 (44) | 0.14 |
| Access to specialty expertise | 29 (34) | 106 (23) | 0.06 |
| Spectrum of patient problems/diseases | 40 (47) | 49 (35) | 0.08 |
| Degree of autonomy | 73 (86) | 101 (73) | 0.02 |
| Enhancement of your clinical knowledge/skills | 36 (43) | 35 (25) | 0.005 |
| Ancillary staff | |||
| Front desk staff in your firm | 34 (40) | 55 (40) | 0.95 |
| Nursing staff in your firm | 64 (78) | 106 (78) | 0.98 |
| Medical assistant staff in your firm | 53 (64) | 87 (63) | 0.90 |
| Time management | |||
| Number of clinic patients seen | 28 (33) | 20 (15) | 0.001* |
| Time allotted to see patients | 24 (28) | 15 (11) | 0.001* |
| Timely availability of follow-up appointments | 24 (29) | 22 (16) | 0.02 |
| Timely availability of acute care appointments | 29 (35) | 27 (20) | 0.01 |
| Ability to focus during clinic | 27 (32) | 23 (16) | 0.007 |
| Ability to balance ward/inpatient duties on clinic days | 16 (19) | 16 (11) | 0.12 |
| Time for learning | 34 (40) | 36 (26) | 0.03 |
| Management of patient phone calls | 13 (16) | 14 (10) | 0.24 |
| Administrative: records/space | |||
| Ease of getting patient records | 19 (22) | 32 (23) | 0.91 |
| Amount of “paperwork” | 11 (13) | 14 (10) | 0.51 |
| Patient record system | 37 (44) | 57 (41) | 0.66 |
| Space for precepting with faculty | 47 (55) | 57 (41) | 0.04 |
| Personal experience | |||
| Personal reward from work | 43 (51) | 32 (23) | <0.001* |
| Relationship with patients | 54 (64) | 59 (42) | 0.002* |
| Continuity of relationship with patients | 48 (57) | 45 (33) | <0.001* |
| Ownership/personal responsibility for patients' care | 52 (62) | 58 (42) | 0.004 |
| Quality of care your patients receive | 30 (35) | 34 (24) | 0.08 |
Differences calculated using chi-square test.
*
Significant at p ≤ 0.002 by Bonferonni correction
In addition to the satisfaction questions, we included two questions asking residents to rate their likelihood “to enter a career in GIM” across a four-point Likert scale: (1) “BEFORE the continuity clinic experience” and (2) “AS A RESULT of the continuity clinic experience.” Our modified survey also included questions regarding gender, postgraduate year, training site, work plan, and practice setting plan.
Statistical Analysis
Demographic and career plan responses were compared across sites using chi-square analysis. Individual satisfaction item responses were skewed toward very satisfied, so we dichotomized responses for these items for analysis into very satisfied (very satisfied response only) and not very satisfied (somewhat satisfied, somewhat dissatisfied, and very dissatisfied).25 Choice of a career in GIM was dichotomized as somewhat or very likely versus somewhat or very unlikely, and “before clinic” and “as a result of clinic” responses were compared using the chi-square test. In addition, we calculated the overall number of residents whose likelihood of entering GIM as a result of the clinic experience was more, less, or unchanged compared to before the clinic experience and compared residents’ likelihood of entering GIM before versus as a result of clinic using the Wilcoxon rank sum test. We examined associations between satisfaction with clinic elements and consideration of a career in GIM using the chi-square test. We applied a Bonferroni correction to these association analyses to account for multiple comparisons.
A Generalized Estimating Equation (GEE) model (to account for the population effect of the three unique study sites) was used to examine the association between elements on the satisfaction survey and GIM career plans as a result of the clinic experience, adjusting for demographic characteristics (gender, postgraduate year) and residents’ baseline interest in a GIM career.22 The selection of variables to include in the model used the following strategy based on the bivariate analysis.25,26 In domains in which only one item was significantly associated with career choice, that item was used. In domains in which more than one item showed a significant association, the model item was chosen based on previous knowledge about the importance of the item for clinic satisfaction and the modifiability of the item (i.e., continuity with patients is modifiable, reward from work is not). In domains in which no items had a significant association, the item that showed the strongest trend toward an association was used in the model. Iterative sensitivity analyses substituting multiple different items for each domain verified stability of the model. All analyses were completed using Statistical Program for the Social Sciences version 18.
Results
A total of 225 residents completed the survey for an overall 90 % response rate (MSSM, 84 %; TUSM, 93 %; JHBMC, 98 %). Residents were evenly distributed by gender, site, and postgraduate year. There were differences in career plans by site. For example, more residents at MSSM planned to pursue careers in academic medicine and a larger percentage of JHBMC residents planned to enter a GIM career before the continuity experience (Table 1).
Table 1.
Resident Characteristics
| Characteristics | Total | MSSM | TUSM | JHBMC | p value |
|---|---|---|---|---|---|
| N (%) | n (%) | n (%) | n (%) | ||
| All | 225 (100) | 93 (41) | 90 (40) | 42 (19) | |
| Female | 112 (50) | 45 (48) | 45 (50) | 22 (52) | 0.91 |
| Postgraduate Year | |||||
| 1 | 66 (29) | 31 (33) | 21 (23) | 14 (33) | 0.54 |
| 2 | 84 (37) | 35 (38) | 35 (39) | 14 (33) | |
| 3 | 75 (33) | 27 (29) | 34 (38) | 14 (33) | |
| Practice setting plan* | |||||
| Academic | 184 (82) | 85 (91) | 69 (77) | 30 (71) | 0.006 |
| Community | 28 (12) | 7 (8) | 17 (19) | 4 (10) | 0.05 |
| Private | 53 (24) | 15 (16) | 32 (36) | 6 (14) | 0.002 |
| Type of work plan* | |||||
| Clinical | 210 (93) | 88 (95) | 83 (92) | 39 (93) | 0.80 |
| Education | 102 (45) | 47 (51) | 38 (42) | 17 (41) | 0.41 |
| Research | 77 (34) | 42 (45) | 16 (18) | 19 (45) | <0.001 |
| Health policy/public health | 43 (19) | 13 (14) | 16 (18) | 14 (33) | 0.02 |
| Likely to consider employment in GIM BEFORE clinic experience | 107 (48) | 40 (43) | 37 (41) | 30 (71) | 0.003 |
Differences calculated using chi-square test
*
Respondents could select >1 choice for this question so percentages may be >100 %
Likelihood of Entering a Career in GIM
Overall, 48 % of residents reported that prior to beginning their residency training they intended to enter a career in GIM. However, 38 % reported being likely to enter a career in GIM as a result of clinic (p = 0.003). Comparing residents’ likelihood to enter GIM as a result of clinic to likelihood to enter a career in GIM before clinic showed that 59 % of residents had no difference in likelihood, 28 % reported a lower likelihood as a result of clinic, and 11 % reported higher likelihood as a result of clinic.
In the bivariate analysis of demographics, female vs. male residents (46 % vs. 31 %, p = 0.03) and JHBMC residents (p < 0.001) were more likely to consider entering GIM as a result of clinic (Table 2).
Table 2.
Demographics by Self-reported Likelihood of Entering GIM AS A RESULT of Clinic
| Demographics | Likely to enter GIM | Unlikely to enter GIM | p value |
|---|---|---|---|
| n = 86 | n = 139 | ||
| n (%) | n (%) | ||
| Overall | 38.2 % | 61.8 % | |
| Female | 51 (46) | 61 (54) | 0.03 |
| Male | 35 (31) | 78 (69) | |
| Postgraduate year | |||
| 1 | 24 (36) | 42 (64) | 0.79 |
| 2 | 31 (37) | 53 (63) | |
| 3 | 31(41) | 44 (59) | |
| Training site | |||
| MSSM | 23 (25) | 70 (75) | 0.001 |
| TUSM | 38 (42) | 52 (58) | |
| JHBMC | 25 (60) | 17 (40) | |
| Likely to consider employment in GIM BEFORE clinic | 72 (67) | 35 (33) | 0.001 |
Differences calculated using chi-square test
Resident Satisfaction with Elements of Clinic
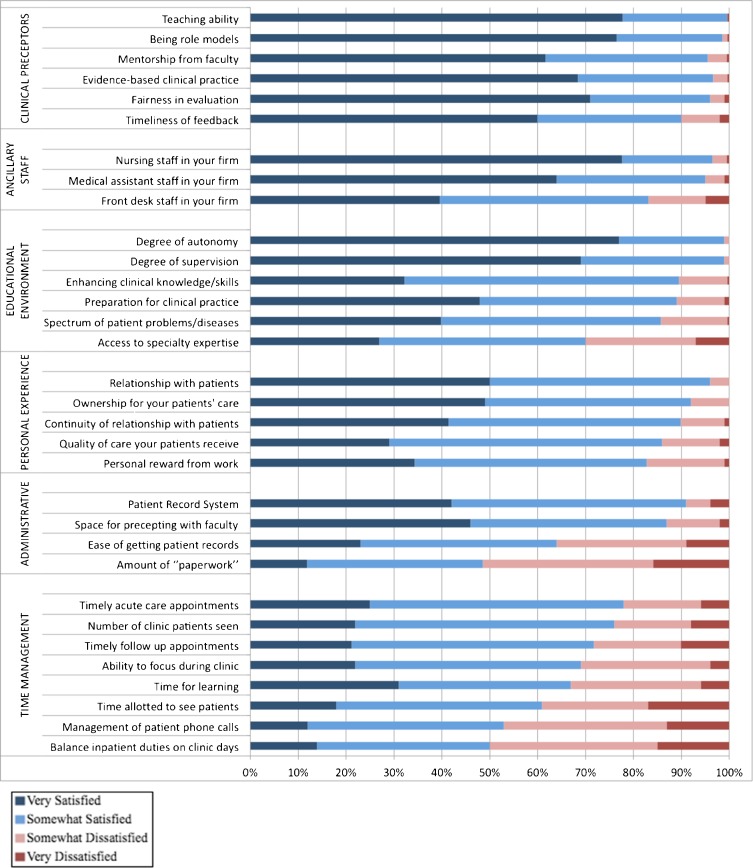
Residents reported high levels of satisfaction for nearly all elements of clinic. On average, 83 % were somewhat satisfied (39.5 %) or very satisfied (43.2 %) across all 32 elements. Highest ratings were given for the clinic preceptor domain (96 % somewhat satisfied or very satisfied) and lowest for time management (66 % somewhat satisfied or very satisfied) (Fig. 1).
Figure 1.
Residents reported satisfaction with elements of clinic.
Association of Clinic Experience with Likelihood of Entering a Career In General Internal Medicine
In the bivariate analyses, those who reported being likely to enter a career in GIM as a result of clinic reported significantly higher rates of being very satisfied with 6 of the 32 clinical elements when compared to those who were unlikely to enter a GIM career as a result of clinic (there were no elements for which they reported lower satisfaction). These included personal reward from work, the relationship with patients, and the continuity of the relationship with patients in the personal experience domain, number of clinic patients seen, and time allotted to see patients in the time management domain and mentorship from faculty in the clinical preceptor domain (Table 3).
In the multivariate GEE model, residents who were very satisfied with the continuity of relationships with their patients (OR 4.08, 95 % CI 2.50–6.64), the number of clinic patients seen (OR 2.40, 95 % CI 1.42–4.05), and who had intended to enter GIM prior to beginning residency clinic (OR 29.0, 95 % CI 24.0–34.8) were more likely to consider a career in GIM based on their outpatient clinical experience (Table 4). Gender and postgraduate year were not associated with intention to enter GIM in the adjusted model. These results were consistent across the sensitivity analyses described in the methods.
Table 4.
Adjusted Odds Ratios of Resident Self-reported Likelihood of Entering GIM AS A RESULT of Clinic across sites
| Clinic elements | GEE: adjusted odds ratio (95 % CI) | p value |
|---|---|---|
| Very satisfied with clinic element: | ||
| Preceptors as mentors | 1.07 (0.28–4.13) | 0.92 |
| Enhancement of clinical knowledge/skills | 1.22 (0.93–1.60) | 0.14 |
| Medical assistant staff in your firm | 1.11 (0.36–3.46) | 0.85 |
| Number of clinic patients seen | 2.40 (1.42–4.05) | 0.001 |
| Space for precepting with faculty | 1.11 (0.60–2.05) | 0.75 |
| Continuity of relationships with patients | 4.08 (2.50–6.64) | 0.001 |
| Demographic characteristics | ||
| Female gender | 1.48 (0.66–3.35) | 0.34 |
| Postgraduate year | ||
| 2 | 0.85 (0.23–3.14) | 0.80 |
| 3 | 0.50 (0.19–1.32) | 0.16 |
| Likely to consider employment in GIM BEFORE clinic experience | 29.0 (24.0–34.8) | 0.001 |
Calculated using a Generalized Estimating Equation across sites
Discussion
In this study of 225 IM residents from three academic training programs in different cities and clinical settings, most residents were satisfied with nearly all elements of their continuity clinic but overall were less likely to enter a GIM career as a result of clinic experience. Most importantly, we found that satisfaction with two elements of clinic, the number of patients seen and continuity of care with patients, was associated with residents’ likelihood of choosing GIM careers.
Surprisingly, we found very high levels of resident satisfaction with most elements of clinic studied in our survey. While one study showed similarly high satisfaction with clinic,19 many have shown that residents frequently feel stressed or overwhelmed by clinic,9 do not value it as highly as other training experiences (e.g., ICU and wards),19 and do not feel prepared to enter outpatient practice.9,27,28 One explanation for this dichotomy is that our study only addressed certain elements of clinic. Factors we did not study, such as patient no-show rates, lack of clinic resources, resident personality characteristics, and overall feelings of stress and/or burnout as well as known influences such as potential monetary compensation,21,22,29 greater comfort with the inpatient setting, and attraction to a specific specialty10 may contribute to the stress and devaluing of ambulatory training.
Despite being relatively satisfied with their clinic experience, 28 % of respondents were less likely to enter GIM as a result of their clinic experience, while only 11 % were more likely to enter a career in GIM as a result of clinic. A study of medical students exposed to an IM outpatient experience reported that equal numbers of students felt that the experience made a career in GIM more (32.1 %) or less attractive (33.0 %).10 The clinic experience does seem to influence some trainees’ career choices, and in our study population more were driven away from a primary care career. Ultimately, some elements of the clinic experience may drive a trainee toward one career path or another.
Our study found that resident satisfaction with the number of clinic patients seen in the time management domain and continuity of relationships with patients in the personal experience domain demonstrated associations with a GIM career choice. Our findings are corroborated by a similar smaller study that found an association between workflow and professional/personal satisfaction and choice of GIM.11 Collectively, these results demonstrate potential areas in which to focus efforts on improving the resident ambulatory clinic experience that may sway IM residents in the direction of primary care careers. Time management issues, such as the number of patients on their schedule, time allotted for patient care, and workflow issues, may adversely affect residents’ perception of a future GIM career. Efforts to improve these aspects of clinic by training residents in time management, increasing the time allotted for patient visits, minimizing inpatient interruptions, and decreasing inpatient/outpatient session overlap may improve residents’ perceptions of primary care careers. Moreover, the associations of residents’ satisfaction with continuity of relationships with patients and personal reward from work and consideration of a GIM career suggest that program and clinic directors should work to achieve real longitudinal relationships for residents and their patients. This has been a challenging problem in most resident clinics, but recent innovations such as the ambulatory long block and the “4 + 1” system of inpatient to ambulatory rotations may improve continuity.18,30
Of note, other studies have shown associations with gender and years in training and a generalist career.31,32 Our unadjusted model demonstrated the association with gender and GIM career choice, but the relationship was not evident in the adjusted model. This may be explained in part by the model’s adjustment for site and desire to enter GIM before the clinic experience, but may also relate to factors specific to the sites in this study.
Another important finding of this study is that, for a majority of residents, being likely to enter GIM before clinic was by far the strongest predictor of the likelihood of entering GIM. This finding highlights the importance of attracting physician trainees to primary care before and during medical school. One potential strategy to attract trainees early is via primary care tracks in residency, which have been shown to produce higher proportions of primary care internists than traditional categorical residencies.36,37 We were unable to study this effect because the small numbers of primary care residents in our programs would not allow for subgroup analysis. Another important strategy is to recruit more medical students into primary care. Fewer medical students are choosing primary care careers, probably because of the lack of financial incentives, an unappealing practice environment (e.g., large workload and short appointment length), and patient characteristics (e.g., multiple social issues).6,22,33 Medical students have reported that they would be more likely to enter primary care if they had increased ambulatory care experiences, more longitudinal relationships with patients, better GIM attending-student interaction, and higher salaries in primary care.22,34 US medical schools have begun to implement changes,35–39 such as primary care tracks, longitudinal ambulatory experiences, and preceptorships, but the impact on trainee career choice is not yet clear.
Our study has a number of important limitations. The percentage of residents reporting a likelihood of entering GIM (48 %) in our study is higher than the nationally reported numbers of approximately 20–27 %.2–8 Because percentages were high at all three sites, which are diverse in the housestaff they attract and their educational mission, the discrepancy seems most likely a result of the way the question was asked (likely to consider) and the answer phrasing (somewhat/very likely). Residents may also overestimate the likelihood that they would pursue a career in GIM before clinic, and the likelihood to pursue a career in GIM as a result of clinic may not correlate with actual career trajectory. We used a retrospective pre-post response as the outcome, limiting our ability to attribute a cause-and-effect relationship to our predictors and outcome and introducing possible recall bias. However, our survey contained a question that assessed baseline interest in a GIM career to control for an individual resident’s pre-clinic proclivity toward GIM. In addition, the wording of the outcome variable “as a result of” encouraged residents to consider whether their desire to go into GIM was attributable to the clinic experience, allowing us to better assess the impact of the clinic experience itself.
Concerns about ambulatory training of IM residents have led to increased scrutiny and regulatory efforts. Our study identified several areas of low resident satisfaction as well as features of the clinic experience that may lead residents to consider a career in GIM. We also found that interest in GIM that precedes residency training is associated with greater likelihood of entering a GIM career down the road. Targeting resources toward improving clinical elements such as patient continuity and workflow efficiency, which are associated with a higher likelihood of entering a primary care career, and increasing medical student interest in primary care may help build the primary care workforce.
Acknowledgments
Contributors
Deborah Korenstein, M.D.
Funding
There were no sources of funding for this study.
Prior Presentations
This work was presented as oral presentations at the National SGIM meetings in May 2011 and May 2012 as well as poster presentations at Regional SGIM in March 2011 and Mount Sinai Educational Research Day in April 2011.
Conflict of Interest
The authors declare that they do not have a conflict of interest.
References
- 1.Bodenheimer T, Pham HH. Primary care: Current problems and proposed solutions. Health Aff (Millwood) 2010;29(5):799–805. doi: 10.1377/hlthaff.2010.0026. [DOI] [PubMed] [Google Scholar]
- 2.Schwartz MD. Health care reform and the primary care workforce bottleneck. J Gen Intern Med. 2012;27(4):469–72. doi: 10.1007/s11606-011-1921-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Salsberg E, Rockey PH, Rivers KL, Brotherton SE, Jackson GR. US residency training before and after the 1997 balanced budget act. JAMA. 2008;300(10):1174–80. doi: 10.1001/jama.300.10.1174. [DOI] [PubMed] [Google Scholar]
- 4.Garibaldi RA, Popkave C, Bylsma W. Career plans for trainees in internal medicine residency programs. Acad Med. 2005;80(5):507–12. doi: 10.1097/00001888-200505000-00021. [DOI] [PubMed] [Google Scholar]
- 5.Jeffe DB, Whelan AJ, Andriole DA. Primary care specialty choices of United States medical graduates, 1997–2006. Acad Med. 2010;85(6):947–58. doi: 10.1097/ACM.0b013e3181dbe77d. [DOI] [PubMed] [Google Scholar]
- 6.Schwartz MD, Linzer M, Babbott D, Divine GW, Broadhead E. Medical student interest in internal medicine. Initial report of the society of general internal medicine interest group survey on factors influencing career choice in internal medicine. Ann Intern Med. 1991;114(1):6–15. doi: 10.7326/0003-4819-114-1-46. [DOI] [PubMed] [Google Scholar]
- 7.Accreditation Council for Graduate Medical Education data resource book [Internet].; 2011. Available from: http://www.acgme.org/acgmeweb/Portals/0/PFAssets/PublicationsBooks/2011-2012_ACGME_DATABOOK_DOCUMENT_Final.pdf. Accessed October 15, 2012.
- 8.Keirns CC, Bosk CL. Perspective: The unintended consequences of training residents in dysfunctional outpatient settings. Acad Med. 2008;83(5):498–502. doi: 10.1097/ACM.0b013e31816be3ab. [DOI] [PubMed] [Google Scholar]
- 9.Nadkarni M, Reddy S, Bates CK, Fosburgh B, Babbott S, Holmboe E. Ambulatory-based education in internal medicine: Current organization and implications for transformation. Results of a national survey of resident continuity clinic directors. J Gen Intern Med. 2011;26(1):16–20. doi: 10.1007/s11606-010-1437-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hauer KE, Durning SJ, Kernan WN, Fagan MJ, Mintz M, O’Sullivan PS, et al. Factors associated with medical students’ career choices regarding internal medicine. JAMA. 2008;300(10):1154–64. doi: 10.1001/jama.300.10.1154. [DOI] [PubMed] [Google Scholar]
- 11.Laponis R, O’Sullivan PS, Hollander H, Cornett P, Julian K. Educating generalists: factors of resident continuity clinic associated with perceived impact on choosing a generalist career. J Grad Med Educ. 2011;3(4):469–474. doi: 10.4300/JGME-D-10-00227.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Weinberger SE, Smith LG, Collier VU. Education committee of the American college of physicians. Redesigning training for internal medicine. Ann Intern Med. 2006;144(12):927–32. doi: 10.7326/0003-4819-144-12-200606200-00124. [DOI] [PubMed] [Google Scholar]
- 13.Holmboe ES, Bowen JL, Green M, Gregg J, DiFrancesco L, Reynolds E, et al. Reforming internal medicine residency training. A report from the Society of General Internal Medicine’s task force for residency reform. J Gen Intern Med. 2005;20(12):1165–72. doi: 10.1111/j.1525-1497.2005.0249.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Meyers FJ, Weinberger SE, Fitzgibbons JP, Glassroth J, Duffy FD, Clayton CP, et al. Redesigning residency training in internal medicine: The consensus report of the Alliance for Academic Internal Medicine Education redesign task force. Acad Med. 2007;82(12):1211–9. doi: 10.1097/ACM.0b013e318159d010. [DOI] [PubMed] [Google Scholar]
- 15.Keitz SA, Holland GJ, Melander EH, Bosworth HB, Pincus SH. VA learners’ perceptions working group. The veterans affairs learners’ perceptions survey: The foundation for educational quality improvement. Acad Med. 2003;78(9):910–7. doi: 10.1097/00001888-200309000-00016. [DOI] [PubMed] [Google Scholar]
- 16.Cannon GW, Keitz SA, Holland GJ, Chang BK, Byrne JM, Tomolo A, et al. Factors determining medical students‘and residents’ satisfaction during VA-based training: Findings from the VA learners’ perceptions survey. Acad Med. 2008;83(6):611–20. doi: 10.1097/ACM.0b013e3181722e97. [DOI] [PubMed] [Google Scholar]
- 17.Warm EJ. Interval examination: The ambulatory long block. J Gen Intern Med. 2010;25(7):750–2. doi: 10.1007/s11606-010-1362-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Warm EJ, Schauer DP, Diers T, Mathis BR, Neirouz Y, Boex JR, et al. The ambulatory long-block: An Accreditation Council for Graduate Medical Education (ACGME) educational innovations project (EIP) J Gen Intern Med. 2008;23(7):921–6. doi: 10.1007/s11606-008-0588-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sisson SD, Boonyasai R, Baker-Genaw K, Silverstein J. Continuity clinic satisfaction and valuation in residency training. J Gen Intern Med. 2007;22(12):1704–10. doi: 10.1007/s11606-007-0412-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Henderson MC, Hunt DK, Williams JW., Jr General internists influence students to choose primary care careers: The power of role modeling. Am J Med. 1996;101(6):648–53. doi: 10.1016/S0002-9343(96)00334-8. [DOI] [PubMed] [Google Scholar]
- 21.DeWitt DE, Curtis JR, Burke W. What influences career choices among graduates of a primary care training program? J Gen Intern Med. 1998;13(4):257–61. doi: 10.1046/j.1525-1497.1998.00076.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.DeZee KJ, Maurer DDO, Colt R, Shimeall W, Mallory R, Powers JMSS, et al. Effect of financial remuneration on specialty choice of fourth-year US medical students. Acad Med. 2011;86(2):187–93. doi: 10.1097/ACM.0b013e3182045ec9. [DOI] [PubMed] [Google Scholar]
- 23.Gazewood JD, Owen J, Rollins LK. Effect of generalist preceptor specialty in a third-year clerkship on career choice. Fam Med. 2002;34(9):673–7. [PubMed] [Google Scholar]
- 24.Wright S, Wong A, Newill C. The impact of role models on medical students. J Gen Intern Med. 1997;12(1):53–6. doi: 10.1007/s11606-006-0007-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fitzmaurice GM, Laird NM, Ware JH. Applied longitudinal analysis. Hoboken, NJ: Wiley; 2004. [Google Scholar]
- 26.Wisnivesky JP, Leventhal H, Halm EA. Predictors of asthma-related health care utilization and quality of life among inner-city patients with asthma. J Allergy Clin Immunol. 2005;116(3):636–42. doi: 10.1016/j.jaci.2005.05.031. [DOI] [PubMed] [Google Scholar]
- 27.Wiest FC, Ferris TG, Gokhale M, Campbell EG, Weissman JS, Blumenthal D. Preparedness of internal medicine and family practice residents for treating common conditions. JAMA. 2002;288(20):2609–14. doi: 10.1001/jama.288.20.2609. [DOI] [PubMed] [Google Scholar]
- 28.Blumenthal D, Gokhale M, Campbell EG, Weissman JS. Preparedness for clinical practice: Reports of graduating residents at academic health centers. JAMA. 2001;286(9):1027–34. doi: 10.1001/jama.286.9.1027. [DOI] [PubMed] [Google Scholar]
- 29.Kassler WJ, Wartman SA, Silliman RA. Why medical students choose primary care careers. Acad Med. 1991;66(1):41–3. doi: 10.1097/00001888-199101000-00012. [DOI] [PubMed] [Google Scholar]
- 30.Mariotti JL, Shalaby M, Fitzgibbons JP. The 4ratio1 schedule: A novel template for internal medicine residencies. J Grad Med Educ. 2010;2(4):541–7. doi: 10.4300/JGME-D-10-00044.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Connelly MT, Sullivan AM, Peters AS, Clark-Chiarelli N, Zotov N, Martin N, et al. Variation in predictors of primary care career choice by year and stage of training. J Gen Intern Med. 2003;18(3):159–69. doi: 10.1046/j.1525-1497.2003.01208.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Compton MT, Frank E, Elon L, Carrera J. Changes in US medical students’ specialty interests over the course of medical school. J Gen Intern Med. 2008;23(7):1095–100. doi: 10.1007/s11606-008-0579-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Markert RJ. Original contributions. Why medical students change to and from primary care as a career choice. Fam Med. 1991;23(5):347–50. [PubMed] [Google Scholar]
- 34.McMurray JE, Schwartz MD, Genero NP, Linzer M. The attractiveness of internal medicine: A qualitative analysis of the experiences of female and male medical students. Ann Intern Med. 1993;119(8):812–8. doi: 10.7326/0003-4819-119-8-199310150-00007. [DOI] [PubMed] [Google Scholar]
- 35.Norris TE, Schaad DC, DeWitt D, Ogur B, Hunt DD. Consortium of Longitudinal Integrated Clerkships. Longitudinal integrated clerkships for medical students: An innovation adopted by medical schools in Australia, Canada, South Africa, and the United States. Acad Med. 2009;84(7):902–7. doi: 10.1097/ACM.0b013e3181a85776. [DOI] [PubMed] [Google Scholar]
- 36.Colgan R, Iafolla CE, Rooks Y, Stewart DL. Increasing student interest in family medicine and urban health care: The family care tract. Md Med. 2009;10(1):21. [PubMed] [Google Scholar]
- 37.Mennin SP, Kalishman S, Friedman M, Pathak D, Snyder J. A survey of graduates in practice from the University of New Mexico’s conventional and community-oriented, problem-based tracks. Acad Med. 1996;71(10):1079–89. doi: 10.1097/00001888-199610000-00015. [DOI] [PubMed] [Google Scholar]
- 38.Medical schools invest in primay care [Internet].; March 22, 2011. Available from: http://www.usnews.com/education/best-graduate-schools/articles/2011/03/22/medical-schools-invest-in-primary-care. Accessed October 15, 2012.
- 39.Corbett EC, Jr, Owen JA, Hayden GF. Effect of a second-year primary care preceptorship on medical students’ career plans. South Med J. 2002;95(7):691–4. [PubMed] [Google Scholar]